Effects of Physical Activity on Cognition, Behavior, and Motor Skills in Youth with Autism Spectrum Disorder: A Systematic Review of Intervention Studies
Abstract
1. Introduction
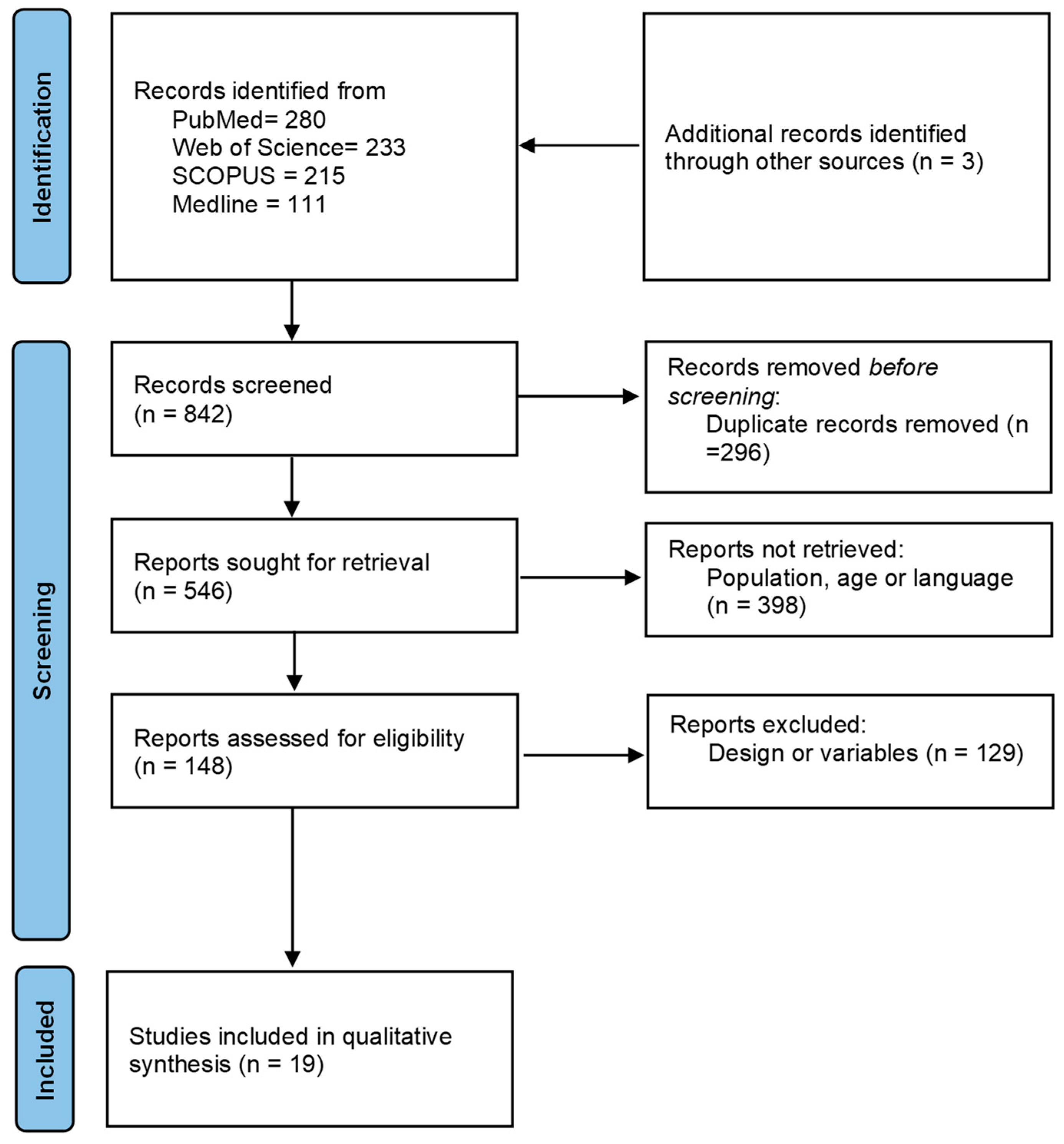
2. Methods
2.1. Search Limits
- (1)
- Physical activity (physical fitness, cardiovascular fitness, physical activity, physical education, fitness, exercise, physical exercise, healthy exercise, aerobic exercise, resistance exercise, and anaerobic exercise).
- (2)
- Autism spectrum disorder (ADD, Asperger, autism, and autistic).
- (3)
- Cognition (cognition, academic, cognitive, executive function, memory, attention, creativity, perception, and behavior)
- (4)
- Children and adolescents (adolescent, teenagers, children, childhood, school-age youth, and student).
