Association between Negative Life Events and Somatic Symptoms: A Mediation Model through Self-Esteem and Depression
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Measurement of Somatic Symptoms
2.3. Measurement of Negative Life Events
2.4. Measurement of Self-Esteem
2.5. Measurement of Depression
2.6. Statistical Methods
3. Results
3.1. Somatic Symptoms of Medical Students
3.2. Statistical Analysis
3.3. Correlation Analysis
3.4. Regression Analysis
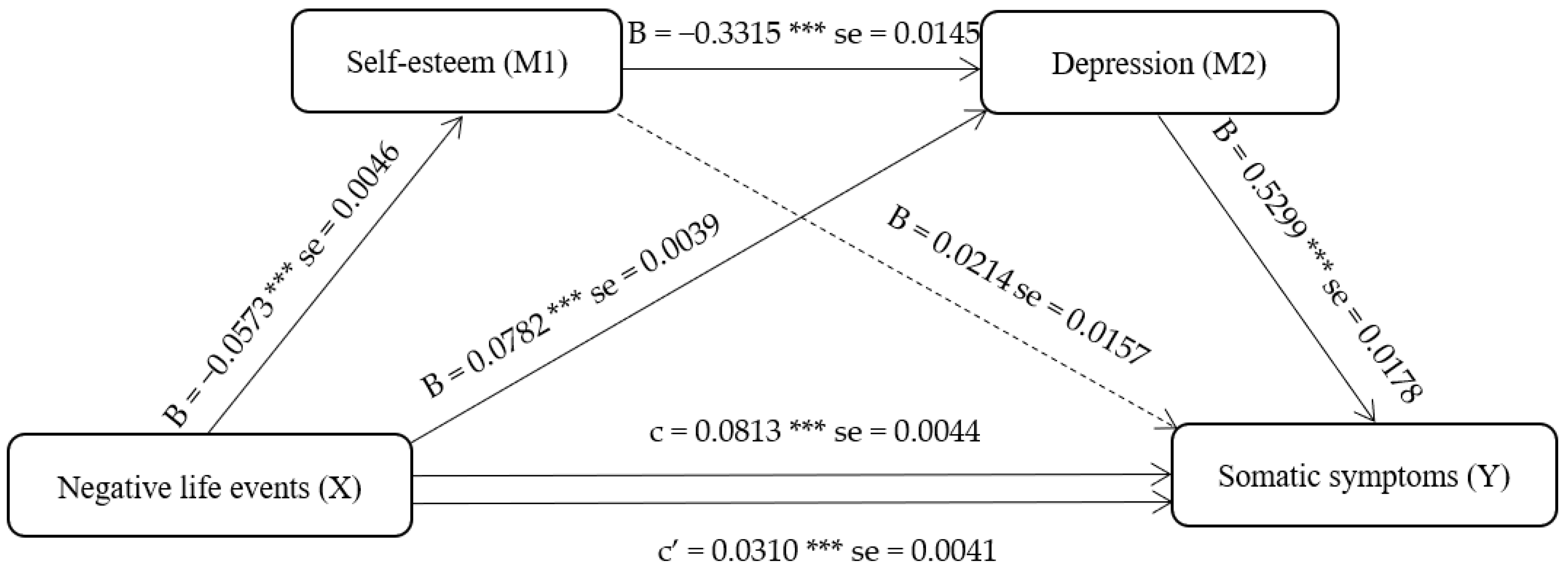
3.5. Mediation Analysis
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Kozlowska, K. Functional somatic symptoms in childhood and adolescence. Curr. Opin. Psychiatry 2013, 26, 485–492. [Google Scholar] [CrossRef]
- Ginsburg, G.S.; Riddle, M.A.; Davies, M. Somatic symptoms in children and adolescents with anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 1179–1187. [Google Scholar] [CrossRef]
- van Geelen, S.M.; Rydelius, P.A.; Hagquist, C. Somatic symptoms and psychological concerns in a general adolescent population: Exploring the relevance of DSM-5 somatic symptom disorder. J. Psychosom. Res. 2015, 79, 251–258. [Google Scholar] [CrossRef]
- Zonneveld, L.N.; Sprangers, M.A.; Kooiman, C.G.; van’t Spijker, A.; Busschbach, J.J. Patients with unexplained physical symptoms have poorer quality of life and higher costs than other patient groups: A cross-sectional study on burden. BMC Health Serv. Res. 2013, 13, 1–11. [Google Scholar] [CrossRef]
- Joustra, M.L.; Janssens, K.A.; Bültmann, U.; Rosmalen, J.G. Functional limitations in functional somatic syndromes and well-defined medical diseases. Results from the general population cohort LifeLines. J. Psychosom. Res. 2015, 79, 94–99. [Google Scholar] [CrossRef]
- Dimsdale, J.E.; Creed, F.; Escobar, J.; Sharpe, M.; Wulsin, L.; Barsky, A.; Lee, S.; Irwin, M.R.; Levenson, J. Somatic symptom disorder: An important change in DSM. J. Psychosom. Res. 2013, 75, 223–228. [Google Scholar] [CrossRef]
- Bonvanie, I.J.; Janssens, K.A.; Rosmalen, J.G.; Oldehinkel, A.J. Life events and functional somatic symptoms: A population study in older adolescents. Br. J. Psychol. 2017, 108, 318–333. [Google Scholar] [CrossRef]
- Cairney, J.; Krause, N. Negative life events and age-related decline in mastery: Are older adults more vulnerable to the control-eroding effect of stress? J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2008, 63, S162–S170. [Google Scholar] [CrossRef]
- Avison, W.; Gotlib, I.H. Stress and Mental Health: Contemporary Issues and Prospects for the Future; Springer Science & Business Media: Berlin/Heidelberg, Germany, 1994. [Google Scholar]
- Zhang, Y.; Zhang, J.; Zhu, S.; Du, C.; Zhang, W. Prevalence and predictors of somatic symptoms among child and adolescents with probable posttraumatic stress disorder: A cross-sectional study conducted in 21 primary and secondary schools after an earthquake. PLoS ONE 2015, 10, e0137101. [Google Scholar] [CrossRef]
- Heshmati, R.; Azmoodeh, S.; Caltabiano, M.L. Pathway linking different types of childhood trauma to somatic symptoms in a subclinical sample of female college students: The mediating role of experiential avoidance. J. Nerv. Ment. Dis. 2021, 209, 497–504. [Google Scholar] [CrossRef]
