Professional Quality of Life of Healthcare Workers in Hospital Emergency Departments
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.3. Data Collection
2.4. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weibel, L.; Gabrion, I.; Aussedat, M.; Kreutz, G. Work-related stress in an emergency medical dispatch center. Ann. Emerg. Med. 2003, 41, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Quijano, S.; Navarro, J.; Yepes, M.; Berger, R.; Romeo, M. La auditoría del sistema humano (ASH) para el análisis del comportamiento humano en las organizaciones. [Auditing the human system (ASH) for the analysis of human behavior in organizations]. Pap. De Psicol. 2008, 29, 92–106. [Google Scholar]
- Aguado, J.I.; Bátiz, A.; Quintana, S. El estrés en el personal sanitario de los hospitales: Situación actual. [Stress in hospital health personnel: Current status]. Med. Y Segur. Del Trab. 2013, 59, 259–275. [Google Scholar] [CrossRef][Green Version]
- Chóliz, M. Ansiedad y trastornos del sueño [Anxiety and sleep disorders]. In Emociones y salud [Emotions and Health]; Fernández-Abascal, E.G., Palmero, F., Eds.; Ariel: Barcelona, Spain, 1999; pp. 159–182. [Google Scholar]
- Reimer, M.A.; Flemons, W.W. Quality of life in sleep disorders. Sleep Med. Rev. 2003, 7, 335–349. [Google Scholar] [CrossRef]
- Chen, Y.S.; Chen, M.C.; Chou, F.H.C.; Sun, F.C.; Chen, P.C.; Tsai, K.Y.; Chao, S.S. The relationship between quality of life and posttraumatic stress disorder or major depression for firefighters in Kaohsiung, Taiwan. Qual. Life Res. 2007, 16, 1289–1297. [Google Scholar] [CrossRef]
- Angelo, R.P.; Chambel, M.J. The reciprocal relationship between work characteristics and employee burnout and engagement: A longitudinal study of firefighters. Stress Health 2015, 31, 106–114. [Google Scholar] [CrossRef]
- Carbonel-Siam, A.T.; Torres-Valle, A. Evaluación de la percepción del riesgo laboral. [Evaluation of occupational risk perception]. Ing. Mecánica 2010, 13, 18–25. [Google Scholar]
- Kripke, D.F.; Garfinkel, L.; Wingard, D.L.; Klauber, M.R.; Marler, M.R. Mortality associated with sleep duration and insomnia. Arch. Gen. Psychiatry 2002, 59, 131–136. [Google Scholar] [CrossRef]
- Kupfer, D.J.; Reynolds, C.F. Management of insomnia. N. Engl. J. Med. 1997, 336, 341–346. [Google Scholar] [CrossRef]
- Nowell, P.D.; Mazumdar, S.; Buysse, D.J.; Dew, M.A.; Reynolds, C.F.; Kupfer, D.J. Benzodiazepines and zolpidem for chronic insomnia. A meta-analysis of treatment efficacy. JAMA 1997, 278, 2170–2177. [Google Scholar] [CrossRef]
