Individual and Contextual Variables as Predictors of MRI-Related Perceived Anxiety
Abstract
1. Introduction
2. Individual and Contextual Variables
3. The Current Study
4. Study One
4.1. Materials and Methods
4.1.1. Participants
4.1.2. Materials
4.1.3. Procedure
4.2. Results
4.3. Discussion
5. Study Two
5.1. Materials and Methods
5.1.1. Participants
5.1.2. Materials
5.1.3. Procedure
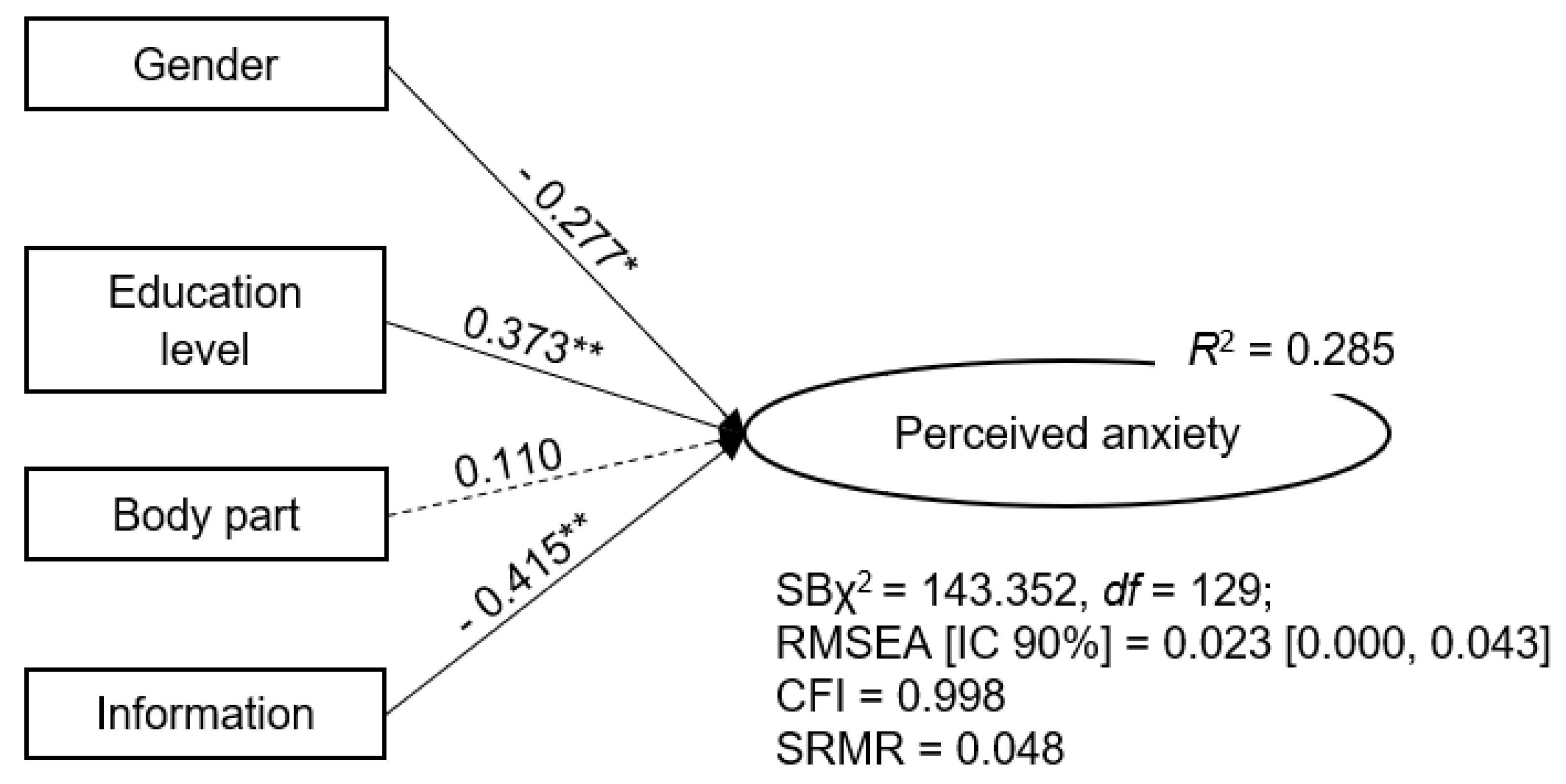
5.2. Results
5.3. Discussion
6. General Discussion
7. Limitations, Strengths, and Further Studies
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arda, K.N.; Akay, S.; Yetkin, S. Is there a relationship between oxygen saturation and MRI-induced anxiety? A prospective study. Clin. Imaging 2020, 60, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Almutlaq, Z.M. Discussion of the causes, effect and potential methods of alleviating patient anxiety when undergoing magnetic resonance imaging (MRI). Egypt. J. Hosp. Med. 2018, 72, 4473–4477. [Google Scholar] [CrossRef]
- Siafaka, P.I.; Okur, N.Ü.; Karantas, I.D.; Okur, M.E.; Gündoğdu, E.A. Current update on nanoplatforms as therapeutic and diagnostic tools: A review for the materials used as nanotheranostics and imaging modalities. Asian J. Pharm. Sci. 2021, 16, 24–46. [Google Scholar] [CrossRef] [PubMed]
- Nakarada-Kordic, I.; Reay, S.; Bennett, G.; Kruse, J.; Lydon, A.M.; Sim, J. Can virtual reality simulation prepare patients for an MRI experience? Radiography 2020, 26, 205–213. [Google Scholar] [CrossRef]
- Cable, J.; Bormann, S. Anxiety during “first time” magnetic resonance imaging. J. Health Res. 2015, 9, 64–68. [Google Scholar]
- Dziuda, Ł.; Zieliński, P.; Baran, P.; Krej, M.; Kopka, L. A study of the relationship between the level of anxiety declared by MRI patients in the STAI questionnaire and their respiratory rate acquired by a fibre-optic sensor system. Sci. Rep. 2019, 9, 4341. [Google Scholar] [CrossRef]
- Bolejko, A.; Hagell, P. Effects of an information booklet on patient anxiety and satisfaction with information in magnetic resonance imaging: A randomized, single-blind, placebo-controlled trial. Radiography 2021, 27, 162–167. [Google Scholar] [CrossRef]
- van Minde, D.; Klaming, L.; Weda, H. Pinpointing moments of high anxiety during an MRI examination. Int. J. Behav. Med. 2014, 21, 487–495. [Google Scholar] [CrossRef]
- Ahlander, B.M.; Engvall, J.; Ericsson, E. Anxiety during magnetic resonance imaging of the spine in relation to scanner design and size. Radiography 2020, 26, 110–116. [Google Scholar] [CrossRef]
