Abstract
Dementia-related suicide is not well known. This study aimed to understand the characteristics of suicide risk among people with dementia and dementia family caregivers in South Korea. According to a systematic review of PRISMA guidelines, six electronic databases were searched for research published from 2010 to 2021. Ten studies were included. Among the included studies on people with dementia, one study (25%) showed no increase in the death risk of suicide, while three studies (75%) revealed suicide risk. Furthermore, in the dementia family caregivers, one study (17%) reported suicides and five studies (83%) reported suicide ideation (SI). Early dementia and independence or partial dependence in activities of daily living and home-based care are related to suicide risk in people with dementia. Meanwhile, suicide risk in dementia family caregivers is related to care burden, dementia severity, and poor approaches to coping with the family member’s dementia. The studies reviewed, which demonstrate heterogenous methodologies, suggest that both people with dementia and dementia family caregivers face suicide risk. The results of the current study offer insights useful for the prevention and treatment of mental health issues in both groups.
1. Introduction
Some studies reported that, among dementias, Alzheimer’s disease was not associated with a major risk of acting out, except in subjects with relatively concomitant depressive symptoms and evidence of hopelessness [1]. People with dementia are unlikely to attempt suicide because their cognitive impairment impacts suicidal ideation (SI) and implementation; consequently, dementia is not considered a risk factor for suicide [2]. By contrast, the risk appears more clearly in behavioral variant frontotemporal dementia (bvFTD) [3]. SI and suicides have been continually reported among people with dementia in Western and Asian countries [2,4,5,6].
Suicide risk in dementia patients may arise from various factors, such as dementia stage; race; a history of diagnosed depression or other psychiatric illnesses; and previous suicide attempts [4,7]. Notably, the number of suicides among people with dementia in South Korea increased from 555 in 2013 to 598 in 2017; cumulative suicides among people with dementia over this five-year period have been estimated at 2958 which accounted for 3.6% of all suicides among Korean individuals with mental illnesses [8].
A notable factor in reducing suicide risk in older adults is the presence of family members who can act as “gatekeepers” [9]. However, dementia family caregivers themselves experience SI [10,11] and homicidal ideation [10,12]. Their care difficulties are associated with uncertain prognosis, treatment, dementia symptom-related stress, and endless care [10,13,14,15]. The health and economic burden of people with dementia under the age of 64 years is rapidly increasing in the city of Seoul, South Korea [16]. The burden of caring for a family member with dementia increases as the symptoms worsen in people with dementia [14]. Support costs for a patient with very mild dementia have been reported to be twice as low as for a patient with severe dementia [17]; the more severe the dementia, the greater the financial burden on the family. The care burden is highly likely to be linked to the primary caregivers’ depression [14]. In a previous study [18], 75% of family caring for people with dementia reported depression.
Moreover, although depression and anxiety management are required for suicide prevention in people with dementia [4], there is lack of a professional medical system that can treat and manage the mental health of people with dementia [15]. In addition, it has been reported that people with dementia and dementia family caregivers differently exhibit SI [2,4,10,11]. It is known that dementia family caregivers have high caring stress, but the factors that put them at risk of suicide have rarely been studied.
Despite people with dementia and dementia family caregivers facing problems that may lead to suicide, research on suicide risk in these groups is lacking in both Western and Korean contexts. Although some studies have examined suicide risk among people with dementia and dementia family caregivers in Korea, to the best of our knowledge, no systematic reviews have been conducted. Korea is a rapidly aging society with a growing number of people with dementia; therefore, it is crucial to develop a comprehensive understanding of suicide risk in people with dementia and dementia family caregivers in Korea. Thus, this study aimed to synthesize the characteristics of suicide risk for people with dementia and dementia family caregivers in Korea over the last ten years (2010–2021).
