Abstract
Mindfulness is a mental state that can be achieved through meditation. So far, studies have shown that practicing mindfulness on a consistent and regular basis can improve attentional functions and emotional well-being. Mindfulness has recently begun to be used in the field of child development. The goal of this study is to assess if a mindfulness program may help primary school students in reducing anxiety and depression while also improving their temperamental characteristics. This multi-arm pre-post study included 41 subjects recruited in the fifth year of two primary school classes. Participants were randomly assigned to the experimental and control groups. The experimental group, but not the control group, underwent an eight-week mindfulness training. Every week, the program included 60-min group sessions. QUIT (Italian Questionnaires of Temperament) and TAD (Test for Anxiety and Depression in Childhood and Adolescence) were used to assess temperament, and anxiety and depression, respectively. Both groups were administered both instruments before and after mindfulness intervention. The mindfulness program lowered anxiety levels and was effective in changing temperament dimensions: there was an increase in social orientation (SO), positive emotionality (PE), and attention (AT), as well as a decrease in inhibition to novelty (IN) and negative emotionality. Path analysis revealed that AT may promote the improvement of both SO and IN. Similarly, PE may be promoted by the decrease of IN. Clinical implications are discussed.
1. Introduction
Mindfulness-based interventions are mainly complex programs with more components cultivating mindfulness, such as breathing awareness practice, working with thoughts and emotions, awareness practices of senses and daily life, kindness practice, etc., and they represent the central teaching of Buddhist practice [1]. In the last twenty years, mindfulness-based interventions have been increasingly representing key elements related to the dialogue between the eastern and the western world. According to Kabat-Zinn, mindfulness could be described as the process of paying particular attention, on purpose, to the present moment, and in a non-judgmental manner [1]. It is conceptualized by modern psychology as the development of a particular type of attention given to the present moment, characterized by acceptance of experience and suspension of judgment, which allows the practitioner to respond in the most appropriate way to any given situation rather than simply reacting to it. Though meditation is not the only way to practice mindfulness, most authors agree that the development of mindfulness is associated with the practice of meditation [2,3,4,5,6,7,8]. The construct of mindfulness is currently used with four different but interconnected meanings: mindfulness as a traditional meditation practice, as a modern clinical intervention, as a state, and as a trait [2]. One of the essential objectives of any psychology or institution that intervenes towards subjects in developmental age is to favor the development and maintenance of the individual’s health and the prevention of physical and mental discomfort [9]. In recent decades, mindfulness-based interventions have been proved to improve mental health and well-being among adults and youth as well [2,5].
The World Health Organization [10] has provided a definition of the concept of health that includes four domains: a state of physical, mental, social, and spiritual well-being. In this perspective, in the general population it has been shown that mindfulness is related to lower levels of depression and anxiety [11]. The estimated number of hours of mindfulness meditation practice did not affect depression or anxiety directly but did reduce these indirectly by increasing mindfulness. Accordingly, emotional regulation plays a significant mediating role between mindfulness and symptoms of depression and anxiety and suggest that meditation focusing on reducing worry and rumination may be especially useful in reducing the risk of developing clinical depression [11]. Meta-analytic evidence also showed that mindfulness-based therapy is a promising intervention for treating anxiety and mood problems in clinical populations [12]. The practice allows the individual to explore their own body dimension in an autonomous, spontaneous, decentralized way and to understand over time the relationships between the cognitive, emotional and physical-sensorial spheres [13,14,15]. This aspect is even more relevant in developmental age, as children often use the body as a metaphor or vehicle of information for their own internal experience. Their body and mind are in constant evolution, it is important for this to favor the development of educational tools and methods aimed at the continuous and progressive integration and harmonization of these two systems [16,17]. The significant role of mental health problems in developmental age and the associated risks underline the importance and the need to evaluate the effectiveness of school prevention programs that aim to promote protective factors and the ability to cope effectively with stress in all children and adolescents. Many school prevention programs have limitations [18], such as focusing on a single development domain, or they are short-term interventions and cannot be integrated and extended within the school curriculum [19,20,21,22,23,24,25,26,27,28,29,30,31]. Current research highlights the usefulness of mindfulness interventions in various problems of developmental age, however to date we have a small amount of controlled and randomized efficacy studies and it is considered useful to further develop research relating to the effects of particular processes developed by mindfulness meditation [32,33]. Hence, this study aims to investigate whether a mindfulness program with primary school children can be effective in reducing anxiety and depression levels and in changing temperament dimensions [30,31,33,34].
Recent research suggests that maternal mindfulness during pregnancy may have positive effects on temperament and infant development. Specifically, this association may be mediated by reduced anxiety symptoms in pregnant women who score high on mindfulness [35]. However, the specific effects of a structured mindfulness intervention on temperamental dimensions of primary school children are not known and we set out to explore the possible effects of mindfulness on children’s temperament. In particular, we planned that, in parallel, an experimental group underwent a mindfulness intervention and a control group underwent daily school activities. Measures related to temperament, anxiety, and depression were administered before and after the intervention. The following were hypothesized: with respect to before intervention measures, the experimental group, but not the control group, would show improvement related to temperament (in particular, in relation to its attentional dimension), anxiety, and depression.
2. Materials and Methods
2.1. Trial Design
As stated in the ClinicalTrials.gov Identifier NCT05179096 (https://clinicaltrials.gov/ct2/show/NCT05179096; accessed on 2 March 2022; the “Mind the Child study”), our study is an interventional controlled trial with a randomized allocation. The intervention model follows a parallel assignment, and the primary purpose is supportive care. The study was conducted in accordance with the Declaration of Helsinki.
2.2. Participants
Eligibility criteria were as follows: ages eligible for study were from 9 to 11 years old, sexes eligible for study were both females and males accepted as healthy volunteers. Inclusion criteria were as follows: children aged 9 to 11 years; children have reasonable comprehension of spoken language and can follow simple instructions; children and their parents are willing to attend all intervention sessions; children and parents have an adequate understanding of Italian. Exclusion criteria: concurrent enrollment in other intervention trials; child or parent regularly practice complementary health interventions such as meditation. The mindfulness program was carried out in an Italian public primary school in Pisa. Parents of all the subjects enrolled in the study provided their written informed consent.
