Perceived Stressful Life Events and Suicide Risk in Adolescence: The Mediating Role of Perceived Family Functioning
Abstract
1. Introduction
2. Methods
2.1. Sample
2.2. Instruments
2.3. Data Analysis
3. Results
3.1. Sample Features
3.2. Correlation and Regression Analysis
- Comparing Model 1 (Adjusted R-square = 0.14.2, p < 0.001) with Model 2 (Adjusted R-square = 0.178, p < 0.001) showed that SLE impact perception makes a significant contribution to the model.
- Comparing Model 1 (Adjusted R-square = 0.136, p < 0.001) with Model 3 (Adjusted R-square = 0.216, p < 0.001) showed that family functioning makes a significant contribution to the model.
- Comparing Model 2 (Adjusted R-square = 0.178, p < 0.001) with Model 4 (Adjusted R-square = 0.24, p < 0.001) showed that family functioning and SLE impact perception taken together make a significant contribution to the model in which SLE impact perception is taken alone.
- Comparing Model 3 (Adjusted R-square = 0.216, p < 0.001) with Model 4 (Adjusted R-square = 0.24, p < 0.001) showed that family functioning and SLE impact perception taken together make a significant contribution to the model in which family functioning is taken alone.
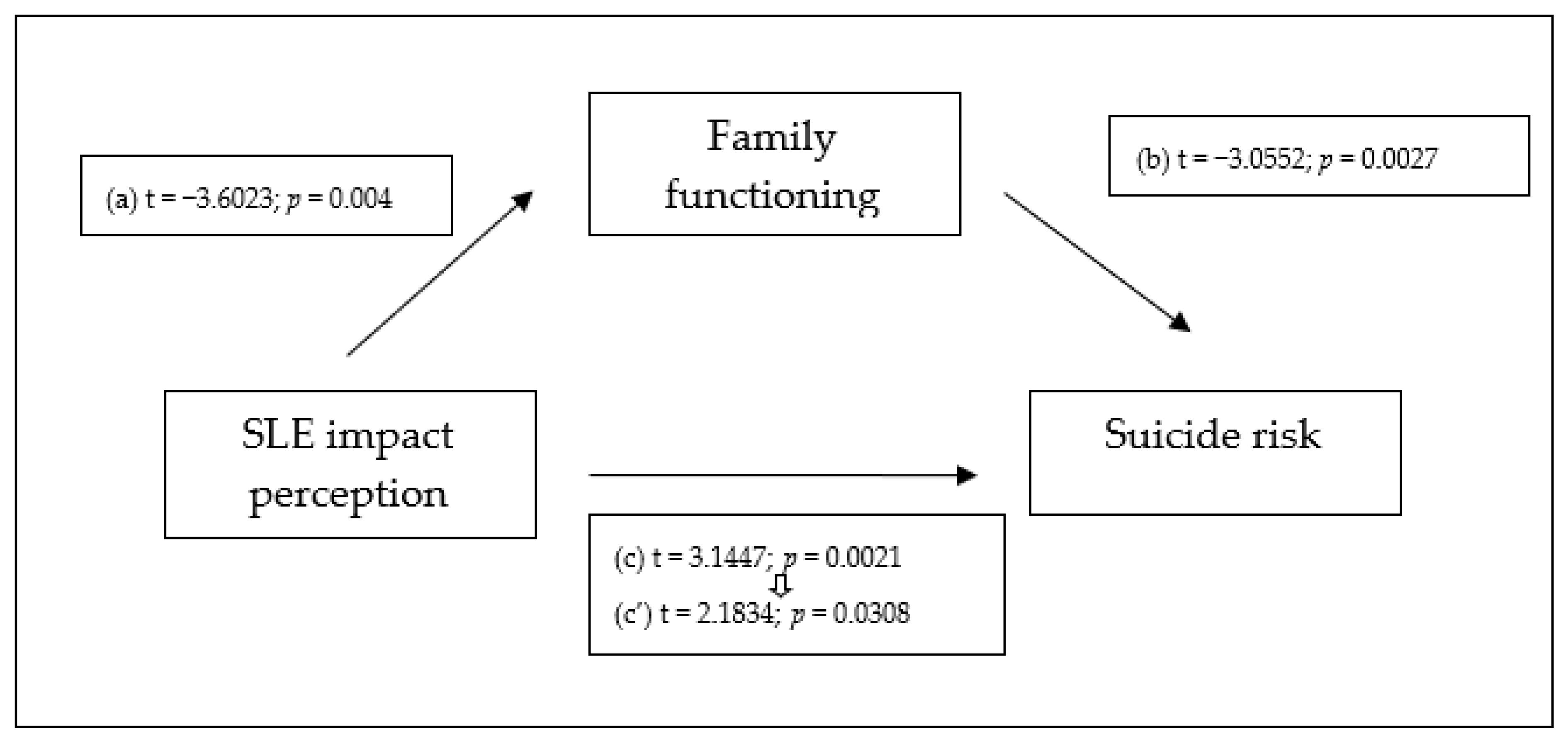
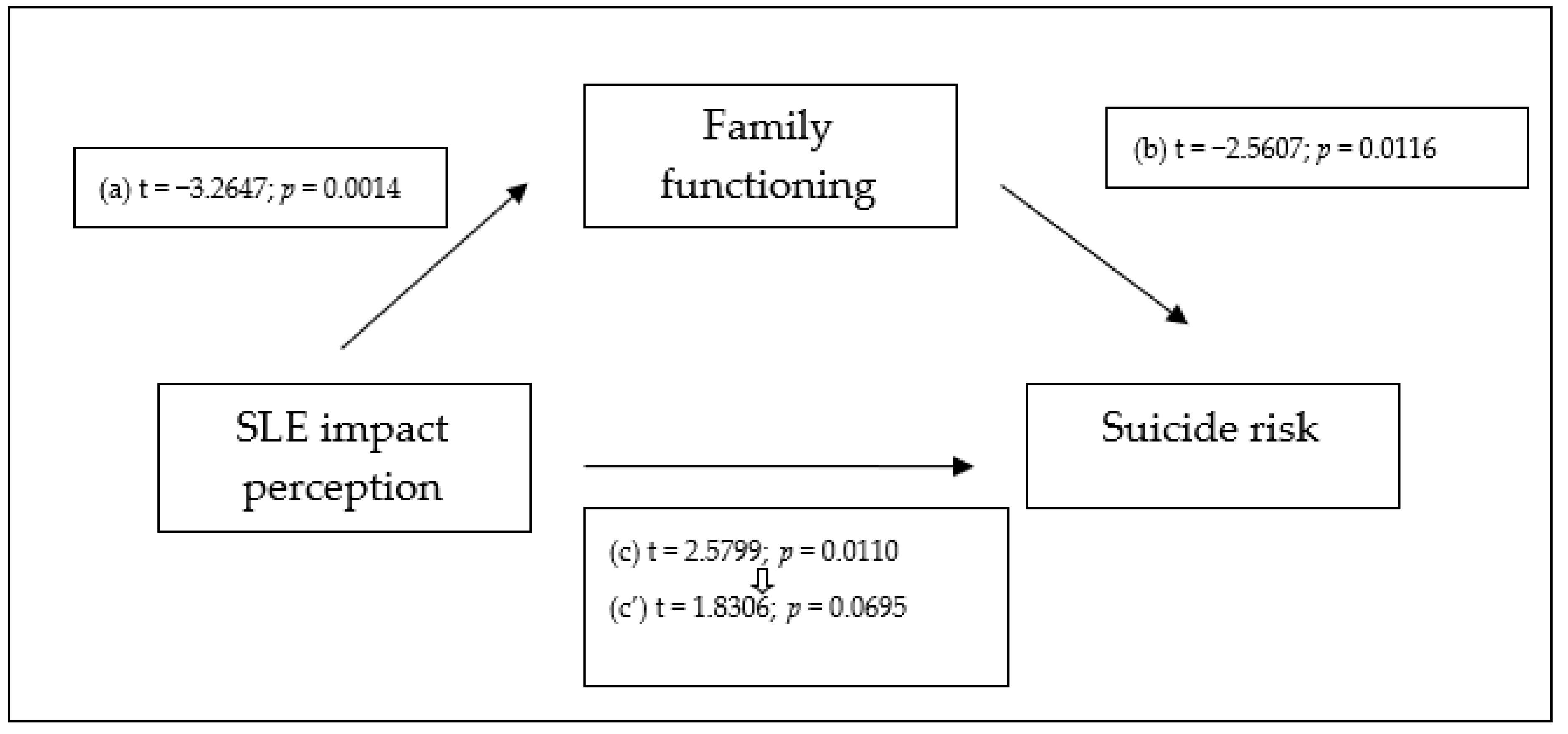
3.3. Mediation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al-Halabí, S.; Fonseca-Pedrero, E. Suicidal Behavior Prevention: The Time to Act is Now. Clin. Health 2021, 32, 89–92. [Google Scholar] [CrossRef]
- WHO Suicide. Available online: https://www.who.int/news-room/fact-sheets/detail/suicide (accessed on 20 November 2023).