- Nguyen, X.V.; Tahir, S.; Bresnahan, B.W.; Andre, J.B.; Lang, E.V.; Mossa-Basha, M.; Mayr, N.A.; Bourekas, E.C. Prevalence and Financial Impact of Claustrophobia, Anxiety, Patient Motion, and Other Patient Events in Magnetic Resonance Imaging. Top. Magn. Reason. Imaging 2020, 29, 125–130. [Google Scholar] [CrossRef]
- Klaming, L.; van Minde, D.; Weda, H.; Nielsen, T.; Duijm, L.E. The Relation Between Anticipatory Anxiety and Movement During an MR Examination. Acad. Radiol. 2015, 22, 1571–1578. [Google Scholar] [CrossRef] [PubMed]
- Semedo, C.S.; Diniz, A.M.; Herédia, V. Training health professionals in patient-centered communication during magnetic resonance imaging to reduce patients’ perceived anxiety. Patient Educ. Couns. 2020, 103, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Barlow, D.H. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. Am. Psychol. 2000, 55, 1247–1263. [Google Scholar] [CrossRef] [PubMed]
- Tazegul, G.; Etcioglu, E.; Yildiz, F.; Yildiz, R.; Tuney, D. Can MRI related patient anxiety be prevented? Magn. Reason. Imaging 2015, 33, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Thu, H.; Etcioglu, E.; Yildiz, F.; Tuney, D. Factors associated with increased anxiety in the MRI waiting room. J. Radiol. Nurs. 2015, 34, 140–174. [Google Scholar] [CrossRef]
- Katz, R.C.; Wilson, L.; Frazer, N. Anxiety and its determinants in patients undergoing magnetic resonance imaging. J. Behav. Ther. Exp. Psychiatry 1994, 25, 131–134. [Google Scholar] [CrossRef]
- Baran, P.; Truszczynski, O.; Dziuda, L. Anxiety in patients undergoing magnetic resonance imaging. Pol. J. Aviat. Med. Psychol. 2015, 21, 5–8. [Google Scholar] [CrossRef]
- Chapman, H.A.; Bernier, D.; Rusak, B. MRI-related anxiety levels change within and between repeated scanning sessions. Psychiatry Res. 2010, 182, 160–164. [Google Scholar] [CrossRef]
- Ahlander, B.M.; Årestedt, K.; Engvall, J.; Maret, E.; Ericsson, E. Development and validation of a questionnaire evaluating patient anxiety during Magnetic Resonance Imaging: The Magnetic Resonance Imaging-Anxiety Questionnaire (MRI-AQ). J. Adv. Nurs. 2016, 72, 1368–1380. [Google Scholar] [CrossRef]
- Harris, L.M.; Menzies, R.G.; Robinson, J. Predictors of panic symptoms during magnetic resonance imaging scans. Int. J. Behav. Med. 2001, 8, 80–87. [Google Scholar] [CrossRef]
- Napp, A.E.; Enders, J.; Roehle, R.; Diederichs, G.; Rief, M.; Zimmermann, E.; Martus, P.; Dewey, M. Analysis and Prediction of Claustrophobia during MR Imaging with the Claustrophobia Questionnaire: An Observational Prospective 18-month Single-Center Study of 6500 Patients. Radiology 2017, 283, 148–157. [Google Scholar] [CrossRef]
