The Number of Monthly Night Shift Days and Depression Were Associated with an Increased Risk of Excessive Daytime Sleepiness in Emergency Physicians in South Korea
Abstract
1. Introduction
2. Materials and Methods
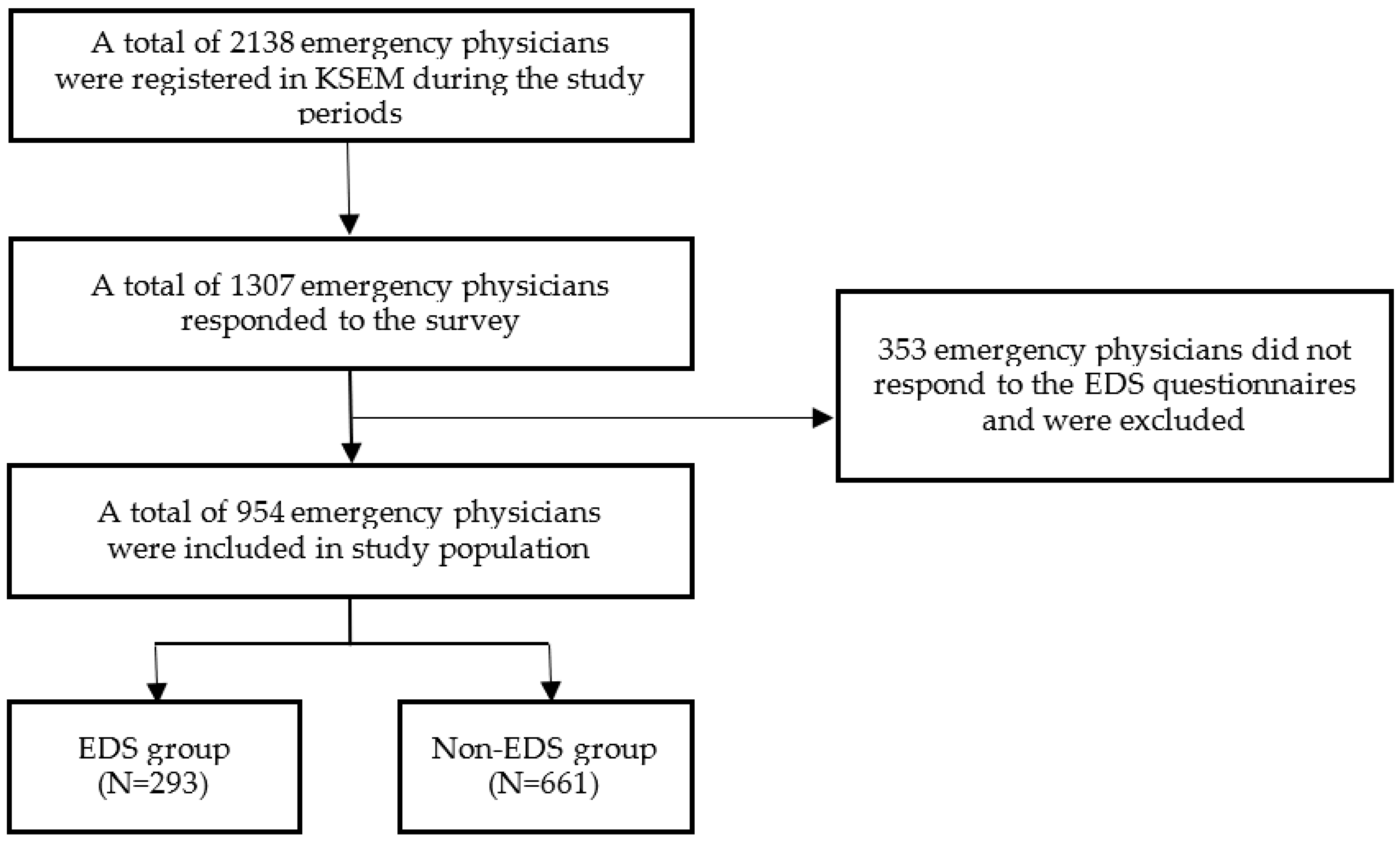
2.1. Study Population
2.2. Study Variables and Measurements
2.3. Study Outcomes
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Participants
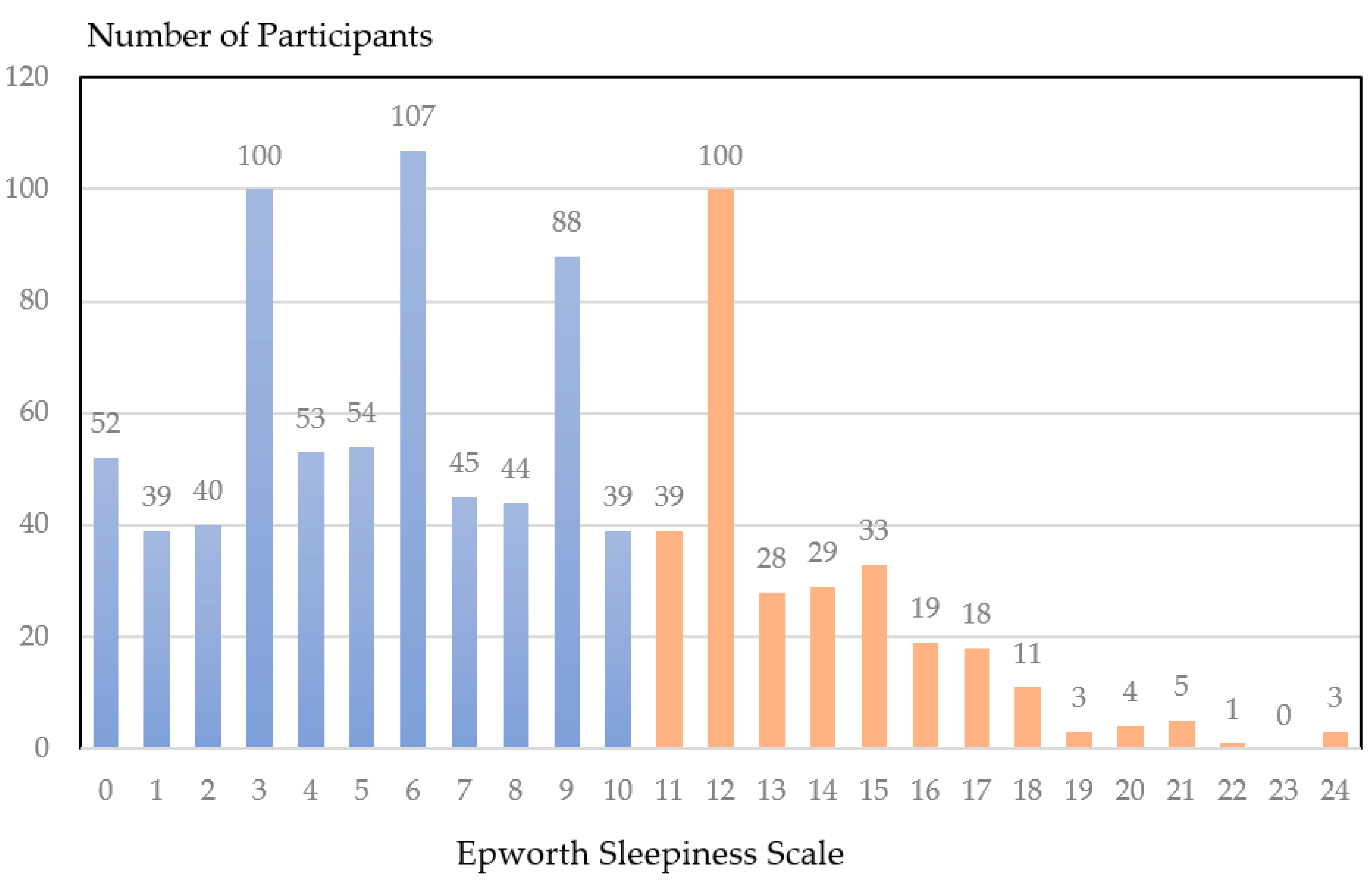
3.2. Prevalence of EDS
3.3. Factors Associated with EDS
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheng, W.-J.; Cheng, Y. Night shift and rotating shift in association with sleep problems, burnout and minor mental disorder in male and female employees. Occup. Environ. Med. 2017, 74, 483–488. [Google Scholar] [CrossRef]
- Havakuk, O.; Zukerman, N.; Flint, N.; Sadeh, B.; Margolis, G.; Konigstein, M.; Keren, G.; Aviram, G.; Shmilovich, H. Shift work and the risk of coronary artery disease: A cardiac computed tomography angiography study. Cardiology 2018, 139, 11–16. [Google Scholar] [CrossRef]
- Su, T.C.; Lin, L.Y.; Baker, D.; Schnall, P.L.; Chen, M.F.; Hwang, W.C.; Chen, C.F.; Wang, J.D. Elevated blood pressure, decreased heart rate variability and incomplete blood pressure recovery after a 12-hour night shift work. J. Occup. Health 2008, 50, 380–386. [Google Scholar] [CrossRef]
- Potter, G.D.; Skene, D.J.; Arendt, J.; Cade, J.E.; Grant, P.J.; Hardie, L.J. Circadian rhythm and sleep disruption: Causes, metabolic consequences, and countermeasures. Endocr. Rev. 2016, 37, 584–608. [Google Scholar] [CrossRef]
- Dawson, D.; Reid, K. Fatigue, alcohol and performance impairment. Nature 1997, 388, 235. [Google Scholar] [CrossRef]
- Joo, E.Y.; Yoon, C.W.; Koo, D.L.; Kim, D.; Hong, S.B. Adverse effects of 24 hours of sleep deprivation on cognition and stress hormones. J. Clin. Neurol. 2012, 8, 146–150. [Google Scholar] [CrossRef]
- Kaneita, Y.; Ohida, T. Association of current work and sleep situations with excessive daytime sleepiness and medical incidents among Japanese physicians. J. Clin. Sleep Med. 2011, 7, 512–522. [Google Scholar] [CrossRef]
