Relationship between Problematic Smartphone Use, Sleep Quality and Bedtime Procrastination: A Mediation Analysis
Abstract
1. Introduction
1.1. Mechanisms by Which Smartphone Use Affects Sleep
1.1.1. Disruption of Circadian Rhythms
1.1.2. Increased Arousal
1.1.3. Bedtime Procrastination and Sleep Displacement
2. Materials and Methods
2.1. Participants and Procedure
2.2. Instruments
2.2.1. Sleep Quality
2.2.2. Bedtime Procrastination
2.2.3. Problematic Smartphone Use
2.2.4. Smartphone Usage Pattern
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Correlations
3.3. Mean Comparison between Genders
3.4. Comparison between Age Groups
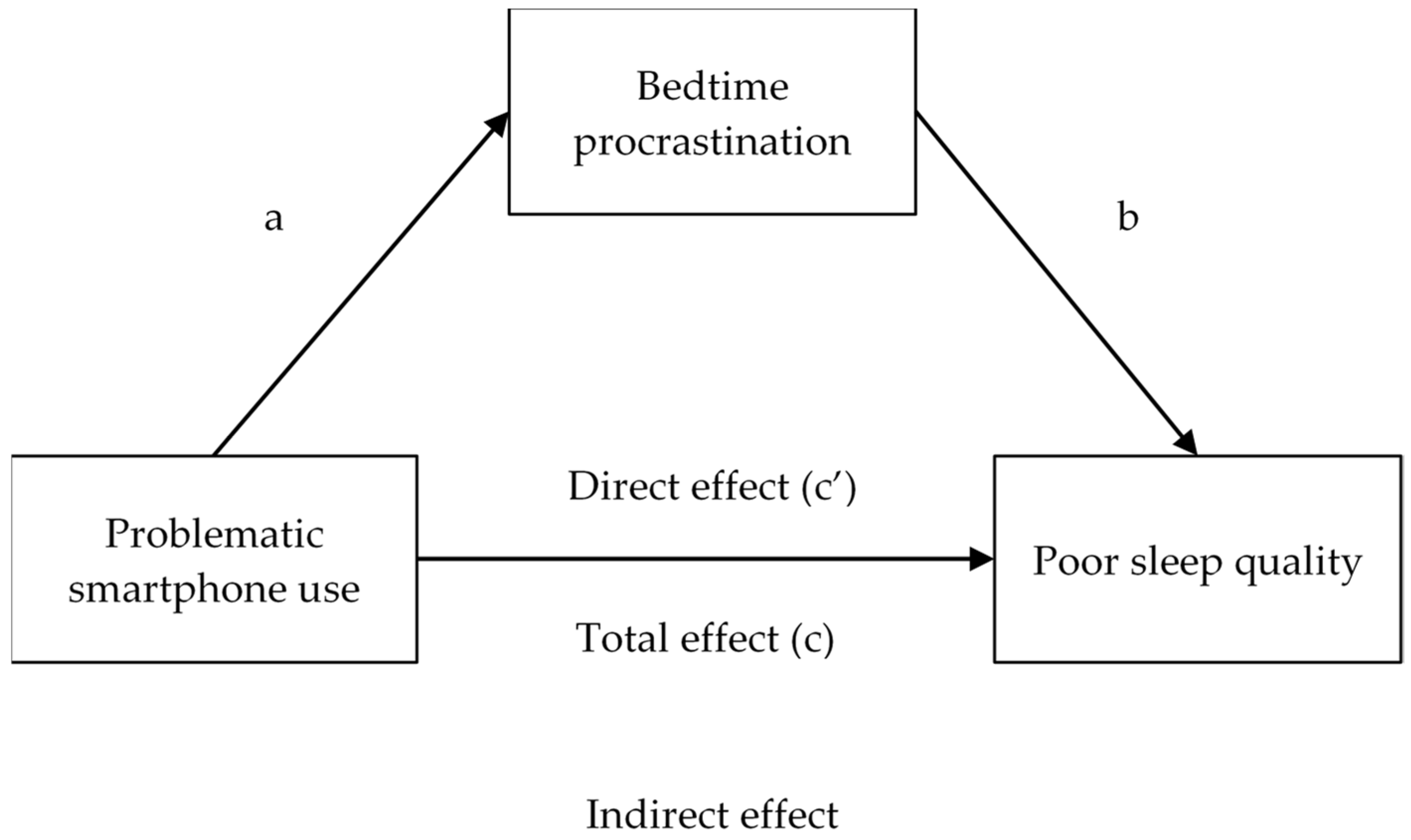
3.5. Mediation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Scott, A.J.; Webb, T.L.; Martyn-St James, M.; Rowse, G.; Weich, S. Improving Sleep Quality Leads to Better Mental Health: A Meta-Analysis of Randomised Controlled Trials. Sleep Med. Rev. 2021, 60, 101556. [Google Scholar] [CrossRef] [PubMed]
- Spanish Society of Neurology. Los Problemas Del Sueño Amenazan la Salud Y la Calidad de Vida de Hasta El 45% De la Población Mundial. 2021. Available online: https://www.sen.es/saladeprensa/pdf/Link263.pdf (accessed on 18 May 2023).
