Effects of Myofascial Release Technique along with Cognitive Behavior Therapy in University Students with Chronic Neck Pain and Forward Head Posture: A Randomized Clinical Trial
Abstract
1. Introduction
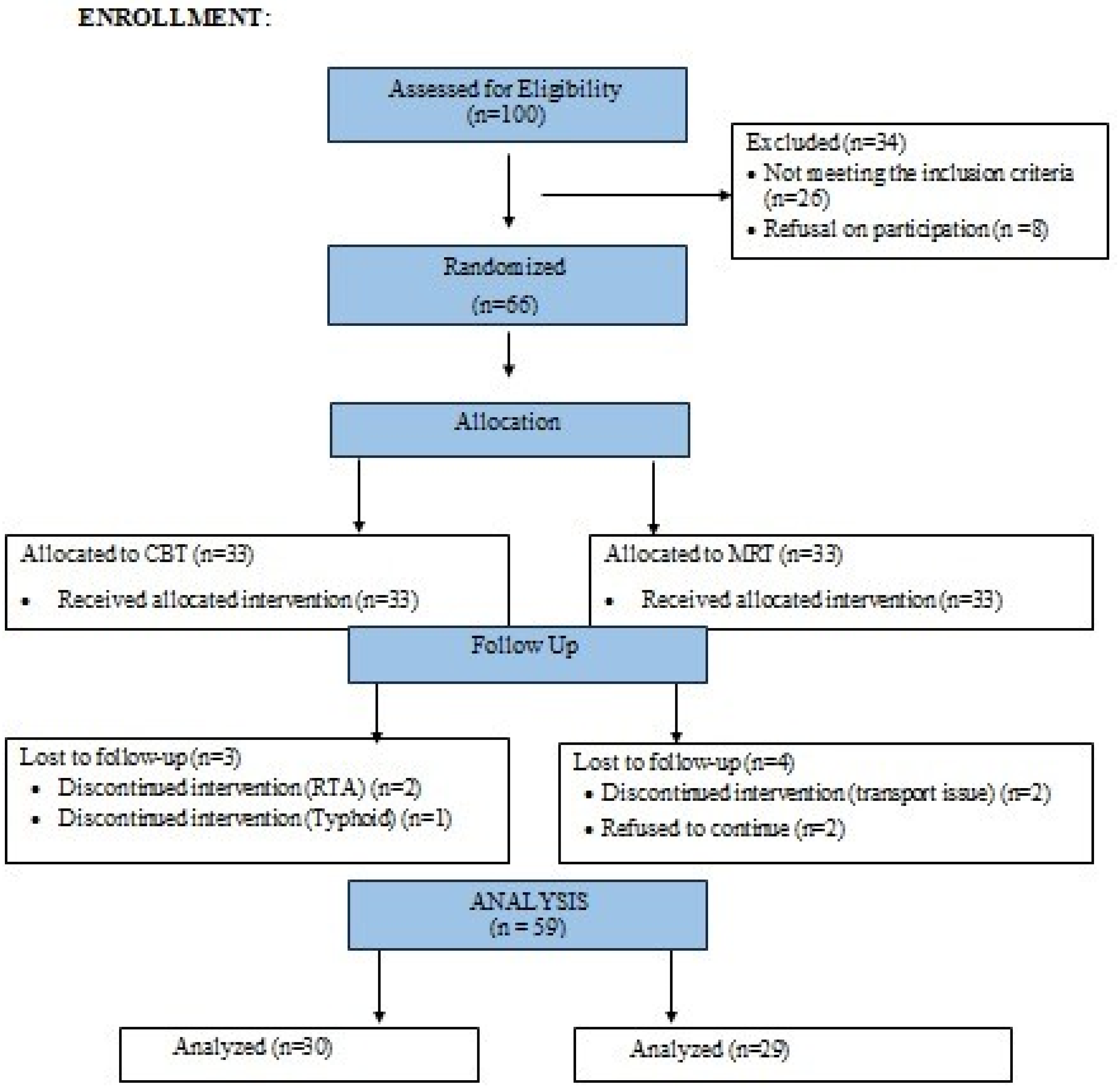
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Calculation
2.3. Inclusion and Exclusion Criteria
2.4. Randomization and Masking
2.5. Intervention
2.6. Outcome Measures
2.7. Data Analysis
3. Results
4. Discussion
4.1. Limitations of the Study
4.2. Strength and Implications of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Misailidou, V.; Malliou, P.; Beneka, A.; Karagiannidis, A.; Godolias, G. Assessment of patients with neck pain: A review of definitions, selection criteria, and measurement tools. J. Chirop. Med. 2010, 9, 49–59. [Google Scholar] [CrossRef]
- Harman, K.; Hubley-Kozey, C.L.; Butler, H. Effectiveness of an exercise program to improve forward head posture in normal adults: A randomized, controlled 10-week trial. J. Man. Manip. Ther. 2005, 13, 163–176. [Google Scholar] [CrossRef]
- Alsiwed, K.T.; Alsarwani, R.M.; Alshaikh, S.A.; Howaidi, R.A.; Aljahdali, A.J.; Bassi, M.M. The prevalence of text neck syndrome and its association with smartphone use among medical students in Jeddah, Saudi Arabia. J. Musculoskelet. Surg. Res. 2021, 5, 266–272. [Google Scholar] [CrossRef]
- Ylinen, J. Physical exercises and functional rehabilitation for the management of chronic neck pain. Eur. Medicophys. 2007, 43, 119–132. [Google Scholar]
- Szeto, G.P.; Straker, L.; Raine, S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl. Ergon. 2002, 33, 75–84. [Google Scholar] [CrossRef]
- Kim, S.Y.; Koo, S.J. Effect of duration of smartphone use on muscle fatigue and pain caused by forward head posture in adults. J. Phys. Ther. Sci. 2016, 28, 1669–1672. [Google Scholar] [CrossRef]
- Abdollahzade, Z.; Shadmehr, A.; Malmir, K.; Ghotbi, N. Effects of 4 week postural corrective exercise on correcting forward head posture. J. Mod. Rehab. 2017, 11, 85–92. [Google Scholar]
- Naz, A.; Bashir, M.S.; Noor, R. Prevalence of forward head posture among university students. Rawal Med. J. 2018, 43, 260–262. [Google Scholar]
- Gupta, B.D.; Aggarwal, S.; Gupta, B.; Gupta, M.; Gupta, N. Effect of deep cervical flexor training vs. conventional isometric training on forward head posture, pain, neck disability index in dentists suffering from chronic neck pain. J. Clin. Diagn. Res. 2013, 7, 2261–2264. [Google Scholar] [CrossRef]
- Joshi, R.; Poojary, N. The Effect of Muscle Energy Technique and Posture Correction Exercises on Pain and Function in Patients with Non-specific Chronic Neck Pain Having Forward Head Posture—A Randomized Controlled Trail. Int. J. Ther. Massage Bodyw. 2022, 15, 14–21. [Google Scholar]
