Relationship Dysfunction in Couples When One Partner Is Diagnosed with Borderline Personality Disorder: Findings from a Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measurements
2.3.1. Primary Outcomes
2.3.2. Secondary Outcomes
2.4. Sampling, Processing, and Analysis of Saliva Samples
2.5. Data Analysis
2.6. Sample Characteristics
3. Results
3.1. Predispositioning Factors
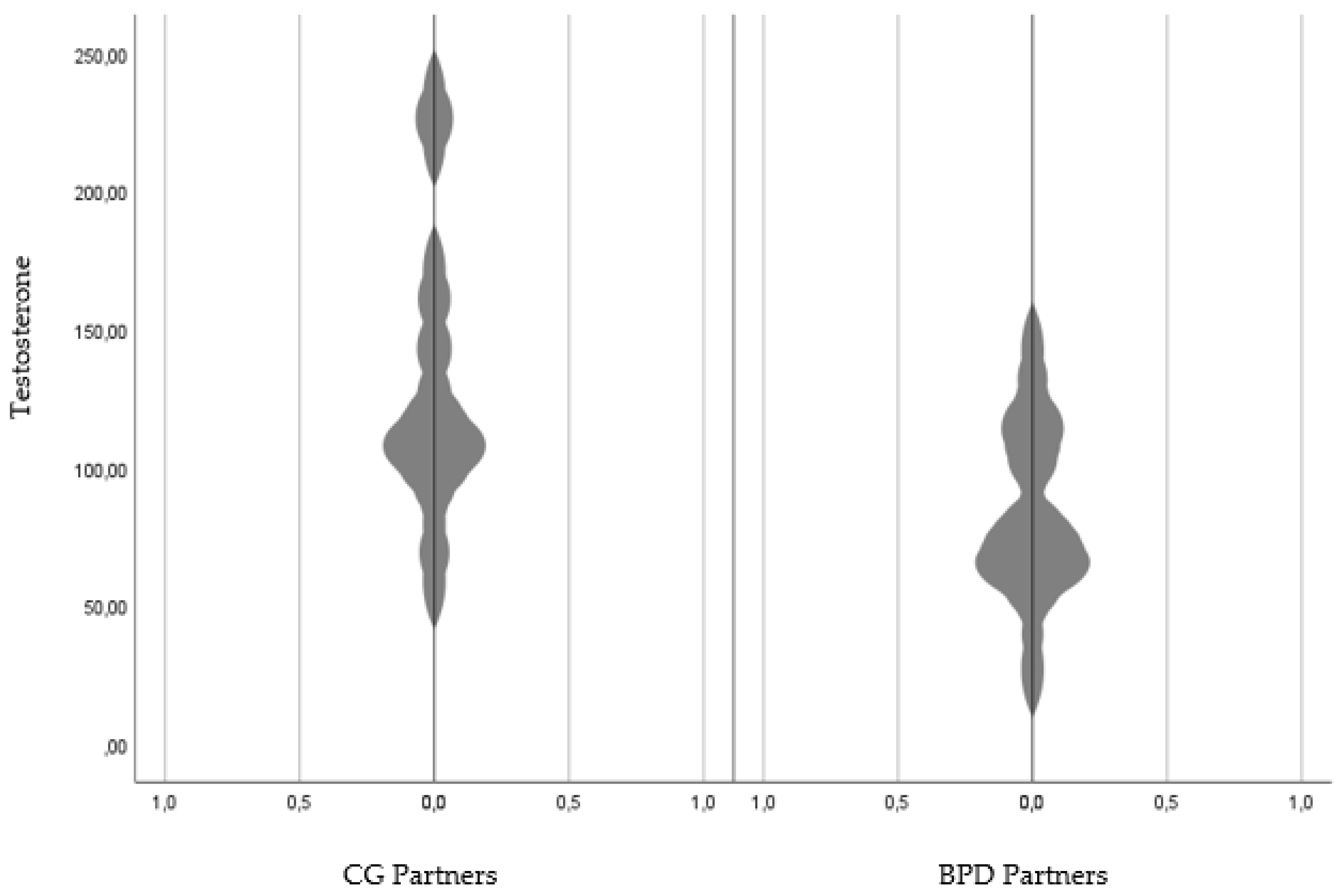
3.2. Hormone Levels in Saliva
3.3. Relationship Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tomko, R.L.; Trull, T.J.; Wood, P.K.; Sher, K.J. Characteristics of borderline personality disorder in a community sample: Comorbidity, treatment utilization, and general functioning. J. Personal. Disord. 2014, 28, 734–750. [Google Scholar] [CrossRef] [PubMed]
- Ellison, W.D.; Rosenstein, L.K.; Morgan, T.A.; Zimmerman, M. Community and Clinical Epidemiology of Borderline Personality Disorder. Psychiatr. Clin. N. Am. 2018, 41, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Bodem, K.; Vogel, R.; Walker, J.; Kröger, C. Health care costs of borderline personality disorder and matched controls with major depressive disorder: A comparative study based on anonymized claims data. Eur. J. Health Econ. 2017, 18, 1125–1135. [Google Scholar] [CrossRef] [PubMed]
- Hastrup, L.H.; Jennum, P.; Ibsen, R.; Kjellberg, J.; Simonsen, E. Societal costs of Borderline Personality Disorders: A matched-controlled nationwide study of patients and spouses. Acta Psychiatr. Scand. 2019, 140, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Stepp, S.D.; Scott, L.N.; Morse, J.Q.; Nolf, K.A.; Hallquist, M.N.; Pilkonis, P.A. Emotion dysregulation as a maintenance factor of borderline personality disorder features. Compr. Psychiatry 2014, 55, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, J.G.; Lyons-Ruth, K. BPD’s interpersonal hypersensitivity phenotype: A gene-environment- developmental model. J. Personal. Disord. 2008, 22, 22–41. [Google Scholar] [CrossRef]
- Smith, M.; South, S. Romantic attachment style and borderline personality pathology: A meta-analysis. Clin. Psychol. Rev. 2020, 75, 101781. [Google Scholar] [CrossRef]
- Dixon-Gordon, K.L.; Turner, B.J.; Zachary Rosenthal, M.; Chapman, A.L. Emotion Regulation in Borderline Personality Disorder: An Experimental Investigation of the Effects of Instructed Acceptance and Suppression. Behav. Ther. 2017, 48, 750–764. [Google Scholar] [CrossRef]
- Miano, A.; Fertuck, E.A.; Roepke, S.; Dziobek, I. Romantic Relationship Dysfunction in Borderline Personality Disorder-A Naturalistic Approach to Trustworthiness Perception. Personal. Disord. Theory Res. Treat. 2017, 8, 281–286. [Google Scholar] [CrossRef]
- Trull, T.J.; Solhan, M.B.; Tragesser, S.L.; Jahng, S.; Wood, P.K.; Piasecki, T.M.; Watson, D. Affective Instability: Measuring a Core Feature of Borderline Personality Disorder with Ecological Momentary Assessment. J. Abnorm. Psychol. 2008, 117, 647–661. [Google Scholar] [CrossRef]
- Van Zutphen, L.; Siep, N.; Jacob, G.A.; Goebel, R.; Arntz, A. Emotional sensitivity, emotion regulation and impulsivity in borderline personality disorder: A critical review of fMRI studies. Neurosci. Biobehav. Rev. 2015, 51, 64–76. [Google Scholar] [CrossRef]
- Daley, S.E.; Burge, D.; Hammen, C. Borderline personality disorder symptoms as predictors of 4-year romantic relationship dysfunction in young women: Addressing issues of specificity. J. Abnorm. Psychol. 2000, 109, 451–460. Available online: http://doi.apa.org/getdoi.cfm?doi=10.1037/0021-843X.109.3.451 (accessed on 1 January 2020). [CrossRef] [PubMed]
