Family Metacognitive Training (MCT-F): Adapting MCT to Mothers with Psychosis and Their Adolescent Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Measures
2.4. Procedure
2.4.1. Step 1: Assessment
2.4.2. Step 2: Decision
2.4.3. Step 3: Administration
2.4.4. Step 4: Production
2.4.5. Step 5: Topical Experts
2.4.6. Step 6: Integration
2.4.7. Steps 7 and 8: Training and Testing
2.4.8. Data Analysis
3. Results
3.1. Step 1: Assessment of Needs and Different Intervention Options
3.2. Step 2: Decision
3.3. Step 3: Administration
3.4. Step 4: Production
3.5. Step 5: Topical Experts
3.6. Step 6: Integration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ochoa, S.; Haro, J.M.; Torres, J.V.; Pinto-Meza, A.; Palacín, C.; Bernal, M.; Brugha, T.; Prat, B.; Usall, J.; Alonso, J.; et al. What is the relative importance of self reported psychotic symptoms in epidemiological studies? Results from the ESEMeD--Catalonia Study. Schizophr. Res. 2008, 102, 261–269. [Google Scholar] [CrossRef]
- McGrath, J.J.; Hearle, J.; Jenner, L.; Plant, K.; Drummond, A.; Barkla, J.M. The fertility and fecundity of patients with psychoses. Acta Psychiatr. Scand. 1999, 99, 441–446. [Google Scholar] [CrossRef]
- Howard, L.M.; Kumar, R.; Thornicroft, G. Psychosocial characteristics and needs of mothers with psychotic disorders. Br. J. Psychiatry J. Ment. Sci. 2001, 178, 427–432. [Google Scholar] [CrossRef]
- Seeman, M.V. Sex differences in schizophrenia relevant to clinical care. Expert Rev. Neurother. 2021, 21, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Haukka, J.; Suvisaari, J.; Lönnqvist, J. Fertility of patients with schizophrenia, their siblings, and the general population: A cohort study from 1950 to 1959 in Finland. Am. J. Psychiatry 2003, 160, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Gayer-Anderson, C.; Morgan, C. Social networks, support and early psychosis: A systematic review. Epidemiol. Psychiatr. Sci. 2013, 22, 131–146. [Google Scholar] [CrossRef] [PubMed]
- Gentile, S.; Fusco, M.L. Schizophrenia and motherhood. Psychiatry Clin. Neurosci. 2019, 73, 376–385. [Google Scholar] [CrossRef]
- Wan, M.W.; Moulton, S.; Abel, K.M. A review of mother-child relational interventions and their usefulness for mothers with schizophrenia. Arch. Women’s Ment. Health 2008, 11, 171–179. [Google Scholar] [CrossRef]
- Andrea, R.; Joanne, N.; Michael, G.; Seeman, M.V. Parental Psychiatric Disorder: Distressed Parents and their Families. In Parental Psychiatric Disorder: Distressed Parents and Their Families, 3rd ed.; Cambridge University Press: Cambridge, UK, 2015; pp. 1–370. [Google Scholar] [CrossRef]
- Jones, N.; Godzikovskaya, J.; Zhao, Z.; Vasquez, A.; Gilbert, A.; Davidson, L. Intersecting disadvantage: Unpacking poor outcomes within early intervention in psychosis services. Early Interv. Psychiatry 2019, 13, 488–494. [Google Scholar] [CrossRef]
- Radley, J.; Sivarajah, N.; Moltrecht, B.; Klampe, M.L.; Hudson, F.; Delahay, R.; Barlow, J.; Johns, L.C. A Scoping Review of Interventions Designed to Support Parents With Mental Illness That Would Be Appropriate for Parents with Psychosis. Front. Psychiatry 2022, 12, 787166. [Google Scholar] [CrossRef]
- Cudjoe, E.; Tam CH, L.; Effah, D.; Amegashie, E.F.; Tweneboah, A.O. Living with parental mental illness is like a roller coaster: Reflections on children’s lifeworld in the family setting. J. Clin. Nurs. 2023, 32, 3516–3527. [Google Scholar] [CrossRef] [PubMed]
- Cooklin, A. Promoting children’s resilience to parental mental illness: Engaging the child’s thinking. Adv. Psychiatr. Treat. 2013, 19, 229–240. [Google Scholar] [CrossRef]