- Fonseca-Pedrero, E.; Pérez de Albéniz, A.; Fonseca-Pedrero, E.; Pérez de Albéniz, A. Evaluación de La Conducta Suicida En Adolescentes: A Propósito de La Escala Paykel de Suicidio. Papeles Psicólogo 2020, 41, 106–115. [Google Scholar] [CrossRef]
- WHO Preventing Suicide: A Global Imperative. Available online: https://www.who.int/publications/i/item/9789241564779 (accessed on 6 November 2023).
- Pedreira, J.L. Conductas suicidas en la adolescencia: Una guía práctica para la intervención y la prevención. Rev. Psicopatología Psicol. Clínica 2019, 24, 217–237. [Google Scholar] [CrossRef]
- American Psychiatry Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR). Available online: https://www.psychiatry.org:443/psychiatrists/practice/dsm (accessed on 13 December 2023).
- Vázquez López, P.; Armero Pedreira, P.; Martínez Sánchez, L.; Garcia Cruz, J.M.; Bonet Luna, C.; Notario Herrero, F.; Sánchez Vázquez, A.R.; Rodríguez Hernández, P.J.; Díez Suárez, A. Autolesiones y conducta suicida en niños y adolescentes. Lo que la pandemia nos ha desvelado. An. Pediatría 2023, 98, 204–212. [Google Scholar] [CrossRef]
- Espandian, A.; González, M.; Reijas, T.; Florez, G.; Ferrer, E.; Saiz, P.A.; Salgado-Barreira, A.; González, A.; Brenlla, J.; Docasar, L.; et al. Factores predictores de riesgo de repetición de intento de suicidio en una muestra de pacientes ambulatorios. Rev. Psiquiatr. Salud Ment. 2020, 13, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Sarti, P.; Colliva, C.; Varrasi, S.; Guerrera, C.S.; Platania, G.A.; Boccaccio, F.M.; Castellano, S.; Pirrone, C.; Pani, L.; Tascedda, F.; et al. A Network Study to Differentiate Suicide Attempt Risk Profiles in Male and Female Patients with Major Depressive Disorder. Clin. Psychol. Psychother. 2023, 1–14. [Google Scholar] [CrossRef]
- Carballo, J.J.; Figueroa, A.; Oquendo, M.A.; Soutullo, C. Suicidio En Niños y Adolescentes: Ideas, Intentos y Suicidio Consumado. Prevención, Evaluación y Tratamiento. In Manual de Psiquiatría infantil y del Adolescente; Editorial Panamericana: San Juan, PR, USA, 2012; pp. 395–410. [Google Scholar]
- Stein, D.J.; Chiu, W.T.; Hwang, I.; Kessler, R.C.; Sampson, N.; Alonso, J.; Borges, G.; Bromet, E.; Bruffaerts, R.; de Girolamo, G.; et al. Cross-National Analysis of the Associations between Traumatic Events and Suicidal Behavior: Findings from the WHO World Mental Health Surveys. PLoS ONE 2010, 5, e10574. [Google Scholar] [CrossRef]
- Carballo, J.J.; Llorente, C.; Kehrmann, L.; Flamarique, I.; Zuddas, A.; Purper-Ouakil, D.; Hoekstra, P.J.; Coghill, D.; Schulze, U.M.E.; Dittmann, R.W.; et al. Psychosocial Risk Factors for Suicidality in Children and Adolescents. Eur. Child Adolesc. Psychiatry 2020, 29, 759–776. [Google Scholar] [CrossRef]
- Fjeldsted, R.; Teasdale, T.W.; Bach, B. Childhood Trauma, Stressful Life Events, and Suicidality in Danish Psychiatric Outpatients. Nord. J. Psychiatry 2020, 74, 280–286. [Google Scholar] [CrossRef]
- Brodsky, B.S.; Stanley, B. Adverse Childhood Experiences and Suicidal Behavior. Psychiatr. Clin. N. Am. 2008, 31, 223–235. [Google Scholar] [CrossRef]
- Dube, S.R.; Anda, R.F.; Felitti, V.J.; Chapman, D.P.; Williamson, D.F.; Giles, W.H. Childhood Abuse, Household Dysfunction, and the Risk of Attempted Suicide Throughout the Life Span Findings from the Adverse Childhood Experiences Study. JAMA 2001, 286, 3089–3096. [Google Scholar] [CrossRef] [PubMed]