- Salzer, S.; Streeck, U.; Jaeger, U.; Masuhr, O.; Warwas, J.; Leichsenring, F.; Leibing, E. Patterns of Interpersonal Problems in Borderline Personality Disorder. J. Nerv. Ment. Dis. 2013, 201, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Bartholomew, K.; Horowitz, L.M. Attachment styles among young adults. J. Personal. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef]
- Collins, N.L.; Feeney, B.C. Working Models of Attachment Shape Perceptions of Social Support: Evidence from Experimental and Observational Studies. J. Personal. Soc. Psychol. 2004, 87, 363–383. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.L.; Feeney, B.C. A safe haven: An attachment theory perspective on support seeking and caregiving in intimate relationships. J. Personal. Soc. Psychol. 2000, 78, 1053–1073. [Google Scholar] [CrossRef] [PubMed]
- Levy, K.N.; Meehan, K.B.; Weber, M.; Reynoso, J.; Clarkin, J.F. Attachment and borderline personality disorder: Implications for psychotherapy. Psychopathology 2005, 38, 64–74. [Google Scholar] [CrossRef]
- Ball, J.S.; Links, P.S. Borderline personality disorder and childhood trauma: Evidence for a causal relationship. Curr. Psychiatry Rep. 2009, 11, 63–68. [Google Scholar] [CrossRef]
- Ibrahim, J.; Cosgrave, N.; Woolgar, M. Childhood maltreatment and its link to borderline personality disorder features in children: A systematic review approach. Clin. Child Psychol. Psychiatry 2018, 23, 57–76. [Google Scholar] [CrossRef]
- Infurna, M.R.; Brunner, R.; Holz, B.; Parzer, P.; Giannone, F.; Reichl, C.; Fischer, G.; Resch, F.; Kaess, M. The specific role of childhood abuse, parental bonding, and family functioning in female adolescents with borderline personality disorder. J. Personal. Disord. 2016, 30, 177–192. [Google Scholar] [CrossRef]
- Bouchard, S.; Sabourin, S. Borderline Personality Disorder and Couple Dysfunctions. Am. J. Psychiatry 2009, 150, 1906–1970. [Google Scholar] [CrossRef] [PubMed]
- Miano, A.; Dziobek, I.; Roepke, S. Characterizing couple dysfunction in borderline personality disorder. J. Personal. Disord. 2020, 34, 181–198. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Gómez, S.; Frías, Á.; Palma, C. Romantic Relationships of People with Borderline Personality: A Narrative Review. Psychopathology 2017, 50, 175–187. [Google Scholar] [CrossRef]
- Roediger, E. Schematherapie: Grundlagen, Modell und Praxis, 3rd ed.; Schattauer: Stuttgart, Germany, 2018. [Google Scholar]
- Young, J.E.; Klosko, J.S.; Weishaar, M.E. Schema Therapy: A Practitioner’s Guide; Guilford Press: New York, NY, USA, 2003. [Google Scholar]
- Drews, E.; Fertuck, E.A.; Koenig, J.; Kaess, M.; Arntz, A. Hypothalamic-pituitary-adrenal axis functioning in borderline personality disorder: A meta-analysis. Neurosci. Biobehav. Rev. 2019, 96, 316–334. [Google Scholar] [CrossRef]
- Kuhlmann, A.; Bertsch, K.; Schmidinger, I.; Thomann, P.A.; Herpertz, S.C. Morphometric differences in central stress-regulating structures between women with and without borderline personality disorder. J. Psychiatry Neurosci. 2013, 38, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, D.J.; Choi-Kain, L.W. The hypothalamic-pituitary-adrenal axis in borderline personality disorder: A review. Harv. Rev. Psychiatry 2009, 17, 167–183. [Google Scholar] [CrossRef] [PubMed]