2.3. Interventions
Following TIDieR (Template for Intervention Description and Replication) criteria [36], the “Mind the Child study” consisted of 2 arms: an experimental group, undergoing a mindfulness intervention program, and a control/no intervention group, following daily routine school activities. The mindfulness program was carried out by an experienced psychotherapist, certificated as a mindfulness instructor. The experimental group underwent the eight-week mindfulness program consisting of group sessions of 60 min per week [37]. The mindfulness program was originally conceived and conducted according to the protocols described in the literature [30,31] and is described in detail in Supplementary Table S1 [38,39]. Briefly, the intervention was related to mindful eating practice, mindfulness exercises as “paying attention to here and now”, breath-based practices, body scan exercises, and walk practice.
2.4. Outcome Measures
2.4.1. Primary Outcome Measures
Italian Questionnaires of Temperament (QUIT; [40]). QUIT is a questionnaire consisting of 54 items that measure temperamental dimensions: inhibition to novelty (IN), attention (AT), motor activity (MA), social orientation (SO), positive and negative emotionality (PE and NE, respectively). Each item ranks on a 6-point scale with responses ranging from “rarely” to “often”. The Cronbach α of each of the QUIT dimensions was found to be >0.75 [40]. During this study, the questionnaire was filled in by the teachers. In the current study, all the subscales showed good internal consistency (α’s between 0.76 and 0.85).
2.4.2. Secondary Outcome Measures
Test for Anxiety and Depression in Childhood and Adolescence (TAD; [41]; Italian version in [42]). In order to measure anxiety and depression, the TAD (Scale A), a self-report questionnaire filled in by the students, was used [42]. The scale assesses the frequency and severity of symptoms. TAD is comprised of 22 items: 11 items are related to depression, while the other 11 items assess anxious symptoms. TAD is a 4-point, Likert-type, scale which indicates the frequency and severity of each item, with responses ranging from “never” to “often”. Cronbach’s α of the TAD-Scale A is 0.84 [42]. In this study, the questionnaire is filled in by the children. In the current study, this scale showed good internal consistency (α = 0.88). Overall, the questionnaires took between 10 and 25 min to be completed. The scales were administered in a counterbalanced fashion to control for order and sequence effects. No external incentives were offered for participating in this study.
2.5. Sample Size
Following recommendations to carry out pilot investigations, a minimum sample size of 12 per group was considered [43] in order to carry out our pilot trial [44,45]. Eighty-nine subjects were assessed for eligibility among public primary school students in Pisa. Among students assessed for eligibility, 43 declined to participate to the intervention, while 5 were not enrolled since children and their parents were not willing to attend all intervention sessions. A total of 41 subjects were enrolled in the study for randomized allocation.
2.6. Randomization
Subjects were randomly assigned in a 1:1 ratio to either the experimental intervention group (mindfulness) or the no-intervention group (daily routine school activities) using a computer-generated basic randomization sequence. Randomization was carried out after the baseline assessment by a statistician who was not otherwise involved in the study and had no interaction with the study participants. The allocation was and will be blinded to the outcome evaluators, and participants were told not to reveal their group assignment to the outcome evaluators. The psychologists that carried out the intervention were not the same as the outcome evaluators.
2.7. Statistical Analysis
All basic statistical analyzes were performed with SPSS® 27 (IBM Corp., Armonk, NY, USA) and SigmaPlot® 14 (Systat software, Chicago, IL, USA). Shapiro–Wilk test was performed to verify the non-normality of the distributions. In order to compare age between control and mindfulness samples we applied a Mann–Whitney Rank Sum Test (MWRST), while to compare gender frequency we applied the Fisher Exact Test, because over 20% of the expected values in the contingency table were less than five. For comparisons between groups, before treatment, a Friedman’s two-way analysis of variance on ranks (F-tw-ANOVA) with Dunnett post-hoc group rank sums comparisons against a control group were used; while, for comparisons within groups, after treatment, a F-tw-ANOVA with Tukey post-hoc rank sums comparisons were used. In order to identify the best models predicting each of the QUIT subscales, the General Linear Model (GLM) regression analysis was used and all the QUIT variables that showed a significant effect after mindfulness intervention were considered. For each of the QUIT subscales to be predicted as a criterion, the model showing the highest adjusted R2 was considered.
In order to explore and confirm a possible path model, obtain goodness-of-fit indices, and maximum-likelihood estimates of model parameters, AMOS 27.0 was employed. For each predictor, the Variance Inflation Factor (VIF) was calculated, and it always fell within the range (1.05–2.64), indicating that there was no significant multicollinearity [46]. The p values reported were two-tailed, and a p value < 0.05 was considered significant. Before performing path analysis, we analyzed the relationships between the variables. The absolute fit indices utilized in this study were χ2 and the root mean square error of approximation (RMSEA); the incremental fit indices used in this investigation were the comparative fit index (CFI) and the Tucker–Lewis index (TLI). CFI and TLI values of 0.90 or higher, and RMSEA values of 0.06 or lower, were considered a “good fit.” A better fit is indicated by χ2 values that are closer to zero. Since χ2 is sensitive to the sample size employed in the model fit analysis, it was not suggested as a model fit judgement [47]. Hence, it was just reported in this study but not used as a fit statistic. We employed the following model fit criteria [48]: TLI and CFI: ≥0.90 indicated acceptable fit, ≥0.95 indicated excellent fit; RMSEA: ≤0.08 indicated acceptable fit, ≤0.06 indicated excellent fit, and its 90% confidence interval (CI) was reported.