2.2. Selection Criteria
2.3. Data Extraction and Reliability
2.4. Quality Assessment and Level of Evidence
3. Results
3.1. General Findings
3.2. Acute Effect of Physical Activity on Cognition, Behavior, and Motor Skill
3.3. Chronic Effect of Physical Activity on Cognition, Behavior, and Motor Skill
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition Text Revision (DSM-5-TR®); American Psychiatric Pub.: Washington, DC, USA, 2022. [Google Scholar]
- Eaton, C.; Roarty, K.; Doval, N.; Shetty, S.; Goodall, K.; Rhodes, S.M. The Prevalence of Attention Deficit/Hyperactivity Disorder Symptoms in Children and Adolescents with Autism Spectrum Disorder without Intellectual Disability: A Systematic Review. J. Atten. Disord. 2023, 27, 1360–1376. [Google Scholar] [CrossRef]
- Hallmayer, J.; Cleveland, S.; Torres, A.; Phillips, J.; Cohen, B.; Torigoe, T.; Miller, J.; Fedele, A.; Collins, J.; Smith, K.; et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch. Gen. Psychiatry 2011, 68, 1095–1102. [Google Scholar] [CrossRef] [PubMed]
- Maenner, M.J.; Shaw, K.A.; Baio, J. Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill. Summ. 2020, 69, 1–12. [Google Scholar] [CrossRef]
- Salari, N.; Rasoulpoor, S.; Rasoulpoor, S.; Shohaimi, S.; Jafarpour, S.; Abdoli, N.; Khaledi-Paveh, B.; Mohammadi, M. The global prevalence of autism spectrum disorder: A comprehensive systematic review and meta-analysis. Ital. J. Pediatr. 2022, 48, 1–16. [Google Scholar] [CrossRef]
- Bombonato, C.; Del Lucchese, B.; Ruffini, C.; Di Lieto, M.C.; Brovedani, P.; Sgandurra, G.; Cioni, G.; Pecini, C. Far Transfer Effects of Trainings on Executive Functions in Neurodevelopmental Disorders: A Systematic Review and Metanalysis. Neuropsychol. Rev. 2023, 34, 98–133. [Google Scholar] [CrossRef]
- Mallise, C.A.; Lane, A.E.; Woolard, A.J.; Whalen, O.M.; Murphy, V.E.; Karayanidis, F.; Campbell, L.E. The temperament features associated with autism spectrum disorder in childhood: A systematic review. Res. Dev. Disabil. 2020, 104, 103711. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ariza, A.; Grao-Cruces, A.; de Loureiro, N.E.M.; Martínez-López, E.J. Influence of physical fitness on cognitive and academic performance in adolescents: A systematic review from 2005–2015. Int. Rev. Sport Exerc. Psychol. 2017, 10, 108–133. [Google Scholar] [CrossRef]
- Berkson, G.; Tupa, M. Early development of stereotyped and self-injurious behaviors. J. Early Interv. 2000, 23, 1–19. [Google Scholar] [CrossRef]
- Cibralic, S.; Kohlhoff, J.; Wallace, N.; McMahon, C.; Eapen, V. Emotional Regulation and Language in Young Children with and without Autism Traits. J. Early Interv. 2023, 45, 83–103. [Google Scholar] [CrossRef]
- Melo, C.; Ruano, L.; Jorge, J.; Pinto Ribeiro, T.; Oliveira, G.; Azevedo, L.; Temudo, T. Prevalence and determinants of motor stereotypies in autism spectrum disorder: A systematic review and meta-analysis. Autism 2020, 24, 569–590. [Google Scholar] [CrossRef]
- Berse, T.; Rolfes, K.; Barenberg, J.; Dutke, S.; Kuhlenbaumer, G.; Volker, K.; Winter, B.; Wittig, M.; Knecht, S. Acute physical exercise improves shifting in adolescents at school: Evidence for a dopaminergic contribution. Front. Behav. Neurosci. 2015, 9, 196. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, J.; Dounavi, K.; Craig, E.A. The efficacy of using telehealth to coach parents of children with autism spectrum disorder on how to use naturalistic teaching to increase mands, tacts and intraverbals. J. Dev. Phys. Disabil. 2023, 35, 417–447. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.; Bond, C. A cross-national review of evidence-based psychosocial treatments for children and adolescents with autistic spectrum disorders in the United Kingdom, Ireland, and United States. Psychol. Sch. 2017, 54, 1160–1175. [Google Scholar] [CrossRef]
- Xiao, N.; Shinwari, K.; Kiselev, S.; Huang, X.; Li, B.; Qi, J. Effects of equine-assisted activities and therapies for individuals with autism spectrum disorder: Systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2023, 20, 2630. [Google Scholar] [CrossRef] [PubMed]
- Hodges, A.K.; Hathaway, K.L.; McMahon, M.X.; Volkert, V.M.; Sharp, W.G. Treatment of Feeding Concerns in Children with Autism Spectrum Disorder: A Systematic Review of Behavioral Interventions with Caregiver Training. Behav. Modif. 2023, 47, 936–958. [Google Scholar] [CrossRef] [PubMed]
- Juliano, A.C.; Alexander, A.O.; DeLuca, J.; Genova, H. Feasibility of a school-based mindfulness program for improving inhibitory skills in children with autism spectrum disorder. Res. Dev. Disabil. 2020, 101, 103641. [Google Scholar] [CrossRef]
- Milajerdi, H.R.; Sheikh, M.; Najafabadi, M.G.; Saghaei, B.; Naghdi, N.; Dewey, D. The Effects of Physical Activity and Exergaming on Motor Skills and Executive Functions in Children with Autism Spectrum Disorder. Games Health J. 2021, 10, 33–42. [Google Scholar] [CrossRef]