- Kaplan, K.; Brusilovskiy, E.; O’Shea, A.M.; Salzer, M.S. Child protective service disparities and serious mental illnesses: Results from a national survey. Psychiatr. Serv. 2019, 70, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Mendoza-García, S.; García-Mieres, H.; Lopez-Carrilero, R.; Sevilla-Llewellyn-Jones, J.; Birulés, I.; Barajas, A.; Lorente-Rovira, E.; Gutiérrez-Zotes, A.; Grasa, E.; Pousa, E.; et al. Influence of Maternal and Paternal History of Mental Health in Clinical, Social Cognition and Metacognitive Variables in People with First-Episode Psychosis. J. Pers. Med. 2022, 12, 1732. [Google Scholar] [CrossRef] [PubMed]
- Radley, J.; Barlow, J.; Johns, L.C. Sociodemographic characteristics associated with parenthood amongst patients with a psychotic diagnosis: A cross-sectional study using patient clinical records. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1897–1906. [Google Scholar] [CrossRef]
- Cooklin, A. “Living upside down”: Being a young carer of a parent with mental illness. Adv. Psychiatr. Treat. 2010, 16, 141–146. [Google Scholar] [CrossRef]
- Goldstein, J.M.; Cherkerzian, S.; Tsuang, M.T.; Petryshen, T.L. Sex differences in the genetic risk for schizophrenia: History of the evidence for sex-specific and sex-dependent effects. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2013, 162, 698–710. [Google Scholar] [CrossRef]
- Barajas, A.; Pelaez, T.; González, O.; Usall, J.; Iniesta, R.; Arteaga, M.; Jackson, C.; Baños, I.; Sánchez, B.; Dolz, M.; et al. Predictive capacity of prodromal symptoms in first-episode psychosis of recent onset. Early Interv. Psychiatry 2019, 13, 414–424. [Google Scholar] [CrossRef]
- Schmidt, S.J.; Schultze-Lutter, F.; Schimmelmann, B.G.; Maric, N.P.; Salokangas, R.K.R.; Riecher-Rössler, A.; van der Gaag, M.; Meneghelli, A.; Nordentoft, M.; Marshall, M.; et al. EPA guidance on the early intervention in clinical high risk states of psychoses. Eur. Psychiatry 2015, 30, 388–404. [Google Scholar] [CrossRef]
- Tapias, E.; Coromina, M.; Grases, N.; Ochoa, S. Psychological Treatments with Children of Parents with Mental Illness: A Systematic Review. Child Youth Care Forum 2021, 50, 1107–1130. [Google Scholar] [CrossRef]
- Radley, J.; Barlow, J.; Johns, L.C. The Needs and Experiences of Parents with Psychosis: A Qualitative Interview Study. J. Child Fam. Stud. 2022, 32, 2431–2443. [Google Scholar] [CrossRef]
- Wolpert, M.; Hoffman, J.; Martin, A.; Fagin, L.; Cooklin, A. An exploration of the experience of attending the Kidstime programme for children with parents with enduring mental health issues: Parents’ and young people’s views. Clin. Child Psychol. Psychiatry 2015, 20, 406–418. [Google Scholar] [CrossRef]
- Rosenblum, K.L.; Muzik, M.; Morelen, D.M.; Alfafara, E.A.; Miller, N.M.; Waddell, R.M.; Schuster, M.M.; Ribaudo, J. A Community-based Randomized Controlled Trial of Mom Power Parenting Intervention for Mothers with Interpersonal Trauma Histories and their Young Children. Arch. Women’s Ment. Health 2017, 20, 673. [Google Scholar] [CrossRef]
- Fraser, E.; Pakenham, K.I. Evaluation of a resilience-based intervention for children of parents with mental illness. Aust. N. Z. J. Psychiatry 2008, 42, 1041–1050. [Google Scholar] [CrossRef]
- Steenhuis, L.A.; Pijnenborg GH, M.; van der Stouwe EC, D.; Hartman, C.A.; Aleman, A.; Bartels-Velthuis, A.A.; Nauta, M.H. The Longitudinal Association Between Preadolescent Facial Emotion Identification and Family Factors, and Psychotic Experiences in Adolescence (The TRAILS Study). Child Psychiatry Hum. Dev. 2020, 51, 187. [Google Scholar] [CrossRef]
- Kilford, E.J.; Garrett, E.; Blakemore, S.J. The development of social cognition in adolescence: An integrated perspective. Neurosci. Biobehav. Rev. 2016, 70, 106–120. [Google Scholar] [CrossRef] [PubMed]
- Marston, N.; Stavnes, K.; Van Loon LM, A.; Drost, L.M.; Maybery, D.; Mosek, A.; Nicholson, J.; Solantaus, T.; Reupert, A. A content analysis of Intervention Key Elements and Assessments (IKEA): What’s in the black box in the interventions directed to families where a parent has a mental illness? Child Youth Serv. 2016, 37, 112–128. [Google Scholar] [CrossRef]