3. Results
3.1. Group Comparisons
As reported in the CONSORT flow diagram [49] of the study in Figure 1, 41 subjects (34.15% females; mean age = 10.78, SD = 0.38) belonging to two fifth-year primary school classes were included in the study. The control group was composed by 18 subjects (4 females, 22.22%) and the mindfulness group was composed by 23 subjects (10 females, 43.48%). As a first step, we compared gender frequency and age between control and mindfulness samples to evaluate gender and age homogeneity among groups. Fisher Exact Test revealed that gender frequency was not significantly different (p = 1), between the two groups, while MWRST showed that age was not significantly different (p = 0.874), as well. Thus, control and mindfulness groups were homogeneous regarding gender and age. Hence, we compared the scores shown by participants between the two groups, before mindfulness intervention, and within the two groups, after mindfulness intervention, regarding scales and subscales of the study measures. Regarding pre-intervention baseline measures, Dunnett’s post-hoc analysis of F-tw-ANOVA revealed that control and mindfulness samples did not show scores that were significantly different for the TAD (TAD-Anxiety: p = 0.378; TAD-Depression: p = 0.271), and the QUIT (QUIT-SO: p = 0.738; QUIT-IN: p = 0.198; QUIT-MA: p = 0.207; QUIT-PE: p = 0.132; QUIT-NE: p = 0.792; QUIT-AT: p = 0.566). Conversely, comparing post-intervention measures, Dunnett’s post-hoc analysis of F-tw-ANOVA revealed that control and mindfulness samples did not show a significant difference regarding TAD (TAD-Anxiety: p = 0.269; TAD-Depression: p = 0.386) but, with respect to control sample, mindfulness sample showed a significant increase in SO (QUIT-SO: p = 0.002), MA (QUIT-MA: p = 0.005), PE (QUIT-PE: p < 0.001) and AT (QUIT-AT: p < 0.001) subscales, as well as a decrease in IN (QUIT-IN: p < 0.001) and in NE (QUIT-NE: p = 0.004) subscales (Table 1).
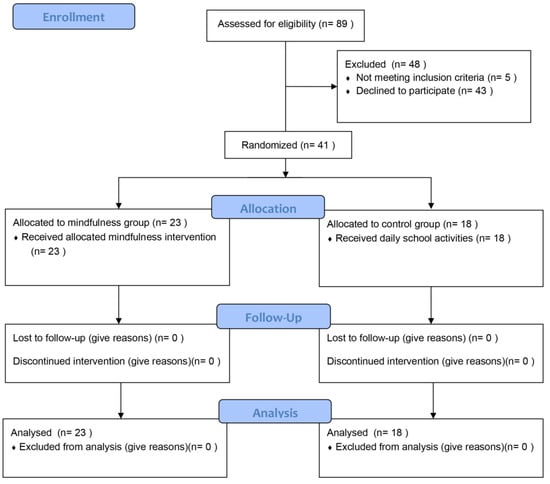
Figure 1.
CONSORT flow diagram of the study.

Table 1.
Group comparisons among the study measures between Mindfulness (n = 23) and Control (n = 18) samples assessed pre-intervention and post-intervention.
In order to identify the effects of mindfulness intervention on each group, we compared separately control and mindfulness groups before and after mindfulness intervention. As expected, Tukey’s post-hoc test of F-tw-ANOVA revealed that the control sample, after the mindfulness intervention, did not show scores that were significantly different for the TAD (TAD-Anxiety: p = 0.602; TAD-Depression: p = 0.775), and the QUIT (QUIT-SO: p = 0.908; QUIT-IN: p = 0.694; QUIT-MA: p = 0.991; QUIT-PE: p = 0.954; QUIT-NE: p = 0.881; QUIT-AT: p = 0.871). Conversely, Tukey’s post-hoc test of F-tw-ANOVA revealed that the mindfulness sample, after the mindfulness intervention, showed a significant improvement regarding anxiety (TAD-Anxiety: p = 0.006), but not in depression symptoms (TAD-Depression: p = 0.756). Regarding QUIT dimensions, the mindfulness sample, after the mindfulness intervention, showed a significant increase in SO (QUIT-SO: p < 0.001), PE (QUIT-PE: p < 0.001) and AT (QUIT-AT: p < 0.001) subscales, as well as an improvement in IN (QUIT-IN: p < 0.001) and in NE (QUIT-NE: p < 0.001) subscales (Table 2).

Table 2.
Group comparisons among the study measures within Mindfulness (n = 23) and Control (n = 18) samples assessed pre-intervention and post-intervention.
3.2. GLM Regressions
In order to identify the best models predicting each of the QUIT subscales, we carried out the best GLM regression analysis and all the QUIT variables that showed a significant effect after mindfulness intervention were considered (with the exception of MA). The VIF was computed for each predictor and for all significant predictors always fell within the range (1.16–2.54) which is considered as evidence of a lack of substantial multicollinearity [50]. Results of the best subset regression analysis predicting each of the significant QUIT subscales for mindfulness group are reported in Table 3.

Table 3.
GLM regression analyses predicting QUIT-SO, QUIT-IN, QUIT-PE, QUIT-NE and QUIT-AT subscales score from the other QUIT subscales for Mindfulness sample post-intervention (n = 23).
First, we evaluated which of the QUIT variables were able to predict QUIT-SO. QUIT-AT subscale was a unique significant predictor (β = 0.571, p = 0.015) of QUIT-SO subscale. When inspecting which of the QUIT variables were able to predict QUIT-IN, QUIT-PE, and QUIT-AT were found to be significant predictors (β = −0.536, p = 0.022 for QUIT-PE; β = 0.394, p = 0.04 for QUIT-AT). QUIT-PE was found to be uniquely predicted by QUIT-IN (β = −0.482, p = 0.022), while QUIT-AT was found to be predicted by both QUIT-SO and QUIT-IN (β = 0.506, p = 0.015 for QUIT-SO; β = −0.543, p = 0.04 for QUIT-IN). QUIT-NE was not found to be predicted by any of the QUIT subscales.
3.3. Path Analysis
Path analytic models were tested using AMOS 27 for mindfulness group post-intervention to evaluate if there was a possible particular association among QUIT subscales. Skewness ranged from −1.21 to 0.87, and kurtosis ranged from −1.1 to 0.91. When using path analysis or structural equation modeling (SEM), acceptable skewness values range from −3 to +3, and acceptable kurtosis values range from −10 to +10 [45,46]. Values that are below or above these ranges are questionable, although path analysis and SEM are highly robust analytical methods, thus minor deviations may not indicate severe assumptions violations [51]. We used the Maximum Likelihood (ML) estimator.
