COVID-19 and the Nervous System from a Cuban Experience
Abstract
:1. Introduction
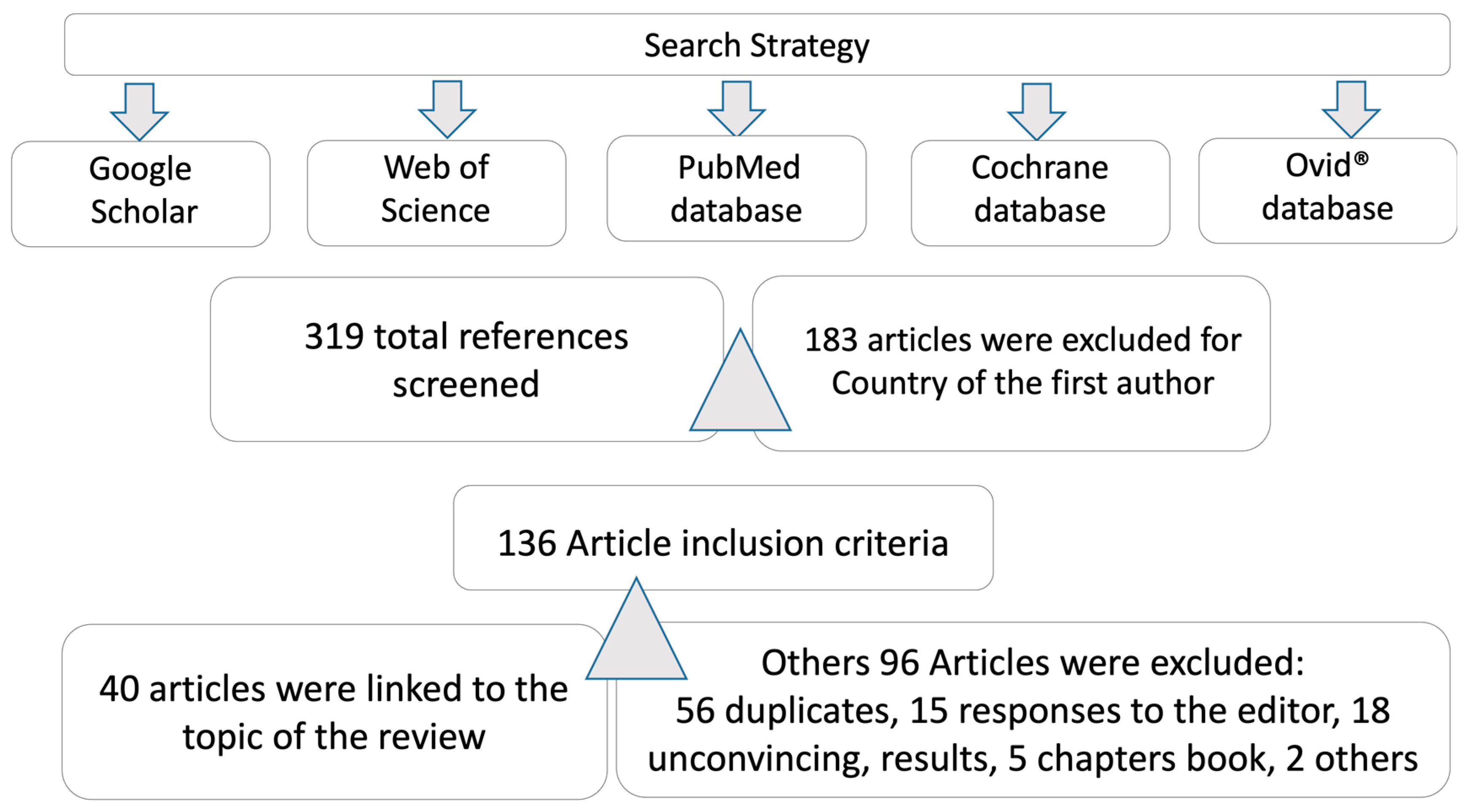
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Extraction
3. Results
3.1. General Considerations on Neurology and COVID-19
3.1.1. Neurologists and COVID-19
3.1.2. COVID-19-Induced Brain Dysfunction
3.2. Neuropsychology, Cognition, and Affective State in COVID-19
Psychological Security and COVID-19
3.3. Pathogenesis and Biomarkers
3.4. Neuroprotection, Neurodegeneration, and COVID-19
3.5. Neuropsychiatry Manifestation and COVID-19
3.5.1. Most Frequent Symptom of CNS in COVID-19
3.5.2. Most Frequent Symptoms of PNS in COVID-19
3.6. COVID-19 and Other Neurological Diseases
3.6.1. Epilepsy and COVID-19
3.6.2. Hereditary Ataxias and COVID-19
3.6.3. Cerebrovascular Disease and COVID-19
3.7. Psychoneuroimmunology and COVID-19
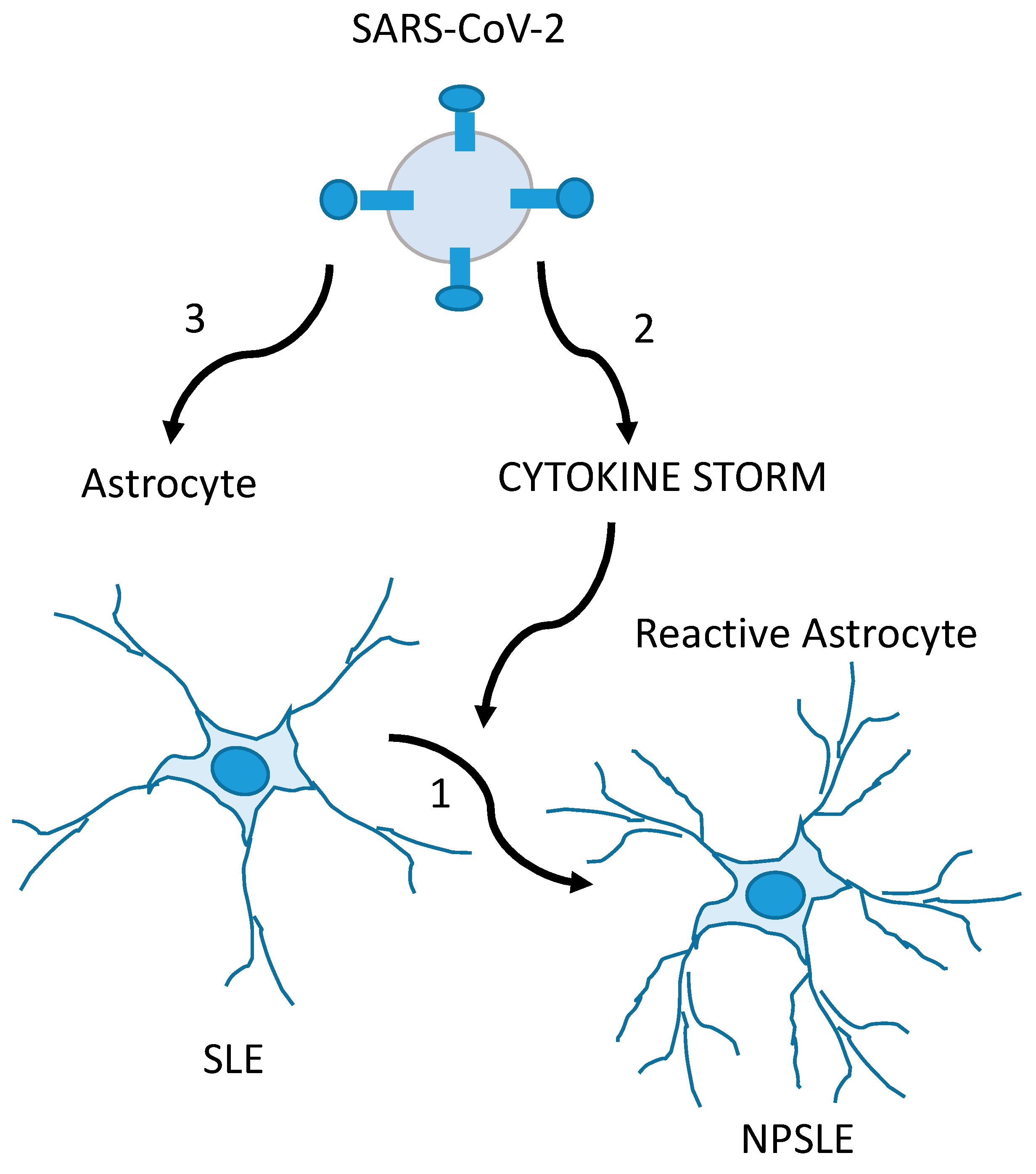
3.8. COVID-19 and Autoimmune Diseases
3.9. Intervention and Risk Management
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Josephson, S.A.; Kamel, H. Neurology and COVID-19. JAMA 2020, 324, 1139–1140. [Google Scholar] [CrossRef] [PubMed]
- Valdes, P.A.; Evans, A.C.; Valdes, M.J.; Poo, M.M. A call for international research on COVID-19-induced brain dysfunctions. Natl. Sci. Rev. 2021, 8, nwab190. [Google Scholar] [CrossRef] [PubMed]