- Galland, B.C.; Gray, A.R.; Penno, J.; Smith, C.; Lobb, C.; Taylor, R.W. Gender Differences in Sleep Hygiene Practices and Sleep Quality in New Zealand Adolescents Aged 15 to 17 Years. Sleep Health 2017, 3, 77–83. [Google Scholar] [CrossRef]
- Fatima, Y.; Doi, S.A.R.; Najman, J.M.; Mamun, A.A. Exploring Gender Difference in Sleep Quality of Young Adults: Findings from a Large Population Study. Clin. Med. Res. 2016, 14, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Liao, Y.; Kelly, B.C.; Xie, L.; Xiang, Y.-T.; Qi, C.; Pan, C.; Hao, W.; Liu, T.; Zhang, F.; et al. Gender and Regional Differences in Sleep Quality and Insomnia: A General Population-Based Study in Hunan Province of China. Sci. Rep. 2017, 7, 43690. [Google Scholar] [CrossRef] [PubMed]
- João, K.A.D.R.; de Jesus, S.N.; Carmo, C.; Pinto, P. The Impact of Sleep Quality on the Mental Health of a Non-Clinical Population. Sleep Med. 2018, 46, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Madrid-Valero, J.J.; Kirkpatrick, R.M.; González-Javier, F.; Gregory, A.M.; Ordoñana, J.R. Sex Differences in Sleep Quality and Psychological Distress: Insights from a Middle-Aged Twin Sample from Spain. J. Sleep Res. 2023, 32, e13714. [Google Scholar] [CrossRef]
- Stahl, S.M. Stahl’s Essential Psychopharmacology: Neuroscientific Basis and Practical Applications, 1st ed.; Cambridge University Press: Cambridge, UK, 2022; ISBN 978-1-00-905336-5. [Google Scholar]
- Merikanto, I.; Kortesoja, L.; Benedict, C.; Chung, F.; Cedernaes, J.; Espie, C.A.; Morin, C.M.; Dauvilliers, Y.; Partinen, M.; De Gennaro, L.; et al. Evening-Types Show Highest Increase of Sleep and Mental Health Problems during the COVID-19 Pandemic-Multinational Study on 19 267 Adults. Sleep 2022, 45, zsab216. [Google Scholar] [CrossRef]
- Lin, L.-Y.; Wang, J.; Ou-Yang, X.-Y.; Miao, Q.; Chen, R.; Liang, F.-X.; Zhang, Y.-P.; Tang, Q.; Wang, T. The Immediate Impact of the 2019 Novel Coronavirus (COVID-19) Outbreak on Subjective Sleep Status. Sleep Med. 2021, 77, 348–354. [Google Scholar] [CrossRef]
- Dal Santo, F.; González-Blanco, L.; Rodríguez-Revuelta, J.; Marina González, P.A.; Paniagua, G.; García-Álvarez, L.; De La Fuente-Tomás, L.; Sáiz, P.A.; García-Portilla, M.P.; Bobes, J. Early Impact of the COVID-19 Outbreak on Sleep in a Large Spanish Sample. Behav. Sleep. Med. 2022, 20, 100–115. [Google Scholar] [CrossRef]
- Trott, M.; Driscoll, R.; Iraldo, E.; Pardhan, S. Changes and Correlates of Screen Time in Adults and Children during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. eClinicalMedicine 2022, 48, 101452. [Google Scholar] [CrossRef] [PubMed]
- Lapierre, M.A.; Zhao, P.; Custer, B.E. Short-Term Longitudinal Relationships Between Smartphone Use/Dependency and Psychological Well-Being Among Late Adolescents. J. Adolesc. Health 2019, 65, 607–612. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Statistics. Encuesta sobre Equipamiento y Uso de Tecnologías de Información y Comunicación (TIC) en los Hogares. 2022. Available online: https://www.ine.es/prensa/tich_2022.pdf (accessed on 18 May 2023).
- Smartme Analytics Digital Consumer by Generation. Available online: https://smartmeanalytics.com/insight/digital-consumer-by-generation-2022 (accessed on 18 May 2023).
- Kwon, M.; Kim, D.-J.; Cho, H.; Yang, S. The Smartphone Addiction Scale: Development and Validation of a Short Version for Adolescents. PLoS ONE 2013, 8, e83558. [Google Scholar] [CrossRef] [PubMed]
- Billieux, J.; Maurage, P.; Lopez-Fernandez, O.; Kuss, D.J.; Griffiths, M.D. Can Disordered Mobile Phone Use Be Considered a Behavioral Addiction? An Update on Current Evidence and a Comprehensive Model for Future Research. Curr. Addict. Rep. 2015, 2, 156–162. [Google Scholar] [CrossRef]
- Horwood, S.; Anglim, J. Personality and Problematic Smartphone Use: A Facet-Level Analysis Using the Five Factor Model and HEXACO Frameworks. Comput. Hum. Behav. 2018, 85, 349–359. [Google Scholar] [CrossRef]
- Lepp, A.; Li, J.; Barkley, J.E. College Students’ Cell Phone Use and Attachment to Parents and Peers. Comput. Hum. Behav. 2016, 64, 401–408. [Google Scholar] [CrossRef]
- Panova, T.; Carbonell, X. Is Smartphone Addiction Really an Addiction? J. Behav. Addict. 2018, 7, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Montag, C.; Wegmann, E.; Sariyska, R.; Demetrovics, Z.; Brand, M. How to Overcome Taxonomical Problems in the Study of Internet Use Disorders and What to Do with “Smartphone Addiction”? J. Behav. Addict. 2021, 9, 908–914. [Google Scholar] [CrossRef]
- Servidio, R. Self-Control and Problematic Smartphone Use among Italian University Students: The Mediating Role of the Fear of Missing out and of Smartphone Use Patterns. Curr. Psychol. 2021, 40, 4101–4111. [Google Scholar] [CrossRef]
- Sha, P.; Sariyska, R.; Riedl, R.; Lachmann, B.; Montag, C. Linking Internet Communication and Smartphone Use Disorder by Taking a Closer Look at the Facebook and Whatsapp Applications. Addict. Behav. Rep. 2019, 9, 100148. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Lee, D.; Nam, C.R.; Kim, D.Y.; Park, S.; Kwon, J.-G.; Kweon, Y.-S.; Lee, Y.; Kim, D.J.; Choi, J.-S. Distinct Patterns of Internet and Smartphone-Related Problems among Adolescents by Gender: Latent Class Analysis. J. Behav. Addict. 2018, 7, 454–465. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013; ISBN 978-0-89042-555-8. [Google Scholar]
- World Health Organization. International Classification of Diseases 11th Revision (ICD-11). Available online: https://icd.who.int/ (accessed on 8 August 2023).