- Bortolla, R.; Spada, G.E.; Galli, M.; Visitini, R.; Talè, C.; Maffei, C. Psychophysiological aspects of Borderline Personality Disorder reactivity to interpersonal stimuli: Associations to components of childhood abuse. Mediterr. J. Clin. Psychol. 2022, 10. [Google Scholar] [CrossRef]
- Kröner, J.; Schaitz, C.; Maier, A.; Connemann, B.; Sosic-Vasic, Z. Endokrinologische Korrelate der Borderline-Persönlichkeitsstörung TT—Association between interpersonal or social-evaluative stress and borderline-personality disorder in the context of endocrinological findings. Nervenheilkunde 2018, 37, 891–896. [Google Scholar] [CrossRef]
- Cackowski, S.; Reitz, A.C.; Ende, G.; Kleindienst, N.; Bohus, M.; Schmahl, C.; Krause-Utz, A. Impact of stress on different components of impulsivity in borderline personality disorder. Psychol. Med. 2014, 44, 3329–3340. [Google Scholar] [CrossRef]
- Deckers, J.W.M.; Lobbestael, J.; van Wingen, G.A.; Kessels, R.P.C.; Arntz, A.; Egger, J.I.M. The influence of stress on social cognition in patients with borderline personality disorder. Psychoneuroendocrinology 2015, 52, 119–129. [Google Scholar] [CrossRef]
- Greeff, A.P.; Bruyne, T.d. Conflict management style and marital satisfaction. J. Sex Marital. Ther. 2000, 26, 321–334. [Google Scholar] [PubMed]
- Rusbult, C.E.; Buunk, B.P. Commitment Processes in Close Relationships: An Interdependence Analysis. J. Soc. Pers. Relatsh. 1993, 10, 175–204. [Google Scholar] [CrossRef]
- Links, P.S.; Heslegrave, R.J. Prospective Studies of Outcome: Understanding Mechanisms of Change in Patients with Borderline Personality Disorder; Elsevier Science: Amsterdam, The Netherlands, 2000; Volume 23. [Google Scholar]
- Paris, J.; Braverman, S. Successful and unsuccessful marriages in borderline patients. J. Am. Acad. Psychoanal. 1995, 23, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Bouchard, S.; Sabourin, S.; Lussier, Y.; Villeneuve, E. Relationship quality and stability in couples when one partner suffers from borderline personality disorder. J. Marital. Fam. Ther. 2009, 35, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Porcerelli, J.H.; Cogan, R.; Hibbard, S. Personality characteristics of partner violent men: A Q-sort approach. J. Personal. Disord. 2004, 18, 151–162. [Google Scholar] [CrossRef]
- Christensen, A.; Shenk, J.L. Communication Conflict and Psychological Distance in Nondistressed Clinic and Divorcing Couples. J. Consult. Clin. Psychol. 1991, 59, 458–463. [Google Scholar] [CrossRef]
- Lawson, D.M.; Brossart, D.F. Interpersonal Problems and Personality Features as Mediators between Attachment and Intimate Partner Violence. Violence Vict. 2013, 28, 414–428. [Google Scholar] [CrossRef]
- Stepp, S.D.; Smith, T.D.; Morse, J.Q.; Hallquist, M.N.; Pilkonis, P.A. Prospective associations among borderline personality disorder symptoms, interpersonal problems, and aggressive behaviors. J. Interpers. Violence 2012, 27, 103–124. [Google Scholar] [CrossRef]
- Brownridge, D.A.; Tyler, K.A. Borderline personality and dating violence among college students: A path analysis. J. Aggress. Maltreatment Trauma 2022, 1–19. [Google Scholar] [CrossRef]
- Dabbs, J.; Hargrove, M.F. Age, testosterone, and behavior among female prison inmates. Psychosom. Med. 1997, 59, 477–480. [Google Scholar] [CrossRef]
- Grotzinger, A.D.; Mann, F.D.; Patterson, M.W.; Tackett, J.L.; Tucker-Drob, E.M.; Harden, K.P. Hair and salivary testosterone, hair cortisol, and externalizing behaviors in adolescents. Psychol. Sci. 2018, 29, 688–699. [Google Scholar] [CrossRef] [PubMed]