- Haug, T.T.; Mykletun, A.; Dahl, A.A. The association between anxiety, depression, and somatic symptoms in a large population: The HUNT-II study. Psychosom. Med. 2004, 66, 845–851. [Google Scholar] [CrossRef]
- Konno, C.; Suzuki, M.; Osaki, K.A.; Furihata, R.; Takahashi, S.; Kaneita, Y.; Ohida, T.; Uchiyama, M. Depressive symptoms and somatic complaints in Japanese adults. J. Jpn. Soc. Psychosom. Obstet. Gynecol. 2010, 15, 136–228. [Google Scholar]
- Hamamura, T.; Mearns, J. Depression and somatic symptoms in Japanese and American college students: Negative mood regulation expectancies as a personality correlate. Int. J. Psychol. 2019, 54, 351–359. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Ramos, M.A.; Torre, M.; Segal, J.B.; Peluso, M.J.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: A systematic review and meta-analysis. JAMA 2016, 316, 2214–2236. [Google Scholar] [CrossRef]
- Mao, Y.; Zhang, N.; Liu, J.; Zhu, B.; He, R.; Wang, X. A systematic review of depression and anxiety in medical students in China. BMC Med. Educ. 2019, 19, 1–13. [Google Scholar] [CrossRef]
- Rauschenberg, C.; Schulte-Strathaus, J.C.; van Os, J.; Goedhart, M.; Schieveld, J.N.; Reininghaus, U. Negative life events and stress sensitivity in youth’s daily life: An ecological momentary assessment study. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1641–1657. [Google Scholar] [CrossRef]
- Wong, Y.S.; Zulkefly, N.S.; Tan, K.A. Stressful life events and depressive symptoms among adolescents in Malaysia: The mediating role of maladaptive cognitive schema. Int. J. Adolesc. Med. Health 2020, 33, 493–500. [Google Scholar] [CrossRef]
- Stikkelbroek, Y.; Bodden, D.H.; Kleinjan, M.; Reijnders, M.; van Baar, A.L. Adolescent depression and negative life events, the mediating role of cognitive emotion regulation. PLoS ONE 2016, 11, e0161062. [Google Scholar] [CrossRef]
- Harter, S.; Leahy, R.L. The Construction of the Self: A Developmental Perspective. J. Cogn. Psychother. 2001, 15, 383–384. [Google Scholar] [CrossRef]
- Branden, N. The Power of Self-Esteem; Health Communications, Inc.: Deerfield Beach, FL, USA, 2021. [Google Scholar]
- Gao, F.; Yao, Y.; Yao, C.; Xiong, Y.; Ma, H.; Liu, H. The mediating role of resilience and self-esteem between negative life events and positive social adjustment among left-behind adolescents in China: A cross-sectional study. BMC Psychiatry 2019, 19, 1–10. [Google Scholar] [CrossRef]
- Li, W.; Zhang, L.; Liu, B.; Cao, H. The impact of negative interpersonal life events on social adaptation of Chinese college students: Mediator effect of self-esteem. Soc. Behav. Personal. Int. J. 2013, 41, 705–714. [Google Scholar] [CrossRef]
- Aboalshamat, K.; Jawhari, A.; Alotibi, S.; Alzahrani, K.; Al-Mohimeed, H.; Alzahrani, M.; Rashedi, H. Relationship of self-esteem with depression, anxiety, and stress among dental and medical students in Jeddah, Saudi Arabia. J. Int. Med. Dent. 2017, 4, 61–68. [Google Scholar] [CrossRef]
- Wan, Y.; Chen, R.; Wang, S.; Orton, S.; Wang, D.; Zhang, S.; Sun, Y.; Tao, F. Effects of self-esteem on the association between negative life events and suicidal ideation in adolescents. Int. J. Environ. Res. Public Health 2019, 16, 2846. [Google Scholar] [CrossRef]
