Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China’s Xizang Region: The Mediating Effect of Cognitive Emotion Regulation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sleep Quality
2.3. Cognitive Emotion Regulation
2.4. Symptoms of Anxiety
2.5. Depression Symptoms
2.6. Other Variables
2.7. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Correlation Analysis
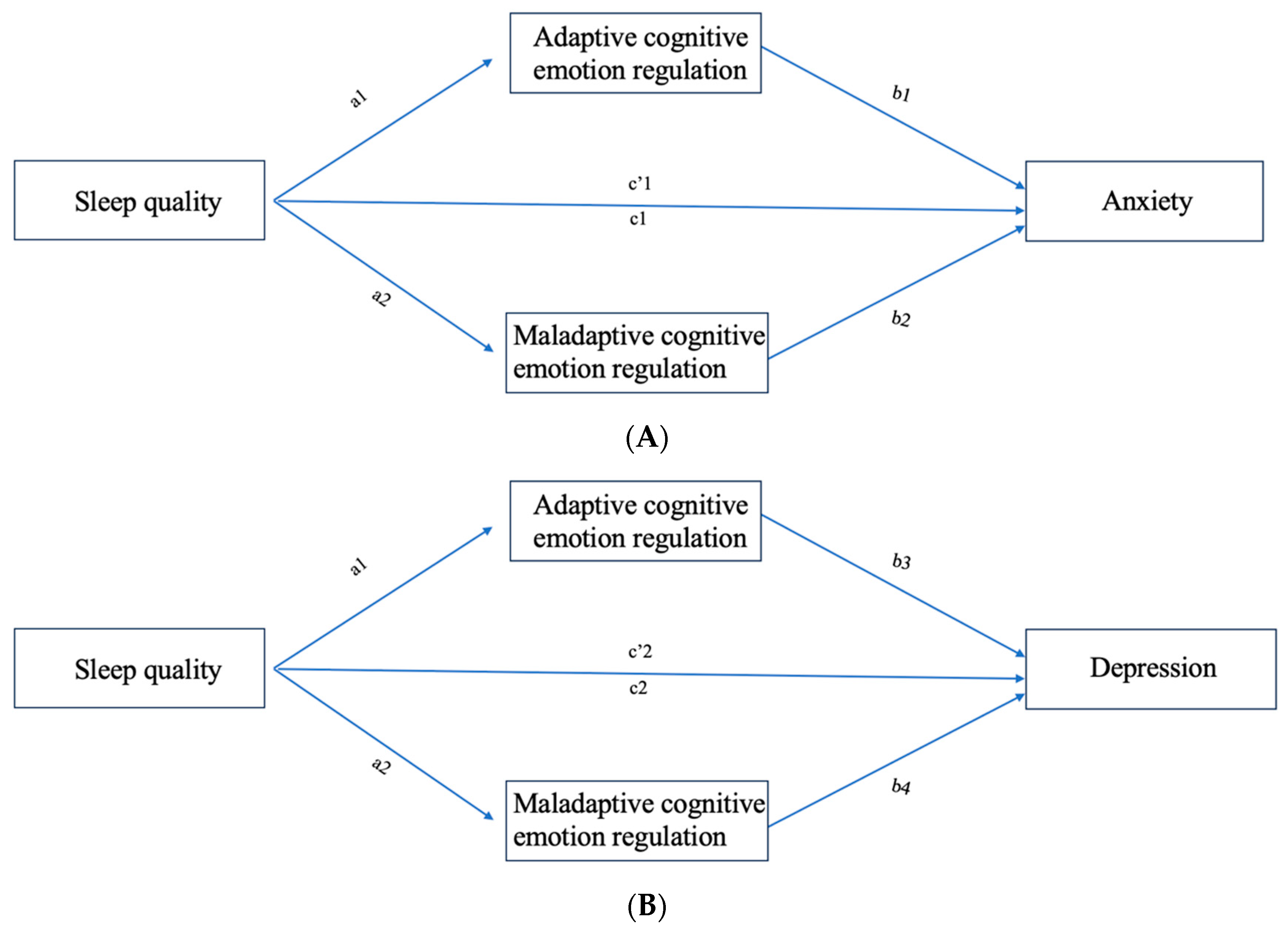
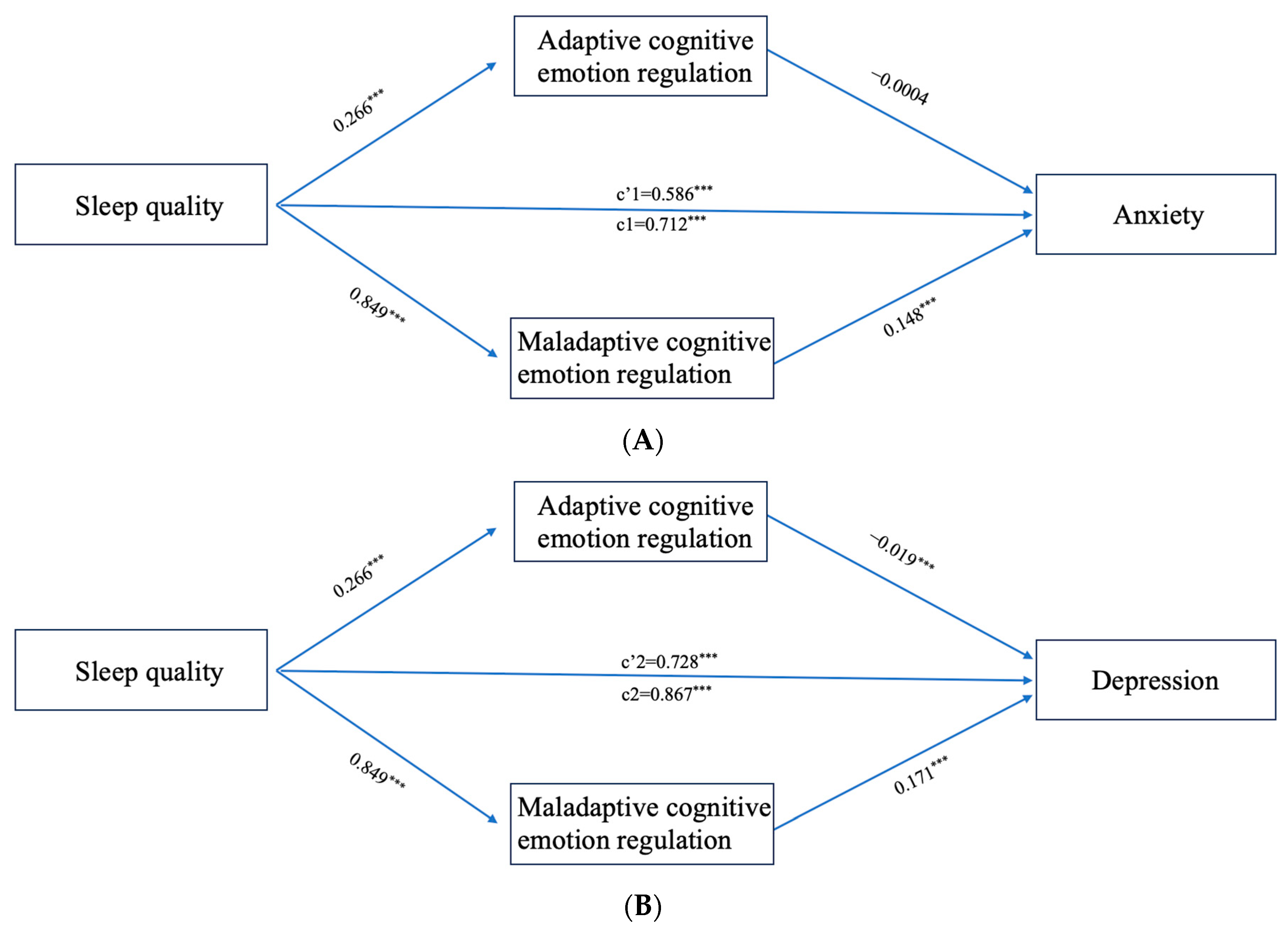
3.3. Results of the CERS Mediating Effect Analysis
3.4. Specific Types of CERS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CERS | Cognitive emotion regulation strategies |
| CPSQI | Chinese version of the Pittsburgh Sleep Quality Index |
| CERQ | Cognitive Emotion Regulation Questionnaire |
| PHQ-9 | Patient Health Questionnaire-9 |
| GAD-7 | Generalized Anxiety Disorder Scale-7 |
| CERQ-C | Chinese version of the Cognitive Emotion Regulation Questionnaire |
| SD | Standard deviation |
| BMI | Body mass index |
| SB | Self-blame |
| Acc | Acceptance |
| Rum | Rumination |
| P-Ref | Positive refocusing |
| R-Plan | Refocus on planning |
| P-Reap | Positive reappraisal |
| PP | Putting into perspective |
| Cat | Catastrophizing |
| BO | Blaming others |
| CERQ-A | Adaptive Cognitive Emotion Regulation Questionnaire score |
| CERQ-M | Maladaptive Cognitive Emotion Regulation Questionnaire score |
| CI | Confidence Interval |
References
- Li, W.; Zhao, Z.; Chen, D.; Peng, Y.; Lu, Z. Prevalence and associated factors of depression and anxiety symptoms among college students: A systematic review and meta-analysis. J. Child Psychol. Psychiatry 2022, 63, 1222–1230. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Ping, S.; Liu, X. Gender differences in depression, anxiety, and stress among college students: A longitudinal study from China. J. Affect. Disord. 2020, 263, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Mirchandaney, R.; Barete, R.; Asarnow, L.D. Moderators of Cognitive Behavioral Treatment for Insomnia on Depression and Anxiety Outcomes. Curr. Psychiatry Rep. 2022, 24, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Tsuno, N.; Besset, A.; Ritchie, K. Sleep and depression. J. Clin. Psychiatry 2005, 66, 1254–1269. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Deng, J.; He, Y.; Deng, X.; Huang, J.; Huang, G.; Gao, X.; Lu, C. Prevalence and correlates of sleep disturbance and depressive symptoms among Chinese adolescents: A cross-sectional survey study. BMJ Open 2014, 4, e005517. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Su, H.; Zou, Y.; Chen, J.; Wu, J.; Chang, W. Sleep quality of Chinese adolescents: Distribution and its associated factors. J. Paediatr. Child Health 2012, 48, 138–145. [Google Scholar] [CrossRef]