- Pajer, K.; Tabbah, R.; Gardner, W.; Rubin, R.T.; Czambel, R.K.; Wang, Y. Adrenal androgen and gonadal hormone levels in adolescent girls with conduct disorder. Psychoneuroendocrinology 2006, 31, 1245–1256. [Google Scholar] [CrossRef] [PubMed]
- Roepke, S.; Ziegenhorn, A.; Kronsbein, J.; Merkl, A.; Bahri, S.; Lange, J.; Lübbert, H.; Schweiger, U.; Heuser, I.; Lammers, C.-H. Incidence of polycystic ovaries and androgen serum levels in women with borderline personality disorder. J. Psychiatr. Res. 2010, 44, 847–852. [Google Scholar] [CrossRef] [PubMed]
- Thomas, N.; Gurvich, C.; Hudaib, A.R.; Gavrilidis, E.; Kulkarni, J. Systematic review and meta-analysis of basal cortisol levels in Borderline Personality Disorder compared to non-psychiatric controls. Psychoneuroendocrinology 2019, 102, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Dettenborn, L.; Kirschbaum, C.; Gao, W.; Spitzer, C.; Roepke, S.; Otte, C.; Wingenfeld, K. Increased hair testosterone but unaltered hair cortisol in female patients with borderline personality disorder. Psychoneuroendocrinology 2016, 71, 176–179. [Google Scholar] [CrossRef]
- Rausch, J.; Gäbel, A.; Nagy, K.; Kleindienst, N.; Herpertz, S.C.; Bertsch, K. Increased testosterone levels and cortisol awakening responses in patients with borderline personality disorder: Gender and trait aggressiveness matter. Psychoneuroendocrinology 2015, 55, 116–127. [Google Scholar] [CrossRef]
- Eck, S.R.; Bangasser, D.A. The effects of early life stress on motivated behaviors: A role for gonadal hormones. Neurosci. Biobehav. Rev. 2020, 119, 86–100. [Google Scholar] [CrossRef]
- Ehrenthal, J.C.; Levy, K.N.; Scott, L.N.; Granger, D.A. Attachment-related regulatory processes moderate the impact of adverse childhood experiences on stress reaction in borderline personality disorder. J. Personal. Disord. 2018, 32, 93–114. [Google Scholar] [CrossRef]
- Martín-Blanco, A.; Ferrer, M.; Soler, J.; Arranz, M.J.; Vega, D.; Calvo, N.; Elices, M.; Sanchez-Mora, C.; García-Martinez, I.; Salazar, J.; et al. The role of hypothalamus–pituitary–adrenal genes and childhood trauma in borderline personality disorder. Eur. Arch. Psychiatry Clin. Neurosci. 2016, 266, 307–316. [Google Scholar] [CrossRef]
- Martín-Blanco, A.; Ferrer, M.; Soler, J.; Salazar, J.; Vega, D.; Andión, O.; Sanchez-Mora, C.; Arranz, M.J.; Ribases, M.; Feliu-Soler, A.; et al. Association between methylation of the glucocorticoid receptor gene, childhood maltreatment, and clinical severity in borderline personality disorder. J. Psychiatr. Res. 2014, 57, 34–40. [Google Scholar] [CrossRef]
- Eisenegger, C.; Haushofer, J.; Fehr, E. The role of testosterone in social interaction. Trends Cogn. Sci. 2011, 15, 263–271. [Google Scholar] [CrossRef]
- Lachkar, J. Narcissistic/Borderline Couple; Taylor and Francis Ltd.: London, UK, 2003. [Google Scholar]
- Wittchen, H.-U.; Zaudig, M.; Fydrich, T. SKID Strukturiertes Klinisches Interview für DSM-IV (SKID I und SKID II). Handanweisung; Hogrefe: Göttingen, Germany, 2021. [Google Scholar]
- Margraf, J.; Cwik, J.C. Mini-DIPS Open Access: Diagnostisches Kurzinterview Bei Psychischen Störungen. 2017. Available online: http://mini-dips.rub.de (accessed on 4 December 2016).
- Hautzinger, M.; Keller, F.; Kühner, C. BDI II Beck Depressions-Inventar Revision Manual; Psychological Corporation: San Antonio, TX, USA, 2006. [Google Scholar]
- Goldberg, D.; Williams, P. General Health Questionnaire (GHQ-12). Hogrefe. 2011. Available online: https://www.testzentrale.de/shop/user-s-guide.html (accessed on 4 December 2016).