- Xin, Y.; Li, Q.; Liu, C. Adolescent self-esteem and social adaptation: Chain mediation of peer trust and perceived social support. Soc. Behav. Personal. Int. J. 2019, 47, 1–9. [Google Scholar] [CrossRef]
- Masselink, M.; Van Roekel, E.; Hankin, B.L.; Keijsers, L.; Lodder, G.M.A.; Vanhalst, J.; Verhagen, M.; Young, J.F.; Oldehinkel, A.J. The Longitudinal Association between Self-esteem and Depressive Symptoms in Adolescents: Separating Between-Person Effects from Within-Person Effects. Eur. J. Pers. 2018, 32, 653–671. [Google Scholar] [CrossRef]
- Ranøyen, I.; Stenseng, F.; Klöckner, C.A.; Wallander, J.; Jozefiak, T. Familial aggregation of anxiety and depression in the community: The role of adolescents’ self-esteem and physical activity level (the HUNT Study). BMC Public Health 2015, 15, 1–16. [Google Scholar] [CrossRef]
- Saricali, M.; Satici, S.A.; Satici, B.; Gocet-Tekin, E.; Griffiths, M.D. Fear of COVID-19, mindfulness, humor, and hopelessness: A multiple mediation analysis. Int. J. Ment. Health Addict. 2022, 20, 2151–2164. [Google Scholar] [CrossRef]
- Moroney, E.; Lee, S.S.; Ebbert, A.M.; Luthar, S.S. Digital media use frequency, online behaviors, and risk for negative mental health in adolescents in high-achieving schools. Clin. Child Psychol. Psychiatry 2023, 28, 237–254. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Patient Health Questionnaire Primary Care Study Group and Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Yan, W.; Li, Y.; Sui, N. The relationship between recent stressful life events, personality traits, perceived family functioning and internet addiction among college students. Stress Health 2014, 30, 3–11. [Google Scholar] [CrossRef]
- Tang, J.; Yang, W.; Ahmed, N.I.; Ma, Y.; Liu, H.Y.; Wang, J.J.; Wang, P.X.; Du, Y.K.; Yu, Y.Z. Stressful Life Events as a Predictor for Nonsuicidal Self-Injury in Southern Chinese Adolescence. Medicine 2016, 95, e2637. [Google Scholar] [CrossRef]
- Rosenberg, M. Society and the Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 2015. [Google Scholar]
- Rhee, H.; Miles, M.S.; Halpern, C.T.; Holditch-Davis, D. Prevalence of recurrent physical symptoms in US adolescents. Pediatr. Nurs. 2005, 31, 314. [Google Scholar]
- Ibrayeva, Z.; Aldyngurov, D.; Myssayev, A.; Meirmanov, S.; Zhanaspayev, M.; Khismetova, Z.; Muzdubayeva, Z.; Smail, E.; Yurkovskaya, O.; Pivina, L.; et al. Depression, anxiety and somatic distress in domestic and international undergraduate medical students in Kazakhstan. Iran. J. Public Health 2018, 47, 919. [Google Scholar]
- Kapfhammer, H.P. Somatic symptoms in depression. Dialogues Clin. Neurosci. 2022, 8, 227–239. [Google Scholar] [CrossRef]
- Silverstein, B. Gender differences in the prevalence of somatic versus pure depression: A replication. Am. J. Psychiatry 2002, 159, 1051–1052. [Google Scholar] [CrossRef]
- Tang, W.; Kang, Y.; Xu, J.; Li, T. Associations of suicidality with adverse life events, psychological distress and somatic complaints in a Chinese medical student sample. Community Ment. Health J. 2020, 56, 635–644. [Google Scholar] [CrossRef]
- Won, S.-D.; Lee, S.H.; Kim, S.; Jun, J.Y.; Shin, S.-S. Somatic symptoms as mediating factors between the perceived social support and the health-related quality of life in North Korean defectors. Psychiatry Investig. 2017, 14, 407. [Google Scholar] [CrossRef]