- Harris, E.C.; Barraclough, B. Suicide as an Outcome for Mental Disorders. A Meta-Analysis. Br. J. Psychiatry J. Ment. Sci. 1997, 170, 205–228. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Borges, G.; Bromet, E.J.; Alonso, J.; Angermeyer, M.; Beautrais, A.; Bruffaerts, R.; Chiu, W.T.; de Girolamo, G.; Gluzman, S.; et al. Cross-National Prevalence and Risk Factors for Suicidal Ideation, Plans and Attempts. Br. J. Psychiatry 2008, 192, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Malone, K.M.; Oquendo, M.A.; Haas, G.L.; Ellis, S.P.; Li, S.; Mann, J.J. Protective Factors against Suicidal Acts in Major Depression: Reasons for Living. Am. J. Psychiatry 2000, 157, 1084–1088. [Google Scholar] [CrossRef] [PubMed]
- Orozco, R.; Benjet, C.; Borges, G.; Moneta Arce, M.F.; Fregoso Ito, D.; Fleiz, C.; Villatoro, J.A. Association between Attempted Suicide and Academic Performance Indicators among Middle and High School Students in Mexico: Results from a National Survey. Child Adolesc. Psychiatry Ment. Health 2018, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Szlyk, H.S. Suicidal Ideation among Youths at Risk of School Dropout: Impact of Student Demographics, Stressors, and Academic Self-Concept. Health Soc. Work 2020, 45, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Fonseca-Pedrero, E.; Al-Halabí, S.; Pérez-Albéniz, A.; Debbané, M. Risk and Protective Factors in Adolescent Suicidal Behaviour: A Network Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1784. [Google Scholar] [CrossRef]
- De Luca, S.; DiCorcia, D. Suicide Risk among Adolescents Involved in the Justice System: Risk and Suggestions for Prevention. In Serving the Stigmatized: Working within the Incarcerated Environment; Oxford University Press: New York, NY, USA, 2018; pp. 17–40. ISBN 978-0-19-067875-3. [Google Scholar]
- Meza, J.I.; Snyder, S.; Shanholtz, C. Equitable Suicide Prevention for Youth Impacted by the Juvenile Legal System. Front. Psychiatry 2022, 13, 994514. [Google Scholar] [CrossRef]
- Teplin, L.A.; Stokes, M.L.; McCoy, K.P.; Abram, K.M.; Byck, G.R. Suicidal Ideation and Behavior in Youth in the Juvenile Justice System: A Review of the Literature. J. Correct. Health Care Off. J. Natl. Comm. Correct. Health Care 2015, 21, 222–242. [Google Scholar] [CrossRef]
- Balazs, J.; Miklosi, M.; Halasz, J.; Horváth, L.O.; Szentiványi, D.; Vida, P. Suicidal Risk, Psychopathology, and Quality of Life in a Clinical Population of Adolescents. Front. Psychiatry 2018, 9, 17. [Google Scholar] [CrossRef]
- Li, X.; Phillips, M.R.; Zhang, Y.; Xu, D.; Yang, G. Risk Factors for Suicide in China’s Youth: A Case-Control Study. Psychol. Med. 2008, 38, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Zhou, Y.; Luo, D.; Yan, S.; Liu, M.; Wang, M.; Li, X.; Yang, B.X.; Li, Y.; Liu, L.Z. Association of Family Function and Suicide Risk in Teenagers with a History of Self-Harm Behaviors: Mediating Role of Subjective Wellbeing and Depression. Front. Public Health 2023, 11, 1164999. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Sánchez, F.A.; Brambila-Tapia, A.J.L.; Cárdenas-Fujita, L.S.; Toledo-Lozano, C.G.; Samudio-Cruz, M.A.; Gómez-Díaz, B.; García, S.; Rodríguez-Arellano, M.E.; Zamora-González, E.O.; López-Hernández, L.B. Family Functioning and Suicide Attempts in Mexican Adolescents. Behav. Sci. 2023, 13, 120. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Hu, Y.-Q.; Zeng, Z.-H.; Liu, S.-J.; Wu, T.; Zhang, G.-H. The Relationship of Family Functioning and Suicidal Ideation among Adolescents: The Mediating Role of Defeat and the Moderating Role of Meaning in Life. Int. J. Environ. Res. Public Health 2022, 19, 15895. [Google Scholar] [CrossRef] [PubMed]