2. Materials and Methods
2.1. Literature Search Strategy
This study complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [19]. Six search engine databases—the Korea Citation Index (KCI), earticle, Google Scholar, Web of Science, PubMed, and PsycINFO—were used for this review. A search was performed with (AND/OR/NOT). KCI, earticle, and Google Scholar were searched for Korean-language studies using Korean keywords, including (dementia AND suicide) OR (dementia elderly AND suicide) and (dementia family AND suicide) OR (dementia family AND suicide risk). The Web of Science, PubMed, and PsycINFO databases were searched using English keywords, including (dementia AND suicide AND South Korea) OR (dementia elderly AND suicide AND South Korea) and (dementia family AND suicide AND South Korea) OR (dementia family AND suicide risk AND South Korea).
2.2. Eligibility Criteria
The authors set the inclusion and exclusion criteria for the selected studies. The inclusion criteria were as follows: (1) target of people with dementia and dementia family caregivers in South Korea, (2) suicide risk outcome (e.g., suicidal behavior or SI) in the target population, (3) qualitative and quantitative methods (e.g., suicide-related case analyses, cross-sectional studies, cohort studies), (4) articles with original data (i.e., not reviews, systematic reviews, or meta-analyses), (5) peer-reviewed published studies written in Korean or English, and (6) published between 2010 and 2021. The exclusion criteria were as follows: (1) did not present suicide-related outcomes of people with dementia and dementia family caregivers, (2) non-South Korean participants, and (3) published outside the study extraction period.
2.3. Analytical Process
The study selection process was recorded using an Excel spreadsheet and is illustrated using the PRISMA flow chart [20]. Studies were selected for review only if the authors reached a consensus. Collected data included information on SI, SA, and suicides among people with dementia and dementia family caregivers and the included studies collected data using both qualitative and quantitative methods.
2.4. Study Selection
Six search engines were used to search for the above mentioned keywords. Study selection was performed by each author and duplicate studies were removed. Thereafter, the titles and abstracts were evaluated based on the inclusion and exclusion criteria, such as measurable outcomes of suicide risk and the participation of people with dementia and dementia family caregivers.
2.5. Quality Appraisal and Assessment
The types of studies in the review included cohort, qualitative, and cross-sectional studies. Thus, the present study used the Mixed Methods Appraisal Tool (MMAT), which is used to assess the quality of qualitative, quantitative, and mixed research [21]. The MMAT includes criteria such as whether the research questions and data are presented clearly and in a suitable manner for the type of research. Both authors performed quality appraisals on the selected studies using the MMAT. When the authors disagreed, a final decision was made after discussion.
2.6. Data Extraction and Synthesis
The authors performed data extraction on the included studies based on the Cochrane data extraction forms [22]. The data extraction process was performed according to the study focus, study type, characteristics of the dementia family caregivers and people with dementia, prevalence of suicide risk, risk or protective factors, and outcomes. Each author conducted data extraction for all included studies and recorded the results in an additional file. Subsequently, the differences between the authors’ data extraction results were analyzed and resolved through reconfirmation and communication.
3. Results
3.1. Search Outcome
The initial search yielded 143 studies with the required keywords; 48 studies remained after removing duplicates. Assessment of the selected studies based on whether they met the inclusion and exclusion criteria for this review resulted in 11 studies remaining. During the study selection process, one study involved suicide prevention and was thus excluded as it did not meet the criteria. Finally, 10 studies with full text were selected for this review (Figure 1).
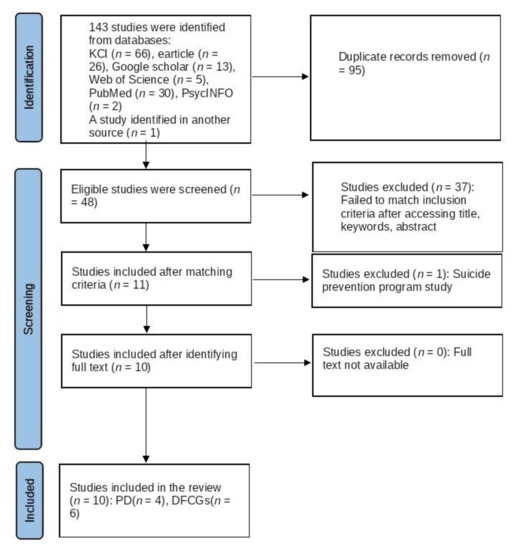
Figure 1.