- Im, B.; Kim, Y.; Chung, Y.; Hwang, S. Effects of scapular stabilization exercise on neck posture and muscle activation in individuals with neck pain and forward head posture. J. Phys. Ther. Sci. 2015, 28, 951–955. [Google Scholar] [CrossRef]
- Suwaidi, A.S.; Moustafa, I.M.; Kim, M.; Oakley, P.A.; Harrison, D.E. A Comparison of Two Forward Head Posture Corrective Approaches in Elderly with Chronic Non-Specific Neck Pain: A Randomized Controlled Study. J. Clin. Med. 2023, 12, 542. [Google Scholar] [CrossRef]
- Travell, J.G.; Simons, D.G. Myofascial Pain and Dysfunction: The Trigger Point Manual; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1992. [Google Scholar]
- Cabrera-Martos, I.; Rodríguez-Torres, J.; López-López, L.; Prados-Román, E.; Granados-Santiago, M.; Valenza, M.C. Effects of an active intervention based on myofascial release and neurodynamics in patients with chronic neck pain: A randomized controlled trial. Physiother. Theory Pract. 2022, 38, 1145–1152. [Google Scholar] [CrossRef]
- Park, S.J.; Lee, R.; Yoon, D.M.; Yoon, K.B.; Kim, K.; Kim, S.H. Factors associated with increased risk for pain catastrophizing in patients with chronic neck pain: A retrospective cross-sectional study. Medicine 2016, 95, e4698. [Google Scholar] [CrossRef]
- Cox, L.G.; Kidgell, D.J.; Iles, R.A. Neck-specific strengthening exercises and cognitive therapy for chronic neck pain: A systematic review. Phys. Ther. Rev. 2019, 24, 335–345. [Google Scholar] [CrossRef]
- Castro, M.; Daltro, C.; Kraychete, D.C.; Lopes, J. The cognitive behavioral therapy causes an improvement in quality of life in patients with chronic musculoskeletal pain. Ar. Neuro-Psiquiatr. 2012, 70, 864–868. [Google Scholar] [CrossRef]
- Monticone, M.; Baiardi, P.; Vanti, C.; Ferrari, S.; Nava, T.; Montironi, C.; Rocca, B.; Foti, C.; Teli, M. Chronic neck pain and treatment of cognitive and behavioural factors: Results of a randomised controlled clinical trial. Eur. Spine J. 2012, 21, 1558–1566. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Consort Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Int. J. Surg. 2011, 9, 672–677. [Google Scholar] [CrossRef]
- Khalid, A.; Ahmad, J.; Michelle, A.; Nazir, S.; Khalid, N.; Jabbar, F. Comparative effects of Myofascial Technique Alone and In Combination with Isometrics on Myofascial pain Syndrome Due to Excessive Smartfone Usage: Effect of Isometrics, Myofascial and Isolated Myofascial Release Technique on Myofascial Pain Syndrome. Pak. Biomed. J. 2022, 5, 212–217. [Google Scholar] [CrossRef]