- Ng, T.P.; Tan, W.C. Prevalence and determinants of excessive daytime sleepiness in an Asian multi-ethnic population. Sleep Med. 2005, 6, 523–529. [Google Scholar] [CrossRef]
- Chen, L.; Luo, C.; Liu, S.; Chen, W.; Liu, Y.; Li, Y.; Du, Y.; Zou, H.; Pan, J. Excessive daytime sleepiness in general hospital nurses: Prevalence, correlates, and its association with adverse events. Sleep Breath. 2019, 23, 209–216. [Google Scholar] [CrossRef]
- Garbarino, S.; Durando, P.; Guglielmi, O.; Dini, G.; Bersi, F.; Fornarino, S.; Toletone, A.; Chiorri, C.; Magnavita, N. Sleep apnea, sleep debt and daytime sleepiness are independently associated with road accidents. A cross-sectional study on truck drivers. PLoS ONE 2016, 11, e0166262. [Google Scholar] [CrossRef]
- Pack, A.I.; Pack, A.M.; Rodgman, E.; Cucchiara, A.; Dinges, D.F.; Schwab, C.W. Characteristics of crashes attributed to the driver having fallen asleep. Accid. Anal. Prev. 1995, 27, 769–775. [Google Scholar] [CrossRef]
- AlShareef, S.M. Excessive daytime sleepiness and associations with sleep-related motor vehicle accidents: Results from a nationwide survey. Sleep Breath. 2021, 25, 1671–1676. [Google Scholar] [CrossRef]
- Ng, W.L.; Freak-Poli, R.; Peeters, A. The prevalence and characteristics associated with excessive daytime sleepiness among Australian workers. J. Occup. Environ. Med. 2014, 56, 935–945. [Google Scholar]
- Hara, C.; Rocha, F.L.; Lima-Costa, M.F.F. Prevalence of excessive daytime sleepiness and associated factors in a Brazilian community: The Bambuí study. Sleep Med. 2004, 5, 31–36. [Google Scholar] [CrossRef]
- Lee, H.M.; Cho, K.H.; Yang, H.J.; Kim, I.B.; Lee, K.J.; Han, S.B.; Oh, S.H.; Kim, C.; Park, J.S.; Kang, Y.J. Final report of 2015 Korean emergency physician survey (KEPS). J. Korean Soc. Emerg. Med. 2016, 27, 1–24. [Google Scholar]
- Taherdoost, H. Determining sample size; how to calculate survey sample size. Int. J. Econ. Manag. Syst. 2017, 2, 237–239. [Google Scholar]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef]
- Cho, Y.W.; Lee, J.H.; Son, H.K.; Lee, S.H.; Shin, C.; Johns, M.W. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. 2011, 15, 377–384. [Google Scholar] [CrossRef]