PRISMA flow diagram of studies on suicide risk among people with dementia and dementia family caregivers. PD: People with dementia. DFCGs: Dementia family caregivers.
3.2. Quality of Methodology
The Appendix A presents the quality assessment results for each included study (Table A1). In this review, the criteria for qualitative studies and quantitative non-randomized studies were included among the MMAT methodological quality criteria according to the study design. The MMAT quality appraisal was applied to qualitative studies (n = 2), including news article analyses, cohort studies (n = 3), and quantitative studies (n = 5). Most studies were evaluated as appropriate.
3.3. Characteristics of Included Studies on People with Dementia and Dementia Family Caregivers
Of the ten studies in this review (Table 1), seven were written in Korean [6,12,23,24,25,26,27] and three in English [5,28,29]. All included studies analyzed Korean data. Four studies focused on people with dementia [5,6,28,29], analyzing the characteristics of SI [6] and suicides [5,28,29] in people with dementia using quantitative and cohort research methods. Six studies focused on dementia family caregivers [12,23,24,25,26,27]; of these, four investigated SI using quantitative methods [24,25,26,27] and one used focus group interviews and addressed dementia family caregivers’ SI [12]. Only one study conducted a content analysis of newspaper articles to uncover suicides in dementia family caregivers [23]. Of the six dementia family caregiver studies, one study focused only on spouses [26] and one [24] on adult children; the remaining studies focused on both spouses and adult children [12,23].

Table 1.
Characteristics of suicide risk among people with dementia and dementia family caregivers.
3.4. People with Dementia
3.4.1. Gender and Age
Kim and Hyun [6] studied 298 participants who were long-term care registered in nursing and home-based care facilities with other condition. One study [5], which used the National Health Insurance Service Senior Cohort data from 2004 to 2012 for people with dementia, included 36,541 people with dementia. In both studies [5,6], women comprised a higher proportion of the sample than men. Regarding age, the mean age was 84.1 years in one study [6] and people with dementia aged 75 years or more accounted for 69.5% of the sample in the other study [5]. Two other studies [28,29] addressed the gender and age composition of suicide in people with dementia or mild cognitive impairment. Men accounted for 42.2% in one study [28], with a mean age of 71.42 years. In the other study [29], the suicide rate for men was higher than that for women, and the suicide rate for those in their 60s was higher than that for those in their 80s.
3.4.2. Dementia Severity and Heath Condition
In four studies, participants were restricted to people diagnosed with dementia, prescribed antidementia drugs, registered with the Clinical Research Center for Dementia of Korea, or with a dementia related conditions [5,6,28,29]. In three studies, Mini-Mental State Examination (MMSE) scores were used as a criterion for participation or suggested [5,6,28]. One study indicated an MMSE-KC score was between 15 and 23 [6]. The other study used an MMSE score ≤26 [5]. Regarding suicides among people with dementia, the Korean Mini-Mental State Examination (K-MMSE) mean SD score was 21.29 [28].
In South Korea, the long-term care grade can identify the level of support required for people with dementia such as performing activities of daily living (ADL) and instrumental activities of daily living (IADL). In two studies [6,29], the long-term care service use or eligibility were presented.
3.4.3. Risk Factors Influencing suicides and SI in People with Dementia
Although both studies [5,6] dealt with the relationship between mental health and suicide risk, different results were reported. A positive association between depression and SI was determined in the study by Kim and Hyun [6]. However, the other study found that suicide was associated with dementia rather than mental health problems [5]. The associated risk factors of SI for people with dementia were depression, previous SA, at-home care, and partial ADL dependency [6]. In the other study, time since dementia diagnosis was associated with suicide risk [5]. Meanwhile, in both studies, suicide risk was found for those who received care at home than for those who received care in an institution [6,29]. Moreover, conditions that did not result in full ADL dependence were identified with suicide risk in two studies [6,29].