- Shellhaas, R.A. Neurologists and COVID-19: A note on courage in a time of uncertainty. Neurology 2020, 94, 855–857. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, A.L.; Arcaño, D.K.; Pérez, D.Z. La psicología como ciencia en el afrontamiento a la COVID-19: Apuntes generales. Acad. Cienc. Cuba 2020, 10, 839. Available online: https://revistaccuba.sld.cu/index.php/revacc/article/view/839/855 (accessed on 6 September 2023).
- Velázquez, L. COVID-19: A challenge for science worldwide. Acad. Cienc. Cuba 2020, 10, 763. Available online: https://revistaccuba.sld.cu/index.php/revacc/article/view/763/792 (accessed on 6 September 2023).
- Broche-Pérez, Y. Neuropsychological Cognitive Sequelae in COVID-19 patients. MEDICC Rev. 2021, 23, 78. [Google Scholar] [CrossRef]
- Gutiérrez, A.K.; Cruz, A.Y.; Zaldivar, E.D. Management of health personnel’ psychological safety, in emergency situations by COVID-19 in the hospitable or isolation context. Rev. Cuba Enfermería 2020, 36, e3704. [Google Scholar]
- Hernández, I.; Gutiérrez, L. Basic Manual of Psychological First Aid. University of Guadalajara: Guadalajara, Mexico, 2014; Available online: https://psicologosemergenciasbaleares.files.wordpress.com/2016/08/manual-primeros-auxilios-psicolc3b3gicos_2014.pdf (accessed on 6 September 2023).
- Zambrano, V.H. Psychosocial Impact of the Earthquake of April 16, 2016 in the 5 de Agosto Parish in the City of Esmeraldas. Bachelor’s Thesis, Salesian Polytechnic University, Quito, Ecuador, 2018. Available online: http://dspace.ups.edu.ec/handle/123456789/16544 (accessed on 6 September 2023).