- Thomée, S. Mobile Phone Use and Mental Health. A Review of the Research That Takes a Psychological Perspective on Exposure. Int. J. Environ. Res. Public Health 2018, 15, 2692. [Google Scholar] [CrossRef]
- Kardefelt-Winther, D. A Conceptual and Methodological Critique of Internet Addiction Research: Towards a Model of Compensatory Internet Use. Comput. Hum. Behav. 2014, 31, 351–354. [Google Scholar] [CrossRef]
- Widyanto, L.; Griffiths, M. ‘Internet Addiction’: A Critical Review. Int. J. Ment. Health Addict. 2006, 4, 31–51. [Google Scholar] [CrossRef]
- Abo-Ali, E.A.; Al-Ghanmi, A.; Hadad, H.; Etaiwi, J.; Bhutta, K.; Hadad, N.; Almilaibary, A.; Ghareeb, W.A.; Sanad, A.; Zaytoun, S. Problematic Smartphone Use: Prevalence and Associated Factors Among Health Sciences Students in Saudi Arabia. J. Prev. 2022, 43, 659–671. [Google Scholar] [CrossRef] [PubMed]
- Ratan, Z.A.; Parrish, A.-M.; Alotaibi, M.S.; Hosseinzadeh, H. Prevalence of Smartphone Addiction and Its Association with Sociodemographic, Physical and Mental Well-Being: A Cross-Sectional Study among the Young Adults of Bangladesh. Int. J. Environ. Res. Public Health 2022, 19, 16583. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Wang, Z.; Zhu, Y.; Shi, X. The Prevalence and Psychosocial Factors of Problematic Smartphone Use Among Chinese College Students: A Three-Wave Longitudinal Study. Front. Psychol. 2022, 13, 877277. [Google Scholar] [CrossRef]
- Ballestar-Tarín, M.L.; Simó-Sanz, C.; Chover-Sierra, E.; Saus-Ortega, C.; Casal-Angulo, C.; Martínez-Sabater, A. Self-Perception of Dependence as an Indicator of Smartphone Addiction. Establishment of a Cut-off Point in the SPAI-SP Inventory. Int. J. Environ. Res. Public Health 2020, 17, 3838. [Google Scholar] [CrossRef] [PubMed]
- De-Solá, J.; Talledo, H.; de Fonseca, F.R.; Rubio, G. Prevalence of Problematic Cell Phone Use in an Adult Population in Spain as Assessed by the Mobile Phone Problem Use Scale (MPPUS). PLoS ONE 2017, 12, e0181184. [Google Scholar] [CrossRef] [PubMed]
- Winkler, A.; Jeromin, F.; Doering, B.K.; Barke, A. Problematic Smartphone Use Has Detrimental Effects on Mental Health and Somatic Symptoms in a Heterogeneous Sample of German Adults. Comput. Hum. Behav. 2020, 113, 106500. [Google Scholar] [CrossRef]
- Chen, B.; Liu, F.; Ding, S.; Ying, X.; Wang, L.; Wen, Y. Gender Differences in Factors Associated with Smartphone Addiction: A Cross-Sectional Study among Medical College Students. BMC Psychiatry 2017, 17, 341. [Google Scholar] [CrossRef] [PubMed]
- Amador-Licona, N.; Carpio-Mendoza, J.J.; Guízar-Mendoza, J.M.; Rodríguez-Sánchez, P. Auto-percepción del Uso Problemático del Teléfono Móvil en Estudiantes Universitarios de Acuerdo a su Sexo. Cuad. Hispanoam. Psicol. 2019, 19, 1–16. [Google Scholar] [CrossRef]
- Choi, S.-W.; Kim, D.-J.; Choi, J.-S.; Ahn, H.; Choi, E.-J.; Song, W.-Y.; Kim, S.; Youn, H. Comparison of Risk and Protective Factors Associated with Smartphone Addiction and Internet Addiction. J. Behav. Addict. 2015, 4, 308–314. [Google Scholar] [CrossRef] [PubMed]
- De-Solá, J.; Rubio, G.; Talledo, H.; Pistoni, L.; Van Riesen, H.; Rodríguez de Fonseca, F. Cell Phone Use Habits Among the Spanish Population: Contribution of Applications to Problematic Use. Front. Psychiatry 2019, 10, 883. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.-F.; Hsu, H.-T.; Lin, P.-C.; Yang, Y.-J.; Huang, Y.-T.; Ko, C.-H.; Wang, H.-H. The Effect of Age, Gender, and Job on Skin Conductance Response among Smartphone Users Who Are Prohibited from Using Their Smartphone. Int. J. Environ. Res. Public Health 2020, 17, 2313. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, J.W.; Choi, T.Y. Risk Factors for Smartphone Addiction in Korean Adolescents: Smartphone Use Patterns. J. Korean Med. Sci. 2017, 32, 1674–1679. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Fernandez, O.; Losada-Lopez, J.L.; Honrubia-Serrano, M.L. Predictors of Problematic Internet and Mobile Phone Usage in Adolescents. Aloma Rev. Psicol. Ciènc. Educ. Esport 2015, 33, 49–58. [Google Scholar] [CrossRef]
- Nayak, J.K. Relationship among Smartphone Usage, Addiction, Academic Performance and the Moderating Role of Gender: A Study of Higher Education Students in India. Comput. Educ. 2018, 123, 164–173. [Google Scholar] [CrossRef]
- Randler, C.; Wolfgang, L.; Matt, K.; Demirhan, E.; Horzum, M.B.; Beşoluk, Ş. Smartphone Addiction Proneness in Relation to Sleep and Morningness–Eveningness in German Adolescents. J. Behav. Addict. 2016, 5, 465–473. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, K.Z.K.; Gong, X.; Zhao, S.J.; Lee, M.K.O.; Liang, L. Examining the Effects of Motives and Gender Differences on Smartphone Addiction. Comput. Hum. Behav. 2017, 75, 891–902. [Google Scholar] [CrossRef]
- De-Solá, J.; Rodríguez de Fonseca, F.; Rubio, G. Cell-Phone Addiction: A Review. Front. Psychiatry 2016, 7, 175. [Google Scholar] [CrossRef]
- Jo, Y.; Bouffard, L. Stability of Self-Control and Gender. J. Crim. Justice 2014, 42, 356–365. [Google Scholar] [CrossRef]
- Jo, Y.; Zhang, Y. Parenting, Self-Control, and Delinquency: Examining the Applicability of Gottfredson and Hirschi’s General Theory of Crime to South Korean Youth. Int. J. Offender Ther. Comp. Criminol. 2014, 58, 1340–1363. [Google Scholar] [CrossRef] [PubMed]