- Blanken, T.F.; Borsboom, D.; Penninx, B.W.; Van Someren, E.J. Network outcome analysis identifies difficulty initiating sleep as a primary target for prevention of depression: A 6-year prospective study. Sleep. 2020, 43, zsz288. [Google Scholar] [CrossRef] [PubMed]
- Soehner, A.M.; Harvey, A.G. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: Results from a nationally representative sample. Sleep 2012, 35, 1367–1375. [Google Scholar] [CrossRef]
- Kim, B.S.; Jeon, H.J.; Hong, J.P.; Bae, J.N.; Lee, J.Y.; Chang, S.M.; Lee, Y.M.; Son, J.; Cho, M.J. DSM-IV psychiatric comorbidity according to symptoms of insomnia: A nationwide sample of Korean adults. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 2019–2033. [Google Scholar] [CrossRef]
- McGowan, S.K.; Behar, E.; Luhmann, M. Examining the Relationship Between Worry and Sleep: A Daily Process Approach. Behav. Ther. 2016, 47, 460–473. [Google Scholar] [CrossRef]
- Ramsawh, H.J.; Stein, M.B.; Belik, S.L.; Jacobi, F.; Sareen, J. Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. J. Psychiatr. Res. 2009, 43, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Quach, J.L.; Nguyen, C.D.; Williams, K.E.; Sciberras, E. Bidirectional Associations Between Child Sleep Problems and Internalizing and Externalizing Difficulties From Preschool to Early Adolescence. JAMA Pediatr. 2018, 172, e174363. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.S.; Gujar, N.; Hu, P.; Jolesz, F.A.; Walker, M.P. The human emotional brain without sleep—A prefrontal amygdala disconnect. Curr. Biol. 2007, 17, R877–R878. [Google Scholar] [CrossRef]
- Garnefski, N.; Kraaij, V.; Benoist, M.; Bout, Z.; Karels, E.; Smit, A. Effect of a cognitive behavioral self-help intervention on depression, anxiety, and coping self-efficacy in people with rheumatic disease. Arthritis Care Res. 2013, 65, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Cunyou, G.; Jingli, G.; Huifeng, D.; Donghe, L.; Xialian, Z.; Jing, B. The effect of Cognitive Emotion Regulation strategies on the vulnerability to Stress-related Sleep Dis- turbance. J. Int. Psychiatry 2016, 43, 83–86. [Google Scholar] [CrossRef]
- Beauregard, M.; Paquette, V.; Lévesque, J. Dysfunction in the neural circuitry of emotional self-regulation in major depressive disorder. Neuroreport 2006, 17, 843–846. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.C.; Dahlen, E.R. Cognitive emotion regulation and the prediction of depression, anxiety, stress, and anger. Personal. Individ. Differ. 2005, 39, 1249–1260. [Google Scholar] [CrossRef]