In the mindfulness group post-intervention, among QUIT subscales, we found that AT was able to significantly predict both SO (β = 0.518, p < 0.001, SE = 0.134) and IN (β = −0.664, p < 0.001, SE = 0.197). Furthermore, PE was found to be significantly predicted by IN (β = −0.629, p < 0.001, SE = 0.163). Overall, AT was found to be the unique QUIT subscale to be able to predict both SO and IN (Figure 2). In turn, IN was found to be the only QUIT subscale that was able to predict PE (χ2 (2) = 0.186, p = 0.911; CFI = 0.996, TLI = 0.98, RMSEA = 0.024 [0.021; 0.027]).
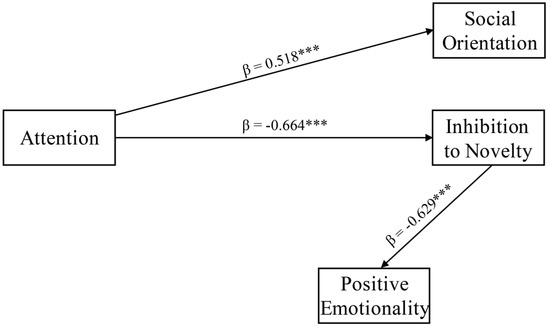
Figure 2.
Path analytic model related to QUIT subscales for Mindfulness sample post-intervention (n = 23). *** indicates p < 0.001.
4. Discussion
Our study aimed at evaluating the effects of a mindfulness intervention on temperament, anxiety, and depression of primary school children (aged 9–11), with respect to children undergoing daily school activities. Our results demonstrate that the mindfulness program was able to significantly reduce anxiety levels [34], but not depressive symptomatology [52]. In addition, mindfulness intervention was able to improve the temperamental dimensions of AT, SO, PE, IN, and NE.
A recent study found that mindfulness interventions in adolescents not only was able to reduce anxiety, but also changed the amygdala’s network features, enhancing structural connectivity [53,54]. In addition, it has been shown that mindfulness-based interventions are effective programs for treating anxiety and mood problems in adult clinical populations [12], as well as for reducing the risk of developing clinical depression through the reduction in worry and rumination [11]. However, we found that the mindfulness program was able to significantly reduce anxiety, but not depression, levels in primary school children ranging from 9 to 11 years old. Interestingly, in a recent meta-analysis it has been also highlighted that mindfulness-based interventions can be effective in children and adolescents with mental health symptoms. Remarkably, in non-clinical populations compared to non-active control, mindfulness-based interventions were also effective improving anxiety and stress but not depression, as in our study [55,56]. Since it has been demonstrated that high levels of shame and maladaptive guilt were related to the onset of preschool depression, as early as age 3 [57], and that shame and guilt exert negative impacts on cognition and attention [58], our non-clinical samples, unlike clinical samples, may not show significant levels of shame or guilt related to an actual clinical manifestation of depression and thus may already show healthy mood levels at baseline that may not necessitate an improvement.
The program was found to be effective in changing the temperamental dimensions, there was an increase in the levels of SO, PE, and AT and a reduction in the levels of IN and NE [52,59], with robust effect magnitudes even in a non-clinical sample [12]. The dimension of MA does not show variations in response to the intervention, possibly because the QUIT evaluates its temporal aspect. QUIT evaluates MA as the speed through which the responses are issued and does not consider the energetic and resistance components, that may be detected by using another tool [56]. The mindfulness program was particularly effective at promoting the development of the dimensions of cognitive performance, such as attention [60], and of prosociality, such as positive emotions and SO [52]. Since these are necessary dimensions for monitoring interpersonal conflict [61], it can be hypothesized that, in children, the practice of mindfulness is able to promote, and possibly improve, the attentional and prosocial resources: they have the opportunity to learn to master an accessible technique that they can use to manage their emotion and to calm down. Research has shown that aggressive/rejected children had difficulties in shifting their attention from a negative to a prosocial affect [62]. After experiencing social failure, aggressive/rejected children were found to be less able to properly manage their behavior, confirming that attention has an important role in prosociality and positive emotionality [62]. In addition, while prior research has shown that prosocial attitudes contribute to attentional broadening, other findings demonstrate that attentional broadening leads to increased prosociality as well, implying a reciprocal relationship between attention and prosocial behavior [63]. It could be also hypothesized that reorienting attention could be a very important effect of our mindfulness intervention. In fact, it has been demonstrated that temporo-parietal-junction (TPJ), that plays a role in reorienting attention, has also been implicated in the inference of other’s effort during movement and the cost of helping. Thus, TPJ, together with its role in reorienting attention, may contribute to higher-level social cognition [64].
Considering the effects of mindfulness on attention [65], it can be hypothesized that, after a mindfulness intervention, the temperamental dimension identified by the QUIT can be influenced as proposed in Figure 2. AT dimension, the main target of the mindfulness intervention, may promote the improvement of both SO and IN dimensions. It may also be hypothesized that, as a positive feedback mechanism, SO and IN dimensions may favor the improvement of the AT dimension. Similarly, PE may be promoted by the decrease of the IN dimension that, in turn, may favor the decrease of the IN dimension, as an additional positive feedback mechanism. Accordingly, it has been shown that adolescents who were behaviorally inhibited as toddlers and young children showed heightened attention bias to threat. More importantly, attention bias to threat moderated the relation between childhood behavioral inhibition and adolescent social withdrawal [66]. Furthermore, over time behavioral inhibition in toddlerhood predicted high levels of social withdrawal in early childhood and this relation was moderated by attention bias [67]. Thus, it can be hypothesized that in our non-clinical sample the mindfulness program, exerting its main effects on attention, directly promoted prosociality and proneness to novelty that, in turn, promoted positive emotions.
There is substantial evidence that the COVID-19 pandemic has had a significant psychological impact as a result of the imposed limitations [68,69,70]. Previous research has extensively shown that mindfulness meditation can be used as a protective factor in several populations, like children [70]. Mindfulness can be able to buffer the negative effects of social media exposure on psychological distress [71]. During the pandemic, teachers practicing mindfulness meditation had a positive impact. The effects of mindfulness on affective empathy, emotional tiredness, anxiety, and depression among Italian female teachers demonstrated that contemplative practices improved psychological well-being and interoceptive awareness [72]. Because there is so much information in the literature regarding the excellent impacts of mindfulness on our health and well-being, it is reasonable to assume that this emotional well-being is linked to improved learning. However, learning and practicing mindfulness is a lengthy process that requires both time and space, so future research should concentrate on concerns of sustainability and group variations. It may take some time to learn mindfulness, depending on how engaged and motivated each individual is.