- Andrade, E. Characterization of the State of Mental Health in the Members of the Ibarra Fire Department Who Participated in the Earthquake of April 16, 2016 in Ecuador. Psychosocial Intervention Program. Bachelor’s Thesis, Universidad Técnica del Norte, Ibarra, Ecuador, 2017. Available online: http://repositorio.utn.edu.ec/handle/123456789/6467 (accessed on 19 July 2023).
- Martinez, J.R.; Rivas, Y.; Bermudez, L.L.; Gutierrez, E.B.; Rivero, I. Effects of COVID-19 on emotional affective states of the adult population of Puerto Padre. Electron. Mag. Dr. Zoilo E Mar. Vidaurreta 2020, 45, 6. Available online: http://revzoilomarinello.sld.cu/index.php/zmv/article/view/2388 (accessed on 6 September 2023).
- Liu, C.H.; Zhang, E.; Fifi Wong, G.T.; Hyun, S.; Chris, H.H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. Available online: https://www.clinicalkey.es/#!/content/journal/1-s2.0-S0165178120311185 (accessed on 29 June 2020). [CrossRef]
- Callís, S.; Guarton, O.M.; Cruz, V.; de-Armas, A.M. Emotional affective states in older adults alone in social isolation during the COVID-19 pandemic. Electron. Mag. Dr. Zoilo E Mar. Vidaurreta 2021, 46, 2491. Available online: http://revzoilomarinello.sld.cu/index.php/zmv/article/view/2491 (accessed on 6 September 2023).