- Sandler, I.N.; Tein, J.Y.; West, S.G. Coping, Stress, and the Psychological Symptoms of Children of Divorce: A Cross-Sectional and Longitudinal Study. Child Dev. 1994, 65, 1744–1763. [Google Scholar] [CrossRef] [PubMed]
- Borowsky, I.W.; Ireland, M.; Resnick, M.D. Adolescent Suicide Attempts: Risks and Protectors. Pediatrics 2001, 107, 485–493. [Google Scholar] [CrossRef]
- Gould, M.S.; Greenberg, T.; Velting, D.M.; Shaffer, D. Youth Suicide Risk and Preventive Interventions: A Review of the Past 10 Years. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 386–405. [Google Scholar] [CrossRef]
- Guibert Reyes, W.; Del Cueto de Inastrilla, E.R. Factores Psicosociales de Riesgo de La Conducta Suicida. Rev. Cuba. Med. Gen. Integral 2003, 19, 123–125. [Google Scholar]
- Pelkonen, M.; Marttunen, M. Child and Adolescent Suicide: Epidemiology, Risk Factors, and Approaches to Prevention. Paediatr. Drugs 2003, 5, 243–265. [Google Scholar] [CrossRef]
- Salirrosas-Alegría, C.; Saavedra-Castillo, J. Percepción de Algunos Estilos de Crianza y El Episodio Depresivo En El Adulto. Rev. Neuro-Psiquiatr. 2014, 77, 160–167. [Google Scholar] [CrossRef]
- Luthar, S.S.; Zelazo, L.B. Research Onresilience: An Integrative Review. Resil. Vulnerability Adapt. Context Child. Advers. 2003, 2, 510–549. [Google Scholar]
- Franklin, J.C.; Ribeiro, J.D.; Fox, K.R.; Bentley, K.H.; Kleiman, E.M.; Huang, X.; Musacchio, K.M.; Jaroszewski, A.C.; Chang, B.P.; Nock, M.K. Risk Factors for Suicidal Thoughts and Behaviors: A Meta-Analysis of 50 Years of Research. Psychol. Bull. 2017, 143, 187–232. [Google Scholar] [CrossRef] [PubMed]
- Caro-Canizares, I.; De Neira, M.D.; Buratti, A.F.; Segura-Frontelo, A.; Baca-Garcia, E.; Carballo, J.J. Stability and Persistence of the Dysregulation Profile in a Followup Study in a Clinical Sample of Children and Adolescents. Adolesc. Psychiatry 2018, 7, 170–178. [Google Scholar] [CrossRef]
- Caro-Cañizares, I.; Vila, M.M.; Durán Pacheco, J.I.; Carballo, J.J. Interpersonal Theory of Suicide and Stressful Life Events in a Clinical Sample of Adolescents in Spain. Early Interv. Psychiatry 2023, 1–9. [Google Scholar] [CrossRef] [PubMed]
- García-Nieto, R.; Blasco-Fontecilla, H.; Paz Yepes, M.; Baca-García, E. Traducción y validación de la Self-Injurious Thoughts and Behaviors Interview en población española con conducta suicida. Rev. Psiquiatr. Salud Ment. 2013, 6, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Nock, M.K.; Holmberg, E.B.; Photos, V.I.; Michel, B.D. Self-Injurious Thoughts and Behaviors Interview: Development, Reliability, and Validity in an Adolescent Sample. Psychol. Assess. 2007, 19, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Oliva Delgado, A.; Jiménez Morago, J.M.; Parra Jiménez, A.; Sánchez-Queija, I. Acontecimientos Vitales Estresantes, Resiliencia y Ajuste Adolescente. Rev. Psicopatología Psicol. Clínica 2008, 13, 53–62. [Google Scholar] [CrossRef]