- Sansi, A.; Nalbant, S.; Ozer, D. Effects of an Inclusive Physical Activity Program on the Motor Skills, Social Skills and Attitudes of Students with and without Autism Spectrum Disorder. J. Autism Dev. Disord. 2020, 51, 2254–2270. [Google Scholar] [CrossRef]
- Nakutin, S.N.; Gutierrez, G. Effect of Physical Activity on Academic Engagement and Executive Functioning in Children with ASD. Sch. Psychol. Rev. 2019, 48, 177–184. [Google Scholar] [CrossRef]
- Raichlen, D.A.; Polk, J.D. Linking brains and brawn: Exercise and the evolution of human neurobiology. Proc. R. Soc. Lond. B Biol. Sci. 2013, 280, 9–18. [Google Scholar] [CrossRef]
- Hillier, A.; Murphy, D.; Ferrara, C. A Pilot Study: Short-term Reduction in Salivary Cortisol Following Low Level Physical Exercise and Relaxation among Adolescents and Young Adults on the Autism Spectrum. Stress Health 2011, 27, 395–402. [Google Scholar] [CrossRef]
- Habibian, M.; Valinejad, A. Comparison of Brain-Derived Neurotrophic Factor (BDNF) and Insulin-like Growth Factor 1 (IGF-1) Responses to Different Endurance Training Intensities in Runner Men. Horiz. Med. Sci. 2017, 23, 273–277. [Google Scholar]
- Leckie, R.L.; Oberlin, L.E.; Voss, M.W.; Prakash, R.S.; Szabo-Reed, A.; Chaddock-Heyman, L.; Phillips, S.M.; Gothe, N.P.; Mailey, E.; Vieira-Potter, V.J.; et al. BDNF mediates improvements in executive function following a 1-year exercise intervention. Front. Hum. Neurosci. 2014, 8, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Ohara, R.; Kanejima, Y.; Kitamura, M.; P Izawa, K. Association between social skills and motor skills in individuals with autism spectrum disorder: A systematic review. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 276–296. [Google Scholar] [CrossRef] [PubMed]
- Columna, L.; Felizola, G.; Prieto, L.; Myers, B.; Streete, D.; Lightburn, A. The experiences of Hispanic families of children with autism spectrum disorder regarding physical activity. Res. Dev. Disabil. 2020, 107, 103785. [Google Scholar] [CrossRef] [PubMed]
- Shahane, V.; Kilyk, A.; Srinivasan, S.M. Effects of physical activity and exercise-based interventions in young adults with autism spectrum disorder: A systematic review. Autism 2024, 28, 276–300. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Hamilton, M. The effects of physical activity on the stereotypic behaviors of children with autism spectrum disorder. J. Sport Exerc. Psychol. 2013, 35, S68. [Google Scholar] [CrossRef]
- Tarr, C.W.; Rineer-Hershey, A.; Larwin, K. The effects of physical exercise on stereotypic behaviors in Autism: Small-n meta-analyses. Focus Autism Other Dev. Disabil. 2020, 35, 26–35. [Google Scholar] [CrossRef]
- Golden, D.; Liang, L.Y.; Getchell, N. The Effects of Xbox Kinect Active Video Gaming on Executive Function, Inhibition, in Children with and without Autism Spectrum Disorder: A Pilot Study. J. Behav. Brain Sci. 2022, 12, 287–301. [Google Scholar] [CrossRef]
- Tse, C.Y.A.; Lee, H.P.; Chan, K.S.K.; Edgar, V.B.; Wilkinson-Smith, A.; Lai, W.H.E. Examining the impact of physical activity on sleep quality and executive functions in children with autism spectrum disorder: A randomized controlled trial. Autism 2019, 23, 1699–1710. [Google Scholar] [CrossRef]
- Nicholson, H.; Kehle, T.J.; Bray, M.A.; Heest, J.V. The effects of antecedent physical activity on the academic engagement of children with autism spectrum disorder. Psychol. Sch. 2011, 48, 198–213. [Google Scholar] [CrossRef]
- Ketcheson, L.; Hauck, J.; Ulrich, D. The effects of an early motor skill intervention on motor skills, levels of physical activity, and socialization in young children with autism spectrum disorder: A pilot study. Autism: The International Journal of Research and Practice. A pilot study. Autism 2016, 21, 481–492. [Google Scholar] [CrossRef]
- Pan, C.Y.; Hsu, P.J.; Chung, I.C.; Hung, C.S.; Liu, Y.J.; Lo, S.Y. Physical activity during the segmented school day in adolescents with and without autism spectrum disorders. Res. Autism Spectr. Disord. 2015, 15, 21–28. [Google Scholar] [CrossRef]
- Brand, S.; Jossen, S.; Holsboer-Trachsler, E.; Pühse, U.; Gerber, M. Impact of aerobic exercise on sleep and motor skills in children with autism spectrum disorders—A pilot study. Neuropsychiatr. Dis. Treat. 2015, 11, 1911–1920. [Google Scholar] [CrossRef]
- Wiggs, K.K.; Thornton, K.; Fredrick, J.W.; Lowman, C.N.; Langberg, J.M.; Becker, S.P. Physical and Extracurricular Activity in Adolescents with and without ADHD: Examining Group Differences and the Role of Cognitive Disengagement Syndrome Symptoms. J. Atten. Disord. 2023, 27, 1207–1222. [Google Scholar] [CrossRef]