3.4.4. Prevalence of Suicides and SI in People with Dementia
One study reported a mean SI score of 5.7 (range: 0–20) and an SA history of 9.9% [6]. Another study revealed that the highest number of suicides (46 suicides) occurred within one year of dementia diagnosis and decreased to 29 during the second year [5]. Furthermore, suicide risk increased more in non-users of long-term care services compared to users [29]. Of the included studies, only one found no increased death risk related to suicide in people with mild cognitive impairment or people with dementia [28].
3.5. Dementia Family Caregivers
3.5.1. Characteristics of Dementia Family Caregivers (Gender, Age, and Dementia Family Caregivers Composition)
In one study, with regard to the types of suicide, completed suicides, completed suicides after homicide, and companion suicides were reported [23]. Across these types, the suicide rate was higher among males, especially for suicide after homicide [23]. In four studies on SI [12,24,26,27], the number of female participants was higher than the number of male participants.
Regarding age, suicide after homicide was reported in 80% of individuals aged 60 years or older, companion suicide in 71.4%, and completed suicides in 55.6% [23]. In one study, three dementia family caregivers were over 60 years old and three were between 42 and 59 years old [12]. There was a difference in the age of dementia family caregivers according to family composition among the included studies. The average age of spouses in one related study was 75.58 [26] and 68.7% of adult children and daughter-in-law were aged 46 to 55 years in another related study [24].
Family member participation composition across the studies was as follows: In a case-based study, four adult children, one daughter-in-law, and one spouse participated [12]. Meanwhile, population-based studies ([24,26,27]) involved 160 spouses [26] and 326 adult children and daughter-in-law [24], and 71.3% of spouses lived with people with dementia [27].
3.5.2. Long-Term Care Grade and Care Duration
Three studies presented the composition of long-term care grades for people with dementia [12,24,26]. Across these three studies, there were more people with dementia with long-term care grades of three and four than with a long-term care grade of five or no grade [12,24,26]. Two studies reported the length of care and the illness period [24,26]. The duration of care was, on average (Mean), 11.48 h a day [26], and the duration of illness was reported in 78.9% as one year to four years [24].
3.5.3. Risk and Protective Factors Influencing Suicide Risk for Dementia Family Caregivers
Suicides were associated with the care burden of dementia family caregivers, the burden of other family members, feeling hopeless regarding recovery, violent behavior and language problems of people with dementia, and absence of alternative caregivers [23]. The risk factors for SI among dementia family caregivers included the absence of alternative caregivers and care burdens (e.g., endless caring and economic, physical, and mental burdens) [12,24,25]. The focus group interview study reported impulsive SI due to their care burdens; dementia family caregivers expressed a sense that the care burden would only end if they died by suicide [12]. Suicide risks related to dementia symptom level and severity were also found [25,26]. In one study on spouses, feelings of entrapment and poor coping strategies were associated with SI [26]. The combination of “high risk-low protective factors” involved the highest levels of SI [27].
Only two studies presented protective factors related to SI among dementia family caregivers. One study detailed that such factors included social activities and resource as protective factors of SI among family living with people with dementia [27]. Another study presented self-efficacy as a protective factor in the relationship between care stress and SI among adult children and daughter-in-law serving as dementia family caregivers [24].
3.5.4. Prevalence of SI, SA, Suicides among Dementia Family Caregivers
Suicidal behavior among dementia family caregivers occurs in diverse forms [23]. In a study consisting only of spouses, although the methodology and sample size were heterogeneous, the reporting rate of SI was higher than that of other studies [26].