- Duke, É.; Montag, C. Smartphone Addiction, Daily Interruptions and Self-Reported Productivity. Addict. Behav. Rep. 2017, 6, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Amez, S.; Baert, S. Smartphone Use and Academic Performance: A Literature Review. Int. J. Educ. Res. 2020, 103, 101618. [Google Scholar] [CrossRef]
- Grant, J.E.; Lust, K.; Chamberlain, S.R. Problematic Smartphone Use Associated with Greater Alcohol Consumption, Mental Health Issues, Poorer Academic Performance, and Impulsivity. J. Behav. Addict. 2019, 8, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Rozgonjuk, D.; Kattago, M.; Täht, K. Social Media Use in Lectures Mediates the Relationship between Procrastination and Problematic Smartphone Use. Comput. Hum. Behav. 2018, 89, 191–198. [Google Scholar] [CrossRef]
- Hidalgo-Fuentes, S. Uso Problemático Del Smartphone y Procrastinación En El Ámbito Académico: Un Meta-Análisis. Electron. J. Res. Educ. Psychol. 2022, 20, 449–468. [Google Scholar] [CrossRef]
- Casale, S.; Fioravanti, G.; Bocci Benucci, S.; Falone, A.; Ricca, V.; Rotella, F. A Meta-Analysis on the Association between Self-Esteem and Problematic Smartphone Use. Comput. Hum. Behav. 2022, 134, 107302. [Google Scholar] [CrossRef]
- Elhai, J.D.; Dvorak, R.D.; Levine, J.C.; Hall, B.J. Problematic Smartphone Use: A Conceptual Overview and Systematic Review of Relations with Anxiety and Depression Psychopathology. J. Affect. Disord. 2017, 207, 251–259. [Google Scholar] [CrossRef]
- Elhai, J.D.; Rozgonjuk, D.; Alghraibeh, A.M.; Yang, H. Disrupted Daily Activities from Interruptive Smartphone Notifications: Relations With Depression and Anxiety Severity and the Mediating Role of Boredom Proneness. Soc. Sci. Comput. Rev. 2021, 39, 20–37. [Google Scholar] [CrossRef]
- Rozgonjuk, D.; Levine, J.C.; Hall, B.J.; Elhai, J.D. The Association between Problematic Smartphone Use, Depression and Anxiety Symptom Severity, and Objectively Measured Smartphone Use over One Week. Comput. Hum. Behav. 2018, 87, 10–17. [Google Scholar] [CrossRef]
- Hartanto, A.; Chua, Y.J.; Quek, F.Y.X.; Wong, J.; Ooi, W.M. Problematic Smartphone Usage, Objective Smartphone Engagement, and Executive Functions: A Latent Variable Analysis. Atten. Percept. Psychophys. 2023. [Google Scholar] [CrossRef] [PubMed]
- Lim, J. The Effect of Adult Smartphone Addiction on Memory Impairment: Focusing on the Mediating effect of Executive Function Deficiencies. J. Digit. Converg. 2018, 16, 299–308. [Google Scholar] [CrossRef]
- Demirci, K.; Akgönül, M.; Akpinar, A. Relationship of Smartphone Use Severity with Sleep Quality, Depression, and Anxiety in University Students. J. Behav. Addict. 2015, 4, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Hughes, N.; Burke, J. Sleeping with the Frenemy: How Restricting ‘Bedroom Use’ of Smartphones Impacts Happiness and Wellbeing. Comput. Hum. Behav. 2018, 85, 236–244. [Google Scholar] [CrossRef]
- Panda, A.; Jain, N.K. Compulsive Smartphone Usage and Users’ Ill-Being among Young Indians: Does Personality Matter? Telemat. Inform. 2018, 35, 1355–1372. [Google Scholar] [CrossRef]
- Volungis, A.M.; Kalpidou, M.; Popores, C.; Joyce, M. Smartphone Addiction and Its Relationship with Indices of Social-Emotional Distress and Personality. Int. J. Ment. Health Addict. 2020, 18, 1209–1225. [Google Scholar] [CrossRef]
- Yang, Z.; Asbury, K.; Griffiths, M.D. “A Cancer in the Minds of Youth?” A Qualitative Study of Problematic Smartphone Use among Undergraduate Students. Int. J. Ment. Health Addict. 2021, 19, 934–946. [Google Scholar] [CrossRef]
- Lewy, A.J. Melatonin and Human Chronobiology. Cold Spring Harb. Symp. Quant. Biol. 2007, 72, 623–636. [Google Scholar] [CrossRef]
- Oster, H.; Challet, E.; Ott, V.; Arvat, E.; De Kloet, E.R.; Dijk, D.-J.; Lightman, S.; Vgontzas, A.; Van Cauter, E. The Functional and Clinical Significance of the 24-Hour Rhythm of Circulating Glucocorticoids. Endocr. Rev. 2017, 38, 3–45. [Google Scholar] [CrossRef]
- Cajochen, C.; Frey, S.; Anders, D.; Späti, J.; Bues, M.; Pross, A.; Mager, R.; Wirz-Justice, A.; Stefani, O. Evening Exposure to a Light-Emitting Diodes (LED)-Backlit Computer Screen Affects Circadian Physiology and Cognitive Performance. J. Appl. Physiol. 2011, 110, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- Cajochen, C.; Münch, M.; Kobialka, S.; Kräuchi, K.; Steiner, R.; Oelhafen, P.; Orgül, S.; Wirz-Justice, A. High Sensitivity of Human Melatonin, Alertness, Thermoregulation, and Heart Rate to Short Wavelength Light. J. Clin. Endocrinol. Metab. 2005, 90, 1311–1316. [Google Scholar] [CrossRef] [PubMed]
- Fisk, A.S.; Tam, S.K.E.; Brown, L.A.; Vyazovskiy, V.V.; Bannerman, D.M.; Peirson, S.N. Light and Cognition: Roles for Circadian Rhythms, Sleep, and Arousal. Front. Neurol. 2018, 9, 56. [Google Scholar] [CrossRef] [PubMed]
- Höhn, C.; Schmid, S.R.; Plamberger, C.P.; Bothe, K.; Angerer, M.; Gruber, G.; Pletzer, B.; Hoedlmoser, K. Preliminary Results: The Impact of Smartphone Use and Short-Wavelength Light during the Evening on Circadian Rhythm, Sleep and Alertness. Clocks Sleep 2021, 3, 66–86. [Google Scholar] [CrossRef] [PubMed]