- Lee, J.; Healy, S.; Haegele, J.A. Environmental and social determinants of leisure-time physical activity in children with autism spectrum disorder. Disabil. Health J. 2022, 15, 101340. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.-Y.; Chu, C.-H.; Tsai, C.-L.; Sung, M.-C.; Huang, C.-Y.; Ma, W.-Y. The impacts of physical activity intervention on physical and cognitive outcomes in children with autism spectrum disorder. Autism Int. J. Res. Pract. 2017, 21, 190–2002. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Li, R.; Wong, S.H.; Sum, R.K.; Wang, P.; Yang, B.; Sit, C.H. The effects of exercise interventions on executive functions in children and adolescents with autism spectrum disorder: A systematic review and meta-analysis. Sports Med. 2022, 52, 75–88. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.; Boutron, I.; Hoffmann, T.; Mulrow, C.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews; BMJ Publishing Group Ltd.: London, UK, 2020. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [Updated September 2016]; The Cochrane Collaboration: London, UK, 2013. [Google Scholar]
- Anderson-Hanley, C.; Tureck, K.; Schneiderman, R.L. Autism and exergaming: Effects on repetitive behaviors and cognition. Psychol. Res. Behav. Manag. 2011, 4, 129. [Google Scholar] [CrossRef]
- Oriel, K.N.; George, C.L.; Peckus, R.; Semon, A. The effects of aerobic exercise on academic engagement in young children with autism spectrum disorder. Pediatr. Phys. Ther. 2011, 23, 187–193. [Google Scholar] [CrossRef]
- Vander, J.; Sprong, M. Commentary on “The Effects of Aerobic Exercise on Academic Engagement in Young Children with Autism Spectrum Disorder”. Pediatr. Phys. Ther. 2011, 23, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Obrusnikova, I.; Bibik, J.M.; Cavalier, A.R.; Manley, K. Integrating Therapy Dog Teams in a Physical Activity Program for Children with Autism Spectrum Disorders. JOPERD J. Phys. Educ. Recreat. Danc. 2012, 83, 37–48. [Google Scholar] [CrossRef]
- Andy, C.Y. Brief Report: Impact of a Physical Exercise Intervention on Emotion Regulation and Behavioral Functioning in Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2020, 50, 4191–4198. [Google Scholar] [CrossRef]
- Zhang, T.; Wang, Y.; Yli-Piipari, S.; Chen, A. Power of the curriculum: Content, context, and learning in physical education. Res. Q. Exerc. Sport 2020, 92, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Rafie, F.; Shikh, M.; Jalali, S.; Pourranjbar, M. Physical Exercises and Motor Skills in Autistic Children. Iran. J. Public Health 2015, 44, 724–725. [Google Scholar]
- Marzouki, H.; Soussi, B.; Selmi, O.; Hajji, Y.; Marsigliante, S.; Bouhlel, E.; Muscella, A.; Weiss, K.; Knechtle, B. Effects of Aquatic Training in Children with Autism spectrum disorder. Biology 2022, 11, 657. [Google Scholar] [CrossRef]
- Haghighi, A.H.; Broughani, S.; Askari, R.; Shahrabadi, H.; Souza, D.; Gentil, P. Combined physical training strategies improve physical fitness, behavior, and social skills of autistic children. J. Autism Dev. Disord. 2022, 53, 4271–4279. [Google Scholar] [CrossRef] [PubMed]
- Ludyga, S.; Gerber, M.; Bruggisser, F.; Leuenberger, R.; Brotzmann, M.; Trescher, S.; Förster, M.; Zou, L.; Herbrecht, E.; Hanke, M. A randomized cross-over trial investigating the neurocognitive effects of acute exercise on face recognition in children with autism spectrum disorder. Autism Res. 2023, 16, 1630–1639. [Google Scholar] [CrossRef]
- Martínez-López, E.J.; Ruiz-Ariza, A.; De La Torre-Cruz, M.; Suárez-Manzano, S. Alternatives of physical activity within school times and effects on cognition. A systematic review and educational practical guide. Psicología Educativa. Rev. Psicólogos Educ. 2021, 27, 37–50. [Google Scholar] [CrossRef]
- Tan, B.W.Z.; Cohen, L.; Pooley, J.A. Physical activity: Its implication on attention span and quality of life in children with autism spectrum disorders. GSTF J. Law Soc. Sci. 2013, 2, 108–116. [Google Scholar] [CrossRef]
- Pan, C.Y.; Tsai, C.L.; Hsieh, K.W. Physical Activity Correlates for Children with Autism Spectrum Disorders in Middle School Physical Education. Res. Q. Exerc. Sport 2011, 82, 491–498. [Google Scholar] [CrossRef]
- Tsuchida, R.; Yamaguchi, T.; Funabashi, D.; Koumi, Y.; Kita, I.; Nishijima, T. Exercise type influences the effect of an acute bout of exercise on hippocampal neuronal activation in mice. Neurosci. Lett. 2022, 783, 136707. [Google Scholar] [CrossRef] [PubMed]
- Earl, R.K.; Ward, T.; Gerdts, J.; Eichler, E.E.; Bernier, R.A.; Hudac, C.M. Sleep problems in children with ASD and gene disrupting mutations. J. Genet. Psychol. 2021, 182, 317–334. [Google Scholar] [CrossRef] [PubMed]
- Pitetti, K.H.; Rendoff, A.D.; Grover, T.; Beets, M.W. The efficacy of a 9-month treadmill walking program on the exercise capacity and weight reduction for adolescents with severe autism. J. Autism Dev. Disord. 2007, 37, 997–1006. [Google Scholar] [CrossRef] [PubMed]