- Adam, E.K.; Quinn, M.E.; Tavernier, R.; McQuillan, M.T.; Dahlke, K.A.; Gilbert, K.E. Diurnal cortisol slopes and mental and physical health outcomes: A systematic review and meta-analysis. Psychoneuroendocrinology 2017, 83, 25–41. [Google Scholar] [CrossRef]
- Granger, D.A.; Shirtcliff, E.A.; Waxler, C.Z.; Usher, B.; Dougan, B.K.; Hastings, P. Salivary testosterone diurnal variation and psychopathology in adolescent males and females: Individual differences and developmental effects. Dev. Psychopathol. 2003, 15, 431–449. [Google Scholar] [CrossRef]
- Jeevanandam, S.; Muthu, P.K. 2D: 4D ratio and its implications in medicine. J. Clin. Diagn. Res. 2016, 10, CM01. [Google Scholar] [CrossRef]
- Balodis, I.M.; Wynne-Edwards, K.E.; Olmstead, M.C. The stress-response-dampening effects of placebo. Horm. Behav. 2011, 59, 465–472. [Google Scholar] [CrossRef]
- Ruttle, P.L.; Serbin, L.A.; Stack, D.M.; Schwartzman, A.E.; Shirtcliff, E.A. Adrenocortical attunement in mother-child dyads: Importance of situational and behavioral characteristics. Biol. Psychol. 2011, 88, 104–111. [Google Scholar] [CrossRef]
- Ehrenthal, J.C.; Dinger, U.; Lamla, A.; Funken, B.; Schauenburg, H. Evaluation der deutschsprachigen version des bindungsfragebogens “Experiences in Close Relationships—Revised” (ECR−RD). [Evaluation of the German version of the attachment questionnaire “Experiences in Close Relationships—Revised” (ECR−RD).]. Psychother. Psychosom. Med. Psychol. 2009, 59, 215–223. [Google Scholar] [CrossRef]
- Klinitzke, G.; Romppel, M.; Häuser, W.; Brähler, E.; Glaesmer, H. Die deutsche Version des Childhood Trauma Questionnaire (CTQ)—Psychometrische Eigenschaften in einer bevölkerungsrepräsentativen Stichprobe. PPmP—Psychother. Textperiodcentered Med. Psychol. 2012, 62, 47–51. [Google Scholar] [CrossRef]
- Bernstein, D.; Fink, L. Manual for the Childhood Trauma Questionnaire; The Psychological Corporation: New York, NY, USA, 1998. [Google Scholar]
- Kongerslev, M.T.; Bach, B.; Rossi, G.; Trauelsen, A.M.; Ladegaard, N.; Løkkegaard, S.S.; Bo, S. Psychometric validation of the Childhood Trauma Questionnaire-Short Form (CTQ-SF) in a Danish clinical sample. Child Abus. Negl. 2019, 94, 104026. [Google Scholar] [CrossRef]
- Borkenau, P.; Ostendorf, F. NEO-FFI NEO-Fünf-Faktoren-Inventar nach Costa und McCrae (NEO-FFI) (2., neu Normierte und Vollständig Überarbeitete Auflage); Hogrefe: Göttingen, Germany, 2008. [Google Scholar]
- Hahlweg, K.; Schindler, L.; Revenstorf, D. Partnerschaftsprobleme: Diagnose und Therapie; Springer: Berlin/Heidelberg, Germany, 1982. [Google Scholar]
- Hooley, J.M.; Hahlweg, K. Marital satisfaction and marital communication in German and English couples. Behav. Assess. 1989, 11, 119–133. [Google Scholar]
- Hahlweg, K. Fragebogen zur Partnerschaftsdiagnostik 2016. Available online: https://www.testzentrale.de/shop/fragebogen-zur-partnerschaftsdiagnostik.html (accessed on 5 December 2016).
- Ledermann, T.; Bodenmann, G.; Gagliardi, S.; Charvoz, L.; Verardi, S.; Rossier, J.; Bertoni, A.; Iafrate, R. Psychometrics of the dyadic coping inventory in three language groups. Swiss J. Psychol. 2010, 69, 201–212. [Google Scholar] [CrossRef]
- Cassidy, J.; Shaver, P.R. Handbook of Attachment: Theory, Research, and Clinical Appication; Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Erkoreka González, L.; Zamalloa Díaz, I.; Rodriguez, S.; Muñoz, P.; Mendizabal Larrea, I.; Zamalloa, M.I.; Arrue, A.; Zumarraga Ortiz, M.; González Torres, M.Á. Attachment anxiety as mediator of the relationship between childhood trauma and personality dysfunction in borderline personality disorder. Clin. Psychol. Psychother. 2022, 29, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Allison, C.J.; Bartholomew, K.; Mayseless, O.; Dutton, D.G. Love as a Battlefield: Attachment and Relationship Dynamics in Couples Identified for Male Partner Violence. J. Fam. Issues 2007, 29, 125–150. [Google Scholar] [CrossRef]