- Lorenzo, J.C.; Díaz, H.; Cuello, M.B.; Ordoñez, L.Y.; Díaz, J.J. Depressive symptoms in patients diagnosed with COVID-19 in Pinar del Rio. Pinar Rio J. Med. Sci. 2021, 25, e4858. Available online: http://scielo.sld.cu/scielo.php?pid=S1561-1942021000100009=sci_arttextting=e (accessed on 6 September 2023).
- Espinosa, Y.; Mesa, D.; Diaz, Y.; Caraballo, L.; Mesa, M.Á. Study of the psychological impact of COVID-19 in students of Medical Sciences, Los Palacios. Cuba J. Public Health 2021, 46, e2659. Available online: http://www.scielosp.org/article/rcsp/2020.v46suppl1/e2659/es/ (accessed on 6 September 2023).
- Zayas, M.L.; Román, I.R.; Rodríguez, L.; Román, M.Y. Psychological impact on children, adolescents and the family related to social isolation by COVID-19. Electron. Mag. Dr. Zoilo E Mar. Vidaurreta 2021, 46, 2528. Available online: http://revzoilomarinello.sld.cu/index.php/zmv/article/view/2528 (accessed on 6 September 2023).
- Macías, A.M.; Ruiz, A.C.; Vidal, A.A. Psychological effects of work on health personnel in pandemic conditions. Guidelines for its proper management. Cuba J. Altern. Psychol. 2021, 58, 58–70. Available online: http://www.alfepsi.org/wp-content/uploads/2021/01/25-alternativas-cubanas-en-psicologia-v9n25-pdf#page=61 (accessed on 6 September 2023).
- Machado, C. Severe COVID-19 Cases: Is Respiratory Distress Partially Explained by Central Nervous System Involvement? MEDICC Rev. 2020, 22, 38–39. [Google Scholar]
- Machado, C.; DeFina, P.A.; Chinchilla, M.; Machado, Y.; Machado, Y. Brainstem Dysfunction in SARS-CoV-2 Infection can be a Potential Cause of Respiratory Distress. Neurol. India 2020, 68, 989–993. [Google Scholar] [PubMed]
- Anosmia and Ageusia as Initial or Unique Symptoms after SARS-CoV-2 Virus Infection. Available online: https://www.preprints.org/manuscript/202004.0272/v1 (accessed on 6 September 2023).
- Yao, L.; Lu, L.; Ma, W. Immunopathological changes, complications, sequelae and immunological memory in COVID-19 patients. Heliyon 2022, 8, e09302. [Google Scholar] [CrossRef]
- Padrón, A.A.; Dorta-Contreras, A. Patogenia de las manifestaciones neurológicas asociadas al SARS-CoV-2. Rev. Cuba Investig. Bioméd. 2020, 39, 1–16. [Google Scholar]
- Rodríguez, R.; Guzmán, P.; Dorta, A.J. Barrier dysfunction and Guillain-Barre syndrome as exponents of endothelial damage in COVID-19. Rev. Neurol. 2020, 71, 430. [Google Scholar]
- Redondo, M.J.; Rodríguez, F.J.; Pérez, O.; Del Valle, M.; Carrera, M. SARS-CoV-2, a new causal agent of guillain-barre syndrome. Rev. Neurol. 2020, 71, 275–276. [Google Scholar]
- Dorta, A.J. Neuroimmunological diagnosis of Guillain-Barré syndrome. Rev. Neurol. 2006, 43, 640. [Google Scholar]
- Rodríguez, J.C.; González, A. Neuroprotective strategies in COVID-19. Acad. Cienc. Cuba 2020, 10, 870. [Google Scholar]
- Lozada, I.D.; Maiguel, J.D.; Moscote, L.R. Neuroprotection in the patient with COVID-19. Cuba J. Biomed. Res. 2021, 40, el407. [Google Scholar]