- Cadenas-Sanchez, C.; Migueles, J.H.; Esteban-Cornejo, I.; Mora-Gonzalez, J.; Henriksson, P.; Rodriguez-Ayllon, M.; Ortega, F.B. Fitness, physical activity and academic achievement in overweight/obese children. J. Sports Sci. 2020, 38, 731–740. [Google Scholar] [CrossRef]
- Tasca, I.; Guidi, M.; Turriziani, P.; Mento, G.; Tarantino, V. Behavioral and Socio-Emotional Disorders in Intellectual Giftedness: A Systematic Review. Child Psychiatry Hum. Dev. 2022, 1–22. [Google Scholar] [CrossRef]
| Database | Search Strategy | Limits | Filter |
|---|---|---|---|
| PubMed |
| Publication date from 1 January 2010 to 1 June 2023 | 283 items filtered |
| Web of Science |
| Species: Humans | 233 items filtered |
| SCOPUS |
| Age: 6–12 and 13–18 | 215 items filtered |
| Medline |
| Language: English, French, and Spanish | 111 items filtered |
| Authors and Variables | A | B | C | D | E | F | Total Score | Quality Level |
|---|---|---|---|---|---|---|---|---|
| Anderson-Hanley et al. (2011) [42]. Exergaming, behaviors, cognition, and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Hillier et al. (2011) [22]. Exercise, relaxation, and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Nicholson et al. (2011) [32]. Physical activity, academic engagement, and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Oriel et al. (2011) [43]. Aerobic exercise, academic engagement, and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Vander and Sprong (2011) [44]. Aerobic exercise, academic engagement, and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Obrusnikova et al. (2012) [45]. Dog in physical activity and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Liu and Hamilton (2013) [28]. Physical activity, stereotypic behaviors, and ASD | 2 | 2 | 2 | 2 | 2 | 2 | 12 | HQ |
| Brand et al. (2015) [35]. Aerobic exercise, sleep, motor skills, and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Ketcheson et al. (2016) [33]. Early motor skill intervention, motor skills, physical activity, socialization, and ASD | 2 | 2 | 2 | 1 | 2 | 2 | 11 | HQ |
| Pan et al. (2017) [38]. Physical activity, physical and cognitive outcomes, and ASD | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Nakutin and Gutierrez (2019) [20]. Jogging for academic engagement | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Tse et al. (2019) [31]. Basketball and inhibitory control | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Andy (2020) [46]. Moderate to vigorous jogging and emotion regulation | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Zhang et al. (2020) [47]. Mini-basketball, working memory, and regulation | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Rafiei et al. (2021) [48]. SPARK and Kinect and executive function | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Golden et al. (2022) [30]. Active video gaming, response time, and accuracy | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Marzouki et al. (2022) [49]. Combined physical training | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Haghighi et al. (2022) [50]. Aquatic training, stereotypic behaviors, communication, and social interaction | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Ludyga et al. (2023) [51]. Aerobic exercise and face recognition task | 2 | 2 | 2 | 1 | 2 | 0 | 9 | HQ |
| Author | Study Design/Intervention Acute or Chronic Confounders/Duration/Went | Sample/Age (Years)/Country | Groups/Physical Activity Measures | Cognition Measures | Results |
|---|---|---|---|---|---|
| Anderson-Hanley et al. (2011) [42] | Interventional, cross-over. Randomly/Acute/Diagnosis with DSM-IV and Gilliam Autism Rating Scale, 2nd edition/2 weeks (2 sessions)/During the summer. | 24 adolescent (4 girls)/10–18/14.8 ± 2.7/USA 10 boys and adolescent/8–21/13.2 ± 3.8/USA | Pilot I: 2 groups: EG (n = 12): Exergame 20 min CG (n = 12): Watched a 20 min video Pilot II: 2 groups: EG (n = 10): Exergaming “cybercycle” | Gilliam Autism Rating Scale, 2nd edition: Measurable behaviors and associated features of autism CCTT: Aspects of executive function, including task switching Stroop: Executive function, including inhibition of response Digit span forward and backward: Executive function captured in the backward performance | Repetitive behaviors significantly decreased, while performance on digits backwards improved following the exergaming conditions compared with the control condition. |
| Hillier et al. (2011) [22] | Interventional, cross-over. Randomly/Chronic/Diagnosis with DSM-IV. Time (each session)/8-week. One session a week/in the early evening (18:15–19:30 h). | 18 Adolescents (2 girls)/13–27/17.1/USA | 1 group: EG: 75 min physical exercise (aerobic, muscle strengthening, and bone strengthening) Cortisol level 2, 4, 6, and 8 | STAI: Self-report anxiety measure before and after each session | A significant reduction in cortisol at the end of the sessions compared with the beginning was observed. This was evaluated using a self-report anxiety measure. While the decreases in stress indicators were not maintained over time, the findings emphasize the potential of exercise and relaxation to improve stress symptoms. |