Finally, the following limitations should, however, be considered. (a) Our samples were relatively small, further studies should replicate our findings in larger samples. (b) Participants were self-selected; this might limit the generalizability of our conclusions. (c) We included a single temperament measure in our study, the QUIT. Future research could replicate our results using other temperamental measures. (d) All of the TAD and QUIT data were measured through a single source (self-rating and teacher rating, respectively). The conclusions would be strengthened by the inclusion of both self- and teacher-ratings for both TAD and QUIT measures. (e) Self-report data tends to inflate associations among variables.
5. Conclusions
Despite these limitations, our study demonstrated that a mindfulness program in a group of primary school children (9–11 years old), with respect to a matched non-active control group, was able to improve anxiety-related symptoms and the temperamental dimensions of SO, PE, AT, IN, and NE.
Our results promote the implementation of mindfulness interventions for primary school children in order to promote anxiety symptoms prevention. More importantly, mindfulness interventions may represent an effective training for reducing loneliness and increasing social contact in daily life [73] and even for improving cognitive function by increasing the neuronal expression of miRNA-29c [74]. Furthermore, a positive relationship was also found between childhood trauma and absorption and depersonalization, as well as a significant negative association between mindfulness and absorption and depersonalization [75], so mindfulness programs may represent effective interventions to promote integration in clinical [76] and non-clinical individuals [77].
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/bs12030074/s1, Table S1: Overview of the 8-week Mindfulness-Based Stress Reduction intervention.
Author Contributions
Conceptualization, A.P.; methodology, A.P. and M.M.; validation, A.P. and M.M.; formal analysis, A.P.; investigation, A.P. and M.M.; resources, A.P. and M.M.; data curation, A.P. and M.M.; writing—original draft preparation, A.P.; writing—review and editing, A.P., A.G.I.M. and M.M.; supervision, A.G. and M.M.; project administration, A.P. and M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki.
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy issue.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion: New York, NY, USA, 1994; ISBN 978-0-7868-8070-6. [Google Scholar]
- Chiesa, A.; Malinowski, P. Mindfulness-Based Approaches: Are They All the Same? J. Clin. Psychol. 2011, 67, 404–424. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Bantam Dell: New York, NY, USA, 2013. [Google Scholar]
- Lutz, A.; Dunne, J.D.; Davidson, R.J. Meditation and the Neuroscience of Consciousness: An Introduction. In The Cambridge Handbook of Consciousness; Zelazo, P.D., Moscovitch, M., Thompson, E., Eds.; Cambridge University Press: Cambridge, UK, 2007; pp. 499–552. ISBN 978-0-511-81678-9. [Google Scholar]
- Segal, Z.V.; Williams, J.M.G.; Teasdale, J.D.; Kabat-Zinn, J. Mindfulness-Based Cognitive Therapy for Depression, 2nd ed.; paperback edition.; The Guilford Press: New York, NY, USA; London, UK, 2018; ISBN 978-1-4625-3703-7. [Google Scholar]
- Tang, Y.-Y.; Hölzel, B.K.; Posner, M.I. The Neuroscience of Mindfulness Meditation. Nat. Rev. Neurosci. 2015, 16, 213–225. [Google Scholar] [CrossRef] [PubMed]
- Conversano, C.; Ciacchini, R.; Orrù, G.; Di Giuseppe, M.; Gemignani, A.; Poli, A. Mindfulness, Compassion, and Self-Compassion Among Health Care Professionals: What’s New? A Systematic Review. Front. Psychol. 2020, 11, 1683. [Google Scholar] [CrossRef] [PubMed]
- Poli, A.; Gemignani, A.; Soldani, F.; Miccoli, M. A Systematic Review of a Polyvagal Perspective on Embodied Contemplative Practices as Promoters of Cardiorespiratory Coupling and Traumatic Stress Recovery for PTSD and OCD: Research Methodologies and State of the Art. Int. J. Environ. Res. Public Health 2021, 18, 11778. [Google Scholar] [CrossRef]
- Keng, S.-L.; Smoski, M.J.; Robins, C.J. Effects of Mindfulness on Psychological Health: A Review of Empirical Studies. Clin. Psychol. Rev. 2011, 31, 1041–1056. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. The World Health Report 1998—Life in the 21st Century: A Vision for All; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- Parmentier, F.B.R.; García-Toro, M.; García-Campayo, J.; Yañez, A.M.; Andrés, P.; Gili, M. Mindfulness and Symptoms of Depression and Anxiety in the General Population: The Mediating Roles of Worry, Rumination, Reappraisal and Suppression. Front. Psychol. 2019, 10, 506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofmann, S.G.; Sawyer, A.T.; Witt, A.A.; Oh, D. The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review. J. Consult. Clin. Psychol. 2010, 78, 169–183. [Google Scholar] [CrossRef]
- Siegel, D.J. Mindfulness Training and Neural Integration: Differentiation of Distinct Streams of Awareness and the Cultivation of Well-Being. Soc. Cogn. Affect Neurosci. 2007, 2, 259–263. [Google Scholar] [CrossRef]
- Kerr, C.E.; Sacchet, M.D.; Lazar, S.W.; Moore, C.I.; Jones, S.R. Mindfulness Starts with the Body: Somatosensory Attention and Top-down Modulation of Cortical Alpha Rhythms in Mindfulness Meditation. Front. Hum. Neurosci. 2013, 7, 12. [Google Scholar] [CrossRef] [Green Version]