- Meijides, C. SARS-CoV 2 from the central nervous system. Cuba J. Biomed. Res. 2020, 39, e1115. [Google Scholar]
- Romero, A.; Ramos, E.; López-Muñoz, F.; Gil-Martín, E.; Escames, G.; Reiter, R.J. Coronavirus disease 2019 (COVID-19) and its neuroinvasive capacity: Is it time for melatonin? Cell. Mol. Neurobiol. 2020, 42, 489–500. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Baylink, D.J.; Chen, C.S.; Reeves, M.E.; Xiao, J.; Lacy, C.; Lau, E.; Cao, H. The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19. J. Transl. Med. 2020, 18, 322. [Google Scholar] [CrossRef]
- Kempuraj, D.; Thangavel, R.; Kempuraj, D.; Ejaz, M.; Selvakumar, G.; Raikwar, S. Neuroprotective effects of flavone luteolin in neuroinflammation and neurotrauma. BioFactors 2020, 47, 190–197. [Google Scholar] [CrossRef]
- Pentón, G.; Marín, J.; McCarty, M.F. C-Phycocyanin-derived Phycocyanobilin as a Potential Nutraceutical Approach for Major Neurodegenerative Disorders and COVID-19- induced Damage to the Nervous System. Curr. Neuropharmacol. 2021, 19, 2250–2275. [Google Scholar] [CrossRef]
- Aguiar, A.M.; Roque, L.; Morejón, M. Neurological manifestations in patients with COVID-19. Univ. Méd. Pinareña 2022, 18, e675. [Google Scholar]
- Moreno-Zambrano, D.; Arévalo-Mora, M.; Freire-Bonifacini, A.; García-Santibanez, R.; Santibañez-Vásquez, R. Manifestaciones neurológicas asociadas a la infección por SARS-CoV-2: Una neuro-revisión de COVID-19. Rev. Ecuat. Neurol. 2020, 29, 115–124. [Google Scholar] [CrossRef]
- Rodriguez, A.J.; Cardona, J.A.; Gutiérrez, E.; Villamizar, R.; Holguin, Y.; Escalera, J.A.; Alvarado-Arnez, L.E.; Bonilla-Aldana, D.K.; Franco-Paredes, C.; Henao-Martinez, A.F.; et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 34, 101623. [Google Scholar] [CrossRef]
- Aldámiz, M.T.; Aledo, A.; Hernández, M.; Catalán, P.; Díez, C.; Martínez, E. COVID-19 Manual for the General Neurologist; SEN Editions: Madrid, Spain; Spanish Society of Neurology: Madrid, Spain, 2020; ISBN 978-84-946708-3-1. [Google Scholar]
- Xu, X.W.; Wu, X.X.; Jiang, X.G.; Xu, K.J.; Ying, L.J.; Ma, C.L.; Li, S.B.; Wang, H.Y.; Zhang, S.; Gao, H.N.; et al. Clinical fidings in a group of patients infected with the 2019 novel coronavirus (SARS-CoV-2) outside of Wuhan, China: Retrospective case series. BMJ 2019, 19, 368. [Google Scholar]
- León., R.; Bender, J.E.; Velázquez, L.C. Affectation of the nervous system by COVID-19. Ann. Cuba Acad. Sci. 2020, 10, 2. [Google Scholar]
- León, R.; Bender, J.E.; Velázquez, L.C. Olfactory dysfunction and COVID-19. Ann. Cuba Acad. Sci. 2020, 10, 2. [Google Scholar]
- Zhang, P. Be Cautious of Comorbidities of COVID-19 and Neurologic Diseases. Neurology Blogs. 2020. Available online: https://blogs.neurology.org/global/invited-commentary-be-cautious-of-comorbidities-of-COVID-19-and-neurologic-diseases/ (accessed on 6 September 2023).