- Kraaij, V.; Garnefski, N. Coping and depressive symptoms in adolescents with a chronic medical condition: A search for intervention targets. J. Adolesc. 2012, 35, 1593–1600. [Google Scholar] [CrossRef]
- Mocan, A.; Iancu, S.; Băban, A.S. Association of cognitive-emotional regulation strategies to depressive symptoms in type 2 diabetes patients. Rom. J. Intern. Med. 2018, 56, 34–40. [Google Scholar] [CrossRef]
- Yan, Z.; Bingkun, L.; Jiakun, W.; Jing, Y.; Linlin, Z. Effect of mindfulness trait factors on sleep quality of college students: The mediating role of cognitive emotion regulation strategies and anxiety. Chin. J. Behav. Med. Brain Sci. 2019, 28, 788–792. [Google Scholar] [CrossRef]
- Hongjun, Y.; Xiongzhao, Z.; Lingyan, L.; Jingqiang, Z.; Xiang, W.; Jie, F.; Na, Y. Effects of Cognitive Emotion Regulation on Sleep Quality of Healthy Youth Female: Mediating and Suppressing Effects of Depression. Chin. J. Clin. Psychol. 2021, 29, 1014–1018. [Google Scholar] [CrossRef]
- Yimei, W.; Ming, Z. Cognitive Coping Group Mental Training for Improving College Students’ Depression. Chin. J. Clin. Psychol. 2010, 18, 127–129. [Google Scholar] [CrossRef]
- Tsai, P.S.; Wang, S.Y.; Wang, M.Y.; Su, C.T.; Yang, T.T.; Huang, C.J.; Fang, S.C. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual. Life Res. 2005, 14, 1943–1952. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.Z.; Luo, F.S.; Yao, S.Q.; Randy, P.A.; John, R.Z.A. Reliability and Validity of the Cognitive Emotion Regulation Questionnaire-Chinese Version. Chin. J. Clin. Psychol. 2007, 15, 121–124+131. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Tong, X.; An, D.; McGonigal, A.; Park, S.P.; Zhou, D. Validation of the Generalized Anxiety Disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. 2016, 120, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Yu, H.; Austin, L. The Effect of Physical Activity on Anxiety: The Mediating Role of Subjective Well-Being and the Moderating Role of Gender. Psychol. Res. Behav. Manag. 2022, 15, 3167–3178. [Google Scholar] [CrossRef]
- Zhang, Y.L.; Liang, W.; Chen, Z.M.; Zhang, H.M.; Zhang, J.H.; Weng, X.Q.; Yang, S.C.; Zhang, L.; Shen, L.J.; Zhang, Y.L. Validity and reliability of Patient Health Questionnaire-9 and Patient Health Questionnaire-2 to screen for depression among college students in China. Asia Pac. Psychiatry 2013, 5, 268–275. [Google Scholar] [CrossRef]