- Taylor, D.J.; Lichstein, K.L.; Durrence, H.H.; Reidel, B.W.; Bush, A.J. Epidemiology of insomnia, depression, and anxiety. Sleep 2005, 28, 1457–1464. [Google Scholar] [CrossRef]
- Wu, Y.; Zhai, L.; Zhang, D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep Med. 2014, 15, 1456–1462. [Google Scholar] [CrossRef]
- Holland, B.; Gosselin, K.; Mulcahy, A. The effect of autogenic training on self-efficacy, anxiety, and performance on nursing student simulation. Nurs. Educ. Perspect. 2017, 38, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Molero, M.M.; Pérez-Fuentes, M.C.; Oropesa, N.F.; Simón, M.M.; Gázquez, J.J. Self-efficacy and emotional intelligence as predictors of perceived stress in nursing professionals. Medicina 2019, 55, 237. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; W.H. Freeman and Company: Nueva York, NY, USA, 1997. [Google Scholar]
- Contreras, F.; Espinosa, J.C.; Esguerra, G.; Haikal, A.; Polanía, A.; Rodríguez, A. Autoeficacia, ansiedad y rendimiento académico en adolescents. [Self-efficacy, anxiety and academic performance in adolescents]. Divers. Perspect. En Psicol. 2005, 1, 183–194. [Google Scholar] [CrossRef]
- Gerin, W.; Litt, M.D.; Deich, J.; Pickering, T.G. Self-efficacy as a moderator of perceived control effects on cardiovascular reactivity: Is enhanced control always beneficial? Psychosom. Med. 1995, 57, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Gollwitzer, P.M.; Bargh, J.A. The Psychology of Action: Linking Cognition and Motivation to Behavior; The Guilford Press: New York, NY, USA, 1996. [Google Scholar]
- Fiabane, E.; Giorgi, I.; Sguazzin, C.; Argentero, P. Work engagement and occupational stress in nurses and other healthcare workers: The role of organisational and personal factors. J. Clin. Nurs. 2013, 22, 2614–2624. [Google Scholar] [CrossRef]
- Cortés, J.A.; Martín, J.; Morente, M.; Caboblanco, M.; Garijo, J.; Rodríguez, A. Clima laboral en atención primaria: ¿qué hay que mejorar? [Work climate in primary care: What needs to be improved?]. Atención Primaria 2003, 32, 288–295. [Google Scholar] [CrossRef]
- Fernández, M.I.; Villagrasa, J.R.; Gamo, M.; Vázquez, J.; Cruz, E.; Aguirre, M.V.; Andradas, V. Estudio de la satisfacción laboral y sus determinantes en trabajadores sanitarios de un área de Madrid. [Study of job satisfaction and its determinants in healthcare workers in an area of Madrid]. Rev. Española De Salud Pública 1995, 69, 487–497. [Google Scholar]