- Li, Y.; Li, M.; Wang, M.; Zhou, Y.; Chang, J.; Xian, Y.; Wang, D.; Mao, L.; Jin, H.; Hu, B. Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study. Stroke Vasc. Neurol. 2020, 5, 279–284. [Google Scholar] [CrossRef]
- Welge, A. Impaired sense of smell and taste. Therapy options in anosmia and dysgeusia. Laryngorhinootologie 2005, 84, S92–S100. [Google Scholar]
- Haehner, A.; Hummel, T.; Reichmann, H. A clinical approach towards smell loss in parkinson’s disease. J. Park. Dis. 2014, 4, 189–195. [Google Scholar] [CrossRef]
- Robinson, M.A.; Gonçalves, C.A.; Noris, E.; Rivero, N.P.; Brigida, A.L.; Schultz, S.; Siniscalco, D.; García, R.J.G. Impact of SARS-CoV-2 on neuropsychiatric disorders. World J. Psychiatry 2021, 11, 347–354. [Google Scholar] [CrossRef]
- Robinson, M.A.; González, M.E.; Bergado, M.E. Autism, developmentand neural plasticity. In Translational Approaches to Autism Spectrum Disorder; Robinson Agramonte, M.A., Ed.; Springer: Berlin/Heidelberg, Germany, 2015; pp. 119–135. [Google Scholar]
- Lorigados, L.; Pavón, N. COVID-19 and neurological conditions. Panor. Cuba Health 2021, 16, 87–96. [Google Scholar]
- Bender, J.E.; Mendieta, M.; León, R.; Hernandez, L. Psychiatric manifestations in relation to SARS-CoV-2 infection. Ann. Cuba Acad. Sci. 2020, 10, 923. [Google Scholar]
- Valdés, M.J.; López, Á.; Palermo, F.J.; Martínez, I.; Martín, V.E.; Crespo, B.; Ruiz, M. Reactive psychoses in the context of the COVID-19 pandemic: Clinical perspectives from a case series. Rev. Psiquiatr. Salud Ment. 2020, 13, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Bender, J.E.; Mendieta, M.; León, R.; Hernandez, L. Epilepsy and COVID-19. Ann. Cuba Acad. Sci. 2020, 10. [Google Scholar]
- Bender, J.; Pedroso, M.D.; León, R.; Chacón, L. Epileptic Crisis, Epilepsy and COVID-19. EC Neurology 2021, 13, 8–18. Available online: https://www.ecronicon.com/ecne/pdf/ECNE-13-00845.pdf (accessed on 6 September 2023).
- Velázquez, L.; Vázquez, Y.; Rodríguez, R. Hereditary ataxias and COVID-19: Possible pathophysiological implications and recommendations. Ann. Cuba Acad. Sci. 2020, 10, e801. Available online: https://revistaccuba.sld.cu/index.php/revacc/article/view/801/830 (accessed on 6 September 2023).
- Specialized Committee of Neurogenetics Neurophysician Branch of Chinese Medical Doctor Association; Jiang, H.; Tang, B. Expert consensus on the management strategy of patients with hereditary ataxia during prevention and control of novel coronavirus pneumonia epidemic. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2020, 37, 359–366. [Google Scholar]
- Bender, J.E.; Mendieta, M.; León, R.; Hernandez, L. Cerebrovascular disease and COVID-19. Ann. Cuba Acad. Sci. 2020, 10, 1170–1172. [Google Scholar]
- Gonzalez, S.; Garófalo, N.; González, A.; Mezquia, N. COVID-19 infection and stroke. Cuba J. Biomed. Res. 2021, 40, E884. [Google Scholar]
- Ibanez, A.; Santamaria, H.; Guerrero, A.; Kornhuber, A.; Ton, A.M.M.; Slachevsky, A.; Teixeira, A.L.; Mar Meza, B.M.; Serrano, C.M.; Cano, C.; et al. The impact of SARS-CoV-2 in dementia across Latin America: Acall for an urgent regional plan and coordinated response. Alzheimer’s Dement. 2020, 6, e12092. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7683959/ (accessed on 6 September 2023). [CrossRef]
- Monet, E.D.; Gross, V.Y.; Alvarez, J.T. COVID-19 from the perspective of Psychoneuroimmunoendocrinology. Ann. Cuba Acad. Sci. 2022, 12. [Google Scholar]
- Noris, E.; Robinson, M.A. Psychoneuroimmunoendocrinology and COVID-19. Electron. Mag. Dr. Zoilo E Mar. Vidaurreta 2021, 46, 2523. Available online: https://revzoilomarinello.sld.cu/index.php/zmv/article/view/2523 (accessed on 6 September 2023).