- Perotta, B.; Arantes-Costa, F.M.; Enns, S.C.; Figueiro-Filho, E.A.; Paro, H.; Santos, I.S.; Lorenzi-Filho, G.; Martins, M.A.; Tempski, P.Z. Sleepiness, sleep deprivation, quality of life, mental symptoms and perception of academic environment in medical students. BMC Med. Educ. 2021, 21, 111. [Google Scholar] [CrossRef]
- Curcio, G.; Ferrara, M.; De Gennaro, L. Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 2006, 10, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Du, X.; Guo, Y.; Li, W.; Teopiz, K.M.; Shi, J.; Guo, L.; Lu, C.; McIntyre, R.S. The associations between sleep situations and mental health among Chinese adolescents: A longitudinal study. Sleep Med. 2021, 82, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Lovato, N.; Gradisar, M. A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Med. Rev. 2014, 18, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Murniati, N.; Kamso, S. The Role of Biopsychosocial Factors on Elderly Depression in Indonesia: Data Analysis of the Indonesian Family Life Survey Wave 5. Proceedings 2022, 83, 19. [Google Scholar] [CrossRef]
- Suchomlinov, A.; Konstantinov, V.V.; Purlys, P. Associations between depression, height and body mass index in adolescent and adult population of Penza city and oblast, Russia. J. Biosoc. Sci. 2021, 53, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Mullarkey, M.C.; Marchetti, I.; Bluth, K.; Carlson, C.L.; Shumake, J.; Beevers, C.G. Symptom centrality and infrequency of endorsement identify adolescent depression symptoms more strongly associated with life satisfaction. J. Affect. Disord. 2021, 289, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Boiko, D.I.; Shkodina, A.D.; Hasan, M.M.; Bardhan, M.; Kazmi, S.K.; Chopra, H.; Bhutra, P.; Baig, A.A.; Skrypnikov, A.M. Melatonergic Receptors (Mt1/Mt2) as a Potential Additional Target of Novel Drugs for Depression. Neurochem. Res. 2022, 47, 2909–2924. [Google Scholar] [CrossRef]
- Daut, R.A.; Fonken, L.K. Circadian regulation of depression: A role for serotonin. Front. Neuroendocrinol. 2019, 54, 100746. [Google Scholar] [CrossRef]
- Wetterberg, L. Clinical importance of melatonin. Prog. Brain Res. 1979, 52, 539–547. [Google Scholar] [CrossRef]
- Liu, Y.; Li, H.; Xu, X.; Li, Y.; Wang, Z.; Zhu, H.; Zhang, X.; Jiang, S.; Li, N.; Gu, S.; et al. The Relationship between Insecure Attachment to Depression: Mediating Role of Sleep and Cognitive Reappraisal. Neural Plast. 2020, 2020, 1931737. [Google Scholar] [CrossRef]