| Nicholson et al. (2011) [32] | Interventional, cross-over. Randomly/Chronic/Diagnosis of ASD/2 weeks. Three times per week. Before the classroom. | 4 children (all boys)/9/9/USA | 1 group: EG: ASD. 12 min jogging intervention + 5 min cool-down | BOSS: On task or academically engaged behavior | Large effect sizes for academic engagement time for all four students. They were more active after the intervention. |
| Oriel et al. (2011) [43] | Interventional, cross-over. Randomly. Contrabalanced/Chronic/Diagnosis of ASD/3 weeks + 3 weeks. Five times per week. Before the classroom. | 9 children (2 girls)/3–6/5.2/USA | 2 groups: EG (n = 9): 15 min of running/jogging followed by a classroom task CG (n = 9): Classroom task that was not preceded by aerobic exercise | AP: Correct academic responses, incorrect academic responses, stereotypic behaviors, and on-task behavior | Statistically significant improvements were found in correct responses following exercise (p < 0.05). No significant differences were found for on-task behavior or stereotypic behaviors. |
| Vander and Sprong (2011) [44] | Interventional, cross-over. Four classes were contrabalanced. Randomly/Chronic/Diagnosis of ASD/3 weeks + 3 weeks. Five times per week. Before the classroom. | 9 children (2 girls)/3–6/5.2/USA | 2 groups: EG (n = 9): 15 min of running/jogging followed by a classroom task CG (n = 9): Classroom task not preceded by exercise | AP: Correct academic responses, incorrect, or no academic responses Stereotypic behaviors (hand-and-arm flapping, body rocking, and toe walking) On-task behavior (when seated and producing academic responses) off-task when they did not produce an academic response and were engaged in disruptive behavior (e.g., crying, out of seat, or playing with objects) | Significant improvements were found in correctly responding following exercise (p < 0.05). No significant differences were found for on-task behavior or stereotypic behaviors. |
| Obrusnikova, Bibik, Cavalier, and Manley (2012) [45] | Interventional, cross-over. Contrabalanced/Acute/Diagnosis ASD Asperger/1 day. In the evening. | 4 children (all boys)/9–11/USA | EG (n = 4): MVPA with a dog CG (n = 4): MVPA The exercise consisted of 4 fitness stations and 2 skill stations (≈20 min) System for observing fitness instruction time | AP: Academic learning time–physical education | Regardless of the order of the intervention, the MVPA gains (Mgain ¼ 0.62) and the on-task behavior gains (Mgain ¼ 3.52) were larger for the therapy dog condition compared with the peer condition. These findings were confirmed in semistructured individual interviews with the children’s parents and instructors. |
| Liu and Hamilton (2013) [28] | Interventional, cross-over/Acute/Age, gender, and disorder. Diagnosis ASD/4 days. Four sessions. Before the classroom. | 23 children and adolescents (6 girls)/5–13/USA | 1 group: Intervention: MVPA for 15 min a day Measures pre and post each season Each day different PA type Heart rate | Children’s behaviors: Stereotypic behavior (was defined as the child not participating in activities in an appropriate manner) and task-engaged behavior (was defined as the child acting appropriately in the current situation while listening to directions, as well as interacting well with others) | Physical activity was identified as moderate or vigorous based on the child’s heart rate. The child was observed for two and a half hours each day and their behaviors were then classified as either stereotypic behavior or task-engaged behavior. No significant behavior differences related to exercise on age, gender, or disorder were observed. |
| Brand et al. (2015) [35] | Interventional, cross-over/Chronic/Diagnosis of ASD with ICD-10/3-week. Three times per week. In the evening. | 10 Children (5 girls)/7–13/10 ± 2.34/Switzerland | 1 group: EG: 60 min (30 min bicycle + 30 min of training in coordination and especially in balance) Motor skills (balancing, throwing, some ball skills…) | Sleep-EEG, beginning and at the end of the study | Mild-to-moderate insomnia was reported in 70% of the children. Compared to nights without previous intervention, on nights following intervention sleep efficiency increased (d = 1.07), sleep onset latency shortened (d = 0.38), and wake time after sleep onset decreased for 63% of the sample (d = 1.09), as assessed via sleep-EEG. Mood in the morning, as rated by parents, improved after three weeks (d = 0.90), as did motor skills (ball playing, balance exercise: ds.0.6). |