- Horwitz, B.N.; Marceau, K.; Narusyte, J.; Ganiban, J.; Spotts, E.L.; Reiss, D.; Lichtenstein, P.; Neiderhiser, J.M. Parental criticism is an environmental influence on adolescent somatic symptoms. J. Fam. Psychol. 2015, 29, 283. [Google Scholar] [CrossRef]
- Choi, Y.; Choi, S.H.; Yun, J.Y.; Lim, J.A.; Kwon, Y.; Lee, H.Y.; Jang, J.H. The relationship between levels of self-esteem and the development of depression in young adults with mild depressive symptoms. Medicine 2019, 98, e17518. [Google Scholar] [CrossRef]
- Kitselaar, W.M.; Van Der Vaart, R.; Perschl, J.; Numans, M.E.; Evers, A.W. Predictors of Persistent Somatic Symptoms in the General Population: A systematic review of cohort studies. Psychosom. Med. 2023, 85, 71–78. [Google Scholar] [CrossRef]
- Aanes, M.M.; Mittelmark, M.B.; Hetland, J. Interpersonal stress and poor health. Eur. Psychol. 2010, 15, 3–11. [Google Scholar] [CrossRef]
- Huynh, V.W. Ethnic microaggressions and the depressive and somatic symptoms of Latino and Asian American adolescents. J. Youth Adolesc. 2012, 41, 831–846. [Google Scholar] [CrossRef] [PubMed]
- Bernaras, E.; Jaureguizar, J.; Garaigordobil, M. Child and Adolescent Depression: A Review of Theories, Evaluation Instruments, Prevention Programs, and Treatments. Front. Psychol. 2019, 10, 543. [Google Scholar] [CrossRef] [PubMed]
- Kern, M.L.; Waters, L.E.; Adler, A.; White, M.A. A multidimensional approach to measuring well-being in students: Application of the PERMA framework. J. Posit. Psychol. 2015, 10, 262–271. [Google Scholar] [CrossRef]
- Orth, U.; Robins, R.W. Understanding the link between low self-esteem and depression. Curr. Dir. Psychol. Sci. 2013, 22, 455–460. [Google Scholar] [CrossRef]
- Sowislo, J.F.; Orth, U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol. Bull. 2013, 139, 213. [Google Scholar] [CrossRef]
- Heimpel, S.A.; Wood, J.V.; Marshall, M.A.; Brown, J.D. Do people with low self-esteem really want to feel better? Self-esteem differences in motivation to repair negative moods. J. Personal. Soc. Psychol. 2002, 82, 128. [Google Scholar] [CrossRef]
- LEE, M.S.; Choi, Y.; YOU, J.S. The relationship of somatic symptoms and self-esteem in adolescence. J. Korean NeuroPsychiatric Assoc. 2000, 39, 323–333. [Google Scholar]
- Gao, B.; Zhao, M.; Feng, Z.; Xu, C. The chain mediating role of cognitive styles and alienation between life events and depression among rural left-behind children in poor areas in Southwest China. J. Affect. Disord. 2022, 306, 215–222. [Google Scholar] [CrossRef]
| Somatic Symptoms Level | Number | Percentage (%) |
|---|---|---|
| No somatic symptoms | 999 | 31.03 |
| Mild somatic symptoms | 1261 | 39.17 |
| Moderate somatic symptoms | 777 | 24.14 |
| Severe somatic symptoms | 182 | 5.66 |
| Somatic Symptom | Number | Percentage (%) |
|---|---|---|
| 1. Stomach pain | 1440 | 64.86 |
| 2. Back pain | 1306 | 58.83 |
| 3. Pain in arms, legs, or joints (knees, hips, etc.) | 1289 | 58.06 |
| 4. Menstrual cramps with periods (females only) | 1210 | 54.50 |
| 5. Headaches | 1637 | 73.74 |
| 6. Chest pain | 899 | 40.50 |
| 7. Nausea, gas, or indigestion | 1732 | 78.02 |
| 8. Constipation, loose bowels, or diarrhea | 1875 | 84.46 |