- Becker, M.; Strunk, K.; Buschhaus, N.; Bühn, S.; Pieper, D. Methodological Quality of Physical Therapy Guidelines and Their Suitability for Adaptation: A Scoping Review. Phys. Ther. 2020, 100, 1296–1306. [Google Scholar] [CrossRef]
- Do, Y.L.; Nam, C.W.; Sung, Y.B.; Kim, K.; Lee, H.Y. Changes in rounded shoulder posture and forward head posture according to exercise methods. J. Phys. Ther. Sci. 2017, 29, 1824–1827. [Google Scholar]
- Zainuddin, I.; Shanat, M. The Interaction of Ergonomic and Anthropometric Factors in Occasional Chair Design for Elderly Malaysians. Int. J. Glob. Optim. Its Appl. 2023, 2, 60–73. [Google Scholar] [CrossRef]
- Young, I.A.; Cleland, J.A.; Michener, L.A.; Brown, C. Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am. J. Phys. Med. Rehabil. 2010, 89, 831–839. [Google Scholar] [CrossRef]
- Farooq, M.N.; Mohseni-Bandpei, M.A.; Gilani, S.A.; Hafeez, A. Urdu version of the neck disability index: A reliability and validity study. BMC Musculoskelet. Disord. 2017, 18, 149. [Google Scholar] [CrossRef]
- Dareh-Deh, H.R.; Hadadnezhad, M.; Letafatkar, A.; Peolsson, A. Therapeutic routine with respiratory exercises improves posture, muscle activity, and respiratory pattern of patients with neck pain: A randomized controlled trial. Sci. Rep. 2022, 12, 4149. [Google Scholar] [CrossRef]
- Elwardany, S.H.; Eleiny, K.E.; Arabia, S. Reliability of Kinovea computer program in measuring cervical range of motion in sagittal plane. Open Access Libr. J. 2015, 2, e1916. [Google Scholar] [CrossRef]
- Ploutarchou, G.; Savva, C.; Karagiannis, C.; Pavlou, K.; O’Sullivan, K.; Korakakis, V. The effectiveness of cognitive behavioural therapy in chronic neck pain: A systematic review with meta-analysis. Cogn. Behav. Ther. 2023, 52, 523–563. [Google Scholar] [CrossRef]
- Urits, I.; Hubble, A.; Peterson, E.; Orhurhu, V.; Ernst, C.A.; Kaye, A.D.; Viswanath, O. An update on cognitive therapy for the management of chronic pain: A comprehensive review. Curr. Pain Headache Rep. 2019, 23, 57. [Google Scholar] [CrossRef]
- Monticone, M.; Cedraschi, C.; Ambrosini, E.; Rocca, B.; Fiorentini, R.; Restelli, M.; Gianola, S.; Ferrante, S.; Zanoli, G.; Moja, L. Cognitive-behavioural treatment for subacute and chronic neck pain. Cochrane Database Syst. Rev. 2015, 5, CD010664. [Google Scholar] [CrossRef]
- Namvar, H.; Olyaei, G.; Moghadam, B.A.; Hosseinifar, M. Effect of myofascial release technique on pain, disability, maximum isometric contraction of the extensor muscles, and pressure pain threshold in patients with chronic nonspecific neck pain: Double blinded randomized clinical trial. Health Sci. 2016, 5, 500–506. [Google Scholar]