- Fernández, M.I.; Moinelo, A.; Villanueva, A.; Andrade, C.; Rivera, M.; Gómez, J.M.; Parrilla, O. Satisfacción laboral de los profesionales de Atención Primaria del Área 10 del Insalud de Madrid. [Job satisfaction of Primary Care professionals in Area 10 of Insalud de Madrid.]. Rev. Española De Salud Pública 2000, 74, 139–147. [Google Scholar] [CrossRef]
- Alonso, M.; Iglesias, A.I.; Franco, A. Percepción de la calidad de vida profesional en un área sanitaria de Asturias. [Perception of professionals’ quality of life in the Asturias a Health Care Area, Spain]. Atención Primaria 2002, 30, 483–489. [Google Scholar] [CrossRef][Green Version]
- Vega-Escaño, J.; Porcel-Gálvez, A.M.; Barrientos-Trigo, S.; Romero-Sánchez, J.M.; Diego-Cordero, R. La turnicidad como factor determinante en la aparición de insomnio en población laboral: Revisión sistemática. [Turnicity as a determining factor in the occurrence of insomnia in the working population: A systematic review]. Rev. Española De Salud Pública 2020, 94, 132. [Google Scholar]
- Ruotsalainen, J.H.; Verbeek, J.H.; Mariné, A.; Serra, C. Preventing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2015, 13, CD002892. [Google Scholar] [CrossRef] [PubMed]
- Bridgeman, P.J.; Bridgeman, M.B.; Barone, J. Burnout syndrome among healthcare professionals. Am. J. Health Syst. Pharm. 2018, 75, 147–152. [Google Scholar] [CrossRef]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef]
- Yates, S.W. Physician Stress and Burnout. Am. J. Med. 2020, 133, 160–164. [Google Scholar] [CrossRef]
- Friganović, A.; Selič, P.; Ilić, B.; Sedić, B. Stress and burnout syndrome and their associations with coping and job satisfaction in critical care nurses: A literature review. Psychiatr. Danub. 2019, 31 (Suppl. 1), 21–31. [Google Scholar]
- Pérez-Valdecantos, D.; Caballero-García, A.; Del Castillo-Sanz, T.; Bello, H.J.; Roche, E.; Córdova, A. Stress salivary biomarkers variation during the work day in Emergencies in healthcare professionals. Int. J. Environ. Res. Public Health 2021, 18, 3937. [Google Scholar] [CrossRef]
- Pérez-Valdecantos, D.; Caballero-García, A.; Del Castillo-Sanz, T.; Bello, H.J.; Roche, E.; Roche, A.; Córdova, A. Variations in salivary stress biomarkers and their relationship with anxiety, self-efficacy and sleeping quality in Emergency health care professionals. Int. J. Environ. Res. Public Health 2021, 18, 9277. [Google Scholar] [CrossRef]