- Bruno, R.M.; Stea, F.; Sicari, R.; Ghiadoni, L.; Taddei, S.; Ungar, A.; Bonuccelli, U.; Tognoni, G.; Cintoli, S.; Del Turco, S.; et al. Vascular Function Is Improved After an Environmental Enrichment Program: The Train the Brain–Mind the Vessel Study. Hypertension 2018, 71, 1218–1225. [Google Scholar] [CrossRef]
- Janz, P.; Dawe, S.; Wyllie, M. Mindfulness-Based Program Embedded Within the Existing Curriculum Improves Executive Functioning and Behavior in Young Children: A Waitlist Controlled Trial. Front. Psychol. 2019, 10, 2052. [Google Scholar] [CrossRef] [PubMed]
- Poli, A.; Maremmani, A.G.I.; Chiorri, C.; Mazzoni, G.-P.; Orrù, G.; Kolacz, J.; Porges, S.W.; Conversano, C.; Gemignani, A.; Miccoli, M. Item Reduction, Psychometric and Biometric Properties of the Italian Version of the Body Perception Questionnaire—Short Form (BPQ-SF): The BPQ-22. Int. J. Environ. Res. Public Health 2021, 18, 3835. [Google Scholar] [CrossRef] [PubMed]
- Bond, L.A.; Hauf, A.M.H. Taking Stock and Putting Stock in Primary Prevention: Characteristics of Effective Programs. J. Prim. Prev. 2004, 24, 199–221. [Google Scholar] [CrossRef]
- Orri, M.; Côté, S.M.; Tremblay, R.E.; Doyle, O. Impact of an Early Childhood Intervention on the Home Environment, and Subsequent Effects on Child Cognitive and Emotional Development: A Secondary Analysis. PLoS ONE 2019, 14, e0219133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balasundaram, P.; Avulakunta, I.D. Human Growth and Development. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Melli, G.; Moulding, R.; Poli, A. Is It More Disgusting If I Think about It? Examining the Interaction of Obsessive Beliefs and Disgust Propensity in Clinical Obsessive-Compulsive Disorder. J. Obs. Compuls. Relat. Disord. 2016, 11, 74–81. [Google Scholar] [CrossRef]
- Melli, G.; Poli, A.; Chiorri, C.; Olatunji, B.O. Is Heightened Disgust Propensity Truly a Risk Factor for Contamination-Related Obsessive-Compulsive Disorder? Behav. Ther. 2019, 50, 621–629. [Google Scholar] [CrossRef] [Green Version]
- Melli, G.; Bulli, F.; Carraresi, C.; Tarantino, F.; Gelli, S.; Poli, A. The Differential Relationship between Mental Contamination and the Core Dimensions of Contact Contamination Fear. J. Anxiety Disord. 2017, 45, 9–16. [Google Scholar] [CrossRef]
- Poli, A.; Melli, G.; Radomsky, A.S. Different Disgust Domains Specifically Relate to Mental and Contact Contamination Fear in Obsessive-Compulsive Disorder: Evidence From a Path Analytic Model in an Italian Clinical Sample. Behav. Ther. 2019, 50, 380–394. [Google Scholar] [CrossRef]
- Conversano, C.; Poli, A.; Ciacchini, R.; Hitchcott, P.; Bazzichi, L.; Gemignani, A. A Psychoeducational Intervention Is a Treatment for Fibromyalgia Syndrome. Clin. Exp. Rheumatol. 2019, 37 (Suppl. S116), 98–104. [Google Scholar]
- Poli, A.; Melli, G.; Ghisi, M.; Bottesi, G.; Sica, C. Anxiety Sensitivity and Obsessive-Compulsive Symptom Dimensions: Further Evidence of Specific Relationships in a Clinical Sample. Pers. Individ. Differ. 2017, 109, 130–136. [Google Scholar] [CrossRef]
- Melli, G.; Carraresi, C.; Poli, A.; Bailey, R. The Role of Metacognitive Beliefs in Health Anxiety. Pers. Individ. Differ. 2016, 89, 80–85. [Google Scholar] [CrossRef]
- Melli, G.; Bailey, R.; Carraresi, C.; Poli, A. Metacognitive Beliefs as a Predictor of Health Anxiety in a Self-Reporting Italian Clinical Sample. Clin. Psychol. Psychother. 2018, 25, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Melli, G.; Carraresi, C.; Poli, A.; Marazziti, D.; Pinto, A. The Role of Guilt Sensitivity in OCD Symptom Dimensions. Clin. Psychol. Psychother. 2017, 24, 1079–1089. [Google Scholar] [CrossRef] [PubMed]
- Flook, L.; Goldberg, S.B.; Pinger, L.; Bonus, K.; Davidson, R.J. Mindfulness for Teachers: A Pilot Study to Assess Effects on Stress, Burnout, and Teaching Efficacy: Mindfulness for Teachers. Mind Brain Educ. 2013, 7, 182–195. [Google Scholar] [CrossRef] [Green Version]
- Kuyken, W.; Weare, K.; Ukoumunne, O.C.; Vicary, R.; Motton, N.; Burnett, R.; Cullen, C.; Hennelly, S.; Huppert, F. Effectiveness of the Mindfulness in Schools Programme: Non-Randomised Controlled Feasibility Study. Br. J Psychiatry 2013, 203, 126–131. [Google Scholar] [CrossRef] [Green Version]
- Bostic, J.Q.; Nevarez, M.D.; Potter, M.P.; Prince, J.B.; Benningfield, M.M.; Aguirre, B.A. Being Present at School. Child Adolesc. Psychiatr. Clin. N. Am. 2015, 24, 245–259. [Google Scholar] [CrossRef]
- Schonert-Reichl, K.A.; Oberle, E.; Lawlor, M.S.; Abbott, D.; Thomson, K.; Oberlander, T.F.; Diamond, A. Enhancing Cognitive and Social–Emotional Development through a Simple-to-Administer Mindfulness-Based School Program for Elementary School Children: A Randomized Controlled Trial. Dev. Psychol. 2015, 51, 52–66. [Google Scholar] [CrossRef] [Green Version]
- Semple, R.J.; Lee, J.; Rosa, D.; Miller, L.F. A Randomized Trial of Mindfulness-Based Cognitive Therapy for Children: Promoting Mindful Attention to Enhance Social-Emotional Resiliency in Children. J Child Fam. Stud. 2010, 19, 218–229. [Google Scholar] [CrossRef]
- van den Heuvel, M.I.; Johannes, M.A.; Henrichs, J.; Van den Bergh, B.R.H. Maternal Mindfulness during Pregnancy and Infant Socio-Emotional Development and Temperament: The Mediating Role of Maternal Anxiety. Early Hum. Dev. 2015, 91, 103–108. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [Green Version]
- Saltzman, A. Mindfulness: A Guide For Teachers. 2012. Available online: https://www.contemplativemind.org/Mindfulness-A_Teachers_Guide.pdf (accessed on 2 March 2022).