- Moritz, S.; Woodward, T.S. Metacognitive Training for Schizophrenia Patients (MCT): A Pilot Study on Feasibility, Treatment Adherence, and Subjective Efficacy. Ger. J. Psychiatry 2007, 41, 207–211. [Google Scholar]
- Penney, D.; Sauvé, G.; Mendelson, D.; Thibaudeau, É.; Moritz, S.; Lepage, M. Immediate and Sustained Outcomes and Moderators Associated With Metacognitive Training for Psychosis: A Systematic Review and Meta-analysis. JAMA Psychiatry 2022, 79, 417. [Google Scholar] [CrossRef]
- Ochoa, S.; López-Carrilero, R.; Barrigón, M.L.; Pousa, E.; Barajas, A.; Lorente-Rovira, E.; González-Higueras, F.; Grasa, E.; Ruiz-Delgado, I.; Cid, J.; et al. Randomized control trial to assess the efficacy of metacognitive training compared with a psycho-educational group in people with a recent-onset psychosis. Psychol. Med. 2017, 47, 1573–1584. [Google Scholar] [CrossRef] [PubMed]
- Salas-Sender, M.; López-Carrilero, R.; Barajas, A.; Lorente-Rovira, E.; Pousa, E.; Barrigón, M.L.; Grasa, E.; Ruiz-Delgado, I.; González-Higueras, F.; Cid, J.; et al. Gender differences in response to metacognitive training in people with first-episode psychosis. J. Consult. Clin. Psychol. 2020, 88, 516–525. [Google Scholar] [CrossRef]
- Chiauzzi, E.; Clayton, A.; Huh-Yoo, J. Videoconferencing-Based Telemental Health: Important Questions for the COVID-19 Era From Clinical and Patient-Centered Perspectives. JMIR Ment. Health 2020, 7, E24021. [Google Scholar] [CrossRef]
- Lupton, D. Young People’s Use of Digital Health Technologies in the Global North: Narrative Review. J. Med. Internet Res. 2021, 23, e18286. [Google Scholar] [CrossRef]
- Santesteban-Echarri, O.; Piskulic, D.; Nyman, R.K.; Addington, J. Telehealth interventions for schizophrenia-spectrum disorders and clinical high-risk for psychosis individuals: A scoping review. J. Telemed. Telecare 2020, 26, 14–20. [Google Scholar] [CrossRef]
- Mendelson, D.; Thibaudeau, E.; Eve Sauvé, G.; Lavigne, K.M.; Bowie, C.R.; Menon, M.; Woodward, T.S.; Lepage, M.; Raucher-Chéné, D. Remote group therapies for cognitive health in schizophrenia-spectrum disorders: Feasible, acceptable, engaging. Schizophr. Res. Cogn. 2022, 28, 100230. [Google Scholar] [CrossRef] [PubMed]
- Riches, S.; Arseneault, L.; Bagher-Niakan, R.; Alsultan, M.; Crush, E.; Fisher, H.L. Protective factors for early psychotic phenomena among children of mothers with psychosis. Front. Psychiatry 2019, 10, 422447. [Google Scholar] [CrossRef] [PubMed]
- Seeman, M.V. Intervention to Prevent Child Custody Loss in Mothers with Schizophrenia. Schizophr. Res. Treat. 2012, 2012, 796763. [Google Scholar] [CrossRef] [PubMed]
- Wingood, G.M.; Diclemente, R.J. The ADAPT-ITT model: A novel method of adapting evidence-based HIV interventions. J. Acquir. Immune Defic. Syndr. 2008, 47, S40–S46. [Google Scholar] [CrossRef] [PubMed]
- Myers, B.; Carney, T.; Browne, F.A.; Wechsberg, W.M. Development of a trauma-informed substance use and sexual risk reduction intervention for young South African women. Patient Prefer. Adherence 2018, 12, 1997–2006. [Google Scholar] [CrossRef] [PubMed]
- Carney, T.; Chimbambo, V.; Johnson, K.; Louw, J.; Myers, B. The adaptation of an evidence-based brief intervention for substance-using adolescents and their caregivers. Psychother. Res. 2020, 30, 728–738. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, C.E.; Wismar, A. A systematic review of community stakeholder involvement during application of the ADAPT-ITT model to adapt trauma interventions for new populations. Psychol. Trauma Theory Res. Pract. Policy 2022, 14, 932–939. [Google Scholar] [CrossRef]