- Alvaro, P.K.; Roberts, R.M.; Harris, J.K. The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Med. 2014, 15, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.A.; Alfano, C.A. Sleep and emotion regulation: An organizing, integrative review. Sleep Med. Rev. 2017, 31, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Gross, J.J. Emotion Regulation: Current Status and FutureProspects. Psychol. Inq. 2015, 26, 1–26. [Google Scholar] [CrossRef]
- Blake, M.J.; Trinder, J.A.; Allen, N.B. Mechanisms underlying the association between insomnia, anxiety, and depression in adolescence: Implications for behavioral sleep interventions. Clin. Psychol. Rev. 2018, 63, 25–40. [Google Scholar] [CrossRef]
- Hom, M.A.; Hames, J.L.; Bodell, L.P.; Buchman-Schmitt, J.M.; Chu, C.; Rogers, M.L.; Chiurliza, B.; Michaels, M.S.; Ribeiro, J.D.; Nadorff, M.R.; et al. Investigating insomnia as a cross-sectional and longitudinal predictor of loneliness: Findings from six samples. Psychiatry Res. 2017, 253, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Muñoz-Navarro, R.; Malonda, E.; Llorca-Mestre, A.; Cano-Vindel, A.; Fernández-Berrocal, P. Worry about COVID-19 contagion and general anxiety: Moderation and mediation effects of cognitive emotion regulation. J. Psychiatr. Res. 2021, 137, 311–318. [Google Scholar] [CrossRef] [PubMed]
- D’Avanzato, C.; Joormann, J.; Siemer, M.; Gotlib, I.H. Emotion regulation in depression and anxiety: Examining diagnostic specificity and stability of strategy use. Cogn. Ther. Res. 2013, 37, 968–980. [Google Scholar] [CrossRef]
- Gruszczyńska, E.; Rzeszutek, M. Affective Well-Being, Rumination, and Positive Reappraisal among People Living with HIV: A Measurement-Burst Diary Study. Appl. Psychol. Health Well Being 2020, 12, 587–609. [Google Scholar] [CrossRef]
- Stikkelbroek, Y.; Bodden, D.H.; Kleinjan, M.; Reijnders, M.; van Baar, A.L. Adolescent Depression and Negative Life Events, the Mediating Role of Cognitive Emotion Regulation. PLoS ONE 2016, 11, e0161062. [Google Scholar] [CrossRef]
- McEvoy, P.M.; Watson, H.; Watkins, E.R.; Nathan, P. The relationship between worry, rumination, and comorbidity: Evidence for repetitive negative thinking as a transdiagnostic construct. J. Affect. Disord. 2013, 151, 313–320. [Google Scholar] [CrossRef]