- Haddock, C.K.; Poston, W.S.; Jitnarin, N.; Jahnke, S.A. Excessive daytime sleepiness in firefighters in the central United States. J. Occup. Environ. Med. 2013, 55, 416–423. [Google Scholar] [CrossRef]
- Bintliff, S. The adult APGAR: A guide to physician wellness. Int. J. Dermatol. 2012, 7, 868–869. [Google Scholar] [CrossRef]
- Park, S.-J.; Choi, H.-R.; Choi, J.-H.; Kim, K.-W.; Hong, J.-P. Reliability and validity of the Korean version of the Patient Health Questionnaire-9 (PHQ-9). Anxiety Mood 2010, 6, 119–124. [Google Scholar]
- Pedersen, A.B.; Mikkelsen, E.M.; Cronin-Fenton, D.; Kristensen, N.R.; Pham, T.M.; Pedersen, L.; Petersen, I. Missing data and multiple imputation in clinical epidemiological research. Clin. Epidemiol. 2017, 9, 157. [Google Scholar] [CrossRef]
- Albert, J.M.; Nelson, S. Generalized causal mediation analysis. Biometrics 2011, 67, 1028–1038. [Google Scholar] [CrossRef]
- Joo, S.; Baik, I.; Yi, H.; Jung, K.; Kim, J.; Shin, C. Prevalence of excessive daytime sleepiness and associated factors in the adult population of Korea. Sleep Med. 2009, 10, 182–188. [Google Scholar] [CrossRef]
- Ozder, A.; Eker, H.H. The prevalence of excessive daytime sleepiness among academic physicians and its impact on the quality of life and occupational performance. Int. J. Occup. Med. Environ. Health. 2015, 28, 721–730. [Google Scholar] [CrossRef][Green Version]
- Singh, R.; Undevia, N.S.; Schuman, C.; Attarian, H. Excessive daytime sleepiness among attending physicians: A pilot survey study at an academic institution. Sleep Med. 2011, 12, 808–810. [Google Scholar] [CrossRef]
- Alhifzi, S.; Al-Ghonimy, A.; Al Aboudi, M.; Al Abdullah, R.; Olaish, A.; BaHammam, A.S. Assessment of sleep quality, daytime sleepiness, and depression among emergency physicians working in shifts. J. Nat. Sci. Med. 2018, 1, 17. [Google Scholar] [CrossRef]
- Park, S.Y.; Cho, K.H.; Kim, H.J.; Kim, I.B.; Seo, B.S.; Choi, S.J.; Yoon, Y.S.; Key, D.; Park, K.H.; Lee, E.S. Excessive Daytime Sleepiness and Its Associated Factors among Emergency Medicine Residents in South Korea: A Nationwide Survey. Emerg. Med. Int. 2021, 2021, 6628361. [Google Scholar] [CrossRef]