- Polillo, A.; Voineskos, A.N.; Foussias, G.; Kidd, S.A.; Sav, A.; Hawley, S.; Soklaridis, S.; Stergiopoulos, V.; Kozloff, N. Using Digital Tools to Engage Patients with Psychosis and Their Families in Research: Survey Recruitment and Completion in an Early Psychosis Intervention Program. JMIR Ment. Health 2021, 8, e24567. [Google Scholar] [CrossRef]
- Fischer, R.; Scheunemann, J.; Bohlender, A.; Duletzki, P.; Nagel, M.; Moritz, S. ‘You are trying to teach us to think more slowly!’: Adapting Metacognitive Training for the acute care setting—A case report. Clin. Psychol. Psychother. 2022, 29, 1877–1885. [Google Scholar] [CrossRef]
- Ochoa, S.; Usall, J.; Haro, J.M.; Araya, S.; Autonell, J.; Busquets, E.; Gost, A. Comparative study of the needs of patients with schizophrenia by gender. Actas Esp. Psiquiatr. 2001, 29, 165–171. [Google Scholar]
- Seeman, M.V. Relational ethics: When mothers suffer from psychosis. Arch. Women’s Ment. Health 2004, 7, 201–210. [Google Scholar] [CrossRef]
- Radley, J.; Barlow, J.; Johns, L. Mental health professionals’ experiences of working with parents with psychosis and their families: A qualitative study. BMC Health Serv. Res. 2021, 21, 393. [Google Scholar] [CrossRef]
- Abel, K.M.; Bee, P.; Gega, L.; Gellatly, J.; Kolade, A.; Hunter, D.; Callender, C.; Carter, L.-A.; Meacock, R.; Bower, P.; et al. An intervention to improve the quality of life in children of parents with serious mental illness: The Young SMILES feasibility RCT. Health Technol. Assess. 2020, 24, 1–136. [Google Scholar] [CrossRef]
- Moritz, S.; Veckenstedt, R.; Randjbar, S.; Vitzthum, F.; Woodward, T.S. Antipsychotic treatment beyond antipsychotics: Metacognitive intervention for schizophrenia patients improves delusional symptoms. Psychol. Med. 2011, 41, 1823–1832. [Google Scholar] [CrossRef]
- Lin, T.; Heckman, T.G.; Anderson, T. The efficacy of synchronous teletherapy versus in-person therapy: A meta-analysis of randomized clinical trials. Clin. Psychol. Sci. Pract. 2022, 29, 167–178. [Google Scholar] [CrossRef]
- Schmitt, J.C.; Valiente, R.M.; García-Escalera, J.; Arnáez, S.; Espinosa, V.; Sandín, B.; Chorot, P. Prevention of Depression and Anxiety in Subclinical Adolescents: Effects of a Transdiagnostic Internet-Delivered CBT Program. Int. J. Environ. Res. Public Health 2022, 19, 5365. [Google Scholar] [CrossRef]
- Espinosa, V.; Garcia-Escalera, J.; Arnáez, S.; Valiente, R.; Sandin, B.; Schmitt, J.C.; Chorot, P. Administración telemática del Protocolo Unificado para el tratamiento transdiagnóstico de los trastornos emocionales en adolescentes (tUP-A): Un estudio de casos. Acción Psicol. 2022, 19, 149–162. [Google Scholar] [CrossRef]
- Robson, E.; Greenwood, K. Rates and Predictors of Disengagement and Strength of Engagement for People With a First Episode of Psychosis Using Early Intervention Services: A Systematic Review of Predictors and Meta-analysis of Disengagement Rates. Schizophr. Bull. Open 2022, 3, 398–404. [Google Scholar] [CrossRef]
- Lecomte, T.; Abdel-Baki, A.; Francoeur, A.; Cloutier, B.; Leboeuf, A.; Abadie, P.; Villeneuve, M.; Guay, S. Group therapy via videoconferencing for individuals with early psychosis: A pilot study. Early Interv. Psychiatry 2021, 15, 1595–1601. [Google Scholar] [CrossRef] [PubMed]
- Dolman, C.; Jones, I.; Howard, L.M. Pre-conception to parenting: A systematic review and meta-synthesis of the qualitative literature on motherhood for women with severe mental illness. Arch. Women’s Ment. Health 2013, 16, 173–196. [Google Scholar] [CrossRef] [PubMed]
- Tchernegovski, P.; Hine, R.; Reupert, A.E.; Maybery, D.J. Adult mental health clinicians’ perspectives of parents with a mental illness and their children: Single and dual focus approaches. BMC Health Serv. Res. 2018, 18, 611. [Google Scholar] [CrossRef] [PubMed]
| ADAPT-ITT | Method | Changes to Intervention |
|---|---|---|