- Smilkstein, G. The Family APGAR: A Proposal for a Family Function Test and Its Use by Physicians. J. Fam. Pract. 1978, 6, 1231–1239. [Google Scholar]
- Bellón Saameño, J.A.; Delgado Sánchez, A.; Luna del Castillo, J.d.D.; Lardelli Claret, P. Validez y fiabilidad del cuestionario de función familiar Apgar-familiar. Aten. Primaria 1996, 18, 289–296. [Google Scholar]
- Baron, R.M.; Kenny, D.A. The Moderator-Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Glassman, L.H.; Weierich, M.R.; Hooley, J.M.; Deliberto, T.L.; Nock, M.K. Child Maltreatment, Non-Suicidal Self-Injury, and the Mediating Role of Self-Criticism. Behav. Res. Ther. 2007, 45, 2483–2490. [Google Scholar] [CrossRef] [PubMed]
- Preacher, K.J.; Hayes, A.F. SPSS and SAS Procedures for Estimating Indirect Effects in Simple Mediation Models. Behav. Res. Methods Instrum. Comput. J. Psychon. Soc. Inc 2004, 36, 717–731. [Google Scholar] [CrossRef] [PubMed]
- Holmbeck, G.N. Post-Hoc Probing of Significant Moderational and Mediational Effects in Studies of Pediatric Populations. J. Pediatr. Psychol. 2002, 27, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Fonseca-Pedrero, E.; Inchausti, F.; Pérez-Gutiérrez, L.; Aritio Solana, R.; Ortuño-Sierra, J.; Sánchez-García, M. a Á.; Lucas-Molina, B.; Domínguez, C.; Foncea, D.; Espinosa, V.; et al. Suicidal Ideation in a Community-Derived Sample of Spanish Adolescents. Rev. Psiquiatr. Salud Ment. Engl. Ed. 2018, 11, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Bedoya Cardona, E.Y.; Montaño Villalba, L.E.; Bedoya Cardona, E.Y.; Montaño Villalba, L.E. Suicidio y Trastorno Mental. CES Psicol. 2016, 9, 179–201. [Google Scholar] [CrossRef]
- Park, S.; Kim, C.Y.; Hong, J.P. Unnatural Causes of Death and Suicide Among Former Adolescent Psychiatric Patients. J. Adolesc. Health 2013, 52, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Díaz de Neira, M.; García-Nieto, R.; de León-Martinez, V.; Pérez Fominaya, M.; Baca-García, E.; Carballo, J.J. Prevalencia y funciones de los pensamientos y conductas autoagresivas en una muestra de adolescentes evaluados en consultas externas de salud mental. Rev. Psiquiatr. Salud Ment.—J. Psychiatry Ment. Health 2015, 8, 137–145. [Google Scholar] [CrossRef]
- Brangwin, E.; Zhao, Z.; Shramko, M.; Toomey, R.B.; Syvertsen, A.K. The Association Between Family Physical Abuse and Suicide Attempts Among Gender Minority Adolescents: A Comparison Study. LGBT Health 2023, 10, 99–108. [Google Scholar] [CrossRef]
- Faravelli, C.; Catena, M.; Scarpato, A.; Ricca, V. Epidemiology of Life Events: Life Events and Psychiatric Disorders in the Sesto Fiorentino Study. Psychother. Psychosom. 2007, 76, 361–368. [Google Scholar] [CrossRef]
- Fergusson, D.M.; Woodward, L.J.; Horwood, L.J. Risk Factors and Life Processes Associated with the Onset of Suicidal Behaviour during Adolescence and Early Adulthood. Psychol. Med. 2000, 30, 23–39. [Google Scholar] [CrossRef]
- Danese, A.; Widom, C.S. Associations Between Objective and Subjective Experiences of Childhood Maltreatment and the Course of Emotional Disorders in Adulthood. JAMA Psychiatry 2023, 80, 1009. [Google Scholar] [CrossRef] [PubMed]
- Shilton, T.; Hertz-Palmor, N.; Matalon, N.; Shani, S.; Dekel, I.; Gothelf, D.; Barzilay, R. Contribution of Risk and Resilience Factors to Suicidality among Mental Health-Help-Seeking Adolescent Outpatients: A Cross-Sectional Study. J. Clin. Med. 2023, 12, 1974. [Google Scholar] [CrossRef] [PubMed]