- Barnes, R.; Deacon, S.; Forbes, M.; Arendt, J. Adaptation of the 6-sulphatoxymelatonin rhythm in shiftworkers on offshore oil installations during a 2-week 12-h night shift. Neurosci. Lett. 1998, 241, 9–12. [Google Scholar]
- Midwinter, M.J.; Arendt, J. Adaptation of the melatonin rhythm in human subjects following nightshift work in Antarctica. Neurosci. Lett. 1991, 122, 195–198. [Google Scholar] [CrossRef]
- Ross, J.K.; Arendt, J.; Horne, J.; Haston, W. Night-shift work in Antarctica: Sleep characteristics and bright light treatment. Physiol. Behav. 1995, 57, 1169–1174. [Google Scholar] [CrossRef]
- Gibbs, M.; Hampton, S.; Morgan, L.; Arendt, J. Predicting circadian response to abrupt phase shift: 6-sulphatoxymelatonin rhythms in rotating shift workers offshore. J. Biol. Rhythm. 2007, 22, 368–370. [Google Scholar] [CrossRef]
- Roberts, R.E.; Duong, H.T. The prospective association between sleep deprivation and depression among adolescents. Sleep 2014, 37, 239–244. [Google Scholar] [CrossRef]
- Bixler, E.O.; Vgontzas, A.N.; Lin, H.-M.; Calhoun, S.L.; Vela-Bueno, A.; Kales, A. Excessive daytime sleepiness in a general population sample: The role of sleep apnea, age, obesity, diabetes, and depression. J. Clin. Endocrinol. Metab. 2005, 90, 4510–4515. [Google Scholar] [CrossRef]
- Breslau, N.; Roth, T.; Rosenthal, L.; Andreski, P. Daytime sleepiness: An epidemiological study of young adults. Am. J. Public Health 1997, 87, 1649–1653. [Google Scholar] [CrossRef]
- Huh, S. Will the year 2016 augur well for better patient safety and health of residents in Korea according to the enactment of the Act for improving the resident training environment and enhancing resident’s status? J. Educ. Eval. Health Prof. 2016, 13, 2. [Google Scholar] [CrossRef]
- Sohn, S.; Seo, Y.; Jeong, Y.; Lee, S.; Lee, J.; Lee, K.J. Changes in the working conditions and learning environment of medical residents after the enactment of the Medical Resident Act in Korea in 2015: A national 4-year longitudinal study. J. Educ. Eval. Health Prof. 2021, 18, 7. [Google Scholar] [CrossRef]
- Lang, C.J.; Appleton, S.L.; Vakulin, A.; McEvoy, R.D.; Vincent, A.D.; Wittert, G.A.; Martin, S.A.; Grant, J.F.; Taylor, A.W.; Antic, N. Associations of undiagnosed obstructive sleep apnea and excessive daytime sleepiness with depression: An Australian population study. J. Clin. Sleep Med. 2017, 13, 575–582. [Google Scholar] [CrossRef]