| Ketcheson et al. (2016) [33] | Interventional, cross-over/Chronic Diagnosis with ADOS-2 and DSM-IV. Time point with cognitive t score/8 weeks. Five times per week. During the summer. | 20 children (5 girls)/4–6/-/USA | 2 groups: EG (n = 11): Motor skill instruction for 4 h/day, CG (n = 9): No intervention TGMD-2: Locomotor skills and object control skills) | ADOS-2: Full-scale intelligence quotients MSEL: Cognitive scales, including non-verbal problem solving, fine, receptive language, and expressive language VABS-2: Standardized parental report measure of overall adaptive behavior POPE: Behavior coding system | A significant effect of time (for decreasing minutes) solitary (F(4, 8.76) = 7.94, p < 0.01). No significant effects of time (for increasing or decreasing minutes) were found in the remaining POPE-dependent variables, including joint engagement, parallel play, or onlooking. Significant differences between groups in all three motor outcomes, locomotor (F(1, 14) = 10.07, p < 0.001, partial η2 = 0.42), object control (F(1, 14) = 12.90, p < 0.001, partial η2 = 0.48), and gross quotient (F(1, 14) = 15.61, p < 0.01, partial η2 = 0.53) were observed. No comparison between ADOS and MSEL. |
| Pan et al. (2017) [38] | Interventional, cross-over, Randomly/Chronic/Diagnosis with DSM-IV-TR/2 × 12-weeks. A total of 2 sessions per week (24 sessions). After school. | 22 children (all boys)/6–12/9.08 ± 1.75/China | 2 groups: 2 TIMES: Time 1: Group A (n = 11): 70 min per session; warm-up (5 min), motor skills (20 min), executive function (20 min), group games (20 min), and cool-down (5 min). Group B (n = 11): No PA session Time 2: Group A: Follow up (No PA session) Group B: 12-weeks intervention Anthropometric measurements and bioelectrical impedance BOT-2: Motor skill proficiency | WCST: Executive function | Both groups of children with autism spectrum disorder exhibited significant improvements in motor skill proficiency (the total motor composite and two motor-area composites) and executive function (three indices of the WCST after 12 weeks of physical activity intervention). In addition, the effectiveness appeared to have been sustained for at least 12 weeks in Group A. |
| Nakutin and Gutierrez (2019) [20] | Interventional/Chronic/Diagnosis with DSM-V/7-weeks, 2 sessions per week (13 sessions) × 2. During academic activities (9h). | 3 children (2 girls)/6–7/-/USA | 1 group—2 times: Intervention: 13 sessions. Jogging duration was 12 min, followed by a 5-min cool-down Non-intervention: 13 sessions | BOSS: Academic engagement GNG: Inhibition Digits forward and backward tasks: Working memory STP: Social validity | Large effect sizes for academic engagement were found. No significant improvement in working memory and inhibition was observed. |
| Tse et al. (2019) [31] | Interventional, Randomly/Chronic/Diagnosis with DSM-V/12-weeks, 2 sessions per week (24 sessions). Before the classroom. | 40 children (8 girls)/8–12/9.95 ± 1.17/China | 2 groups: EG (n = 19): 45 min per session. Warmup (10 min), basketball (30 min), and cool-down (5 min). CG (n = 21): No intervention 4 sleep parameters (ActiGraph GT3X) | GNG: Inhibition control CBTT, FDS, BDS: Working memory | Significant improvement in inhibitory control (EG) was found. No significant improvement in working memory (all) was observed. |
| Andy (2020) [46] | Interventional, cross-over, Randomly/Chronic/Diagnosis with DSM-V/12-weeks, 4 sessions per week (48 sessions). At school. | 27 children (4 girls)/8–12/10.07 ± 1.10/China | 2 groups: EG (n = 15): 30 min per session, jogging. Moderate to vigorous (heart rate monitor) CG (n = 12): No intervention | ERC: Emotion regulation CBCL: Behavioral functioning | Significant improvement in emotion regulation and a reduction in behavioral problems were observed. |
| Zhang et al. (2020) [47] | Interventional/Chronic/Diagnosis with DSM-V/12-weeks, five days per week (60 sessions). At school. | 33 children (5 girls)/3–6/4.92 ± 0.67/China | 2 groups: EG (n = 18): 40 min/session, mini-basketball training program. Moderate intensity (129–149 heart beats per minute). CG (n = 15): No intervention | CHEXI: Executive functions SRS-2 and RSR-R: Core symptoms (social communication impairment and repetitive behavior) | Significantly better performances in working memory (p < 0.01) and regulation behavior (p < 0.05) were observed. |
| Rafiei et al. (2021) [48] | Interventional/Chronic/Diagnosis with DSM-V/8-weeks, three times per week, 35 min/session (24 sessions). After school. | 60 children (3 girls)/6–10/8.45 ± 1.43/Iran | 3 groups: EG1 (n = 20): SPARK EG2 (n = 20): Kinect CG (n = 20): No intervention MABC-2: Motor skills | WCST: Executive function | Significantly better performances in motor skills (aiming and catching) (p < 0.05) on EG1 were observed. EG2 showed more correct responses than the EG1 and CG (conceptual responses and perseverative errors) (p < 0.01). |