- Collins, N.L.; Read, S.J. Adult attachment, working models, and relationship quality in dating couples. J. Personal. Soc. Psychol. 1990, 58, 644–663. [Google Scholar] [CrossRef] [PubMed]
- Fraley, R.C.; Shaver, P.R. Adult romantic attachment: Theoretical developments, emerging controversies, and unanswered questions. Rev. Gen. Psychol. 2000, 4, 132–154. [Google Scholar] [CrossRef]
- Hazan, C.; Shaver, P.R. Attachment as an Organizational Framework for Research on Close Relationships. Psychol. Inq. 1994, 5, 1–22. [Google Scholar] [CrossRef]
- Porter, C.; Palmier-Claus, J.; Branitsky, A.; Mansell, W.; Warwick, H.; Varese, F. Childhood adversity and borderline personality disorder: A meta-analysis. Acta Psychiatr. Scand. 2020, 141, 6–20. [Google Scholar] [CrossRef]
- Schulze, A.; Cloos, L.; Zdravkovic, M.; Lis, S.; Krause-Utz, A. On the interplay of borderline personality features, childhood trauma severity, attachment types, and social support. Bord. Pers. Disord. Emot. Dysregul. 2022, 9, 1–14. [Google Scholar] [CrossRef]
- Godbout, N.; Runtz, M.; MacIntosh, H.; Briere, J. Childhood trauma and couple relationships. Integr. Sci. Pract. 2013, 3, 14–17. [Google Scholar]
- Owen, J.; Quirk, K.; Manthos, M. I get no respect: The relationship between betrayal trauma and romantic relationship functioning. J. Trauma Dissociation 2012, 13, 175–189. [Google Scholar] [CrossRef]
- Thibodeau, M.-È.; Lavoie, F.; Hébert, M.; Blais, M. Pathways linking childhood maltreatment and adolescent sexual risk behaviors: The role of attachment security. J. Sex Res. 2017, 54, 994–1005. [Google Scholar] [CrossRef]
- Yumbul, C.; Cavusoglu, S.; Geyimci, B. The effect of childhood trauma on adult attachment styles, infidelity tendency, romantic jealousy and self-esteem. Procedia-Soc. Behav. Sci. 2010, 5, 1741–1745. [Google Scholar] [CrossRef]
- Clarkin, J.F. Prototypic typology and the Borderline Personality Disorder. J. Abnorm. Psychol. 1983, 92, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Samuel, D.B.; Widiger, T.A. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clin. Psychol. Rev. 2008, 28, 1326–1342. [Google Scholar] [CrossRef]
- Widiger, T.A.; Trull, T.J.; Clarkin, J.F.; Sanderson, C.; Costa, P.T., Jr. A description of the DSM-IV personality disorders with the five-factor model of personality. In Personality Disorders and the Five-Factor Model of Personality, 2nd ed.; American Psychological Association: Washington, DC, USA, 2002; pp. 89–99. [Google Scholar]
- Wilberg, T.; Urnes, Ø.; Friis, S.; Pedersen, G.; Karterud, S. Borderline and Avoidant Personality Disorders and the Five-Factor Model of Personality: A Comparison between DSM-IV Diagnoses and NEO-PI-R; Guilford Publications: New York, NY, USA, 1999; Volume 13. [Google Scholar]
- Towler, A.J.; Stuhlmacher, A.F. Attachment styles, relationship satisfaction, and well-being in working women. J. Soc. Psychol. 2013, 153, 279–298. [Google Scholar] [CrossRef]
- Kirschbaum, C.; Kudielka, B.M.; Gaab, J.; Schommer, N.C.; Hellhammer, D.H. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom. Med. 1999, 61, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Wichmann, S.; Kirschbaum, C.; Böhme, C.; Petrowski, K. Cortisol stress response in post-traumatic stress disorder, panic disorder, and major depressive disorder patients. Psychoneuroendocrinology 2017, 83, 135–141. [Google Scholar] [CrossRef]
- Zorn, J.V.; Schür, R.R.; Boks, M.P.; Kahn, R.S.; Joëls, M.; Vinkers, C.H. Cortisol stress reactivity across psychiatric disorders: A systematic review and meta-analysis. Psychoneuroendocrinology 2017, 77, 25–36. [Google Scholar] [CrossRef]
- Ronay, R.; Carney, D.R. Testosterone’s negative relationship with empathic accuracy and perceived leadership ability. Soc. Psychol. Personal. Sci. 2013, 4, 92–99. [Google Scholar] [CrossRef]
