Mental Health of People with Intellectual Disabilities Living in Residential Care before, during, and after Lockdown
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Setting
2.3. Participants
2.4. Measurement
2.5. Bias
2.6. Study Size
2.7. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Mental Health Report: Transforming Mental Health for All; World Health Organization: Geneva, Switzerland, 2022; ISBN 978-92-4-004933-8. [Google Scholar]
- Ministerio de Sanidad. Plan de Respuesta Temprana en un Escenario de Control de la Pandemia por COVID-19. 2020. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/COVID19_Plan_de_respuesta_temprana_escenario_control.pdf (accessed on 3 September 2022).
- Fernández, E.; García, L. COVID-19 y salud mental. Rev. Española Salud Pública 2020, 94. Available online: https://www.sanidad.gob.es/biblioPublic/publicaciones/recursos_propios/resp/revista_cdrom/Suplementos/Perspectivas/perspectivas4_fernandez_garcia.pdf (accessed on 20 April 2023).
- Utku, A.C.; Budak, G.; Karabay, O.; Güçlü, E.; Okan, H.D.; Vatan, A. Main symptoms in patients presenting in the COVID-19 period. Scott. Med. J. 2020, 65, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Javanmardi, F.; Keshavarzi, A.; Akbari, A.; Emami, A.; Pirbonyeh, N. Prevalence of underlying diseases in died cases of COVID-19: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0241265. [Google Scholar] [CrossRef] [PubMed]
- Crespo-Cuadrado, M.; Verdugo-Alonso, M.A.; Navas, P.; Martínez-Torres, S.; Amor-González, A.M. Impacto de la COVID-19 y discapacidades intelectuales y del desarrollo: Impacto del confinamiento desde la perspectiva de las personas, sus familiares y los profesionales y organizaciones que prestan apoyo. Siglo Cero 2020, 1, 11–36. [Google Scholar] [CrossRef]
- Courtenay, K.; Perera, B. COVID-19 and people with intellectual disability: Impacts of a pandemic. Ir. J. Psychol. Med. 2020, 37, 231–236. [Google Scholar] [CrossRef]
- Unit Nations. Policy Brief: A Disability-Inclusive Response to COVID-19. 2020. Available online: https://www.un.org/sites/un2.un.org/files/spanish_disability_brief.pdf (accessed on 20 April 2023).
- Krahn, G.L.; Klein, D.; Correa-De-Araujo, R. Persons with disabilities as an unrecognized health disparity population. Am. J. Public Health 2015, 105 (Suppl. 2), S198–S206. [Google Scholar] [CrossRef]
- Landes, S.D.; Turk, M.A.; Formica, M.K.; McDonald, K.E.; Stevens, J.D. COVID-19 outcomes among people with intellectual and developmental disability living in residential group homes in New York State. Disabil. Health J. 2020, 13, 100969. [Google Scholar] [CrossRef]
- Lunsky, Y.; Durbin, A.; Balogh, R.; Lin, E.; Palma, L.; Plumptre, L. COVID-19 positivity rates, hospitalizations and mortality of adults with and without intellectual and developmental disabilities in Ontario, Canada. Disabil. Health J. 2022, 15, 101174. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual Of Mental Disorders, 5th ed.; Text Revision (DSM-5-TR); American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar] [CrossRef]
- Taggart, L.; Mulhall, P.; Kelly, R.; Trip, H.; Sullivan, B.; Wallén, E.F. Preventing, mitigating, and managing future pandemics for people with an intellectual and developmental disability—Learnings from COVID-19: A scoping review. J. Policy Pract. Intellect. Disabil. 2022, 19, 4–34. [Google Scholar] [CrossRef]
- Muñoz-Bravo, J.; de Araoz-Sánchez-Dopico, I. Reflexiones sobre el acceso a los servicios de salud de las personas con discapacidad intelectual o del desarrollo en el marco de la crisis sanitaria creada por la pandemia de la Covid-19. Siglo Cero 2021, 1, 197–214. [Google Scholar] [CrossRef]
- Doody, O.; Keenan, P.M. The reported effects of the COVID-19 pandemic on people with intellectual disability and their carers: A scoping review. Ann. Med. 2021, 53, 786–804. [Google Scholar] [CrossRef]
- Drum, C.E.; Oberg, A.; Ditsch, J.; Cooper, K.; Carlin, R. COVID-19 & Adults with Intellectual Disability, Autism, Epilepsy, or Brain Injuries. American Association on Health and Disability. Available online: https://aahd.us/wp-content/uploads/2020/06/COVID-19_DCRM_Intellectual-Disability_Autism_Epilepsy_or_Brain_InjuryBMSF_508.pdf (accessed on 26 April 2023).