- Murphy, K.J.; Brunberg, J.A. Adult claustrophobia, anxiety and sedation in MRI. Magn. Reason. Imaging 1997, 15, 51–54. [Google Scholar] [CrossRef]
- Norbash, A.; Yucel, K.; Yuh, W.; Doros, G.; Ajam, A.; Lang, E.; Pauker, S.; Mayr, N. Effect of team training on improving MRI study completion rates and no-show rates. J. Magn. Reason. Imaging 2016, 44, 1040–1047. [Google Scholar] [CrossRef] [PubMed]
- Forshaw, K.L.; Boyes, A.W.; Carey, M.L.; Hall, A.E.; Symonds, M.; Brown, S.; Sanson-Fisher, R.W. Raised Anxiety Levels Among Outpatients Preparing to Undergo a Medical Imaging Procedure: Prevalence and Correlates. J. Am. Coll. Radiol. 2018, 15, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Heyer, C.M.; Thüring, J.; Lemburg, S.P.; Kreddig, N.; Hasenbring, M.; Dohna, M.; Nicolas, V. Anxiety of patients undergoing CT imaging-an underestimated problem? Acad. Radiol. 2015, 22, 105–112. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, R.; Sims, C.; Owens, R.G.; Dixon, A.K. Patients’ perceptions of magnetic resonance imaging. Clin. Radiol. 1995, 50, 137–143. [Google Scholar] [CrossRef]
- Eshed, I.; Althoff, C.E.; Hamm, B.; Hermann, K.G. Claustrophobia and premature termination of magnetic resonance imaging examinations. J. Magn. Reason. Imaging 2007, 26, 401–404. [Google Scholar] [CrossRef]
- Ajam, A.A.; Tahir, S.; Makary, M.S.; Longworth, S.; Lang, E.V.; Krishna, N.G.; Mayr, N.A.; Nguyen, X.V. Communication and Team Interactions to Improve Patient Experiences, Quality of Care, and Throughput in MRI. Top. Magn. Reason. Imaging 2020, 29, 131–134. [Google Scholar] [CrossRef]
- Hashim, M.J. Patient-Centered Communication: Basic Skills. Am. Fam. Physician 2017, 95, 29–34. [Google Scholar]
- Gaspar, R.; Domings, S.; Diniz, A.M.; Falanga, R. Barriers to and facilitators of older adult’s adherence to health recommendations: Towards an engaging two-way health communication. In Promoting Patient Engagement and Participation for Effective Healthcare Reform; Graffigna, G., Ed.; IGI Global: Hershey, PA, USA, 2016; pp. 58–82. [Google Scholar] [CrossRef]
- Chandra, S.; Mohammadnezhad, M.; Ward, P. Trust and Communication in a Doctor-Patient Relationship: A Literature Review. J. Healthc. Commun. 2018, 3, 36. [Google Scholar] [CrossRef]