- El-Gendy, M.; Lasheen, Y.; Rezkalla, W. Multimodal approach of electrotherapy versus myofascial release in patients with chronic mechanical neck pain: A randomized controlled trial. Physiother. Q. 2019, 27, 6–12. [Google Scholar] [CrossRef]
- Parab, M.; Bedekar, N.; Shyam, A.; Sancheti, P. Immediate effects of myofascial release and cryo-stretching in management of upper trapezius trigger points-a comparative study. J. Soc. Indian Physiother. 2020, 4, 74–78. [Google Scholar] [CrossRef]

| CBT | MRT | |
|---|---|---|
| Outcome Measures | Mean ± SD | Mean ± SD |
| Gender | M = 24 | M = 24 |
| F = 09 | F = 09 | |
| Age (Years) | 22.6364 ± 1.76455 | 22.1212 ± 1.57634 |
| NPRS at baseline | 5.6061 ± 1.74892 | 4.7576 ± 1.65888 |
| CVA angle at baseline (Degrees) | 40.8433 ± 5.55882 | 40.8188 ± 5.82644 |
| NDI at baseline | 18.0606 ± 7.77793 | 15.8788 ± 7.80127 |
| Outcome Measures | N | Mean | Std. Deviation | 95% Confidence Interval for the Mean | F | p Value | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| NPRS at baseline | MRT and CBT | 33 | 5.606 | 1.748 | 4.985 | 6.226 | 1.910 | 0.172 |
| MRT Alone | 33 | 4.757 | 1.658 | 4.169 | 5.345 | |||
| NPRS in the fourth week | MRT and CBT | 30 | 3.133 | 1.041 | 2.744 | 3.522 | 4.089 | 0.047 |
| MRT Alone | 31 | 3.548 | 1.286 | 3.076 | 4.020 | |||
| NPRS in the eighth week | MRT and CBT | 29 | 1.241 | 0.510 | 1.047 | 1.435 | 29.338 | <0.001 |
| MRT Alone | 30 | 2.366 | 0.999 | 1.993 | 2.739 | |||
| Outcome Measures | N | Mean | Std. Deviation | 95% Confidence Interval for the Mean | F | p Value | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| CVA sngle at the Baseline | MRT and CBT | 30 | 40.843 | 5.558 | 38.767 | 42.919 | 0.000 | 0.987 |
| MRT | 32 | 40.818 | 5.826 | 38.718 | 42.919 | |||
| CVA angle in the fourth week | MRT and CBT | 29 | 46.106 | 5.928 | 43.852 | 48.361 | 0.852 | 0.360 |
| MRT | 30 | 44.710 | 5.698 | 42.582 | 46.837 | |||
| CVA angle in the eighth week | MRT and CBT | 29 | 49.655 | 6.545 | 47.165 | 52.145 | 5.812 | 0.019 |
| MRT | 30 | 45.456 | 6.821 | 42.909 | 48.003 | |||
| Outcome Measures | N | Mean | Std. Deviation | 95% Confidence Interval for the Mean | F | p Value | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| NDI at baseline | MRT and CBT | 33 | 18.060 | 7.777 | 15.302 | 20.818 | 1.294 | 0.259 |
| MRT Alone | 33 | 15.878 | 7.801 | 13.112 | 18.645 | |||
| NDI after the fourth week | MRT and CBT | 30 | 11.366 | 3.952 | 9.890 | 12.842 | 3.629 | 0.062 |
| MRT Alone | 31 | 9.322 | 4.407 | 7.705 | 10.939 | |||