- Navas, P.; Amor, A.M.; Crespo, M.; Wolowiec, Z.; Verdugo, M.A. Supports for people with intellectual and developmental disabilities during the COVID-19 pandemic from their own perspective. Res. Dev. Disabil. 2021, 108, 103813. [Google Scholar] [CrossRef] [PubMed]
- Fisher, M.H.; Sung, C.; Kammes, R.R.; Okyere, C.; Park, J. Social support as a mediator of stress and life satisfaction for people with intellectual or developmental disabilities during the COVID-19 pandemic. J. Appl. Res. Intellect. Disabil. 2022, 35, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Thabile, A.S. Leaving no one behind: Intellectual disability during COVID-19 in Africa. Int. Soc. Work 2021, 64, 265–269. [Google Scholar] [CrossRef]
- Randall, K.N.; McKown, G.L. Perceived Impact of the COVID-19 Pandemic on Adults with Intellectual and Developmental Disability: A Qualitative Study. J. Intellect. Disabil. 2022, 17446295221146352. [Google Scholar] [CrossRef]
- Lunsky, Y.; Jahoda, A.; Navas, P.; Campanella, S.; Havercamp, S.M. The mental health and well-being of adults with intellectual disability during the COVID-19 pandemic: A narrative review. J. Policy Pract. Intellect. Disabil. 2022, 19, 35–47. [Google Scholar] [CrossRef]
- Navas, P.; Verdugo, M.Á.; Martínez, S.; Amor, A.M.; Crespo, M.; Deliu, M.M. Impact of COVID-19 on the burden of care of families of people with intellectual and developmental disabilities. J. Appl. Res. Intellect. Disabil. 2022, 35, 577–586. [Google Scholar] [CrossRef]
- Chaplin, E.; Paschos, D.; O’Hara, J.M.; McCarthy, J.; Holt, G.; Bouras, N.; Tsakanikos, E. Mental ill-health and care pathways in adults with intellectual disability across different residential types. Res. Dev. Disabil. 2010, 32, 458–463. [Google Scholar] [CrossRef]
- Smiley, E.; Cooper, S.A.; Finlayson, J.; Jackson, A.; Allan, L.; Mantry, D.; McGrother, C.; McConnachie, A.; Morrison, J. Incidence and predictors of mental ill-health in adults with intellectual disabilities: Prospective study. Br. J. Psychiatry J. Ment. Sci. 2007, 191, 313–319. [Google Scholar] [CrossRef]
- Braga, R.; Felipe-Castaño, E. The Impact of the COVID-19 Lockdown on the Cognitive Functions in Persons with Intellectual and Developmental Disabilities. Int. J. Environ. Res. Public Health 2022, 19, 15511. [Google Scholar] [CrossRef]
- Orden de 13 de Marzo de 2020, Preventive Public Health Measures Are Adopted in the Community of Andalucia as a Con-sequence of the Situation and Evolution of the Coronavirus (COVID-19). Boletín Oficial de la Junta de Andalucía 5. 2020. Available online: https://www.ual.es/application/files/3615/8417/2535/BOJA20-505-00008.pdf (accessed on 3 September 2022).