- Van Der Lely, S.; Frey, S.; Garbazza, C.; Wirz-Justice, A.; Jenni, O.G.; Steiner, R.; Wolf, S.; Cajochen, C.; Bromundt, V.; Schmidt, C. Blue Blocker Glasses as a Countermeasure for Alerting Effects of Evening Light-Emitting Diode Screen Exposure in Male Teenagers. J. Adolesc. Health 2015, 56, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Taillard, J.; Capelli, A.; Sagaspe, P.; Anund, A.; Akerstedt, T.; Philip, P. In-Car Nocturnal Blue Light Exposure Improves Motorway Driving: A Randomized Controlled Trial. PLoS ONE 2012, 7, e46750. [Google Scholar] [CrossRef] [PubMed]
- Chinoy, E.D.; Duffy, J.F.; Czeisler, C.A. Unrestricted Evening Use of Light-Emitting Tablet Computers Delays Self-Selected Bedtime and Disrupts Circadian Timing and Alertness. Physiol. Rep. 2018, 6, e13692. [Google Scholar] [CrossRef] [PubMed]
- Schmid, S.R.; Höhn, C.; Bothe, K.; Plamberger, C.P.; Angerer, M.; Pletzer, B.; Hoedlmoser, K. How Smart Is It to Go to Bed with the Phone? The Impact of Short-Wavelength Light and Affective States on Sleep and Circadian Rhythms. Clocks Sleep 2021, 3, 558–580. [Google Scholar] [CrossRef]
- Wallenius, M.; Hirvonen, A.; Lindholm, H.; Rimpela, A.; Nygård, C.-H.; Saarni, L.; Punamäki, R.-L. Salivary Cortisol in Relation to the Use of Information and Communication Technology (ICT) in School-Aged Children. Psychology 2010, 1, 88–95. [Google Scholar] [CrossRef][Green Version]
- Christakis, D.A.; Liekweg, K.; Garrison, M.M.; Wright, J.A. Infant Video Viewing and Salivary Cortisol Responses: A Randomized Experiment. J. Pediatr. 2013, 162, 1035–1040. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M. More Time on Technology, Less Happiness? Associations Between Digital-Media Use and Psychological Well-Being. Curr. Dir. Psychol. Sci. 2019, 28, 372–379. [Google Scholar] [CrossRef]
- Calamaro, C.J.; Mason, T.B.A.; Ratcliffe, S.J. Adolescents Living the 24/7 Lifestyle: Effects of Caffeine and Technology on Sleep Duration and Daytime Functioning. Pediatrics 2009, 123, e1005–e1010. [Google Scholar] [CrossRef] [PubMed]
- Figueiro, M.G.; Wood, B.; Plitnick, B.; Rea, M.S. The Impact of Watching Television on Evening Melatonin Levels: Impact of Watching Television on Evening Melatonin. J. Soc. Inf. Disp. 2013, 21, 417–421. [Google Scholar] [CrossRef]
- Selmaoui, B.; Touitou, Y. Association Between Mobile Phone Radiation Exposure and the Secretion of Melatonin and Cortisol, Two Markers of the Circadian System: A Review. Bioelectromagnetics 2021, 42, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Kheirinejad, S.; Visuri, A.; Ferreira, D.; Hosio, S. “Leave Your Smartphone out of Bed”: Quantitative Analysis of Smartphone Use Effect on Sleep Quality. Pers. Ubiquitous Comput. 2023, 27, 447–466. [Google Scholar] [CrossRef] [PubMed]
- Altini, M.; Kinnunen, H. The Promise of Sleep: A Multi-Sensor Approach for Accurate Sleep Stage Detection Using the Oura Ring. Sensors 2021, 21, 4302. [Google Scholar] [CrossRef]
- Ferreira, D.; Kostakos, V.; Dey, A.K. AWARE: Mobile Context Instrumentation Framework. Front. ICT 2015, 2, 6. [Google Scholar] [CrossRef]
- Ong, J.C.; Ulmer, C.S.; Manber, R. Improving Sleep with Mindfulness and Acceptance: A Metacognitive Model of Insomnia. Behav. Res. Ther. 2012, 50, 651–660. [Google Scholar] [CrossRef]
- Bodas, M.; Siman-Tov, M.; Peleg, K.; Solomon, Z. Anxiety-Inducing Media: The Effect of Constant News Broadcasting on the Well-Being of Israeli Television Viewers. Psychiatry 2015, 78, 265–276. [Google Scholar] [CrossRef]
- Exelmans, L.; Van Den Bulck, J. Binge Viewing, Sleep, and the Role of Pre-Sleep Arousal. J. Clin. Sleep Med. 2017, 13, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Harbard, E.; Allen, N.B.; Trinder, J.; Bei, B. What’s Keeping Teenagers Up? Prebedtime Behaviors and Actigraphy-Assessed Sleep Over School and Vacation. J. Adolesc. Health 2016, 58, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Mauri, M.; Cipresso, P.; Balgera, A.; Villamira, M.; Riva, G. Why Is Facebook So Successful? Psychophysiological Measures Describe a Core Flow State While Using Facebook. Cyberpsychology Behav. Soc. Netw. 2011, 14, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Van den Bulck, J. Text Messaging as a Cause of Sleep Interruption in Adolescents, Evidence from a Cross-Sectional Study. J. Sleep Res. 2003, 12, 263. [Google Scholar] [CrossRef] [PubMed]
- Woods, H.C.; Scott, H. #Sleepyteens: Social Media Use in Adolescence Is Associated with Poor Sleep Quality, Anxiety, Depression and Low Self-Esteem. J. Adolesc. 2016, 51, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Combertaldi, S.L.; Ort, A.; Cordi, M.; Fahr, A.; Rasch, B. Pre-Sleep Social Media Use Does Not Strongly Disturb Sleep: A Sleep Laboratory Study in Healthy Young Participants. Sleep Med. 2021, 87, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Gillebaart, M. The ‘Operational’ Definition of Self-Control. Front. Psychol. 2018, 9, 1231. [Google Scholar] [CrossRef] [PubMed]
- Heatherton, T.F.; Wagner, D.D. Cognitive Neuroscience of Self-Regulation Failure. Trends Cogn. Sci. 2011, 15, 132–139. [Google Scholar] [CrossRef]
- Zhang, M.X.; Wu, A.M.S. Effects of Smartphone Addiction on Sleep Quality among Chinese University Students: The Mediating Role of Self-Regulation and Bedtime Procrastination. Addict. Behav. 2020, 111, 106552. [Google Scholar] [CrossRef]
- Goldstein, R.Z.; Volkow, N.D. Dysfunction of the Prefrontal Cortex in Addiction: Neuroimaging Findings and Clinical Implications. Nat. Rev. Neurosci. 2011, 12, 652–669. [Google Scholar] [CrossRef]
- Lewis, M. Addiction and the Brain: Development, Not Disease. Neuroethics 2017, 10, 7–18. [Google Scholar] [CrossRef]