- Chadderdon, A.L.; Carns, D.R.; Pudalov, L.R.; McKernan, L.C.; Honce, J.M. Underlying Mechanisms of Psychological Interventions in Magnetic Resonance Imaging and Image-Guided Radiology Procedures. Top. Magn. Reason. Imaging 2020, 29, 157–163. [Google Scholar] [CrossRef]
- Itri, J.N. Patient-centered Radiology. Radiographics 2015, 35, 1835–1846. [Google Scholar] [CrossRef] [PubMed]
- Dewey, M.; Schink, T.; Dewey, C.F. Claustrophobia during magnetic resonance imaging: Cohort study in over 55,000 patients. J. Magn. Reason. Imaging 2007, 26, 1322–1327. [Google Scholar] [CrossRef] [PubMed]
- Foldes, Z.; Ala-Ruona, E.; Burguer, B.; Orsi, G. Anxiety reduction with music and tempo synchronization on magnetic resonance imaging patients. Psychomusicol. Music Mind Brain 2017, 27, 343–349. [Google Scholar] [CrossRef]
- Lo Re, G.; De Luca, R.; Muscarneri, F.; Dorangricchia, P.; Picone, D.; Vernuccio, F.; Salerno, S.; La Tona, G.; Pinto, A.; Midiri, F.; et al. Relationship between anxiety level and radiological investigation. Comparison among different diagnostic imaging exams in a prospective single-center study. Radiol. Med. 2016, 121, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Grey, S.J.; Price, G.; Mathews, A. Reduction of anxiety during MR imaging: A controlled trial. Magn. Reason. Imaging 2000, 18, 351–355. [Google Scholar] [CrossRef]
- Tugwell, J.R.; Goulden, N.; Mullins, P. Alleviating anxiety in patients prior to MRI: A pilot single-centre single-blinded randomised controlled trial to compare video demonstration or telephone conversation with a radiographer versus routine intervention. Radiography 2018, 24, 122–129. [Google Scholar] [CrossRef]
- Jöreskog, K.G.; Goldberger, A.S. Estimation of a model with multiple indicators and multiple causes of a single latent variable. J. Am. Stat. Assoc. 1975, 40, 631–639. [Google Scholar] [CrossRef]
- Sociedade Portuguesa de Ginecologia. Consenso Nacional Sobre Menopausa 2021; Sociedade Portuguesa de Ginecologia: Coimbra, Portugal, 2021; Available online: https://spginecologia.pt/wp-content/uploads/2021/10/Consenso-Nacional-Menopausa-2021.pdf (accessed on 6 May 2023).
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Pais-Ribeiro, J.L.; Honrado, A.; Leal, I. Contribuição para o estudo da adaptação portuguesa das Escalas de Ansiedade, Depressão e Stress (EADS) de 21 itens de Lovibond e Lovibond. Psicol. Saúde Doenças 2004, 5, 229–239. [Google Scholar]
- Jöreskog, K.G. Structural Equation Modeling with Ordinal Variables Using LISREL. 2005. Available online: https://ssicentral.com/wp-content/uploads/2021/04/lis_ordinal.pdf (accessed on 3 March 2021).