- Martín-Fernández, J.; Gómez-Gascón, T.; Martínez-García-Olalla, C.; del Cura-González, M.I.; Cabezas-Peña, M.C.; García-Sánchez, S. Medición de la capacidad evaluadora del cuestionario CVP-35 para la percepción de la calidad de vida profesional. Aten Primaria 2008, 40, 327–334. [Google Scholar] [CrossRef][Green Version]
- Karasek, R. The political implications of psychosocial work redesign: A model of the psychosocial class structure. Int. J. Health Serv. 1989, 19, 481–508. [Google Scholar] [CrossRef] [PubMed]
- Cabezas-Peña, C. La calidad de vida de los profesionales. FMC 2000, 7 (Suppl. 7), 53–68. [Google Scholar]
- Martín, J.; Cortés, J.A.; Morente, M.; Caboblanco, M.; Garijo, J.; Rodríguez, A. Características métricas del cuestionario de calidad de vida profesional. [Metric characteristics of the Quality of Professional Life Questionnaire] (CVP-35). Gac. Sanit. 2004, 18, 129–136. [Google Scholar] [CrossRef]
- Hammer, J.S.; Jones, J.W.; Lyons, J.S.; Sixsmith, D.; Afficiando, E. Measurement of occupational stress in hospital settings: Two validity studies of a measure of self-reported stress in medical emergency rooms. Gen. Hosp. Psychiatry 1985, 7, 156–162. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. Manual STAI, Cuestionario de Ansiedad Estado Rasgo; TEA Ediciones: Madrid, Spain, 1982. [Google Scholar]
- Baessler, J.; Schwarcer, R. Evaluación de la autoeficacia: Adaptación española de la escala de Autoeficacia General. Ansiedad Y Estrés 1996, 2, 1–8. [Google Scholar]
- Bobes, J.; González, M.P.; Sáiz, P.A.; Bascarán, M.T.; Iglesias, C.; Fernández, J.M. Propiedades psicométricas del cuestionario Oviedo de sueño. Psicothema 2000, 12, 107–112. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 1988. [Google Scholar]
- Simon, M.; Molero, M.; Perez-Fuentes, M.; Gazquez, J.; Barragan, A.; Martos, A. Análisis de la relación entre el apoyo social percibido, la autoestima global y la autoeficacia general. [Analysis of the relationship between perceived social support, global self-esteem and general self-efficacy]. Eur. J. Health Res. 2017, 3, 137–149. [Google Scholar] [CrossRef]
| Professionals | n | % (Gender) |
|---|---|---|
| n | 97 | 20.6/79.4 (M/W) |
| Profession | ||
| Nurses | 59 | 60.1 |
| Medical doctors | 38 | 39.9 |
| Place of work | ||
| HCUV | 45 | 46.4 |
| HSBS | 52 | 53.6 |
| Ages (Years) | |
|---|---|
| All participants | 38.6 + 11.9 |
| Nurses | 39.0 ± 13.2 |
| Medical doctors | 39.6 ± 13.5 |
| HCUV | 34.7 ± 9.7 |
| HSBS | 42.4 ± 12.5 |
| Men | 39.9 ± 15.2 |