| Participants | Total Group (N = 954) | EDS Group (N = 293) | Non-EDS Group (N = 661) | p-Value | |
|---|---|---|---|---|---|
| Demographic variables | |||||
| Age | 954 | 42.5 ± 6.1 | 42.1 ± 5.7 | 42.7 ± 6.3 | 0.175 |
| Gender | 954 | 0.112 | |||
| Men | 846 (88.7) | 267 (91.1) | 579 (87.6) | ||
| Woman | 108 (11.3) | 26 (8.9) | 82 (12.4) | ||
| Marital status | 945 | 0.632 | |||
| Married | 832 (88.0) | 254 (87.3) | 578 (88.4) | ||
| Others | 113 (12.0) | 37 (12.7) | 76 (11.6) | ||
| Lifestyle variables | |||||
| Alcohol consumption | 945 | 0.233 | |||
| No | 566 (59.9) | 166 (57.0) | 400 (61.2) | ||
| Yes | 379 (40.1) | 125 (43.0) | 254 (38.8) | ||
| Smoking | 948 | 0.034 | |||
| No | 702 (74.1) | 203 (69.5) | 499 (76.1) | ||
| Yes | 246 (25.9) | 89 (30.5) | 157 (23.9) | ||
| Number of exercises per week | 954 | 1.8 ± 1.8 | 1.7 ± 1.9 | 1.8 ± 1.8 | 0.367 |
| Regular breakfast a | 947 | 2.5 ± 1.4 | 2.5 ± 1.3 | 2.5 ± 1.4 | 0.561 |
| Regular night snacks a | 947 | 2.7 ± 1.2 | 2.9 ± 1.2 | 2.6 ± 1.3 | 0.004 |
| Workloads and working environment variables | |||||
| ED volume c | 884 | 34,375.6 ± 20,317.8 | 36,280.8 ± 20,831.2 | 33,393.9 ± 21,975.8 | 0.042 |
| Monthly working days | 954 | 11.7 ± 4.2 | 11.6 ± 3.8 | 11.7 ± 4.3 | 0.918 |
| Monthly night-shift days | 954 | 5.9 ± 2.4 | 6.2 ± 2.2 | 5.7 ± 2.5 | 0.007 |
| Monthly working hours | 954 | 152.8 ± 51.0 | 151.1 ± 57.9 | 153.6 ± 47.6 | 0.480 |
| ED safety a | 903 | 2.9 ± 1.0 | 2.8 ± 1.0 | 3.0 ± 1.1 | 0.054 |
| Mealtime guaranteed a | 950 | 2.5 ± 1.2 | 2.4 ± 1.1 | 2.6 ± 1.2 | 0.013 |
| Schedule satisfaction b | 949 | 3.4 ± 0.9 | 3.3 ± 0.9 | 3.5 ± 0.9 | <0.001 |
| Income satisfaction b | 954 | 2.8 ± 1.0 | 2.6 ± 1.0 | 2.8 ± 1.0 | 0.008 |
| Job satisfaction b | 882 | 3.2 ± 0.9 | 3.2 ± 0.9 | 3.3 ± 1.0 | 0.235 |
| Sleep and health-related variables | |||||
| Sleep hours | 954 | 7.3 ± 1.4 | 7.3 ± 1.4 | 7.4 ± 1.4 | 0.285 |
| Sleep quality | 951 | <0.001 | |||
| Not very worried | 80 (8.4) | 15 (5.1) | 65 (9.9) | ||
| Not worried | 193 (20.3) | 37 (12.7) | 156 (23.7) | ||