| 9. Shortness of breath | 672 | 30.27 |
| 10. Dizziness | 899 | 40.50 |
| 11. Fainting spells | 208 | 9.37 |
| 12. Feeling tired or having low energy | 1819 | 81.94 |
| 13. Trouble sleeping | 1276 | 57.48 |
| 14. Feeling heart pound or race | 1417 | 63.83 |
| 15. Pain or problems during sexual intercourse | 172 | 7.75 |
| Category | Subcategory | Number (%) | Somatic Symptoms ± SD | t/F | p |
|---|---|---|---|---|---|
| Gender | Male | 1399 (43.46%) | 5.44 ± 4.15 | −19.618 | 0.000 * |
| Female | 1820 (56.54%) | 8.37 ± 4.52 | |||
| Emotional status | Single | 2275 (70.67%) | 7.13 ± 4.42 | 0.699 | 0.485 |
| Not single | 944 (29.33%) | 7.01 ± 4.51 | |||
| Living expenses | <1000 | 294 (9.13%) | 6.52 ± 4.38 | 3.020 | 0.049 * |
| 1000–2000 | 2280 (70.83%) | 7.12 ± 4.36 | |||
| >2000 | 645 (20.04%) | 7.28 ± 4.76 | |||
| One-child | Yes | 2068 (64.24%) | 6.93 ± 4.50 | −2.795 | 0.005 * |
| No | 1151 (35.76%) | 7.39 ± 4.34 | |||
| Religious belief | Yes | 129 (4.01%) | 7.71 ± 4.36 | 1.589 | 0.112 |
| No | 3090 (95.99%) | 7.07 ± 4.45 |
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. Negative life events | 1.000 | |||
| 2. Self-esteem | −0.215 ** | 1.000 | ||
| 3. Depression | 0.389 ** | −0.421 ** | 1.000 | |
| 4. Somatic symptoms | 0.314 ** | −0.218 ** | 0.548 ** | 1.000 |
| Mean | 28.350 | 29.690 | 3.720 | 7.100 |
| SD | 17.116 | 4.570 | 4.298 | 4.450 |
| Negative Life Events | B | SE | β | t | p |
|---|---|---|---|---|---|
| Punishment | 0.194 | 0.029 | 0.157 | 6.596 | <0.001 |
| Personal loss | 0.231 | 0.028 | 0.189 | 8.225 | <0.001 |
| Interpersonal pressure | 0.286 | 0.029 | 0.256 | 9.991 | <0.001 |
| Learning pressure | 0.052 | 0.026 | 0.053 | 1.965 | 0.05 |
| Health adaptation | −0.263 | 0.025 | −0.271 | −10.559 | <0.001 |
| Effect | Product of Coefficients | Boot 95% CI | ||
|---|---|---|---|---|
| Point Estimate | Boot SE | Lower CI | Upper CI | |
| Direct effect: X→Y | 0.0310 | 0.0041 | 0.0229 | 0.0391 |
| Indirect effect 1: X→M1→Y | −0.0012 | 0.0009 | −0.0030 | 0.0006 |
| Indirect effect 2: X→M1→M2→Y | 0.0101 | 0.0012 | 0.0079 | 0.0125 |
| Indirect effect 3: X→M2→Y | 0.0414 | 0.0027 | 0.0363 | 0.0467 |
| Total effect | 0.0813 | 0.0044 | 0.0727 | 0.0898 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lv, S.; Chang, T.; Na, S.; Lu, L.; Zhao, E. Association between Negative Life Events and Somatic Symptoms: A Mediation Model through Self-Esteem and Depression. Behav. Sci. 2023, 13, 243. https://doi.org/10.3390/bs13030243
Lv S, Chang T, Na S, Lu L, Zhao E. Association between Negative Life Events and Somatic Symptoms: A Mediation Model through Self-Esteem and Depression. Behavioral Sciences. 2023; 13(3):243. https://doi.org/10.3390/bs13030243
Chicago/Turabian StyleLv, Sijia, Tong Chang, Siyu Na, Lei Lu, and Erying Zhao. 2023. "Association between Negative Life Events and Somatic Symptoms: A Mediation Model through Self-Esteem and Depression" Behavioral Sciences 13, no. 3: 243. https://doi.org/10.3390/bs13030243
APA StyleLv, S., Chang, T., Na, S., Lu, L., & Zhao, E. (2023). Association between Negative Life Events and Somatic Symptoms: A Mediation Model through Self-Esteem and Depression. Behavioral Sciences, 13(3), 243. https://doi.org/10.3390/bs13030243