- Cáceres-Rodríguez, C.; Yepes-García, I.; Sebastià-Bargues, Á.; Martín-Martín, R. How Did People with Disabilities Experience the COVID-19 Crisis? Situation of People Supported by Guardianship Organizations in Spain. Siglo Cero 2022, 53, 41–60. [Google Scholar] [CrossRef]
- Puyaltó, C.; Beltran, M.; Coll, T.; Diaz-Garolera, G.; Figueras, M.; Fullana, J.; González, C.; Pallisera, M.; Pujolar, J.; Rey, A. Relationships of People with Intellectual Disabilities in Times of Pandemic: An Inclusive Study. Soc. Sci. 2022, 11, 198. [Google Scholar] [CrossRef]
- Amor, A.M.; Navas, P.; Verdugo, M.A.; Crespo, M. Perceptions of people with intellectual and developmental disabilities about COVID-19 in Spain: A cross-sectional study. J. Intellect. Disabil. Res. 2021, 65, 381–396. [Google Scholar] [CrossRef] [PubMed]
- Friedman, C. The COVID-19 pandemic and quality of life outcomes of people with intellectual and developmental disabilities. Disabil. Health J. 2021, 14, 1–8. [Google Scholar] [CrossRef]
- Perera, B.; Laugharne, R.; Henley, W.; Zabel, A.; Lamb, K.; Branford, D.; Courtanay, K.; Alexander, R.; Purandare, K.; Wijeratne, A.; et al. COVID-19 deaths in people with intellectual disability in the UK and Ireland: Descriptive study. BJPsych Open 2020, 6, e123. [Google Scholar] [CrossRef] [PubMed]
- Lake, K.K.; Jachyra, P.; Volpe, T.; Lunsky, Y.; Magnacca, C.; Marcinkiewicz, A.; Hamdani, Y. The Wellbeing and Mental Health Care Experiences of Adults with Intellectual and Developmental Disabilities during COVID-19. J. Ment. Health Res. Intellect. Disabil. 2021, 14, 285–300. [Google Scholar] [CrossRef]
- Verdugo, M.A.; Gómez, L.E.; Arias, B.; Santamaría, M.; Clavero, D.; Tamarit, J. Escala INICO-FEAPS Evaluación Integral de la Calidad de Vida de Personas con Discapacidad Intelectual o del Desarrollo; Publicaciones del INICO Instituto Universitario de Integración en la Comunidad Universidad de Salamanca: Salamanca, Spain, 2013. [Google Scholar]
- Verdugo, M.A.; Gómez, L.E.; Arias, B.; Santamaría, M.; Navallas, E.; Fernández, S.; Hierro, I. Escala San Martín Evaluación de la Calidad de Vida de Personas con Discapacidades Significativas; Fundación Obra San Martín: Santander, Spain, 2014. [Google Scholar]
- Amor, A.M.; Verdugo, M.Á.; Fernández, M.; Aza, A.; Sánchez-Gómez, V.; Wolowiec, Z. Development and Validation of Standardized Quality of Life Measures for Persons with IDD. Behav. Sci. 2023, 13, 452. [Google Scholar] [CrossRef]
- Verdugo, M.A.; Ibáñez, A.; Arias, B. Adaptación transcultural al español de la Escala de Intensidad de los apoyos. Siglo Cero 2007, 38, 5–16. [Google Scholar]
- Thompson, J.R.; Bryant, B.; Campbell, E.M.; Craig, E.M.; Hughes, C.; Rotholz, D.A.; Schalock, R.L.; Silverman, W.; Tasse, M.J.; Wehmeyer, M. Supports Intensity Scale. Users Manual; American Association on Mental Retardation: Silver Spring, MD, USA, 2004. [Google Scholar]
- Thompson, J.R.; Shogren, K.A.; Seo, H.; Wehmeyer, M.L.; Lang, K.M. Creating SIS—A Annual Review Protocol to Determine the Need for Reassessment. Intellect. Dev. Disabil. 2016, 54, 217–228. [Google Scholar] [CrossRef]
- Matson, J.L. The Diagnostic Assessment for the Severely Handicapped-Revised (DASH-II); Disability Consultants LLC: Baton Rouge, LA, USA, 1995. [Google Scholar]
- Novell, R.; Rueda, P.; Salvador-Carulla, L.; Forgas, E. Salud Mental y alteraciones de conducta en las personas con discapacidad intelectual. Guía práctica para técnicos y cuidadores (Diagnostic Assessment for the Severely Handicapped Revised (DASH-II. Spanish version); FEAP: Madrid, Spain, 2003. [Google Scholar]
- Vargas-Vargas, C.; Rafanell, A.; Montalvo, D.; Estarlich, M.; Pomarol-Clotet, E.; Sarró, S. Validity and reliability of the Spanish version of the diagnostic assessment for the severely handicapped (DASH-II). Res. Dev. Disabil. 2015, 36, 537–542. [Google Scholar] [CrossRef]
- Ribot, V.C.; Chang, N.; González, A.L. Efectos de la COVID-19 en la salud mental de la población. Rev. Habanera Cienc. Médicas 2020, 19 (Suppl. S1), 1–11. Available online: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1729-519X2020000400008 (accessed on 4 September 2022).