- Noël, X.; Brevers, D.; Bechara, A. A Neurocognitive Approach to Understanding the Neurobiology of Addiction. Curr. Opin. Neurobiol. 2013, 23, 632–638. [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.-J.; Fowler, J.S.; Tomasi, D. Addiction Circuitry in the Human Brain. Annu. Rev. Pharmacol. Toxicol. 2012, 52, 321–336. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Koob, G.F.; McLellan, A.T. Neurobiologic Advances from the Brain Disease Model of Addiction. N. Engl. J. Med. 2016, 374, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Liang, Y.; Mai, C.; Zhong, X.; Qu, C. General Deficit in Inhibitory Control of Excessive Smartphone Users: Evidence from an Event-Related Potential Study. Front. Psychol. 2016, 7, 511. [Google Scholar] [CrossRef] [PubMed]
- Rebetez, M.M.L.; Rochat, L.; Barsics, C.; Van Der Linden, M. Procrastination as a Self-Regulation Failure: The Role of Inhibition, Negative Affect, and Gender. Personal. Individ. Differ. 2016, 101, 435–439. [Google Scholar] [CrossRef]
- Kroese, F.M.; De Ridder, D.T.D.; Evers, C.; Adriaanse, M.A. Bedtime Procrastination: Introducing a New Area of Procrastination. Front. Psychol. 2014, 5, 611. [Google Scholar] [CrossRef] [PubMed]
- Nauts, S.; Kamphorst, B.A.; Stut, W.; De Ridder, D.T.D.; Anderson, J.H. The Explanations People Give for Going to Bed Late: A Qualitative Study of the Varieties of Bedtime Procrastination. Behav. Sleep. Med. 2019, 17, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.F.; Pychyl, T.A. A Critique of the Construct Validity of Active Procrastination. Personal. Individ. Differ. 2018, 120, 7–12. [Google Scholar] [CrossRef]
- Kroese, F.M.; de Ridder, D.T.D. Health Behaviour Procrastination: A Novel Reasoned Route towards Self-Regulatory Failure. Health Psychol. Rev. 2016, 10, 313–325. [Google Scholar] [CrossRef]
- Ma, X.; Meng, D.; Zhu, L.; Xu, H.; Guo, J.; Yang, L.; Yu, L.; Fu, Y.; Mu, L. Bedtime Procrastination Predicts the Prevalence and Severity of Poor Sleep Quality of Chinese Undergraduate Students. J. Am. Coll. Health 2022, 70, 1104–1111. [Google Scholar] [CrossRef] [PubMed]
- Exelmans, L.; Van Den Bulck, J. Bedtime Mobile Phone Use and Sleep in Adults. Soc. Sci. Med. 2016, 148, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.C.; Woodward, J.; Woltering, S. Nighttime Cell Phone Use and Sleep Quality in Young Adults. Sleep Biol. Rhythm. 2022, 20, 97–106. [Google Scholar] [CrossRef]
- Moulin, K.L.; Chung, C.-J. Technology Trumping Sleep: Impact of Electronic Media and Sleep in Late Adolescent Students. J. Educ. Learn. 2016, 6, 294. [Google Scholar] [CrossRef][Green Version]
- Liu, H.; Zhou, Z.; Huang, L.; Zhu, E.; Yu, L.; Zhang, M. Prevalence of Smartphone Addiction and Its Effects on Subhealth and Insomnia: A Cross-Sectional Study among Medical Students. BMC Psychiatry 2022, 22, 305. [Google Scholar] [CrossRef]
- Rod, N.H.; Dissing, A.S.; Clark, A.; Gerds, T.A.; Lund, R. Overnight Smartphone Use: A New Public Health Challenge? A Novel Study Design Based on High-Resolution Smartphone Data. PLoS ONE 2018, 13, e0204811. [Google Scholar] [CrossRef]
- Alshammari, T.K.; Rogowska, A.M.; Basharahil, R.F.; Alomar, S.F.; Alseraye, S.S.; Al Juffali, L.A.; Alrasheed, N.M.; Alshammari, M.A. Examining Bedtime Procrastination, Study Engagement, and Studyholism in Undergraduate Students, and Their Association with Insomnia. Front. Psychol. 2023, 13, 1111038. [Google Scholar] [CrossRef]
- Hammoudi, S.F.; Mreydem, H.W.; Ali, B.T.A.; Saleh, N.O.; Chung, S.; Hallit, S.; Salameh, P. Smartphone Screen Time Among University Students in Lebanon and Its Association With Insomnia, Bedtime Procrastination, and Body Mass Index During the COVID-19 Pandemic: A Cross-Sectional Study. Psychiatry Investig. 2021, 18, 871–878. [Google Scholar] [CrossRef]
- Carney, C.E.; Harris, A.L.; Moss, T.G.; Edinger, J.D. Distinguishing Rumination from Worry in Clinical Insomnia. Behav. Res. Ther. 2010, 48, 540–546. [Google Scholar] [CrossRef]
- Meier, A.; Reinecke, L.; Meltzer, C.E. “Facebocrastination”? Predictors of Using Facebook for Procrastination and Its Effects on Students’ Well-Being. Comput. Hum. Behav. 2016, 64, 65–76. [Google Scholar] [CrossRef]
- Reinecke, L.; Hartmann, T.; Eden, A. The Guilty Couch Potato: The Role of Ego Depletion in Reducing Recovery Through Media Use. J. Commun. 2014, 64, 569–589. [Google Scholar] [CrossRef]
- Stainton, M.; Lay, C. Trait Procrastinators and Behavior/Trait-Specific Cognitions. J. Soc. Behav. Personal. 2000, 15, 297. [Google Scholar]
- Guo, J.; Meng, D.; Ma, X.; Zhu, L.; Yang, L.; Mu, L. The Impact of Bedtime Procrastination on Depression Symptoms in Chinese Medical Students. Sleep Breath. 2020, 24, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- You, Z.; Li, X.; Ye, N.; Zhang, L. Understanding the Effect of Rumination on Sleep Quality: A Mediation Model of Negative Affect and Bedtime Procrastination. Curr. Psychol. 2023, 42, 136–144. [Google Scholar] [CrossRef]
- Kim, J.-H.; Seo, M.; David, P. Alleviating Depression Only to Become Problematic Mobile Phone Users: Can Face-to-Face Communication Be the Antidote? Comput. Hum. Behav. 2015, 51, 440–447. [Google Scholar] [CrossRef]