| NDI after the eighth week | MRT and CBT | 29 | 5.551 | 2.180 | 4.722 | 6.381 | 5.253 | 0.026 |
| MRT Alone | 30 | 7.166 | 3.130 | 5.997 | 8.335 | |||
| Outcome Measures | Combinations at Different Time Points | Mean Difference | p-Value | 95% Confidence Interval for the Difference | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| NPRS | Baseline to Fourth Week | −2.509 | <0.001 * | −2.825 | −2.193 |
| Baseline to Eighth Week | −4.682 | <0.001 * | −5.203 | −4.161 | |
| Fourth Week to Eighth Week | −2.173 | <0.001 * | −2.558 | −1.788 | |
| Craniovertebral angle (degrees) | Baseline to Fourth Week | −2.463 | <0.001 * | −2.798 | −2.193 |
| Baseline to Eighth Week | −5.193 | <0.001 * | −5.745 | −4.647 | |
| Fourth Week to Eighth Week | −2.731 | <0.001 * | −3.172 | −2.298 | |
| Neck Disability Index | Baseline to Fourth Week | −2.323 | <0.001 * | −2.627 | −2.019 |
| Baseline to Eighth Week | −4.088 | <0.001 * | −4.476 | −3.701 | |
| Fourth Week to Eighth Week | −1.766 | <0.001 * | −1.987 | −1.544 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anwar, S.; Zahid, J.; Alexe, C.I.; Ghazi, A.; Mareș, G.; Sheraz, Z.; Sanchez-Gomez, R.; Perveen, W.; Alexe, D.I.; Gasibat, Q. Effects of Myofascial Release Technique along with Cognitive Behavior Therapy in University Students with Chronic Neck Pain and Forward Head Posture: A Randomized Clinical Trial. Behav. Sci. 2024, 14, 205. https://doi.org/10.3390/bs14030205
Anwar S, Zahid J, Alexe CI, Ghazi A, Mareș G, Sheraz Z, Sanchez-Gomez R, Perveen W, Alexe DI, Gasibat Q. Effects of Myofascial Release Technique along with Cognitive Behavior Therapy in University Students with Chronic Neck Pain and Forward Head Posture: A Randomized Clinical Trial. Behavioral Sciences. 2024; 14(3):205. https://doi.org/10.3390/bs14030205
Chicago/Turabian StyleAnwar, Sahreen, Junaid Zahid, Cristina Ioana Alexe, Abdullah Ghazi, Gabriel Mareș, Zainab Sheraz, Rubén Sanchez-Gomez, Wajida Perveen, Dan Iulian Alexe, and Qais Gasibat. 2024. "Effects of Myofascial Release Technique along with Cognitive Behavior Therapy in University Students with Chronic Neck Pain and Forward Head Posture: A Randomized Clinical Trial" Behavioral Sciences 14, no. 3: 205. https://doi.org/10.3390/bs14030205
APA StyleAnwar, S., Zahid, J., Alexe, C. I., Ghazi, A., Mareș, G., Sheraz, Z., Sanchez-Gomez, R., Perveen, W., Alexe, D. I., & Gasibat, Q. (2024). Effects of Myofascial Release Technique along with Cognitive Behavior Therapy in University Students with Chronic Neck Pain and Forward Head Posture: A Randomized Clinical Trial. Behavioral Sciences, 14(3), 205. https://doi.org/10.3390/bs14030205