| Step 1: Assessment | A research team first approached the subject by reviewing existing literature on different topics and based on their clinical and research experience in the field (the research team included different experts in psychosis, gender, adulthood, adolescence, psychological interventions, and metacognition). | |
| Step 2: Decision | Different topical expert consensus groups discussed the findings from Step 1 and selected MCT. They also identified main themes and specified components for inclusion/exclusion from the original MCT The coordinating team developed materials (MCT-F-v1) based on the topical experts’ proposals. | MCT-F-v1 |
| Step 3: Administration | The different stakeholders (patients, relatives, and adolescents) received the first version and gave initial feedback about the acceptance, feasibility, and attractiveness of the material. | MCT-F-v1 |
| Step 4: Production | The feedback from Step 3 was used by the coordinating team to further modify the content and structure to produce version 2. | MCT-F-v2 |
| Step 5: Topical Experts | Topical experts from the consensus groups were asked to evaluate the current adaptation and suggest other necessary modifications. | MCT-F-v2 |
| Step 6: Integration | All findings and feedback were integrated to produce the final version of the adapted intervention. | MCT-F-v3 |
| Step 7: Training | There will be different training for recruiters, facilitators, and assessors to implement the final MCT-F version. | |
| Step 8: Testing | A pilot randomized controlled trial comparing MCT-F with a waiting list control group is being planned. |
| Domain | Description | Examples of Adaptations |
|---|---|---|
| Context | Increase accessibility; enhance feasibility, acceptability, and compliance | Mothers and children will be able to attend sessions from the same place or separately to facilitate attendance and the intimacy of both parties. Group composition: The groups will be composed of 3–4 mothers with psychosis, their adolescent children, and two therapists. Groups will be formed based on the adolescents’ ages (aged 12 to 16 and 16 to 20) to adapt examples and vocabulary and so they feel more comfortable sharing experiences. Group size: A group of 3 to 4 mothers and adolescents is large enough in case of some participant absences cause those attending to feel exposed. It is also manageable for two facilitators. |
| Persons | Engaging non-mental health adolescent children of mothers with psychosis; assess the tolerability and effectiveness of the MCT-F in mothers and their adolescent children. Promoting the therapist–patient relationship | Application of MCT-F to mothers with psychosis together with their adolescent children in a peer group setting. Therapists will also provide local community references for the mother’s participation. |
| Goal | Clarify and extend goals; improving the children’s knowledge of the disease. | Module 1: Adding content to help adolescents to understand the symptoms of their mother’s disease. Linking MCT-F to healthy populations (adolescents). Describing MCT-F as a training program aiming to increase cognitive flexibility, modify metacognitive beliefs, and decrease dysfunctional coping strategies. |
| Language | Ensuring translation is harmonious with adolescents’ language; replacement of technical terms with colloquialisms. Ensuring Spanish translation is gender inclusive. | Module 2: “Attribution = to infer causes about events” is replaced by “Attribution = to give an explanation or look for a cause of a situation”; “Megalomaniac” is replaced by “thinking we are more important than others”. Module 9: A Spanish metaphor is included to explain the cognitive distortion of overgeneralizing: “I killed a dog, then they called me dog killer”; “Depressive attributional style” is replaced by “depressive thinking”; “Comprehensive assessment” is replaced by “take everything into account”. All modules: use both sexes in verbs, determinants, pronouns, etc. |