4. Discussion
This review aimed to explore suicide risk characteristics among people with dementia and dementia family caregivers in South Korea over the last ten years (2010–2021). Ten studies were included; within this review, there were fewer studies on people with dementia than on dementia family caregivers. Suicide risk was reported for both people with dementia and dementia family caregivers, but the characteristics of suicide risk were different, a finding that is consistent with the results of a previous study [2,4,10,11]. In terms of the related suicide risk among people with dementia, there were 21 published studies spanning 35 years (1980–2015) in a previous systematic review of Alzheimer’s disease, compared to four published studies for people with dementia across 10 years in the current study [30]. Furthermore, the previous review included eight cross-sectional and two longitudinal studies [30], whereas in the current review, only one of the four studies was cross-sectional; the other three were cohort studies. While a prior meta-study found that the effect size of SA was higher than SI among people with dementia [31], the current review found that SA was rarely assessed for people with dementia.
Second, regarding the demographics of dementia family caregiver participants, there generally tended to be more female participants than male participants. However, a study on completed suicides in dementia family caregivers reported a higher prevalence in men than in women. This review revealed gender-related differences between study participants and actual completed suicides among the dementia family caregiver studies. In terms of the social context, since Korean elderly males have in the past been considered breadwinners, they may have lacked care resources for people with dementia as compared to women. Regarding the age of people with dementia, it was difficult to estimate the average owing to the heterogeneity of methods across studies. The dementia family caregiver studies revealed age differences according to family member composition.
Third, prevalence, risk factors, and protective factors for completed suicides, SI, and SA varied due to methodological heterogeneity among the studies. A previous cohort study on SI in people with dementia in eight European countries revealed nationality and depression as suicide risk factors [32]. However, this review showed different results for the associated mental health risks [5]. In addition, the preceding study [32] reported that SI among people with dementia decreased over time and two studies [5,28] in this review were considered in a similar context. The review findings were considered in light of previous studies of suicide risk factors associated with people with dementia such as depression, experience with suicide, and early dementia stage [4,7,32].
Similar to the findings of previous studies [10,11], dementia family caregivers were also exposed to suicide risk. In addition, the factors of suicide risk for dementia family caregivers were similar to those reported in previous studies [10,13,14].
Based on the results of this study, the following recommendations are suggested: Dementia is seen as damage to the nervous tissue in the brain [33] and includes not only memory impairment but also emotional problems [14]. Mental health for people with dementia requires treatment by specialists [14,15]. However, very few hospitals offer specialized mental health care for people with dementia in South Korea [34]. Mental health services for suicide prevention for early-diagnosed people with dementia who are relatively cognitively and physically healthy should be considered. In this review, the scale for SI measurement was identified in four studies [6,24,25,26] and the various measuring SI tools were not used in the included studies. At the various levels, depression, SI, and suicide risk assessments for suicide prevention in dementia patients and caregivers should be considered [35,36,37]. It is also necessary to consider a combined treatment approach, such as robotic and cognitive therapy, to reduce the risk of suicide in people with dementia [38].
Seong et al. [34] reported a lack of employment support for dementia family caregivers. Our review found that the employment status of adult children of people with dementia was related to SI [24]. Support is needed so that dementia family caregivers can balance work and care. However, one study identified bondage from dementia spouse care as a suicide risk. In South Korea, 2.5 times more women had dementia than men in 2019 [39]. More recently, spouses are more likely to become dementia family caregivers than adult children and support for spouses as dementia family caregivers is essential. Based on the results of this review, specific support to alleviate the care burden (e.g., financial support, diversity of care resources, and educational opportunities for coping with the behavioral changes of people with dementia) needs to be introduced.
This study involved several limitations. Regarding suicide risk among people with dementia and dementia family caregivers, the heterogeneity of methodologies prevented us from synthesizing robust new knowledge. Additionally, although the researchers carefully extracted the literature, the possibility of omission cannot be excluded. As the included studies are peer-reviewed studies, biased results may have appeared due to publication bias. Nevertheless, the major contribution of this review is that it addresses the lack of knowledge about suicide risk in people with dementia and dementia family caregivers.