- Guo, J.; Feng, X.L.; Wang, X.H.; van IJzendoorn, M.H. Coping with COVID-19: Exposure to COVID-19 and Negative Impact on Livelihood Predict Elevated Mental Health Problems in Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 3857. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, J.; Naumann, E.; Holmes, E.A.; Tuschen-Caffier, B.; Samson, A.C. Emotion Regulation Strategies in Depressive and Anxiety Symptoms in Youth: A Meta-Analytic Review. J. Youth Adolesc. 2017, 46, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Garnefski, N.; Kraaij, V. Specificity of relations between adolescents’ cognitive emotion regulation strategies and symptoms of depression and anxiety. Cogn. Emot. 2018, 32, 1401–1408. [Google Scholar] [CrossRef] [PubMed]
- Sakakibara, R.; Kitahara, M. The relationship between Cognitive Emotion Regulation Questionnaire (CERQ) and depression, anxiety: Meta-analysis. Shinrigaku Kenkyu 2016, 87, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Chen, L.; Chen, S. Influence of Neuroticism on Depressive Symptoms Among Chinese Adolescents: The Mediation Effects of Cognitive Emotion Regulation Strategies. Front. Psychiatry 2020, 11, 420. [Google Scholar] [CrossRef] [PubMed]
- Kraaij, V.; Garnefski, N. Cognitive, behavioral and goal adjustment coping and depressive symptoms in young people with diabetes: A search for intervention targets for coping skills training. J. Clin. Psychol. Med. Settings 2015, 22, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Molero Jurado, M.D.M.; Pérez-Fuentes, M.D.C.; Fernández-Martínez, E.; Martos Martínez, Á.; Gázquez Linares, J.J. Coping Strategies in the Spanish Population: The Role in Consequences of COVID-19 on Mental Health. Front. Psychiatry 2021, 12, 606621. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S. Emotion regulation and psychopathology: The role of gender. Annu. Rev. Clin. Psychol. 2012, 8, 161–187. [Google Scholar] [CrossRef]
- Quan, L.; Lü, B.; Sun, J.; Zhao, X.; Sang, Q. The relationship between childhood trauma and post-traumatic growth among college students: The role of acceptance and positive reappraisal. Front. Psychol. 2022, 13, 921362. [Google Scholar] [CrossRef]
- Brans, K.; Koval, P.; Verduyn, P.; Lim, Y.L.; Kuppens, P. The regulation of negative and positive affect in daily life. Emotion 2013, 13, 926–939. [Google Scholar] [CrossRef]
| Variable | Category | Number of Samples | Mean (SD)/Percentage (%) |
|---|---|---|---|
| Age | 4325 | 19.90 (1.34) | |
| Gender | Male | 1668 | 38.60 |
| Female | 2657 | 61.40 | |
| Ethnicity | Han Chinese | 1743 | 40.30 |
| Tibetan | 2470 | 57.10 | |
| Other | 112 | 2.60 | |
| Residential location | Urban | 1210 | 28.00 |
| Rural | 3115 | 72.00 | |
| Only child status | Yes | 866 | 20.00 |
| No | 3459 | 80.00 | |
| Family relations | Good | 3887 | 89.90 |
| General | 340 | 7.90 | |
| Poor | 98 | 2.30 | |
| Academic pressure | Mild | 603 | 13.90 |
| Moderate | 1716 | 39.70 | |