- Emerson, L.-M.; Leyland, A.; Hudson, K.; Rowse, G.; Hanley, P.; Hugh-Jones, S. Teaching Mindfulness to Teachers: A Systematic Review and Narrative Synthesis. Mindfulness 2017, 8, 1136–1149. [Google Scholar] [CrossRef] [Green Version]
- Miller, C.J.; Brooker, B. Mindfulness Programming for Parents and Teachers of Children with ADHD. Complementary Ther. Clin. Pract. 2017, 28, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Axia, G. QUIT: Questionari Italiani del Temperamento; Erickson: Trento, Italy, 2002; ISBN 978-88-7946-430-7. [Google Scholar]
- Newcomer, P.L.; Barenbaum, E.M.; Bryant, B.R. Depression and Anxiety in Youth Scale; PRO-ED: Austin, TX, USA, 1994. [Google Scholar]
- Newcomer, P.L.; Barenbaum, E.M.; Bryant, B.R. Test TAD: Test Dell’ansia e Depressione Nell’infanzia e Adolescenza; Erickson: Trento, Italy, 1997; ISBN 978-88-7946-164-1. [Google Scholar]
- Julious, S.A. Sample Size of 12 per Group Rule of Thumb for a Pilot Study. Pharmaceut. Statist. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Bell, M.L.; Whitehead, A.L.; Julious, S.A. Guidance for Using Pilot Studies to Inform the Design of Intervention Trials with Continuous Outcomes. CLEP 2018, 10, 153–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feeley, N.; Cossette, S.; Côté, J.; Héon, M.; Stremler, R.; Martorella, G.; Purden, M. The Importance of Piloting an RCT Intervention. Can. J. Nurs Res. 2009, 41, 85–99. [Google Scholar] [PubMed]
- Menard, S. Applied Logistic Regression Analysis; SAGE Publications, Inc.: Newbury Park, CA, USA, 2002; ISBN 978-0-7619-2208-7. [Google Scholar]
- Park, E.-Y. Path Analysis of Strength, Spasticity, Gross Motor Function, and Health-Related Quality of Life in Children with Spastic Cerebral Palsy. Health Qual. Life Outcomes 2018, 16, 70. [Google Scholar] [CrossRef] [Green Version]
- Marsh, H.W.; Hau, K.-T.; Wen, Z. In Search of Golden Rules: Comment on Hypothesis-Testing Approaches to Setting Cutoff Values for Fit Indexes and Dangers in Overgeneralizing Hu and Bentler’s (1999) Findings. Struct. Equ. Model. A Multidiscip. J. 2004, 11, 320–341. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLoS Med. 2010, 7, e1000251. [Google Scholar] [CrossRef]
- Brown, T.A. Methodology in the social sciences. In Confirmatory Factor Analysis for Applied Research, 2nd ed.; The Guilford Press: New York, NY, USA; London, UK, 2015; ISBN 978-1-4625-1536-3. [Google Scholar]
- Griffin, M.M.; Steinbrecher, T.D. Large-Scale Datasets in Special Education Research. In International Review of Research in Developmental Disabilities; Elsevier: Amsterdam, The Netherlands, 2013; Volume 45, pp. 155–183. ISBN 978-0-12-407760-7. [Google Scholar]
- Zenner, C.; Herrnleben-Kurz, S.; Walach, H. Mindfulness-Based Interventions in Schools—a Systematic Review and Meta-Analysis. Front. Psychol. 2014, 5, 603. [Google Scholar] [CrossRef] [Green Version]
- Tymofiyeva, O.; Henje, E.; Yuan, J.P.; Huang, C.-Y.; Connolly, C.G.; Ho, T.C.; Bhandari, S.; Parks, K.C.; Sipes, B.S.; Yang, T.T.; et al. Reduced Anxiety and Changes in Amygdala Network Properties in Adolescents with Training for Awareness, Resilience, and Action (TARA). Neuro. Clin. 2021, 29, 102521. [Google Scholar] [CrossRef]
- Braschi, C.; Capsoni, S.; Narducci, R.; Poli, A.; Sansevero, G.; Brandi, R.; Maffei, L.; Cattaneo, A.; Berardi, N. Intranasal Delivery of BDNF Rescues Memory Deficits in AD11 Mice and Reduces Brain Microgliosis. Aging Clin. Exp. Res. 2021, 33, 1223–1238. [Google Scholar] [CrossRef] [PubMed]
- Kallapiran, K.; Koo, S.; Kirubakaran, R.; Hancock, K. Review: Effectiveness of Mindfulness in Improving Mental Health Symptoms of Children and Adolescents: A Meta-Analysis. Child. Adolesc. Ment. Health 2015, 20, 182–194. [Google Scholar] [CrossRef] [PubMed]
- Crescentini, C.; Capurso, V.; Furlan, S.; Fabbro, F. Mindfulness-Oriented Meditation for Primary School Children: Effects on Attention and Psychological Well-Being. Front. Psychol. 2016, 7, 805. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luby, J.; Belden, A.; Sullivan, J.; Hayen, R.; McCadney, A.; Spitznagel, E. Shame and Guilt in Preschool Depression: Evidence for Elevations in Self-Conscious Emotions in Depression as Early as Age 3. J. Child. Psychol. Psychiatry 2009, 50, 1156–1166. [Google Scholar] [CrossRef] [Green Version]
- Wang, W.; Song, S.; Wang, J.; Liu, Q.; Huang, L.; Chen, X. Shame on You! When and Why Failure-Induced Shame Impedes Employees’ Learning From Failure in the Chinese Context. Front. Psychol. 2021, 12, 725277. [Google Scholar] [CrossRef]
- Goldsmith, H.H.; Buss, A.H.; Plomin, R.; Rothbart, M.K.; Thomas, A.; Chess, S.; Hinde, R.A.; McCall, R.B. Roundtable: What Is Temperament? Four Approaches. Child. Dev. 1987, 58, 505–529. [Google Scholar] [CrossRef]