- Satorra, A.; Bentler, P.M. Corrections to test statistics and standard erros in covariance structure analysis. In Latente Variable Analysis; von Eye, A., Clogg, C.C., Eds.; SAGE: Newcastle upon Tyne, UK, 1994; pp. 399–419. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 2002. [Google Scholar] [CrossRef]
- Munn, Z.; Pearson, A.; Jordan, Z.; Murphy, F.; Pilkington, D.; Anderson, A. Patient Anxiety and Satisfaction in a Magnetic Resonance Imaging Department: Initial Results from an Action Research Study. J. Med. Imaging Radiat. Sci. 2015, 46, 23–29. [Google Scholar] [CrossRef]
- McLean, C.P.; Anderson, E.R. Brave men and timid women? A review of the gender differences in fear and anxiety. Clin. Psychol. Rev. 2009, 29, 496–505. [Google Scholar] [CrossRef] [PubMed]
- Meyers-Levy, J.; Loken, B. Revisiting gender differences: What we know and what lies ahead. J. Consum. Psychol. 2015, 25, 129–149. [Google Scholar] [CrossRef]
- Dewey, R.S.; Ward, C.; Junor, A.; Horobin, A. Talk to us! Communication is a key factor in improving the comfort of MRI research participants. Health Expect. 2021, 24, 1137–1144. [Google Scholar] [CrossRef] [PubMed]
- Stogiannos, N. Reducing patient’s psychological stress. A guide for MR technologists. Hell. J. Radiol. 2019, 4, 26–30. [Google Scholar] [CrossRef]
- Lang, E.V.; Ward, C.; Laser, E. Effect of team training on patients’ ability to complete MRI examinations. Acad. Radiol. 2010, 17, 18–23. [Google Scholar] [CrossRef]
- Protheroe, J.; Whittle, R.; Bartlam, B.; Estacio, E.V.; Clark, L.; Kurth, J. Health literacy, associated lifestyle and demographic factors in adult population of an English city: A cross-sectional survey. Health Expect. 2017, 20, 112–119. [Google Scholar] [CrossRef]
- Beauchamp, A.; Buchbinder, R.; Dodson, S.; Batterham, R.W.; Elsworth, G.R.; McPhee, C.; Sparkes, L.; Hawkins, M.; Osborne, R.H. Distribution of health literacy strengths and weaknesses across socio-demographic groups: A cross-sectional survey using the Health Literacy Questionnaire (HLQ). BMC Public Health 2015, 15, 678. [Google Scholar] [CrossRef]
- Tsai, T.I.; Yu, W.R.; Lee, S.D. Is health literacy associated with greater medical care trust? Int. J. Qual. Health Care 2018, 30, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Hyde, L.L.; JMackenzie, L.; Boyes, A.W.; Symonds, M.; Brown, S.; Sanson-Fisher, R. Medical Imaging Outpatients’ Experiences With Receiving Information Required for Informed Consent and Preparation: A Cross-Sectional Study. J. Patient Exp. 2018, 5, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Wagenmakers, E.J.; Marsman, M.; Jamil, T.; Ly, A.; Verhagen, J.; Love, J.; Selker, R.; Gronau, Q.F.; Šmíra, M.; Epskamp, S.; et al. Bayesian inference for psychology. Part I: Theoretical advantages and practical ramifications. Psychon. Bull. Rev. 2018, 25, 35–57. [Google Scholar] [CrossRef]
- Wagenmakers, E.J.; Love, J.; Marsman, M.; Jamil, T.; Ly, A.; Verhagen, J.; Selker, R.; Gronau, Q.F.; Dropmann, D.; Boutin, B.; et al. Bayesian inference for psychology. Part II: Example applications with JASP. Psychon. Bull. Rev. 2018, 25, 58–76. [Google Scholar] [CrossRef] [PubMed]
- Bayes Like A Baws: Interpreting Bayesian Repeated Measures [Webpage on the Internet]. 2017. Available online: https://www.cogsci.nl/blog/interpreting-bayesian-repeated-measures-in-jasp (accessed on 6 October 2021).