| Concept | Ensuring concepts of mentally ill health are understood. | Module 2: The content dedicated to addressing the symptoms of “hearing voices” includes examples like impulsion phobias which may be more familiar to adolescent children and make them easier to understand (e.g., “Thirty-nine and forty-three percent of males and females, respectively, had had the intrusive thought of jumping from a high place.”). |
| Method | Promoting adolescent engagement; adapting the intervention structure. | All modules: Worksheets were not included in this first adaptation. The number of modules from the 10-module version of MCT (eight modules and two additional modules) was reduced to 9. The self-esteem additional module is added to the self-esteem and mood module. The content of the relapse prevention worksheet is added to the module dealing with self-stigmatization. |
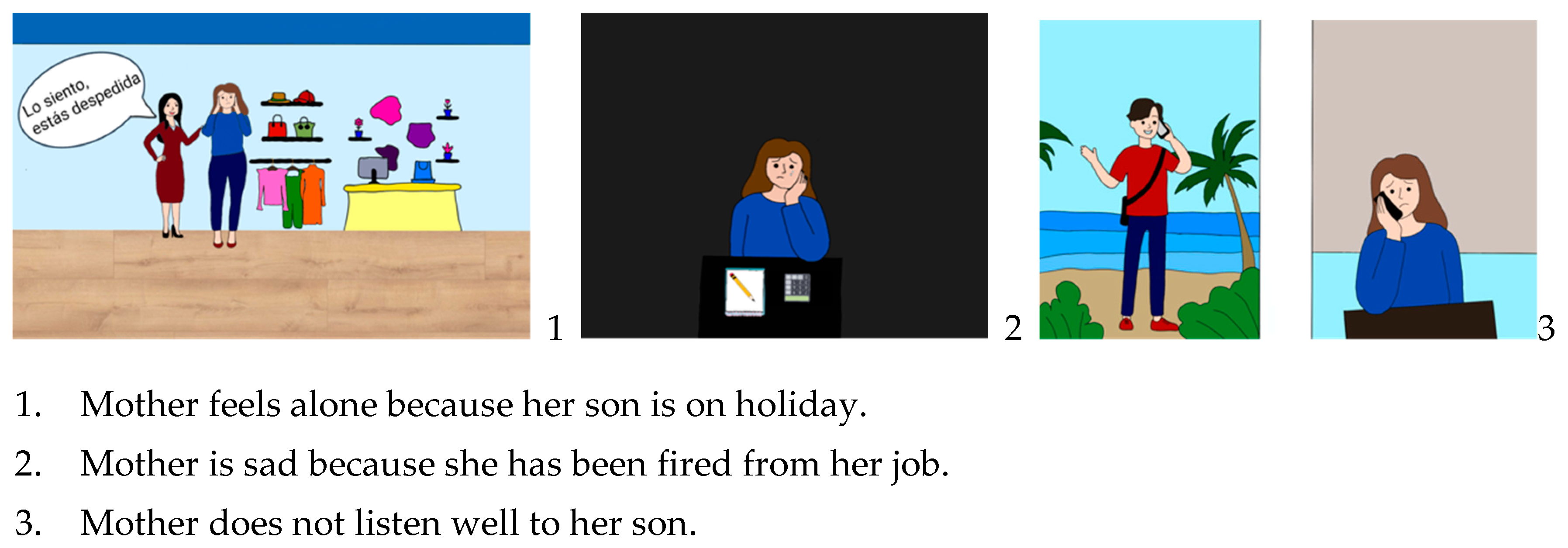
| Metaphors and content | Promoting engagement. Ensuring content is relevant and acceptable for adolescent age groups using current examples. Including examples of relevant stressors for mothers with psychosis, adolescents, and the mother–child relationship. | An introductory and psychoeducational module is added. All modules: Photos with young people (laughing, partying, using the cell phone, etc.) are included. Module 3: Jumping to conclusions in social media (e.g., “Seeing that a follower on Instagram or TikTok has uploaded the same photo or video as you”) or in the COVID-19 pandemic context; challenging false beliefs regarding cannabis consumption. Module 6: Next to the sentence “How can I memorize things better?” is an image of a brain exercising. Module 8: The picture of a screaming mouth and a frightened boy representing the delusions is deleted. Module 9: Added a picture of a hamster rolling on a wheel to represent rumination. Module 10. Added teens’ icons who opened up about their mental health disorders; added data on the prevalence of mental disorders in females and adolescents due to COVID-19. Module 2: The following example is added: Ana’s mother has had a relapse and has been admitted. Ana’s thoughts: the relapse was caused because my grades have gotten worse. Another explanation: Ana’s mother had stopped taking her medication. Moreover, she had had an argument at work and was afraid of losing her job. Module 4: Figure 1 shows an example of new material added to address the bias against disconformity evidence through a possible common situation in the mother–child relationship. Module 8: The following example is added: “Example: Judith’s daughter’s volleyball coach proposes to Judith that her daughter competes this weekend. Background: She is convinced that the coach wants to take away her role as a mother and push them apart. This weekend is Judith’s birthday. But: The coach wants the best for her daughter. Besides, she’s keeping Judith in mind”. Module 9: Exercise including “What do you like about your mother? What is your son/daughter good at?”; Add examples of common cognitive bias among adolescents or in the mother–child relationship (e.g., “I shouted at my son/daughter the other day so I’m a bad mother”). |
| Variable | Patients | Patients’ Relatives | Adolescents | Total | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Do you think the vocabulary of the modules is comprehensive? | 8.00 | 7.50 (0.71) | 9.00 | 8.33 (0.82) | |
| Were you able to understand the explanations, exercises, and examples? | 9.50 (0.71) | 7.00 (0.00) | 9.67 (0.58) | 8.67 (1.37) | |
| How easy would it be for you to incorporate an online program of 10 sessions a week at a frequency of 1 h in the afternoon into your routine? | 7.50 (2.12) | 8.00 (0.00) | 9.00 (1.00) | 8.17 (1.33) | |