| Severe | 2006 | 46.40 | |
| Smoking status | No | 3435 | 79.40 |
| Yes | 890 | 20.60 | |
| Alcohol consumption | No | 2017 | 46.60 |
| Yes | 2308 | 53.40 | |
| BMI | 4325 | 21.37 (3.44) | |
| CPSQI score | 4325 | 5.54 (2.78) | |
| Normal | 2349 | 54.31 | |
| Poor sleep quality | 1976 | 45.69 | |
| GAD-7 score | Normal | 2733 | 63.19 |
| Mild | 1111 | 25.69 | |
| Moderate | 344 | 7.95 | |
| Severe | 137 | 3.17 | |
| PHQ-9 score | normal | 2082 | 48.14 |
| Mild | 1479 | 34.20 | |
| Moderate | 549 | 12.69 | |
| Moderate severe | 160 | 3.70 | |
| Severe | 55 | 1.27 | |
| CERQ-M | 4325 | 42.43 (8.43) | |
| CERQ-A | 4325 | 63.49 (10.11) |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CPSQI | 1 | ||||||||||||
| 2. SB | 0.199 ** | 1 | |||||||||||
| 3. Acc | 0.099 ** | 0.522 ** | 1 | ||||||||||
| 4. Rum | 0.242 ** | 0.491 ** | 0.449 ** | 1 | |||||||||
| 5. P-Ref | 0.075 ** | 0.364 ** | 0.433 ** | 0.528 ** | 1 | ||||||||
| 6. R-Plan | 0.040 ** | 0.353 ** | 0.410 ** | 0.372 ** | 0.506 ** | 1 | |||||||
| 7. P-Reap | −0.035 * | 0.274 ** | 0.387 ** | 0.292 ** | 0.478 ** | 0.757 ** | 1 | ||||||
| 8. PP | 0.207 ** | 0.311 ** | 0.271 ** | 0.409 ** | 0.287 ** | 0.154 ** | 0.129 ** | 1 | |||||
| 9. Cat | 0.288 ** | 0.272 ** | 0.171 ** | 0.419 ** | 0.208 ** | 0.054 ** | −0.027 | 0.607 ** | 1 | ||||
| 10. BO | 0.214 ** | 0.243 ** | 0.175 ** | 0.327 ** | 0.182 ** | 0.045 ** | 0.001 | 0.514 ** | 0.598 ** | 1 | |||
| 11. CERQ-A | 0.103 ** | 0.509 ** | 0.701 ** | 0.568 ** | 0.748 ** | 0.813 ** | 0.792 ** | 0.497 ** | 0.269 ** | 0.245 ** | 1 | ||
| 12. CERQ-M | 0.321 ** | 0.663 ** | 0.439 ** | 0.759 ** | 0.432 ** | 0.274 ** | 0.178 ** | 0.629 ** | 0.791 ** | 0.735 ** | 0.534 ** | 1 | |
| 13. GAD-7 score | 0.497 ** | 0.296 ** | 0.164 ** | 0.354 ** | 0.183 ** | 0.119 ** | 0.033 * | 0.285 ** | 0.366 ** | 0.260 ** | 0.213 ** | 0.434 ** | 1 |
| 14. PHQ-9 score | 0.537 ** | 0.285 ** | 0.148 ** | 0.341 ** | 0.162 ** | 0.069 ** | −0.009 | 0.297 ** | 0.376 ** | 0.269 ** | 0.179 ** | 0.433 ** | 0.806 ** |
| Path | Effect | Boot SE | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Model a | ||||
| Total effect | 0.712 | 0.021 | 0.670 | 0.753 |
| Direct effect | 0.586 | 0.021 | 0.544 | 0.628 |
| Total indirect effect | 0.126 | 0.010 | 0.107 | 0.145 |
| Sleep quality→ CERQ_A→ anxiety | −0.00001 | 0.002 | −0.004 | 0.004 |
| Sleep quality→ CERQ_M→ anxiety | 0.126 | 0.010 | 0.106 | 0.147 |
| Model b | ||||
| Total effect | 0.867 | 0.023 | 0.822 | 0.912 |
| Direct effect | 0.728 | 0.023 | 0.683 | 0.773 |
| Total indirect effect | 0.139 | 0.010 | 0.119 | 0.160 |