5. Conclusions
People with dementia and dementia family caregivers experienced suicide risk after a dementia diagnosis or as the severity of dementia worsened. The findings of our review expand existing knowledge on dementia-related suicide risk literature by offering insights on dementia-related suicide risk among Koreans.
Notably, we found that there were fewer studies on SI than on suicides among people with dementia. Accordingly, it was difficult to obtain sufficient knowledge about suicide risk in people with dementia. The limitations of conducting research on suicide risk in people with dementia may include the cognitive status of people with dementia or difficulty in recruiting research participants. Consequently, additional research must be conducted to monitor and manage suicide risk among people with dementia. Moreover, few studies in this review measured SA. Additional assessment of SA among people with dementia and dementia family caregivers needs to be conducted. Moreover, it is necessary to expand the data for future research by using data from Korea and other countries.
Author Contributions
Conceptualization, J.W.K. and J.Y.P.; methodology, J.W.K. and J.Y.P.; validation, J.W.K. and J.Y.P.; formal analysis, J.W.K. and J.Y.P.; investigation, J.W.K. and J.Y.P.; resources, J.W.K. and J.Y.P.; data curation, J.W.K. and J.Y.P.; writing—original draft preparation, J.W.K.; writing—review and editing, J.Y.P.; visualization, J.Y.P.; supervision, J.W.K.; project administration, J.W.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data is available upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Mixed Methods Appraisal Tool (MMAT) for quality assessment.
Table A1.
Mixed Methods Appraisal Tool (MMAT) for quality assessment.
| Qualitative Study | Clear Research Questions | Data and Research Questions | Qualitative Approach | Appropriateness of Collecting Qualitative Data | Derived Findings from Data | Sufficient Interpretation from the Data | Qualitative Data, Collection, Analysis, and Interpretation |
| Kim (2014) [23] | + | + | + | + | + | + | + |
| Kim & Um (2015) [12] | + | + | + | + | + | + | + |
| Quantitative Nonrandomized | Clear Research Questions | Data and Research Questions | Sample of Population Representativeness | Measurement for Outcome and Intervention (or Exposure) | Outcome | Confounders | Proceeded According to the Research Plan |
| Kim & Hyun (2013) [6] | + | + | + | + | + | + | + |
| An, Lee, Jeon, Son, Kim, & Hong (2019) [28] | + | + | + | + | + | + | + |
| Moon, Choi, & Sohn (2021) [29] | + | + | + | + | + | + | + |
| Choi, Lee & Han (2021) [5] | + | + | + | + | + | + | + |
| Kim, Kim, Jang & Song (2016) [25] | + | + | + | + | + | + | + |
| Park (2018) [27] | + | + | + | + | + | + | + |
| Jeong (2017) [24] | + | + | + | + | + | + | + |
| Du & Han (2018) [26] | + | + | + | + | + | + | + |
Note: Responding: Yes: appropriate (+); No: not appropriate (−); Can’t tell: unable to identify (*).