- Cénat, J.M.; Farahi, S.M.M.M.; Dalexis, R.D.; Darius, W.P.; Bekarkhanechi, F.M.; Poisson, H.; Broussard, C.; Ukwu, G.; Auguste, E.; Nguyen, D.D.; et al. The global evolution of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2022, 315, 70–95. [Google Scholar] [CrossRef] [PubMed]
- Solís, P. Las personas con discapacidad intelectual ante el COVID-19: Una revisión sistemática. En-Claves Pensam. 2022, 16, 1–21. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Sandín, B.; Valiente, R.M.; García-Escalera, J.; Chorot, P. Impacto psicológico de la pandemia de COVID-19: Efectos negativos y positivos en población española asociados al momento de confinamiento nacional. Rev. Psicopatología Psicol. Clínica 2020, 25, 1–22. [Google Scholar] [CrossRef]
- den Houting, J. Stepping out of isolation: Autistic people and COVID-19. Autism Adulthood 2020, 2, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, Y.; Nagarajan, R.; Kumar, G.; Menon, V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020, 293, 113382. [Google Scholar] [CrossRef]
- Peltopuro, M.; Ahonen, T.; Kaartinen, J.; Seppälä, H.; Nrhi, V. Borderline intellectual functioning: A systematic literature review. Intellect. Dev. Disabilil. 2014, 52, 419–443. [Google Scholar] [CrossRef]
- Tostika, V.; Emerson, E.; Hastings, R.P.; Hatton, C. The impact of COVID-19 pandemic on the health of adults with intellectual impairment: Evidence from two longitudinal UK surveys. J. Intellect. Disabil. Res. 2021, 65, 890–897. [Google Scholar]
- Courtenay, K. COVID-19. Challenges for people with intellectual disability. BMJ 2020, 369, m1609. [Google Scholar] [CrossRef]
- Wilson, N.J.; Chen, Y.-W.; Mahoney, N.; Buchanan, A.; Marks, A.; Cordier, R. Experience sampling method and the everyday experiences of adults with intellectual disability: A feasibility study. J. Appl. Res. Intellect. Disabil. 2020, 33, 1328–1339. [Google Scholar] [CrossRef] [PubMed]
| Assessment | Description | |
|---|---|---|
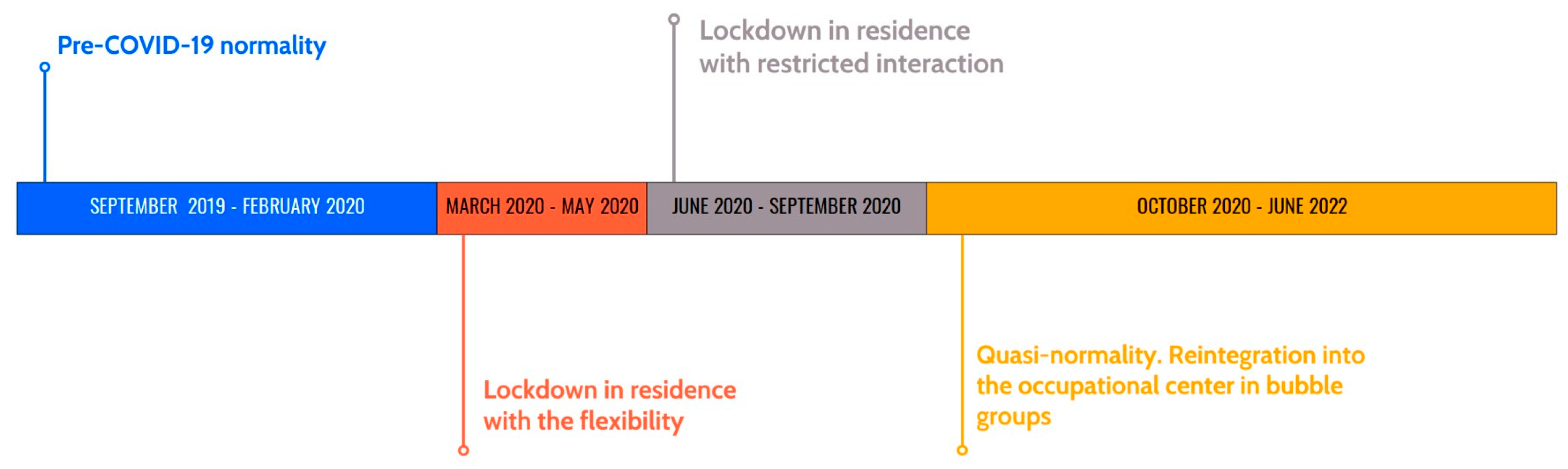
| TIME 1 19 September–20 February | T1: 20 February | Pre-COVID-19 normality |
| TIME 2 March–20 May | T2: 20 May | Lockdown in residence with flexible schedules, activities, and freedom of interaction between all the residential users. |
| TIME 3 June–20 September | T3: 20 September | Residents divided into stable groups. Lockdown in residence with limited interaction between people on the same floor (only men/only young women/only older women) |