- Gijzen, M.W.M.; Rasing, S.P.A.; Creemers, D.H.M.; Smit, F.; Engels, R.C.M.E.; De Beurs, D. Suicide Ideation as a Symptom of Adolescent Depression. a Network Analysis. J. Affect. Disord. 2021, 278, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Joseph, J.G.; El-Mohandes, A.A.E.; Kiely, M.; El-Khorazaty, M.N.; Gantz, M.G.; Johnson, A.A.; Katz, K.S.; Blake, S.M.; Rossi, M.W.; Subramanian, S. Reducing Psychosocial and Behavioral Pregnancy Risk Factors: Results of a Randomized Clinical Trial among High-Risk Pregnant African American Women. Am. J. Public Health 2009, 99, 1053–1061. [Google Scholar] [CrossRef]
- Rodríguez-Blanco, L.; Carballo-Belloso, J.J.; de León, S.; Baca-García, E. A Longitudinal Study of Adolescents Engaged in Non-Suicidal Self Injury (NSSI): Clinical Follow-up from Adolescence to Young Adulthood. Psychiatry Res. 2021, 297, 113711. [Google Scholar] [CrossRef]
- Bowlby, J.; Ainsworth, M.D.S. Child Care and the Growth of Love; Penguin Books: London, UK, 1965; ISBN 978-0-14-020271-7. [Google Scholar]
- Pardo, A.; Roman, M. Reflections on the Baron and Kenny Model of Statistical Mediation. An. Psicol. 2013, 29, 614–623. [Google Scholar]
| Total Sample | N = 147 |
|---|---|
| N (%), M, SD | |
| Age (ranging from 11 to 17) | 147 (100), 15.34, 1.316 |
| N (%), CI | |
| Sex | 147 (100) |
| Male | 90 (61.2) |
| Female | 57 (38.8) |
| Ethnicity | 137 (93.2) |
| Caucasian | 128 (87.1) |
| Latin American | 1 (0.7) |
| Black | 1 (0.7) |
| Gypsy | 1 (0.7) |
| Others | 6 (4.1) |
| Academic performance | 143 (97.3) |
| Repeated course YES | 65 (44.2) |
| Adopted | 143 (97.3) |
| YES | 13 (8.8) |
| Monthly income (EUR per capita) | 106 (72.1) |
| >2500 | 33 (22.4) |
| 2000–2500 | 27 (18.4) |
| 1500–1999 | 18 (12.2) |
| 500–1499 | 24 (16.3) |
| <500 | 4 (2.7) |
| Cohabitation status | 146 (99.3) |
| Family of origin | 126 (85.7) |
| Other relatives | 2 (1.4) |
| Adoptive family | 13 (8.8) |
| Institution | 4 (2.7) |
| Other | 1 (0.7) |
| Clinical diagnoses | 146 (99.3) |
| Behavioral disorders | 89 (60.5) |
| Emotional disorders | 19 (12.9) |
| Anxiety disorders | 16 (10.9) |
| Eating disorders | 11 (7.5) |
| Other | 7 (4.8) |
| No diagnosis | 4 (2.7) |
| 2 | 3 | 4 | 5 | 6 | 7 | Sex | Age | |
|---|---|---|---|---|---|---|---|---|
| R (p) | R (p) | R (p) | R (p) | R (p) | R (p) | R (p) | R (p) | |
| 1. Suicide risk | 0.321 (<0.001) ** | 0.234 (0.005) ** | 0.315 (<0.001) ** | 0.180 (0.031) * | −0.118 (0.158) | 0.063 (0.453) | 0.385 (<0.001) ** | 0.054 (0.519) |
| 2. SLE impact perceived | 0.681 (<0.001) ** | −0.339 (<0.001) ** | 0.171 (0.039) * | −0.272 (<0.001) ** | 0.102 (0.219) | 0.327 (<0.001) ** | −0.056 (0.498) | |
| 3. SLE | −0.302 (<0.001) ** | 0.115 (0.167) | −0.264 (0.001) ** | 0.000 1 | 0.179 (0.03) * | −0.03 (0.714) | ||
| 4. Family functioning | 0.029 (0.736) | 0.236 (0.006) ** | 0.122 (0.156) | −0.198 (0.020) * | 0.184 (0.032) * | |||
| 5. Number of clinical appointments | −0.107 (0.196) | 0.443 (<0.001) ** | 0.182 (0.027) * | −0.010 (0.902) | ||||
| 6. Length of follow-up in days | 0.104 (0.210) | −0.138 (0.095) | 0.151 (0.068) | |||||
| 7. Transferred to adult mental health service | 0.048 (0.546) | 0.125 (0.131) |
| Suicide Risk | |||||
|---|---|---|---|---|---|
| F; df (p) | R | R-Square | Adjusted R-Square | Std. Error of the Estimate | |