| Fair | 232 (24.4) | 64 (21.9) | 168 (25.5) | ||
| Worried | 293 (30.8) | 109 (37.3) | 184 (27.9) | ||
| Very worried | 153 (16.1) | 67 (22.9) | 86 (13.1) | ||
| Health perspective | 949 | <0.001 | |||
| Very unhealthy | 26 (2.7) | 13 (4.5) | 13 (2.0) | ||
| Unhealthy | 178 (18.8) | 81 (27.8) | 97 (14.7) | ||
| Fair | 423 (44.6) | 121 (41.6) | 302 (45.9) | ||
| Healthy | 280 (29.5) | 68 (23.4) | 212 (32.3) | ||
| Very healthy | 42 (4.4) | 8 (2.7) | 34 (5.2) | ||
| Wellness | 907 | <0.001 | |||
| APGAR score > 5 | 311 (34.3) | 67 (23.8) | 244 (39.0) | ||
| APGAR score ≤ 5 | 596 (65.7) | 215 (76.2) | 381 (61.0) | ||
| Depression | 908 | <0.001 | |||
| PHQ-9 < 11 | 650 (71.6) | 147 (51.9) | 503 (80.5) | ||
| PHQ-9 ≥ 11 | 258 (28.4) | 136 (48.1) | 122 (19.5) |
| Univariable Logistic Regression | Multivariable Logistic Regression | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Demographic variables | ||||
| Age | 0.984 | 0.962–1.007 | 0.987 | 0.957–1.017 |
| Gender | ||||
| Male | 1.000 | 1.000 | ||
| Female | 0.688 | 0.432–1.094 | 1.714 | 0.996–2.949 |
| Marital status | ||||
| Married | 1.000 | 1.000 | ||
| Others | 1.065 | 0.723–1.099 | 1.062 | 0.650–1.736 |
| Lifestyle variables | ||||
| Alcohol consumption | ||||
| No | 1.000 | 1.000 | ||
| Yes | 1.192 | 0.900–1.579 | 0.909 | 0.656–1.259 |
| Smoking | ||||
| No | 1.000 | 1.000 | ||
| Yes | 1.389 | 1.022–1.888 | 0.786 | 0.548–1.125 |
| Number of exercises per week | 0.966 | 0.895–1.042 | 1.050 | 0.962–1.147 |
| Regular breakfast a | 0.970 | 0.876–1.074 | 1.807 | 0.964–1.226 |
| Regular night snack a | 1.177 | 1.052–1.317 | 1.080 | 0.952–1.224 |
| Workloads and working environment variables | ||||
| ED volume c | 1.000 | 1.000–1.000 | 1.000 | 1.000–1.000 |
| Monthly working days | 0.998 | 0.966–1.032 | 0.995 | 0.953–1.040 |
| Monthly night-shift days | 1.084 | 1.022–1.149 | 1.106 | 1.028–1.191 |
| Monthly working hours | 0.999 | 0.996–1.002 | 0.998 | 0.994–1.001 |
| ED safety a | 0.870 | 0.756–1.002 | 0.891 | 0.749–1.060 |
| Mealtime guaranteed a | 0.864 | 0.769–0.970 | 0.965 | 0.844–1.105 |
| Schedule satisfaction b | 0.760 | 0.651–0.888 | 0.959 | 0.774–1.188 |
| Income satisfaction b | 0.827 | 0.718–0.953 | 0.904 | 0.743–1.100 |