| Do you think the online format is appropriate for this type of training? | 9.00 (1.41) | 6.00 (0.00) | 7.33 (2.10) | 7.00 (1.60) | |
| Would you recommend the training to others? | 7.00 (2.83) | 9.50 (0.71) | 9.67 (0.58) | 8.83 (1.94) | |
| How much did you enjoy the training and did you find it attractive? | 9.00 (1.41) | 9.00 (0.00) | 8.00 (2.00) | 8.33 (1.37) | |
| In general, did you find the training helpful (for you)? | 7.50 (3.53) | 9.00 (0.00) | 9.67 (0.58) | 8.67 (1.86) | |
| How useful could this training be for the mother–child relationship in your experience? | 5.00 (7.07) | 9.00 (1.41) | 9.33 (1.15) | 7.67 (3.88) | |
| M1 | usefulness | 9.00 (1.41) | 8.50 (2.12) | 9.50 (0.71) | 8.80 (1.30) |
| enjoyment | 9.00 (1.41) | 8.50 (2.12) | 8.67 (0.58) | 8.50 (1.05) | |
| M2 | usefulness | 9.00 (1.41) | 9.00 (1.41) | 9.00 (1.00) | 8.83 (0.98) |
| enjoyment | 8.50 (2.12) | 9.00 (1.41) | 9.00 (1.00) | 8.67 (1.21) | |
| M3 | usefulness | 8.50 (2.12) | 8.50 (2,12) | 9,00 (1.00) | 8.50 (1.38) |
| enjoyment | 8.50 (2.12) | 8.00 (2.83) | 9.00 (1.00) | 8.33 (1.63) | |
| M4 | usefulness | 8.50 (2.12) | 9.50 (0.71) | 9.33 (0.58) | 9.00 (1.09) |
| enjoyment | 8.00 (2.83) | 9.50 (0.71) | 9.00 (1.00) | 8.67 (1.50) | |
| M5 | usefulness | 9.00 (1.41) | 9.50 (0.71) | 9.00 (1.00) | 9.00 (0.89) |
| enjoyment | 9.00 (1.41) | 8.50 (2.12) | 8.33 (0.58) | 8.33 (1.03) | |
| M6 | usefulness | 10.00 (0.00) | 8.50 (2.12) | 9.00 (0.58) | 9.33 (1.21) |
| enjoyment | 10.00 (0.00) | 7.50 (2.12) | 9.00 (1.73) | 8.67 (1.75) | |
| M7 | usefulness | 8.50 (2.12) | 8.50 (2.12) | 9.00 (1.00) | 8.50 (1.38) |
| enjoyment | 8.50 (2.12) | 6.50 (0.71) | 8.00 (1.73) | 7.33 (1.37) | |
| M8 | usefulness | 7.50 (3.53) | 8.00 (2.83) | 8.33 (1.53) | 7.67 (2.06) |
| enjoyment | 9.00 (1.41) | 6.50 (0.71) | 7.00 (1.73) | 7.00 (1.26) | |
| M9 | usefulness | 9.50 (0.71) | 9.00 (1.41) | 9.33 (1.15) | 9.17 (0.98) |
| enjoyment | 7.50 (3.53) | 8.00 (1.41) | 8.67 (0.58) | 7.83 (1.60) | |
| M10 | usefulness | 7.50 (0.71) | 9.50 (0.71) | 8.67 (1.53) | 8.83 (1.17) |
| enjoyment | 8.50 (2.12) | 8.00 (0.00) | 7.67 (1.15) | 8.17 (1.17) | |
| Module | Aim | Examples of Modified Text and New Activities |
|---|---|---|
| 1 | Promote acceptability and reduce possible defenses and fears of participating mothers about talking to their children about psychosis. | The description of psychosis and symptoms is moved from the start to the middle of the presentation. Some content from relapse prevention (early warning symptoms) is brought forward in this first module. Therapists use the vocabulary proposed by the group to refer to crises or disease outbreaks. |
| 2 | Approach symptoms such as hearing voices very carefully and avoid new concerns. | A photo of an aggressive mouth representing “voices” is replaced by an image of an adolescent girl covering her ears. |
| 3 | Enhance adherence and, consequently, increase its acceptability and efficacy. | Task Set 1 examples are narrowed down by selecting the most attractive ones. |
| 4 | Refine the intervention materials to enhance their appeal and comprehensibility. | The text and content of some comics are modified. |
| 5 | Refine the intervention materials to enhance their appeal and comprehensibility. | Some comics are redesigned and colored. |
| 6 | Address relevant stressors for participants. | Add situations related to academic issues (e.g., a picture of a classroom, “meeting with your child’s teacher” as an example of an event to work on). |
| 7 | Ensure content is easily understandable to participants. | Add numbering to comic book bullets. |