| Golden et al. (2022) [30] | Interventional/Acute/Diagnosis with DSM-V/1 session for each condition (20 min). After school. | 8 boys/8–11/10.60 ± 1.52/USA | 3 conditions: EG1 (n = 8): Active video gaming EG2 (n = 8): Brisk walking CG (n = 8): Sedentary video gaming | Flanker task: Response time and accuracy | A significantly higher percentage on incongruent in reaction time for the CG was observed. EG1 and EG2 improved in accuracy. EG2 participants improved significantly in reaction time in the congruent condition. |
| Haghighi et al. (2022) [49] | Interventional/Chronic/Diagnosis with DSM-V/8 weeks, three times per week, 40–60 min/session/after school. | 16 children (7 girls)/6–10/9.00 ± 1.31/Spain | 2 groups: EG (n = 8): Combined physical training (ball game, rhythmic movements, and resistance training) CG (n = 8): No intervention MABC-2: Motor skills Physical fitness (cardiorespiratory fitness, muscle strength, flexibility, balance, and agility) | GARS-2: Stereotypic behaviors, communication, and social interaction | Significantly better performances in indicators of social skills such as stereotypic behavior and communication on EG were observed. Significantly better performances in handgrip strength, upper and lower body power, flexibility, balance, and agility were observed (p < 0.05). |
| Marzouki et al. (2022) [50] | Interventional/Chronic/Diagnosis with DSM-V/8 weeks, two times per week, 50 min/session (16 sessions/after school. | 28 children (7 girls)/6–7/6.30 ± 0.50/Germany | 3 groups: EG1 (n = 10): Technical aquatic activities program EG2 (n = 10): Game-based aquatic activities program CG (n = 8): No intervention TGMD-2: Motor skills | GARS-2: Stereotypic behaviors, communication, and social interaction ERC: Emotional regulation | Both forms of swimming had a positive effect on gross motor skills and stereotypic behaviors. Changes in emotional functioning, with respect to the control group, were observed (p < 0.05). |
| Ludyga et al. (2023) [51] | Interventional/Acute/Diagnosis with DSM-V/1 session/20 min/after school. | 29 children (1 girl)/7–12/10 ± 2/Swiss | 2 condition: EC (n = 8): Acute aerobic exercise (20-min moderately intense cycling) CC (n = 8): No intervention | Face recognition task EEG recordings + Eyetracking: Reaction time, correct responses, and accuracy rates | A greater increase in reaction time in the exercise groupcompared to the CC was observed, as well as impaired face recognition following aerobic exercise. |
| Stimulus | Age | Application | Effects | ||||
|---|---|---|---|---|---|---|---|
| Continuity of the Stimulus | Intensity | Type/Moment of Day | Cognitive and Academic Performance | Behavior | Motor Skills | ||
| 15–30 min aerobic exercise (jogging, bicycle, or swimming) | 3–12 | 5 days/week | 50–70% MHR | Before classroom | >Attention >Academic engagement <Incorrect responding >Correct responding | >Activity ≈Behaviors | ≈Stereotypic behaviors |
| 15–20 min physical exercise (coordination and aerobic), exergames (AURASMA App) | 6–18 | 5 days/week | >75% MHR | Activity break lessons/Classroom/In the evening | >Executive function | >Behaviors | <Stereotypic behaviors <Repetitive behaviors |
| 20–40 min circuit with animal therapy (horses or dog) | 6–12 | 1–2 days/week | MVPA | In the evening | >Task-engaged behavior | >Behaviors | ≈ |
| 30–60 min coordination and balance training | 6–12 | 3–5 days/week | MVPA | In the evening/Homework break | >Neural activity | ≈ | >Coordination and balance |
| 40–75 min aerobic exercise or sport (basketball, tennis, or football) | 6–18 | 2–3 day/week | MVPA | In the evening/Homework break | >Executive function | <Stress and anxiety >Relaxation | Total motor composite |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suárez-Manzano, S.; Ruiz-Ariza, A.; de Loureiro, N.E.M.; Martínez-López, E.J. Effects of Physical Activity on Cognition, Behavior, and Motor Skills in Youth with Autism Spectrum Disorder: A Systematic Review of Intervention Studies. Behav. Sci. 2024, 14, 330. https://doi.org/10.3390/bs14040330
Suárez-Manzano S, Ruiz-Ariza A, de Loureiro NEM, Martínez-López EJ. Effects of Physical Activity on Cognition, Behavior, and Motor Skills in Youth with Autism Spectrum Disorder: A Systematic Review of Intervention Studies. Behavioral Sciences. 2024; 14(4):330. https://doi.org/10.3390/bs14040330
Chicago/Turabian StyleSuárez-Manzano, Sara, Alberto Ruiz-Ariza, Nuno Eduardo Marques de Loureiro, and Emilio J. Martínez-López. 2024. "Effects of Physical Activity on Cognition, Behavior, and Motor Skills in Youth with Autism Spectrum Disorder: A Systematic Review of Intervention Studies" Behavioral Sciences 14, no. 4: 330. https://doi.org/10.3390/bs14040330
APA StyleSuárez-Manzano, S., Ruiz-Ariza, A., de Loureiro, N. E. M., & Martínez-López, E. J. (2024). Effects of Physical Activity on Cognition, Behavior, and Motor Skills in Youth with Autism Spectrum Disorder: A Systematic Review of Intervention Studies. Behavioral Sciences, 14(4), 330. https://doi.org/10.3390/bs14040330