- Van Den Eijnden, R.J.J.M.; Meerkerk, G.-J.; Vermulst, A.A.; Spijkerman, R.; Engels, R.C.M.E. Online Communication, Compulsive Internet Use, and Psychosocial Well-Being among Adolescents: A Longitudinal Study. Dev. Psychol. 2008, 44, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Yen, J.-Y.; Cheng-Fang, Y.; Chen, C.-S.; Chang, Y.-H.; Yeh, Y.-C.; Ko, C.-H. The Bidirectional Interactions between Addiction, Behaviour Approach and Behaviour Inhibition Systems among Adolescents in a Prospective Study. Psychiatry Res. 2012, 200, 588–592. [Google Scholar] [CrossRef] [PubMed]
- Lemola, S.; Perkinson-Gloor, N.; Brand, S.; Dewald-Kaufmann, J.F.; Grob, A. Adolescents’ Electronic Media Use at Night, Sleep Disturbance, and Depressive Symptoms in the Smartphone Age. J. Youth Adolesc. 2015, 44, 405–418. [Google Scholar] [CrossRef]
- Liu, H.; Ji, Y.; Dust, S.B. “Fully Recharged” Evenings? The Effect of Evening Cyber Leisure on next-Day Vitality and Performance through Sleep Quantity and Quality, Bedtime Procrastination, and Psychological Detachment, and the Moderating Role of Mindfulness. J. Appl. Psychol. 2020, 106, 990. [Google Scholar] [CrossRef]
- Huang, T.; Liu, Y.; Tan, T.C.; Wang, D.; Zheng, K.; Liu, W. Mobile Phone Dependency and Sleep Quality in College Students during COVID-19 Outbreak: The Mediating Role of Bedtime Procrastination and Fear of Missing Out. BMC Public Health 2023, 23, 1200. [Google Scholar] [CrossRef]
- You, Z.; Mei, W.; Ye, N.; Zhang, L.; Andrasik, F. Mediating Effects of Rumination and Bedtime Procrastination on the Relationship between Internet Addiction and Poor Sleep Quality. J. Behav. Addict. 2021, 9, 1002–1010. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Royuela-Rico, A.; Macías-Fernández, J. Propiedades Clinimetricas de La Versión Castellana Del Cuestionario de Pittsburgh. Vigilia-Sueño 1997, 9, 81–94. [Google Scholar]
- Brando-Garrido, C.; Montes-Hidalgo, J.; Limonero, J.T.; Gómez-Romero, M.J.; Tomás-Sábado, J. Spanish Version of the Bedtime Procrastination Scale: Cross-Cultural Adaptation and Psychometric Evaluation in a Sample of Nursing Students. Psychol. Rep. 2022, 125, 1765–1779. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.; Lee, J.-Y.; Won, W.-Y.; Park, J.-W.; Min, J.-A.; Hahn, C.; Gu, X.; Choi, J.-H.; Kim, D.-J. Development and Validation of a Smartphone Addiction Scale (SAS). PLoS ONE 2013, 8, e56936. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Fernandez, O. Short Version of the Smartphone Addiction Scale Adapted to Spanish and French: Towards a Cross-Cultural Research in Problematic Mobile Phone Use. Addict. Behav. 2017, 64, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Bulmer, M.G. Principles of Statistics; Courier Corporation: New York, NY, USA, 1979; ISBN 978-0-486-63760-0. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2013; pp. xvii, 507. ISBN 978-1-60918-230-4. [Google Scholar]
- Meshi, D.; Ellithorpe, M.E. Problematic Social Media Use and Social Support Received in Real-Life versus on Social Media: Associations with Depression, Anxiety and Social Isolation. Addict. Behav. 2021, 119, 106949. [Google Scholar] [CrossRef]
- Verbree, A.-R.; Hornstra, L.; Maas, L.; Wijngaards-de Meij, L. Conscientiousness as a Predictor of the Gender Gap in Academic Achievement. Res. High. Educ. 2023, 64, 451–472. [Google Scholar] [CrossRef]
- Busch, P.A.; McCarthy, S. Antecedents and Consequences of Problematic Smartphone Use: A Systematic Literature Review of an Emerging Research Area. Comput. Hum. Behav. 2021, 114, 106414. [Google Scholar] [CrossRef]
- Szymkowiak, A.; Melović, B.; Dabić, M.; Jeganathan, K.; Kundi, G.S. Information Technology and Gen Z: The Role of Teachers, the Internet, and Technology in the Education of Young People. Technol. Soc. 2021, 65, 101565. [Google Scholar] [CrossRef]
- Sirois, F.M.; Nauts, S.; Molnar, D.S. Self-Compassion and Bedtime Procrastination: An Emotion Regulation Perspective. Mindfulness 2019, 10, 434–445. [Google Scholar] [CrossRef]
- Teixeira, L.R.; Lowden, A.; Turte, S.L.; Nagai, R.; Moreno, C.R.; Latorre, M.D.; Marina Fischer, F. Sleep and Sleepiness among Working and Non-Working High School Evening Students. Chronobiol. Int. 2007, 24, 99–113. [Google Scholar] [CrossRef]
- Hynes, M. The Smartphone: A Weapon of Mass Distraction. In The Social, Cultural and Environmental Costs of Hyper-Connectivity: Sleeping Through the Revolution; Emerald Publishing Limited: Bingley, UK, 2021; pp. 71–84. ISBN 978-1-83909-976-2. [Google Scholar]
- Chun, J. Conceptualizing Effective Interventions for Smartphone Addiction among Korean Female Adolescents. Child. Youth Serv. Rev. 2018, 84, 35–39. [Google Scholar] [CrossRef]
- Csibi, S.; Griffiths, M.D.; Demetrovics, Z.; Szabo, A. Analysis of Problematic Smartphone Use Across Different Age Groups within the ‘Components Model of Addiction’. Int. J. Ment. Health Addict. 2021, 19, 616–631. [Google Scholar] [CrossRef]

| Variable | n | % |
|---|---|---|
| Age group | ||
| Young adult (18–25 years) | 134 | 43.4 |
| Adult (26–44 years) | 136 | 44.0 |
| Middle-aged adult (45–60 years) Gender | 39 | 12.6 |
| Women | 148 | 46.8 |
| Men | 165 | 53.2 |
| Occupation | ||
| Student | 125 | 40.3 |
| Worker | 133 | 42.9 |
| Self-employed | 26 | 8.4 |
| Unemployed | 17 | 5.5 |
| Householder/housewife | 2 | 0.6 |
| Other | 7 | 2.3 |
| Level of education | ||
| Early childhood education | 1 | 0.3 |
| Primary education | 4 | 1.3 |
| Secondary education | 101 | 31.6 |