| 8 | Simplify the language used, reducing the amount of text and slides, and adding more visuals. | Task Set 1 examples are narrowed down by selecting the most attractive ones. “This type of decision-making can easily lead to errors, compared to a type of decision-making that involves careful consideration of all available information” is replaced by “+information, +certain, -information, + mistakes”. |
| 9 | Increase acceptability and adherence. | The content order is reversed. The first part addresses depression and the second addresses self-esteem to finish the session on a positive note. |
| 10 | Refine the intervention materials to enhance their appeal and comprehensibility. | Text is converted into bullet points. An image of a girl looking at herself in the mirror, thinking “I am not normal”, is added to the self-stigmatization slide. |
| M (DT) | |
|---|---|
| Do you think the vocabulary of the modules is understandable for both adult and adolescent populations? | 8.86 (1.03) |
| Are the explanations, exercises, and examples comprehensive? | 9.00 (0.68) |
| How feasible would it be for a patient and her adolescent to incorporate an online program of 10 weekly 1-h afternoon sessions into their routine? | 7.07 (1.38) |
| Do you think the online format is appropriate for this type of training? | 7.43 (2.76) |
| Would you recommend the training to patients who meet the criteria? | 9.36 (1.01) |
| In general, do you think training is helpful for women with psychosis who are mothers? | 9.36 (0.74) |
| In general, do you think training is useful for adolescent sons and daughters of women with psychosis? | 8.86 (0.95) |
| In general, can the training be useful for the relationship between mother and adolescent relationship? | 8.86 (0.53) |
| As a professional, how feasible would it be for you to conduct training with this format considering frequency, duration, and number of sessions (10 weekly sessions of 1 h duration)? | 8.36 (1.28) |
| As a professional, how comfortable would you feel doing this training? | 8.64 (1.34) |
| Module 1 | 9.21 (0.89) |
| Module 2 | 8.43 (1.55) |
| Module 3 | 8.64 (1.34) |
| Module 4 | 8.64 (1.21) |
| Module 5 | 8.78 (1.05) |
| Module 6 | 9.00 (0.88) |
| Module 7 | 8.64 (1.21) |
| Module 8 | 8.71 (0.82) |
| Module 9 | 9.00 (1.11) |
| Module 10 | 9.14 (0.95) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Espinosa, V.; Arin-González, P.; Jiménez-Lafuente, A.; Pardo, N.; López-Carrilero, R.; Birulés, I.; Barajas, A.; Pélaez, T.; Díaz-Cutraro, L.; Verdaguer-Rodríguez, M.; et al. Family Metacognitive Training (MCT-F): Adapting MCT to Mothers with Psychosis and Their Adolescent Children. Behav. Sci. 2024, 14, 97. https://doi.org/10.3390/bs14020097
Espinosa V, Arin-González P, Jiménez-Lafuente A, Pardo N, López-Carrilero R, Birulés I, Barajas A, Pélaez T, Díaz-Cutraro L, Verdaguer-Rodríguez M, et al. Family Metacognitive Training (MCT-F): Adapting MCT to Mothers with Psychosis and Their Adolescent Children. Behavioral Sciences. 2024; 14(2):97. https://doi.org/10.3390/bs14020097
Chicago/Turabian StyleEspinosa, Victoria, Paula Arin-González, Alba Jiménez-Lafuente, Nerea Pardo, Raquel López-Carrilero, Irene Birulés, Ana Barajas, Trinidad Pélaez, Luciana Díaz-Cutraro, Marina Verdaguer-Rodríguez, and et al. 2024. "Family Metacognitive Training (MCT-F): Adapting MCT to Mothers with Psychosis and Their Adolescent Children" Behavioral Sciences 14, no. 2: 97. https://doi.org/10.3390/bs14020097
APA StyleEspinosa, V., Arin-González, P., Jiménez-Lafuente, A., Pardo, N., López-Carrilero, R., Birulés, I., Barajas, A., Pélaez, T., Díaz-Cutraro, L., Verdaguer-Rodríguez, M., Gutiérrez-Zotes, A., Palma-Sevillano, C., Varela-Casals, P., Salas-Sender, M., Aznar, A., Ayesa-Arriola, R., Pousa, E., Canal-Rivero, M., Garrido-Torres, N., ... Ochoa, S. (2024). Family Metacognitive Training (MCT-F): Adapting MCT to Mothers with Psychosis and Their Adolescent Children. Behavioral Sciences, 14(2), 97. https://doi.org/10.3390/bs14020097