| Job satisfaction b | 0.911 | 0.780–1.063 | 1.209 | 0.989–1.478 |
| Sleep and health-related variables | ||||
| Sleep hours | 0.947 | 0.856–1.047 | 0.988 | 0.882–1.106 |
| Sleep quality | ||||
| Not very worried | 1.000 | 1.000 | ||
| Not worried | 1.035 | 0.531–2.019 | 0.634 | 0.305–1.319 |
| Fair | 1.648 | 0.874–3.106 | 0.560 | 0.318–0.985 |
| Worried | 2.569 | 1.391–4.745 | 0.796 | 0.486–1.303 |
| Very worried | 3.366 | 1.760–6.436 | 0.996 | 0.638–1.556 |
| Health perspective | ||||
| Very unhealthy | 1.000 | 1.000 | ||
| Unhealthy | 0.842 | 0.369–1.921 | 1.970 | 0.565–6.870 |
| Fair | 0.410 | 0.184–0.911 | 1.666 | 0.661–4.200 |
| Healthy | 0.328 | 0.145–0.740 | 1.262 | 0.526–3.041 |
| Very healthy | 0.236 | 0.080–0.700 | 1.416 | 0.590–3.398 |
| Wellness | ||||
| APGAR score > 5 | 1.000 | 1.000 | ||
| APGAR score ≤ 5 | 2.029 | 1.484–2.776 | 1.395 | 0.953–2.043 |
| Depression | ||||
| PHQ-9 < 11 | 1.000 | 1.000 | ||
| PHQ-9 ≥ 11 | 3.570 | 2.635–4.835 | 2.635 | 1.799–3.861 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.Y.; Lee, H.M.; Kim, J. The Number of Monthly Night Shift Days and Depression Were Associated with an Increased Risk of Excessive Daytime Sleepiness in Emergency Physicians in South Korea. Behav. Sci. 2022, 12, 279. https://doi.org/10.3390/bs12080279
Park SY, Lee HM, Kim J. The Number of Monthly Night Shift Days and Depression Were Associated with an Increased Risk of Excessive Daytime Sleepiness in Emergency Physicians in South Korea. Behavioral Sciences. 2022; 12(8):279. https://doi.org/10.3390/bs12080279
Chicago/Turabian StylePark, Song Yi, Hyung Min Lee, and Jiyoung Kim. 2022. "The Number of Monthly Night Shift Days and Depression Were Associated with an Increased Risk of Excessive Daytime Sleepiness in Emergency Physicians in South Korea" Behavioral Sciences 12, no. 8: 279. https://doi.org/10.3390/bs12080279
APA StylePark, S. Y., Lee, H. M., & Kim, J. (2022). The Number of Monthly Night Shift Days and Depression Were Associated with an Increased Risk of Excessive Daytime Sleepiness in Emergency Physicians in South Korea. Behavioral Sciences, 12(8), 279. https://doi.org/10.3390/bs12080279