- Felver, J.C.; Tipsord, J.M.; Morris, M.J.; Racer, K.H.; Dishion, T.J. The Effects of Mindfulness-Based Intervention on Children’s Attention Regulation. J. Atten. Disord. 2017, 21, 872–881. [Google Scholar] [CrossRef] [Green Version]
- Dignath, D.; Eder, A.B.; Steinhauser, M.; Kiesel, A. Conflict Monitoring and the Affective-Signaling Hypothesis—An Integrative Review. Psychon. Bull. Rev. 2020, 27, 193–216. [Google Scholar] [CrossRef]
- Wilson, B.J. The Role of Attentional Processes in Children’s Prosocial Behavior with Peers: Attention Shifting and Emotion. Dev. Psychopathol. 2003, 15, 313–329. [Google Scholar] [CrossRef]
- Mukherjee, S.; Srinivasan, N.; Kumar, N.; Manjaly, J.A. Perceptual Broadening Leads to More Prosociality. Front. Psychol. 2018, 9, 1821. [Google Scholar] [CrossRef]
- Olivo, D.; Di Ciano, A.; Mauro, J.; Giudetti, L.; Pampallona, A.; Kubera, K.M.; Hirjak, D.; Wolf, R.C.; Sambataro, F. Neural Responses of Benefiting From the Prosocial Exchange: The Effect of Helping Behavior. Front. Psychol. 2021, 12, 606858. [Google Scholar] [CrossRef] [PubMed]
- Yakobi, O.; Smilek, D.; Danckert, J. The Effects of Mindfulness Meditation on Attention, Executive Control and Working Memory in Healthy Adults: A Meta-Analysis of Randomized Controlled Trials. Cogn. Res. 2021, 45, 543–560. [Google Scholar] [CrossRef]
- Pérez-Edgar, K.; Bar-Haim, Y.; McDermott, J.M.; Chronis-Tuscano, A.; Pine, D.S.; Fox, N.A. Attention Biases to Threat and Behavioral Inhibition in Early Childhood Shape Adolescent Social Withdrawal. Emotion 2010, 10, 349–357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Edgar, K.; Reeb-Sutherland, B.C.; McDermott, J.M.; White, L.K.; Henderson, H.A.; Degnan, K.A.; Hane, A.A.; Pine, D.S.; Fox, N.A. Attention Biases to Threat Link Behavioral Inhibition to Social Withdrawal over Time in Very Young Children. J. Abnorm. Child. Psychol. 2011, 39, 885–895. [Google Scholar] [CrossRef] [Green Version]
- Poli, A.; Gemignani, A.; Conversano, C. The Psychological Impact of SARS-CoV-2 Quarantine: Observations through the Lens of the Polyvagal Theory. Clin. Neuropsychiatry 2020, 17, 112–114. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Saurabh, K.; Ranjan, S. Compliance and Psychological Impact of Quarantine in Children and Adolescents Due to COVID-19 Pandemic. Indian J. Pediatr. 2020, 87, 532–536. [Google Scholar] [CrossRef]
- Tortella, G.R.; Seabra, A.B.; Padrão, J.; Díaz-San Juan, R. Mindfulness and Other Simple Neuroscience-Based Proposals to Promote the Learning Performance and Mental Health of Students during the COVID-19 Pandemic. Brain Sci. 2021, 11, 552. [Google Scholar] [CrossRef]
- Matiz, A.; Fabbro, F.; Paschetto, A.; Cantone, D.; Paolone, A.R.; Crescentini, C. Positive Impact of Mindfulness Meditation on Mental Health of Female Teachers during the COVID-19 Outbreak in Italy. Int. J. Environ. Res. Public Health 2020, 17, 6450. [Google Scholar] [CrossRef]
- Lindsay, E.K.; Young, S.; Brown, K.W.; Smyth, J.M.; Creswell, J.D. Mindfulness Training Reduces Loneliness and Increases Social Contact in a Randomized Controlled Trial. Proc. Natl. Acad. Sci. USA 2019, 116, 3488–3493. [Google Scholar] [CrossRef] [Green Version]
- Hashizume, S.; Nakano, M.; Kubota, K.; Sato, S.; Himuro, N.; Kobayashi, E.; Takaoka, A.; Fujimiya, M. Mindfulness Intervention Improves Cognitive Function in Older Adults by Enhancing the Level of MiRNA-29c in Neuron-Derived Extracellular Vesicles. Sci. Rep. 2021, 11, 21848. [Google Scholar] [CrossRef] [PubMed]
- Perona-Garcelán, S.; García-Montes, J.M.; Rodríguez-Testal, J.F.; López-Jiménez, A.M.; Ruiz-Veguilla, M.; Ductor-Recuerda, M.J.; Benítez-Hernández, M.d.M.; Arias-Velarde, M.Á.; Gómez-Gómez, M.T.; Pérez-Álvarez, M. Relationship Between Childhood Trauma, Mindfulness, and Dissociation in Subjects With and Without Hallucination Proneness. J. Trauma Dissociation 2014, 15, 35–51. [Google Scholar] [CrossRef] [PubMed]
- Poli, A.; Maremmani, A.G.I.; Conversano, C.; Muscas, G.; Gemignani, A.; Pozza, A.; Miccoli, M. Different Dissociation and Alexithymia Domains Specifically Relate to Patients with Psychogenic Non-Epileptic Seizures (PNES) and with PNES and Comorbid Epilepsy (PNES+EP). J. Affect. Disord. Rep. 2022, 7, 100296. [Google Scholar] [CrossRef]
- D’Antoni, F.; Feruglio, S.; Matiz, A.; Cantone, D.; Crescentini, C. Mindfulness Meditation Leads To Increased Dispositional Mindfulness And Interoceptive Awareness Linked To A Reduced Dissociative Tendency. J. Trauma Dissociation 2021, 23, 8–23. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).