| Model 1 | 24,841; 1 (<0.001) ** | 0.385 | 0.148 | 0.142 | 0.555 |
| Model 2 | 16,571; 2 (<0.001) ** | 0.435 | 0.189 | 0.178 | 0.544 |
| Model 3 | 19,424; 2 (<0.001) ** | 0.477 | 0.227 | 0.216 | 0.528 |
| Model 4 | 15,113; 3 (<0.001) ** | 0.507 | 0.257 | 0.24 | 0.520 |
| IV to Mediators (a path) | |||
| Coeff | t | p | |
| Family APGAR | −0.0948 | −3.6023 | 0.0004 |
| Direct Effects of Mediators on DV (b path) | |||
| Coeff | t | p | |
| Family APGAR | −0.0709 | −3.0552 | 0.0027 |
| Total Effect of IV on DV (c path) | |||
| Coeff | t | p | |
| SLE impact perception | 0.0228 | 3.1447 | 0.0021 |
| Direct Effect of IV on DV (c’ path) | |||
| Coeff | t | p | |
| SLE impact perception | 0.0161 | 2.1834 | 0.0308 |
| Model Summary for DV Model | |||
| R-square | Adjusted R-square | F | p |
| 0.1307 | 0.1175 | 9.9214 | 0.0001 |
| Bootstrap Results for Indirect Effects | |||
| Indirect Effects of IV on DV through Proposed Mediators (ab paths) | |||
| Data | Boot | Bias | |
| Total | 0.0067 | 0.0069 | 0.0001 |
| Family APGAR | 0.0067 | 0.0069 | 0.0001 |
| Bias-Corrected Confidence Intervals | |||
| Lower | Upper | ||
| Total | 0.0018 | 0.0150 | |
| Family APGAR | 0.0018 | 0.0150 | |
| IV to Mediators (a path) | |||
| Coeff | t | p | |
| Family APGAR | −0.0842 | −3.2647 | 0.0014 |
| Direct Effects of Mediators on DV (b path) | |||
| Coeff | t | p | |
| Family APGAR | −0.0579 | −2.5607 | 0.0116 |
| Total Effect of IV on DV (c path) | |||
| Coeff | t | p | |
| SLE impact perception | 0.0176 | 2.5799 | 0.0110 |
| Direct Effect of IV on DV (c’ path) | |||
| Coeff | t | p | |
| SLE impact perception | 0.0127 | 1.8306 | 0.0695 |
| Partial Effect of Control Variables on DV | |||
| Coeff | t | p | |
| Sex | 0.4098 | 4.2517 | 0.0000 |
| Age | 0.0326 | 0.9232 | 0.3576 |
| Model Summary for DV Model | |||
| R-square | Adjusted R-square | F | p |
| 0.2523 | 0.2293 | 10.9646 | 0.0000 |
| Bootstrap Results for Indirect Effects | |||
| Indirect Effects of IV on DV through Proposed Mediators (ab paths) | |||
| Data | Boot | Bias | |
| Total | 0.0049 | 0.0048 | −0.0001 |
| Family APGAR | 0.0049 | 0.0048 | −0.0001 |
| Bias-Corrected Confidence Intervals | |||
| Lower | Upper | ||
| Total | 0.0012 | 0.0121 | |
| Family APGAR | 0.0012 | 0.0121 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caro-Cañizares, I.; Sánchez-Colorado, N.; Baca-García, E.; Carballo, J.J. Perceived Stressful Life Events and Suicide Risk in Adolescence: The Mediating Role of Perceived Family Functioning. Behav. Sci. 2024, 14, 35. https://doi.org/10.3390/bs14010035
Caro-Cañizares I, Sánchez-Colorado N, Baca-García E, Carballo JJ. Perceived Stressful Life Events and Suicide Risk in Adolescence: The Mediating Role of Perceived Family Functioning. Behavioral Sciences. 2024; 14(1):35. https://doi.org/10.3390/bs14010035
Chicago/Turabian StyleCaro-Cañizares, Irene, Nuria Sánchez-Colorado, Enrique Baca-García, and Juan J. Carballo. 2024. "Perceived Stressful Life Events and Suicide Risk in Adolescence: The Mediating Role of Perceived Family Functioning" Behavioral Sciences 14, no. 1: 35. https://doi.org/10.3390/bs14010035
APA StyleCaro-Cañizares, I., Sánchez-Colorado, N., Baca-García, E., & Carballo, J. J. (2024). Perceived Stressful Life Events and Suicide Risk in Adolescence: The Mediating Role of Perceived Family Functioning. Behavioral Sciences, 14(1), 35. https://doi.org/10.3390/bs14010035