- Fitzpatrick, S.; Liebman, R.E.; Varma, S.; Norouzian, N.; Chafe, D.; Traynor, J.; Goss, S.; Earle, E.; Di Bartolomeo, A.; Latham, M.; et al. Protocol Development of Sage: A Novel Conjoint Intervention for Suicidal and Self-Injuring People with Borderline Personality Disorder and Their Significant Others. Cogn. Behav. Pract. 2023; in press. [Google Scholar] [CrossRef]
| BPD (n = 14) | CG (n = 12) | Statistics | p | |
|---|---|---|---|---|
| Age in years (M/SD) | 25.90 (6.84) | 22.36 (1.95) | t(10.05) = −1.59 | 0.142 |
| BMI in kg/m2 (M/SD) | 27.08 (7.92) | 22.82 (3.54) | t(11.59) = −1.59 | 0.138 |
| Relationship duration 1 | 18.00 (15.02) | 36.64 (20.58) | t(26) = 2.74 | ≤0.01 |
| Level of education | 0/5/5/4 | 0/1/2/9 | X2(2) = 5.06 | 0.08 |
| (no degree/main/middle/high school *) | ||||
| Oral contraception (no/yes) | 7/7 | 4/8 | X2(1) = 1.35 | 0.246 |
| Current smoking (no/yes) | 8/6 | 10/2 | X2(1) = 1.82 | 0.178 |
| BDI-II (M/SD) | 32.64 (12.74) | 1.64 (2.59) | t(26) = −9.26 | <0.001 |
| GHQ-12 (M/SD) | 20.79 (7.44) | 7.57 (3.11) | t(26) = −6.36 | <0.001 |
| SCID-II Personality Disorder (M/SD) 2 | 6.36 (1.82) | 0.64 (1.15) | t(26) = −9.92 | <0.001 |
| Anxious-Avoidant PD | 86% | 7% | ||
| Dependent PD | 57% | 7% | ||
| OCDP | 50% | 21% | ||
| Negativistic PD | 71% | 7% | ||
| Depressive PD | 86% | 0% | ||
| Paranoid PD | 50% | 0% | ||
| Schizotypical PD | 21% | 7% | ||
| Schizoid PD | 43% | 0% | ||
| Histrionic PD | 21% | 0% | ||
| Narcissistic PD | 0% | 0% | ||
| Borderline PD | 100% | 0% | ||
| Antisocial PD | 50% | 14% |
| Partner BPD | Partner CG | Statistics | p | |
|---|---|---|---|---|
| (n = 12) | (n = 12) | |||
| Age in years (M/SD) | 28.88 (10.41) | 26.92 (6.79) | t(18) = −0.51 | 0.12 |
| BMI in kg/m2 (M/SD) | 27.19 (5.97) | 26.05 (6.02) | t(18) = −0.42 | 0.68 |
| Level of school education | 1/2/3/6 | 0/0/6/6 | X2(3) = 4.00 | 0.26 |
| (no degree/main/middle/high school *) | ||||
| Current smoking (no/yes) | 7/5 | 9/3 | X2(1) = 0.750 | 0.39 |
| BDI-II (M/SD) | 4.92 (3.32) | 10.82 (11.86) | t(21) = −1.73 | 0.09 |
| GHQ-12 (M/SD) | 12.09 (9.24) | 9.25 (3.41) | t(21) = −1.04 | 0.31 |
| SCID-II Personality Disorder (M/SD) 1 | 2.00 (1.67) | 1.58 (2.15) | t(21) = −0.52 | 0.61 |
| Anxious-Avoidant PD | 17% | 8% | ||
| Dependent PD | 8% | 0% | ||
| OCDP | 42% | 42% | ||
| Negativistic PD | 17% | 8% | ||
| Depressive PD | 8% | 8% | ||
| Paranoid PD | 25% | 8% | ||
| Schizotypical PD | 8% | 8% | ||
| Schizoid PD | 8% | 8% | ||
| Histrionic PD | 8% | 17% | ||
| Narcissistic PD | 8% | 0% | ||
| Borderline PD | 8% | 0% | ||
| Antisocial PD | 50% | 50% |
| Females | Males | |||||||
|---|---|---|---|---|---|---|---|---|
| BPD | CG | F(df) | p | Partner BPD | Partner CG | F(df) | p | |
| (M/SE) | (M/SE) | ES (95% CI) | (M/SE) | (M/SE) | ES (95% CI) | |||
| Attachment Styles | ||||||||
| Anxiety | 82.86 (3.94) | 35.57 (3.94) | 72.14 (26.1) | <0.001 | 53.36 (5.27) | 38.83 (5.04) | 3.97 (21,1) | ≤0.05 |
| 3.1 (1.97–4.21) | 0.8 (0.05–1.65) | |||||||
| Avoidance | 47.57 (3.89) | 27.14 (3.94) | 13.81 (26.1) | <0.001 | 44.55 (3.77) | 32.25 (3.61) | 5.54 (21,1) | <0.05 |
| 1.4 (0.53–2.18) | 0.9 (0.07–1.80) | |||||||
| Childhood Maltreatment | ||||||||
| Overall CM Load | 104.63 (2.60) | 86.43 (2.60) | 24.46 (26.1) | <0.001 | 96.36 (2.10) | 88.58 (2.01) | 7.15 (21,1) | ≤0.01 |
| 1.8 (0.91–2.69) | 1.0 (0.17–1.93) | |||||||
| Emotional abuse | 21.64 (0.73) | 15.57 (0.73) | 34.63 (26.1) | <0.001 | 19.00 (0.76) | 17.17 (0.73) | 3.05 (21,1) | 0.09 |
| 2.1 (1.20–3.09) | 0.7 (0.16–1.53) | |||||||
| Physical abuse | 18.43 (0.69) | 15.14 (0.69) | 11.43 (26.1) | <0.01 | 16.55 (0.50) | 15.58 (0.48) | 1.92 (21,1) | 0.18 |
| 1.2 (0.42–20.4) | 0.5 (0.29–1.38) | |||||||
| Sexual abuse | 18.79 (0.94) | 14.79 (0.94) | 9.15 (26.1) | <0.01 | 16.46 (0.87) | 14.17 (0.84) | 3.59 (21,1) | 0.07 |
| 1.1 (0.30–1.90) | 0.8 (0.09–1.61) | |||||||
| Emotional neglect | 8.21 (0.58) | 5.07 (0.58) | 14.53 (26.1) | <0.001 | 6.09 (0.44) | 5.58 (0.43) | 0.68 (21,1) | 0.42 |