- Noris, E.; Robinson, M.A.; Gonçalves, C.A. Utility of serum s100b as a marker in systemic lupus erythematosus. Patients during and after the SARS-CoV-2 pandemic. Arch. Med. Res. 2022, 53, 543–544. [Google Scholar] [CrossRef] [PubMed]
- Diaz, A.; Peláez, A.A.; Fuentes, M.; Cabrera, M.N.; Goncalves, C.A.; Schultz, S.; Siniscalco, D.; Robinson, M.A. SARS-CoV-2 Infection and Risk Management in Multiple Sclerosis. Diseases 2021, 9, 32. [Google Scholar] [CrossRef] [PubMed]
- Correa-Díaz, E.P.; Ortiz-Yépez, M.A.; Barrera-Madera, R.A.; Santos-Gamarro, M.J.; Paredes-González, V.E.; Acuña Chong, M.G.; Toral-Granda, A.M.; Miño-Zambrano, J.E.; Caiza-Zambrano, F.J.; Jácome-Sánchez, E.C. Ecuadorian recommendations for patients with multiple sclerosis in relation to a coronavirus pandemic (COVID-19). Ecuad. J. Neurol. 2020, 29, 12–15. [Google Scholar]
- Jiménez, A.D.; Gracia, F.; Adda, P.M.A.; Santos, V.S.B.B.; Enamorado, T.; Céspedes, J.V.; Rivera, V.M. Central American Consensus for the Treatment of Multiple Sclerosis and Therapeutic Attitudes Facing the COVID-19 Pandemic. 2020. Available online: http://www.lactrimsweb.org/wp-content/uploads/2020/11/39-Guias-Consenso-CAC.pdf (accessed on 6 September 2023).
- Fragoso, Y.D.; Schiavetti, I.; Carmisciano, L.; Ponzano, M.; Steinberg, J.; Treviño-Frenk, I.; Ciampi, E.; Vecino, M.C.A.; Correa, E.P.; Carcamo, C.; et al. Coronavirus disease 2019 in Latin American patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2021, 55, 103173. [Google Scholar] [CrossRef]
- Machado, C. Dangers and Management of Obstructive Sleep Apnea Syndrome in COVID-19 patients. MEDICC Rev. 2021, 23, 10. [Google Scholar]
- Chacón, L.M. Electroencephalogram and neurological manifestations in times of COVID-19. Why and how to do it? Ann. Cuba Acad. Sci. 2020, 10, 3. [Google Scholar]
- Valdés, R.R.; Vega, H. Guideline for Neurophysiological studies performance and their utility during a pandemic outbreak (COVID-19). Investig. Medicoquir. 2021, 13, 1. [Google Scholar]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robinson-Agramonte, M.d.l.A.; Sánchez, T.S.; García, E.N.; Barrera, O.R.S.; Siniscalco, D. COVID-19 and the Nervous System from a Cuban Experience. Behav. Sci. 2023, 13, 776. https://doi.org/10.3390/bs13090776
Robinson-Agramonte MdlA, Sánchez TS, García EN, Barrera ORS, Siniscalco D. COVID-19 and the Nervous System from a Cuban Experience. Behavioral Sciences. 2023; 13(9):776. https://doi.org/10.3390/bs13090776
Chicago/Turabian StyleRobinson-Agramonte, Maria de los Angeles, Teresa Serrano Sánchez, Elena Noris García, Orlando Rafael Serrano Barrera, and Dario Siniscalco. 2023. "COVID-19 and the Nervous System from a Cuban Experience" Behavioral Sciences 13, no. 9: 776. https://doi.org/10.3390/bs13090776
APA StyleRobinson-Agramonte, M. d. l. A., Sánchez, T. S., García, E. N., Barrera, O. R. S., & Siniscalco, D. (2023). COVID-19 and the Nervous System from a Cuban Experience. Behavioral Sciences, 13(9), 776. https://doi.org/10.3390/bs13090776