| Sleep quality → CERQ_A → depression | −0.005 | 0.002 | −0.011 | −0.001 |
| Sleep quality → CERQ_M → depression | 0.145 | 0.011 | 0.123 | 0.167 |
| Mediating Variable (M) | Effect of Sleep Quality on M (a) | Effect of M on Anxiety (b) | Direct Effect (c’) | Indirect Effect (ab) | Effect of M on Depression (b) | Direct Effect (c’) | Indirect Effect (ab) |
|---|---|---|---|---|---|---|---|
| SB | 0.158 *** | 0.306 *** | 0.665 *** | 0.048 *** | 0.308 *** | 0.820 *** | 0.049 *** |
| Acc | 0.071 *** | 0.153 *** | 0.703 *** | 0.011 *** | 0.138 *** | 0.859 *** | 0.010 *** |
| Rum | 0.222 *** | 0.347 *** | 0.636 *** | 0.077 *** | 0.354 *** | 0.790 *** | 0.079 *** |
| P-Ref | 0.053 *** | 0.219 *** | 0.702 *** | 0.012 *** | 0.208 *** | 0.857 *** | 0.011 *** |
| R-Plan | 0.024 *** | 0.119 *** | 0.711 *** | 0.003 | 0.055 ** | 0.867 *** | 0.001 |
| P-Reap | −0.045 ** | 0.060 *** | 0.716 *** | −0.003 *** | 0.006 | 0.869 *** | 0.001 |
| PP | 0.166 *** | 0.283 *** | 0.666 *** | 0.047 *** | 0.326 *** | 0.814 *** | 0.054 *** |
| Cat | 0.281 *** | 0.321 *** | 0.622 *** | 0.090 *** | 0.365 *** | 0.766 *** | 0.103 *** |
| BO | 0.187 *** | 0.238 *** | 0.669 *** | 0.045 *** | 0.267 *** | 0.818 *** | 0.050 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Guang, Z.; Zhang, J.; Han, L.; Zhang, R.; Chen, Y.; Chen, Q.; Liu, Z.; Gao, Y.; Wu, R.; et al. Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China’s Xizang Region: The Mediating Effect of Cognitive Emotion Regulation. Behav. Sci. 2023, 13, 861. https://doi.org/10.3390/bs13100861
Wang Y, Guang Z, Zhang J, Han L, Zhang R, Chen Y, Chen Q, Liu Z, Gao Y, Wu R, et al. Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China’s Xizang Region: The Mediating Effect of Cognitive Emotion Regulation. Behavioral Sciences. 2023; 13(10):861. https://doi.org/10.3390/bs13100861
Chicago/Turabian StyleWang, Yingting, Zixuan Guang, Jinjing Zhang, Lixin Han, Rongqiang Zhang, Yichun Chen, Qi Chen, Zhenjia Liu, Yuan Gao, Ruipeng Wu, and et al. 2023. "Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China’s Xizang Region: The Mediating Effect of Cognitive Emotion Regulation" Behavioral Sciences 13, no. 10: 861. https://doi.org/10.3390/bs13100861
APA StyleWang, Y., Guang, Z., Zhang, J., Han, L., Zhang, R., Chen, Y., Chen, Q., Liu, Z., Gao, Y., Wu, R., & Wang, S. (2023). Effect of Sleep Quality on Anxiety and Depression Symptoms among College Students in China’s Xizang Region: The Mediating Effect of Cognitive Emotion Regulation. Behavioral Sciences, 13(10), 861. https://doi.org/10.3390/bs13100861