| Higher education | 207 | 66.8 |
| Marital status | ||
| Singled | 145 | 45.5 |
| Married | 162 | 52.6 |
| Divorced | 5 | 1.6 |
| Other | 1 | 0.3 |
| Children | ||
| Yes | 64 | 20.6 |
| No | 249 | 79.4 |
| Use smartphone in bed | ||
| Yes | 247 | 78.7 |
| No | 66 | 21.3 |
| Time spent using a smartphone in bed | ||
| Less than 15 min | 42 | 16.2 |
| Between 16 and 30 min | 90 | 33.2 |
| Between 31 and 60 min | 89 | 34.0 |
| More than 60 min | 41 | 16.6 |
| Smartphone activity in bed | ||
| Calling | 3 | 1.1 |
| Texting | 15 | 5.7 |
| Internet browsing | 59 | 22.4 |
| Social networks | 89 | 33.8 |
| Multimedia entertainment | 82 | 31.2 |
| Videogames | 4 | 1.5 |
| Other | 11 | 4.2 |
| Variable | M | SD |
|---|---|---|
| 1. Sleep quality (PSQI) | 7.5 | 3.6 |
| 2. Problematic smartphone use (SAS-SV) | 29.1 | 10.1 |
| 3. Bedtime procrastination (BPS) | 29.1 | 7.3 |
| 4. Years with a smartphone | 12.0 | 4.3 |
| 5. Daily hours of smartphone use | 5.0 | 2.8 |
| 6. Days per week using the smartphone in bed | 5.9 | 1.9 |
| 7. Time spent using a smartphone in bed | 2.5 | 1.0 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|
| 1. Sleep quality (PSQI) | Coef. | — | ||||||
| p | ||||||||
| 2. Problematic smartphone use (SAS-SV) | Coef. | 0.160 ** | — | |||||
| p | 0.005 | |||||||
| 3. Bedtime procrastination (BPS) | Coef. | 0.298 *** | 0.363 *** | — | ||||
| p | 0.000 | 0.000 | ||||||
| 4. Years with a smartphone | Coef. | −0.065 | −0.034 | −0.140 * | — | |||
| p | 0.254 | 0.547 | 0.014 | |||||
| 5. Daily hours of smartphone use | Coef. | 0.222 ** | 0.358 *** | 0.186 ** | −0.040 | — | ||
| p | 0.000 | 0.000 | 0.001 | 0.487 | ||||
| 6. Days per week of smartphone use in bed | Coef. | −0.006 | 0.201 ** | 0.175 * | −0.017 | 0.183 *** | — | |
| p | 0.922 | 0.001 | 0.005 | 0.784 | 0.004 | |||
| 7. Time spent using a smartphone in bed | Coef. | 0.173 ** | 0.286 *** | 0.347 *** | −0.172 ** | 0.275 *** | 0.288 *** | — |
| p | 0.005 | 0.000 | 0.000 | 0.006 | 0.000 | 0.000 | ||
| 8. Age | Coef. | −0.063 | −0.202 *** | −0.229 *** | 0.548 *** | −0.171 ** | −0.230 *** | −0.221 *** |
| p | 0.268 | 0.000 | 0.000 | 0.000 | 0.003 | 0.000 | 0.000 |
| Variable | Men | Women | t | gl | p | Cohen’s d | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| 1. Sleep quality (PSQI) | 7.5 | 3.6 | 7.6 | 3.6 | 0.210 | 308 | 0.834 | 0.02 |
| 2. Problematic smartphone use (SAS-SV) | 27.4 | 9.9 | 31.0 | 10.0 | 3.248 | 308 | 0.001 | 0.36 |
| 3. Bedtime procrastination (BPS) | 28.7 | 7.1 | 29.5 | 7.5 | 1.031 | 308 | 0.303 | 0.11 |
| 4. Years with a smartphone | 12.7 | 4.3 | 11.3 | 3.8 | −2.311 | 306 | 0.021 | −0.26 |
| 5. Daily hours of smartphone use | 4.7 | 2.4 | 5.8 | 3.2 | 3.115 | 306 | 0.002 | 0.35 |
| 6. Days per week using the smartphone in bed | 6.1 | 1.8 | 6.0 | 1.7 | 0.729 | 253 | 0.467 | 0.09 |
| 7. Time spent using a smartphone in bed | 2.4 | 0.9 | 2.6 | 0.9 | 1.740 | 257 | 0.083 | 0.22 |
| Variable | Young Adults (18–25 Years) | Adults (26–44 Years) | Middle-Aged Adults (45–60 Years) | F(2, 306) | p | η2 | |||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | ||||
| Sleep quality (PSQI) | 7.7 | 3.6 | 7.5 | 3.5 | 6.9 | 3.9 | 0.60 | 0.548 | 0.00 |
| Problematic smartphone use (SAS-SV) | 31.6 | 9.5 | 27.6 | 10.3 | 25.4 | 9.3 | 8.73 | <0.001 | 0.05 |
| Bedtime procrastination (BPS) | 30.7 | 7.6 | 28.3 | 7.0 | 26.2 | 6.3 | 7.15 | 0.001 | 0.05 |
| Variable | Comparison | Mean Diff. | SD | p | 95% CI | |
|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||
| Problematic smartphone use (SAS-SV) | YA vs. A | 4.0 | 1.2 | 0.003 | 1.12 | 6.90 |
| YA vs. MAA | 6.2 | 1.8 | 0.002 | 1.92 | 10.55 | |
| A vs. MAA | 2.2 | 1.8 | 0.651 | −2.09 | 6.52 | |
| Bedtime procrastination (BPS) | YA vs. A | 2.3 | 0.9 | 0.022 | 0.26 | 4.47 |
| YA vs. MAA | 4.4 | 1.3 | 0.002 | 1.30 | 7.60 | |
| A vs. MAA | 2.1 | 1.3 | 0.333 | −1.06 | 5.23 | |
| Effect | B | SE (B) | t | p | 95% CI | |
|---|---|---|---|---|---|---|
| Lower Limit | Upper Limit | |||||
| a: PSU → BP | 0.26 | 0.03 | 6.83 | <0.001 | 1.55 | 3.20 |
| b: BP → PSQ | 0.14 | 0.03 | 4.75 | <0.001 | 0.11 | 0.31 |
| c (total): PSU → PSQ | 0.06 | 0.02 | 2.84 | 0.005 | −0.02 | 1.47 |
| c’ (direct): PSU → PSQ | 0.02 | 0.02 | 1.01 | 0.312 | −0.52 | 1.00 |
| a*b (indirect): PSU → BP → PSQ | 0.04 | 0.02 | 0.05 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Correa-Iriarte, S.; Hidalgo-Fuentes, S.; Martí-Vilar, M. Relationship between Problematic Smartphone Use, Sleep Quality and Bedtime Procrastination: A Mediation Analysis. Behav. Sci. 2023, 13, 839. https://doi.org/10.3390/bs13100839
Correa-Iriarte S, Hidalgo-Fuentes S, Martí-Vilar M. Relationship between Problematic Smartphone Use, Sleep Quality and Bedtime Procrastination: A Mediation Analysis. Behavioral Sciences. 2023; 13(10):839. https://doi.org/10.3390/bs13100839
Chicago/Turabian StyleCorrea-Iriarte, Santiago, Sergio Hidalgo-Fuentes, and Manuel Martí-Vilar. 2023. "Relationship between Problematic Smartphone Use, Sleep Quality and Bedtime Procrastination: A Mediation Analysis" Behavioral Sciences 13, no. 10: 839. https://doi.org/10.3390/bs13100839
APA StyleCorrea-Iriarte, S., Hidalgo-Fuentes, S., & Martí-Vilar, M. (2023). Relationship between Problematic Smartphone Use, Sleep Quality and Bedtime Procrastination: A Mediation Analysis. Behavioral Sciences, 13(10), 839. https://doi.org/10.3390/bs13100839