References
- Haw, C.; Harwood, D.; Hawton, K. Dementia and suicidal behavior: A review of the literature. Int. Psychogeriatr. 2009, 21, 440–453. [Google Scholar] [CrossRef] [PubMed]
- Koyama, A.; Fujise, N.; Matsushita, M.; Ishikawa, T.; Hashimoto, M.; Ikeda, M. Suicidal ideation and related factors among dementia patients. J. Affect. Disord. 2015, 178, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Alberici, A.; Cottini, E.; Cosseddu, M.; Borroni, B.; Padovani, A. Suicide risk in frontotemporal lobe degeneration: To be considered, to be prevented. Alzheimer Dis. Assoc. Disord. 2012, 26, 194–196. [Google Scholar] [CrossRef] [PubMed]
- Seyfried, L.S.; Kales, H.C.; Ignacio, R.V.; Conwell, Y.; Valenstein, M. Predictors of suicide in patients with dementia. Alzheimers Dement. 2011, 7, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.W.; Lee, K.S.; Han, E. Suicide risk within 1 year of dementia diagnosis in older adults a nationwide retrospective cohort study. J. Psychiatry Neurosci. 2021, 46, E119–E127. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.P.; Hyun, M.-Y. Depression and suicidal ideation in elders with dementia. J. Korean Acad. Nurs. 2013, 43, 296–303. [Google Scholar] [CrossRef]
- Diehl-Schmid, J.; Jox, R.; Gauthier, S.; Belleville, S.; Racine, E.; Schüle, C.; Turecki, S.; Richard-Devantoy, S. Suicide and assisted dying in dementia: What we know and what we need to know. A narrative literature review. Int. Psychogeriatr. 2017, 29, 1247–1259. [Google Scholar] [CrossRef] [PubMed]
- Korea Foundation for Suicide Prevention. 5 Years (2013–2017) National Suicide and Death Analysis Report. 2021. Available online: http://www.kfsp.org (accessed on 10 January 2022).
- Lapierre, S.; Erlangsen, A.; Waern, M.; De Leo, D.; Oyama, H.; Scocco, P.; Gallo, J.; Szanto, K.; Conwell, Y.; Draper, B.; et al. A systematic review of elderly suicide prevention programs. Crisis 2011, 32, 88–98. [Google Scholar] [CrossRef]
- Anderson, J.G.; Eppes, A.; O’Dwyer, S.T. “Like death is near”: Expressions of suicidal and homicidal ideation in blog posts of family caregivers of people with dementia. Behav. Sci. 2019, 9, 22. [Google Scholar] [CrossRef] [PubMed]
- Joling, K.J.; O’Dwyer, S.T.; Hertogh, C.M.; van Hout, H.P. The occurrence and persistence of thoughts of suicide, self-harm and death in family caregivers of people with dementia: A longitudinal data analysis over 2 years. Int. J. Geriatr. Psychiatry 2018, 33, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Um, K.W. A study on care experience of family members of elderly with dementia after policy implementation of dementia special rating—Focusing on difficulty of care and necessary social services. Korean J. Gerontol. Soc. Welf. 2015, 12, 349–371. [Google Scholar]
- Haji Assa, A.; Umberger, R.A. A concept analysis of family caregivers’ uncertainty of patient’s illness. Nurs. Forum 2022, 57, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.G.; Han, C. Diagnosis and treatment of dementia in primary care. J. Korean Med. Ass. 2013, 56, 1104–1112. [Google Scholar] [CrossRef][Green Version]
- Lee, D.W.; Seong, S.J. Korean national dementia plans: From 1st to 3rd. J. Korean Med. Assoc. 2018, 61, 298–303. [Google Scholar] [CrossRef]
- Yoon, H.; Shon, C. A study on the health-economic burden of dementia in Seoul, Korea. Seoul Stud. 2021, 22, 73–89. [Google Scholar]
- National Institute of Dementia. Korean Dementia Observatory 2021; National Institute of Dementia: Seoul, Korea, 2021.
- Hue, M.S.; Kim, J.S.; Youn, H.S. Predictors of depression and life satisfaction among family caregivers for demented elderly. J. Korea Gerontol. Soc. 2004, 24, 111–128. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT), Version 2018; Registration of Copyright (#1148552); Canadian Intellectual Property Office: Gatineau, QC, Canada, 2018.
- The Cochrane Collaboration. 2022. Available online: https://dplp.cochrane.org/data-extraction-forms (accessed on 10 January 2022).