| 1.4 (0.56–2.22) | 0.3 (−0.5–1.15) | |||||||
| Physical neglect | 12.71 (0.47) | 11.50 (0.47) | 3.35 (26.1) | 0.079 | 13.00 (0.43) | 11.50 (0.41) | 6.31 (21,1) | <0.05 |
| 0.7 (0.10–1.43) | 1.0 (0.12–1.86) | |||||||
| Experience of inconsistency | 13.21 (0.41) | 9.71 (0.41) | 35.72 (26,1) | <0.001 | 12.00 (0.54) | 10.17 (0.52) | 6.02 (21,1) | <0.05 |
| 2.2 (1.23–3.12) | 1.0 (0.10–1.83) | |||||||
| Personality Traits | ||||||||
| Neuroticism | 3.14 (0.18) | 1.40 (0.14) | 60.63 (20.1) | <0.001 | 1.68 (0.19) | 1.03 (0.18) | 6.02 (21,1) | <0.05 |
| 3.4 (2.01–4.72) | 1.0 (0.10–1.84) | |||||||
| Extraversion | 1.47 (0.13) | 2.70 (0.10) | 55.87 (20.1) | <0.001 | 2.06 (0.17) | 2.49 (0.16) | 3.31 (21,1) | 0.08 |
| 2.9 (1.62–4.10) | 0.7 (0.12–1.57) | |||||||
| Openness | 2.67 (0.18) | 2.29 (0.14) | 2.76 (20.1) | 0.113 | 3.02 (0.14) | 2.27 (0.14) | 14.51 (21,1) | <0.001 |
| 0.7 (0.19–1.60) | 1.5 (0.57–2.44) | |||||||
| Conscientiousness | 2.37 (0.20) | 2.95 (0.15) | 5.81 (20.1) | <0.05 | 2.36 (0.17) | 2.76 (0.16) | 2.93 (21,1) | 0.1 |
| 1.0 (0.07–1.92) | 0.7 (0.16–1.53) | |||||||
| Agreeableness | 2.43 (0.20) | 2.95 (0.15) | 4.53 (20.1) | <0.05 | 2.42 (0.15) | 2.53 (0.15) | 0.27 (21,1) | 0.61 |
| 0.9 (0.06–1.76) | 0.2 (−0.63–1.01) | |||||||
| Females | Males | |||||||
|---|---|---|---|---|---|---|---|---|
| BPD (M/SE) | CG (M/SE) | F(df) ES (95% CI) | p | Partner BPD (M/SE) | Partner CG (M/SE) | F(df) ES (95% CI) | p | |
| Partnership Questionnaire | ||||||||
| PFB Sum | 66.00 (3.20) | 76.57 (3.20) | 5.45 (26,1) 0.9 (0.07–1.63) | <0.05 | 66.64 (3.25) | 68.00 (3.11) | 0.09 (21,1) 0.1 (−0.7–0.94) | 0.76 |
| Questionnaire for Assessing Dyadic Coping | ||||||||
| QADC Sum | 89.00 (6.91) | 106.64 (4.13) | 4.81 (17,1) 1.0 (0.08–2.07) | <0.05 | 95.75 (4.35) | 93.75 (3.32) | 0.07 (17,1) 0.1 (−1.05–0.82) | 0.80 |
| Positive Coping | 106.80 (6.72) | 121.00 (4.02) | 3.29 (17,1) 0.9 (0.19–1.94) | 0.087 | 116.43 (3.76) | 112.58 (2.87) | 0.66 (17,1) 0.4 (−0.59–1.29) | 0.43 |
| Negative Coping | 17.80 (1.41) | 14.36 (0.85) | 4.37 (17,1) 0.9 (0.15–1.98) | ≤0.05 | 21.29 (1.84) | 18.83 (1.40) | 1.13 (17,1) 0.5 (−0.43–1.46) | 0.30 |
| Problem List | ||||||||
| PL Sum | 13.83 (1.58) | 6.50 (1.58) | 10.81 (22,1) 1.3 (0.45–2.23) | <0.01 | 14.00 (2.27) | 10.91 (2.18) | 0.96 (21,1) 0.4 (−0.43–1.12) | 0.34 |
| ECR | CTQ | NEO-FFI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Anxiety | Avoidance | EA | PA | SA | EN | PN | EI | Overall | Neuroticism | |
| PL | 0.465 *** | 0.525 *** | 0.405 ** | 0.338 * | 0.069 | 0.073 | 0.256 | 0.327 * | 0.324 * | 0.482 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kroener, J.; Schaitz, C.; Karabatsiakis, A.; Maier, A.; Connemann, B.; Schmied, E.; Sosic-Vasic, Z. Relationship Dysfunction in Couples When One Partner Is Diagnosed with Borderline Personality Disorder: Findings from a Pilot Study. Behav. Sci. 2023, 13, 253. https://doi.org/10.3390/bs13030253
Kroener J, Schaitz C, Karabatsiakis A, Maier A, Connemann B, Schmied E, Sosic-Vasic Z. Relationship Dysfunction in Couples When One Partner Is Diagnosed with Borderline Personality Disorder: Findings from a Pilot Study. Behavioral Sciences. 2023; 13(3):253. https://doi.org/10.3390/bs13030253
Chicago/Turabian StyleKroener, Julia, Caroline Schaitz, Alexander Karabatsiakis, Anna Maier, Bernhard Connemann, Elisa Schmied, and Zrinka Sosic-Vasic. 2023. "Relationship Dysfunction in Couples When One Partner Is Diagnosed with Borderline Personality Disorder: Findings from a Pilot Study" Behavioral Sciences 13, no. 3: 253. https://doi.org/10.3390/bs13030253
APA StyleKroener, J., Schaitz, C., Karabatsiakis, A., Maier, A., Connemann, B., Schmied, E., & Sosic-Vasic, Z. (2023). Relationship Dysfunction in Couples When One Partner Is Diagnosed with Borderline Personality Disorder: Findings from a Pilot Study. Behavioral Sciences, 13(3), 253. https://doi.org/10.3390/bs13030253