| TIME 4 21 October–22 June | T4: 22 June | Quasi-normality. Reintegration into the occupational center in bubble groups. Interaction with family home users is allowed for two weeks in June, but the new restriction to the bubble group was reinstated in mid-June 2021. As a result, data collection was extended until the restrictions were reduced to a minimum, which took one year for this phase. |
| Variables | or % (n) |
|---|---|
| Sex | |
| Women | 54.2% (13) |
| Men | 45.8% (11) |
| Age | 40.17 ± 13.09 |
| Level of Intellectual Disability | |
| Mild | 29.2% (7) |
| Moderate | 70.8% (17) |
| T1. 1 | T2. 2 | T3. 3 | T4. 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Anxiety | 2.04 | 2.33 | 1.79 | 1.91 | 2.67 | 3.41 | 2.12 | 2.27 |
| Depression | 4.46 | 4.42 | 4.21 | 4.21 | 5.12 | 5.17 | 4.50 | 4.59 |
| Syn. Organic | 2.42 | 1.86 | 3.26 | 3.24 | 3.79 | 3.5 | 2.83 | 2.53 |
| T1. 1 | T2. 2 | T3. 3 | T4. 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Support Needs Total Score | 77.83 | 22.78 | 78 | 23.1 | 82.04 | 19.19 | 77.71 | 23.81 |
| Home Living | 78.08 | 21.08 | 79.92 | 19.64 | 81.04 | 19.21 | 79.71 | 20.84 |
| Community Living | 73.42 | 28.3 | 74.08 | 27.52 | 73.71 | 27.89 | 73.25 | 29.10 |
| Employment | 73.5 | 27.13 | 77.83 | 24 | 76.83 | 25.59 | 73.58 | 28.61 |
| Health and Safety | 76.42 | 24.02 | 78 | 24.87 | 79.21 | 23.79 | 77.29 | 25.61 |
| Social activities | 75.08 | 22.94 | 75.38 | 25.73 | 77.92 | 22.9 | 77.17 | 23.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gil-Llario, M.D.; Díaz-Rodríguez, I.; Fernández-García, O.; Estruch-García, V.; Bisquert-Bover, M.; Ballester-Arnal, R. Mental Health of People with Intellectual Disabilities Living in Residential Care before, during, and after Lockdown. Behav. Sci. 2023, 13, 695. https://doi.org/10.3390/bs13080695
Gil-Llario MD, Díaz-Rodríguez I, Fernández-García O, Estruch-García V, Bisquert-Bover M, Ballester-Arnal R. Mental Health of People with Intellectual Disabilities Living in Residential Care before, during, and after Lockdown. Behavioral Sciences. 2023; 13(8):695. https://doi.org/10.3390/bs13080695
Chicago/Turabian StyleGil-Llario, María Dolores, Irene Díaz-Rodríguez, Olga Fernández-García, Verónica Estruch-García, Mar Bisquert-Bover, and Rafael Ballester-Arnal. 2023. "Mental Health of People with Intellectual Disabilities Living in Residential Care before, during, and after Lockdown" Behavioral Sciences 13, no. 8: 695. https://doi.org/10.3390/bs13080695
APA StyleGil-Llario, M. D., Díaz-Rodríguez, I., Fernández-García, O., Estruch-García, V., Bisquert-Bover, M., & Ballester-Arnal, R. (2023). Mental Health of People with Intellectual Disabilities Living in Residential Care before, during, and after Lockdown. Behavioral Sciences, 13(8), 695. https://doi.org/10.3390/bs13080695