- Asante, S.; Acheampong, F. Patients’ knowledge, perception, and experience during magnetic resonance imaging in Ghana: A single centre study. Radiography 2021, 27, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Lubetkin, E.I.; Zabor, E.C.; Isaac, K.; Brennessel, D.; Kemeny, M.M.; Hay, J.L. Health literacy, information seeking, and trust in information in Haitians. Am. J. Health Behav. 2015, 39, 441–450. [Google Scholar] [CrossRef]
- Madl, J.; Janka, R.; Bay, S.; Rohleder, N. MRI as a Stressor: The Psychological and Physiological Response of Patients to MRI, Influencing Factors, and Consequences. J. Am. Coll. Radiol. 2022, 19, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Borem, L.M.A.; Figueiredo, M.F.S.; Silveira, M.F.; Neto, J.F.R. The knowledge about diagnostic imaging methods among primary care and medical emergency physicians. Radiol. Bras. 2013, 46, 341–345. [Google Scholar] [CrossRef]
- Tugwell-Allsup, J.; Pritchard, A.W. The experience of patients participating in a small randomised control trial that explored two different interventions to reduce anxiety prior to an MRI scan. Radiography 2018, 24, 130–136. [Google Scholar] [CrossRef]
- Carlsson, S.; Carlsson, E. ‘The situation and the uncertainty about the coming result scared me but interaction with the radiographers helped me through’: A qualitative study on patients’ experiences of magnetic resonance imaging examinations. J. Clin. Nurs. 2013, 22, 3225–3234. [Google Scholar] [CrossRef]
- Graffigna, G. (Ed.) Promoting Patient Engagement and Participation for Effective Healthcare Reform; Medical Information Science Reference; IGI Global: Hershey, PA, USA, 2016. [Google Scholar]
- Head, M.L.; Holman, L.; Lanfear, R.; Kahn, A.T.; Jennions, M.D. The extent and consequences of p-hacking in science. PLoS Biol. 2015, 13, e1002106. [Google Scholar] [CrossRef] [PubMed]
- Shadish, W.R.; Cook, T.D.; Campbell, D.T. Designs for Generalized Causal Inference; Houghton Mifflin Company: Boston, MA, USA, 2002. [Google Scholar]
- Paulhus, D.L. Socially desirable responding on self-reports. In Encyclopedia of Personality and Individual Differences; Zeigler-Hill, V., Schackelford, T.K., Eds.; Springer: Cham, Switzerland, 2017; pp. 1–5. [Google Scholar] [CrossRef]
- Paunonen, S.V.; LeBel, E.P. Socially desirable responding and its elusive effects on the validity of personality assessments. J. Pers. Soc. Psychol. 2012, 103, 158–175. [Google Scholar] [CrossRef] [PubMed]
- Diniz, A.M.; Amado, N. Procedures for successful data collection through psychological tests in the elderly. Psicol. Reflexão Crítica 2014, 27, 491–497. [Google Scholar] [CrossRef]
- Morrow, M.; Waters, J.; Marris, E. MRI for breast cancer screening, diagnosis, and treatment. Lancet 2011, 378, 1804–1811. [Google Scholar] [CrossRef] [PubMed]
- Oztek, M.A.; Brunnquell, C.L.; Hoff, M.N.; Boulter, D.J.; Mossa-Basha, M.; Beauchamp, L.H.; Haynor, D.L.; Nguyen, X.V. Practical Considerations for Radiologists in Implementing a Patient-friendly MRI Experience. Top. Magn. Reason. Imaging 2020, 29, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, C.J. An effect size primer: A guide for clinicians and researchers. Prof. Psychol. Res. Pract. 2009, 40, 532–538. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; SAGE Publications: New York, NY, USA, 2018. [Google Scholar]
| n | % | |
|---|---|---|
| Age | ||
| 18–44 | 46 | 22.55 |
| 45–64 | 98 | 48.04 |
| ≥65 | 60 | 29.41 |