| Women | 39.5 ± 12.1 |
| Test | Score | Result |
|---|---|---|
| MPSS-R | 65.6 | High working stress |
| STAI state/trait | 25.2/24.7 | Low anxiety |
| Self-efficacy | 29.3 | High efficacy level |
| COS | 4.1 | Optimal subjective satisfaction of sleep |
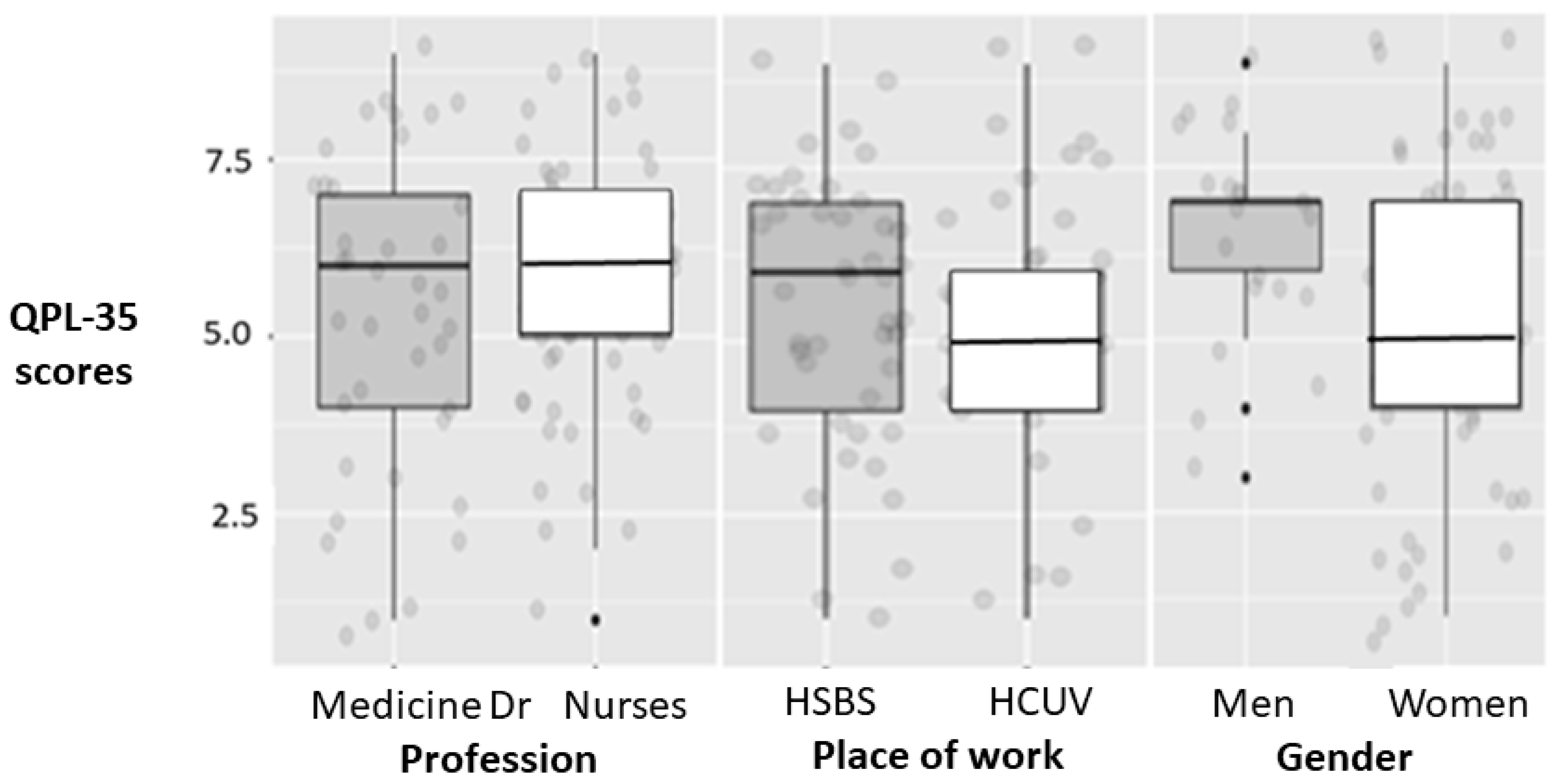
| Dimension 1: Managerial Support | Dimension 2: Workloads | Dimension 3: Intrinsic Motivation | Overall Perceived Quality of Professional Life | |
|---|---|---|---|---|
| Women | 7.6 ± 1.9 | 6.5 ± 1.4 | 8.1 ± 0.9 | 5.4 ± 2.0 |
| Men | 7.2 ± 2.4 | 6.0 ± 2.1 | 7.5 ± 1.8 | 6.0 ± 2.3 |
| Nurse | 7.0 ± 2.0 | 6.3 ± 1.7 | 8.0 ± 1.3 | 5.8 ± 2.0 |
| Medical Dr | 7.6 ± 2.4 | 6.4 ± 1.8 | 7.8 ± 1.6 | 5.1 ± 2.3 |
| HCUV | 8.0 ± 2.1 | 6.4 ± 1.7 | 8.3 ± 0.9 | 5.5 ± 1.2 |
| HSBS | 7.2 ± 1.8 | 6.7 ±1.4 | 7.8 ± 1.0 | 5.5 ± 2.0 |
| TOTAL | 7.5 ± 1.9 | 6.8 ± 1.5 | 8.0 ± 1.0 | 5.6 ± 2.0 |
| Group Comparison | Dimension 1: Managerial Support | Dimension 2: Workloads | Dimension 3: Intrinsic Motivation | Overall Perceived Quality of Professional Life |
|---|---|---|---|---|
| Men vs. Women | −0.06 | 0.27 | −0.45 | 0.64 |
| Medical Dr vs. Nurses | −0.06 | 0.44 | −0.35 | −0.25 |
| HCUV vs. HSBS | 0.03 | −0.18 | −0.08 | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Valdecantos, D.; Caballero-García, A.; Bello, H.J.; Noriega-González, D.; Palomar-Ciria, N.; Roche, A.; Roche, E.; Córdova-Martínez, A. Professional Quality of Life of Healthcare Workers in Hospital Emergency Departments. Behav. Sci. 2022, 12, 188. https://doi.org/10.3390/bs12060188
Pérez-Valdecantos D, Caballero-García A, Bello HJ, Noriega-González D, Palomar-Ciria N, Roche A, Roche E, Córdova-Martínez A. Professional Quality of Life of Healthcare Workers in Hospital Emergency Departments. Behavioral Sciences. 2022; 12(6):188. https://doi.org/10.3390/bs12060188
Chicago/Turabian StylePérez-Valdecantos, Daniel, Alberto Caballero-García, Hugo J. Bello, David Noriega-González, Nora Palomar-Ciria, Alba Roche, Enrique Roche, and Alfredo Córdova-Martínez. 2022. "Professional Quality of Life of Healthcare Workers in Hospital Emergency Departments" Behavioral Sciences 12, no. 6: 188. https://doi.org/10.3390/bs12060188
APA StylePérez-Valdecantos, D., Caballero-García, A., Bello, H. J., Noriega-González, D., Palomar-Ciria, N., Roche, A., Roche, E., & Córdova-Martínez, A. (2022). Professional Quality of Life of Healthcare Workers in Hospital Emergency Departments. Behavioral Sciences, 12(6), 188. https://doi.org/10.3390/bs12060188