- Kim, W.K. Analysis of newspaper articles on murder or suicide on family caregivers with dementia. Health Soc. Welf. Rev. 2014, 34, 219–246. [Google Scholar]
- Jeong, H.-C. A study on the effect of elderly dementia caregiver’s stress to their suicidal ideation—Mediating effect of self-efficacy. J. Korea Contents Assoc. 2017, 17, 167–182. [Google Scholar]
- Kim, J.Y.; Kim, J.B.; Jang, D.Y.; Song, I.H. A study on the effect of caregiver burden on suicidal ideation among caregiver for the elderly with dementia. J. Korean Gerontol. Soc. 2016, 36, 883–903. [Google Scholar]
- Du, N.-H.; Han, S.-J. Factors affecting the suicidal ideation in spouse caregivers of the elderly with dementia living in the community. J. Korea Converg. Soc. 2018, 9, 241–250. [Google Scholar] [CrossRef]
- Park, M.J. Effect of latent class types of risk and protective factors on the suicidal ideation of family members living with dementia patients in community. J. Korean Gerontol. Soc. 2018, 38, 1107–1125. [Google Scholar] [CrossRef]
- An, J.H.; Lee, K.E.; Jeon, H.J.; Son, S.J.; Kim, S.Y.; Hong, J.P. Risk of suicide and accidental deaths among elderly patients with cognitive impairment. Alzheimers Res. Ther. 2019, 11, 32. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.; Choi, M.; Sohn, M. Suicide among older adults with dementia: Effects of Korea’s long-term care insurance system. Int. J. Environ. Res. Public Health 2021, 18, 6582. [Google Scholar] [CrossRef] [PubMed]
- Serafini, G.; Calcagno, P.; Lester, D.; Girardi, P.; Amore, M.; Pompili, M. Suicide risk in Alzheimer’s disease: A systematic review. Curr. Alzheimer Res. 2016, 13, 1083–1099. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, F.J.Á.; Rubio-Aparicio, M.; Muñoz, P.G.; Herrero, A.M.G.; Sánchez-Meca, J.; Navarro-Mateu, F. Suicide and dementia: Systematic review and meta-analysis. Rev. Psiquiatr. Salud Ment. 2020, 13, 213–227. [Google Scholar] [CrossRef]
- Holmstrand, C.; Rahm Hallberg, I.; Saks, K.; Leino-Kilpi, H.; Renom Guiteras, A.; Verbeek, H.; Zabalegui, A.; Sutcliffe, C.; Lethin, C. Associated factors of suicidal ideation among older persons with dementia living at home in eight European countries. Aging Ment. Health 2021, 25, 1730–1739. [Google Scholar] [CrossRef] [PubMed]
- Oh, B.H. Diagnosis and treatment for behavioral and psychological symptoms of dementia. J. Korean Med. Assoc. 2009, 52, 1048–1054. [Google Scholar] [CrossRef][Green Version]
- Seong, S.J.; Lee, K.J.; Kim, W.J.; Kim, K.; Lee, D.W. A study on complementary policy to enhance the effectiveness of national dementia policy in terms of medical services. J. Korean Neuropsychiatr. Assoc. 2021, 60, 396–405. [Google Scholar] [CrossRef]
- Costantini, L.; Pasquarella, C.; Odone, A.; Colucci, M.E.; Costanza, A.; Serafini, G.; Aguglia, A.; Murri, M.B.; Brakoulias, V.; Amore, M.; et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): A systematic review. J. Affect. Disord. 2021, 279, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A. Manual for the Beck Scale for Suicide Ideation San Antonio; Psychological Corporation: San Antonio, TX, USA, 1991. [Google Scholar]
- Baertschi, M.; Costanza, A.; Canuto, A.; Weber, K. The dimensionality of suicidal ideation and its clinical implications. Int. J. Methods Psychiatr. Res. 2019, 28, e1755. [Google Scholar] [CrossRef] [PubMed]
- Vostrý, M.; Fischer, S.; Cmorej, P.C.; Nesvadba, M.; Peřan, D.; Šín, R. Combined therapy for patients after ischemic stroke as a support of social adaptability. Neuro Endocrinol. Lett. 2020, 40, 329–332. [Google Scholar]
- MOHW. 2020. Available online: http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=032901&CONT_SEQ=361682 (accessed on 10 January 2022).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).