| Education level | ||
| Low (up to 4 years completed) a | 84 | 41.18 |
| No education | 8 | 3.92 |
| High (at least 5 years completed) | 120 | 58.82 |
| Body part examined | ||
| Head | 64 | 31.37 |
| Musculoskeletal | 36 | 17.64 |
| Abdominal | 37 | 18.14 |
| Pelvic | 37 | 18.14 |
| Breast | 30 | 14.71 |
| Item | β | R2 |
|---|---|---|
| 1. I found it hard to wind down | 0.947 | 0.897 |
| 2. I was aware of dryness of my mouth | 0.659 | 0.434 |
| 3. I experienced breathing difficulty | 0.810 | 0.656 |
| 4. I tended to over-react to situations | 0.905 | 0.819 |
| 5. I experienced trembling (e.g., in the hands) | 0.794 | 0.630 |
| 6. I felt that I was using a lot of nervous energy | 0.908 | 0.824 |
| 7. I was worried about situations in which I might panic and make a fool of myself | 0.861 | 0.741 |
| 8. I found myself getting agitated | 0.930 | 0.865 |
| 9. I found it difficult to relax | 0.942 | 0.887 |
| 10. I was intolerant of anything that kept me from getting on with what I was doing | 0.881 | 0.776 |
| 11. I felt I was close to panic | 0.951 | 0.904 |
| 12. I felt that I was rather touchy | 0.868 | 0.753 |
| 13. I was aware of the action of my heart in the absence of physical exertion | 0.824 | 0.679 |
| 14. I felt scared without any good reason | 0.970 | 0.941 |
| AVE | 0.882 | |
| CR | 0.990 |
| n | % | |
|---|---|---|
| Age | ||
| 18–44 | 55 | 22.72 |
| 45–64 | 117 | 48.35 |
| ≥65 | 70 | 28.93 |
| Education level | ||
| Low (up to 4 years completed) a | 106 | 43.80 |
| No education | 8 | 3.31 |
| High (at least 5 years completed) | 136 | 56.20 |
| Factors | P(incl) | P(excl) | P(incl|data) | P(excl|data) | BF10 |
|---|---|---|---|---|---|
| PA | 0.263 | 0.263 | 0.001 | 0.003 | 0.347 |
| Education level | 0.263 | 0.263 | 7.070 × 10−4 | 0.005 | 0.151 |
| PA × education level | 0.263 | 0.263 | 0.912 | 4.507 × 10−4 | 2022.938 |
| Information | 0.263 | 0.263 | 0.004 | 0.025 | 0.170 |
| PA × information | 0.263 | 0.263 | 0.886 | 0.007 | 135.718 |
| Education level × information | 0.263 | 0.263 | 0.383 | 0.508 | 0.755 |
| PA × education level × information | 0.053 | 0.053 | 0.083 | 0.380 | 0.217 |
| Factors | M of PA | Analysis of Effects | |||
|---|---|---|---|---|---|
| Pre-MRI | Post-MRI | P(incl) | P(incl|data) | BF10 | |
| Received information | 6.84 | 3.30 | 0.50 | 0.99 | 81.81 |
| Did not receive information | 5.24 | 5.53 | 0.5 | 0.12 | 0.13 |
| Low education | 6.95 | 3.29 | 0.50 | 0.99 | 88.50 |
| High education | 4.86 | 5.94 | 0.50 | 0.26 | 0.35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farinha, M.N.; Semedo, C.S.; Diniz, A.M.; Herédia, V. Individual and Contextual Variables as Predictors of MRI-Related Perceived Anxiety. Behav. Sci. 2023, 13, 458. https://doi.org/10.3390/bs13060458
Farinha MN, Semedo CS, Diniz AM, Herédia V. Individual and Contextual Variables as Predictors of MRI-Related Perceived Anxiety. Behavioral Sciences. 2023; 13(6):458. https://doi.org/10.3390/bs13060458
Chicago/Turabian StyleFarinha, Margarida N., Carla S. Semedo, António M. Diniz, and Vasco Herédia. 2023. "Individual and Contextual Variables as Predictors of MRI-Related Perceived Anxiety" Behavioral Sciences 13, no. 6: 458. https://doi.org/10.3390/bs13060458
APA StyleFarinha, M. N., Semedo, C. S., Diniz, A. M., & Herédia, V. (2023). Individual and Contextual Variables as Predictors of MRI-Related Perceived Anxiety. Behavioral Sciences, 13(6), 458. https://doi.org/10.3390/bs13060458





