Effects of Mind-Body Interventions on Adolescents’ Cooperativeness and Emotional Symptoms
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Participants
2.3. Trainings
2.4. Self-Report Measures
2.4.1. Temperament and Character Inventory-125
2.4.2. Strengths and Difficulties Questionnaire—Adolescents Version
2.4.3. Daily Practice Diaries
2.5. Data Analysis
3. Results
3.1. Training Attendance and Practice Time
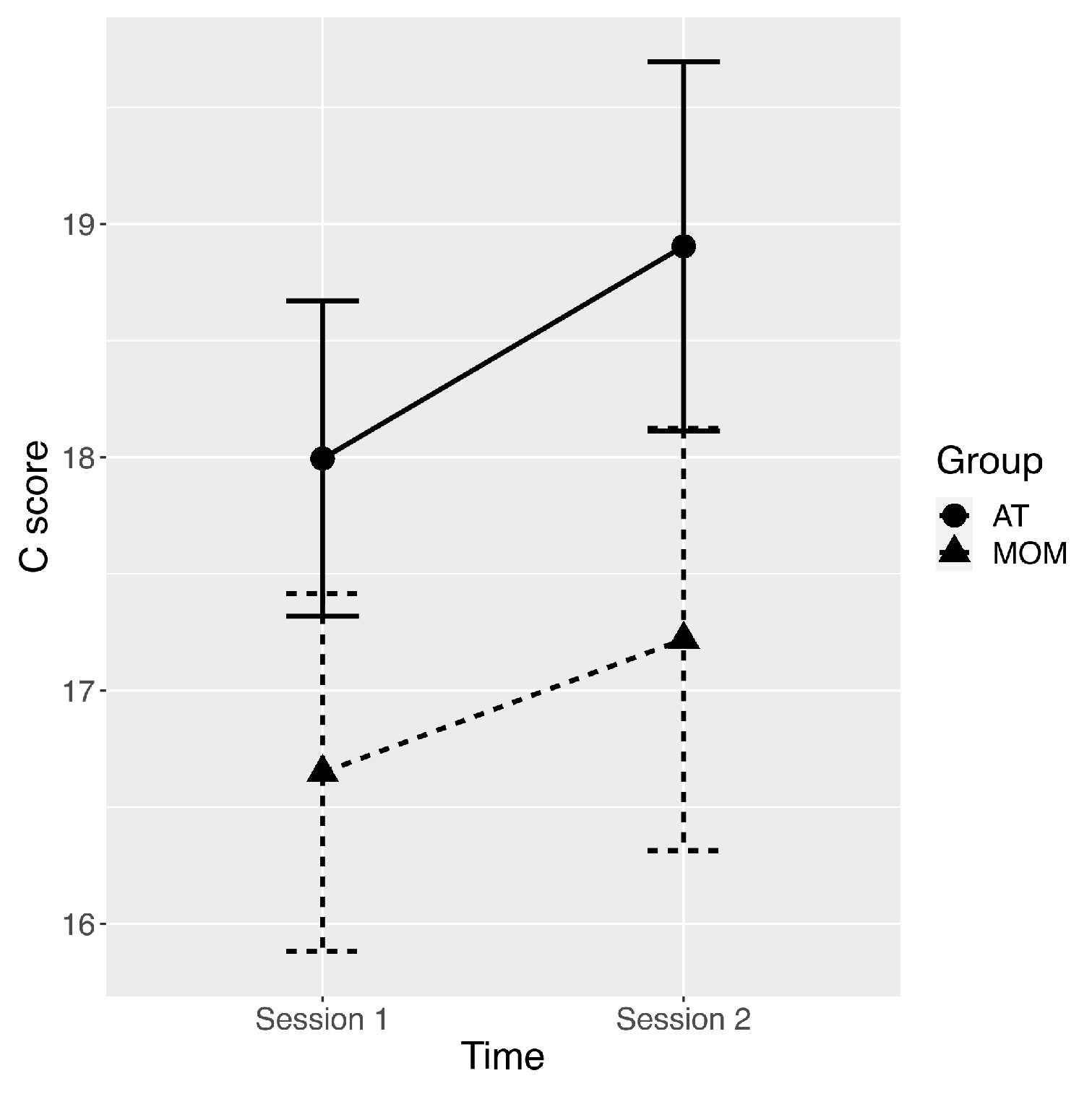
3.2. Changes in Character Traits
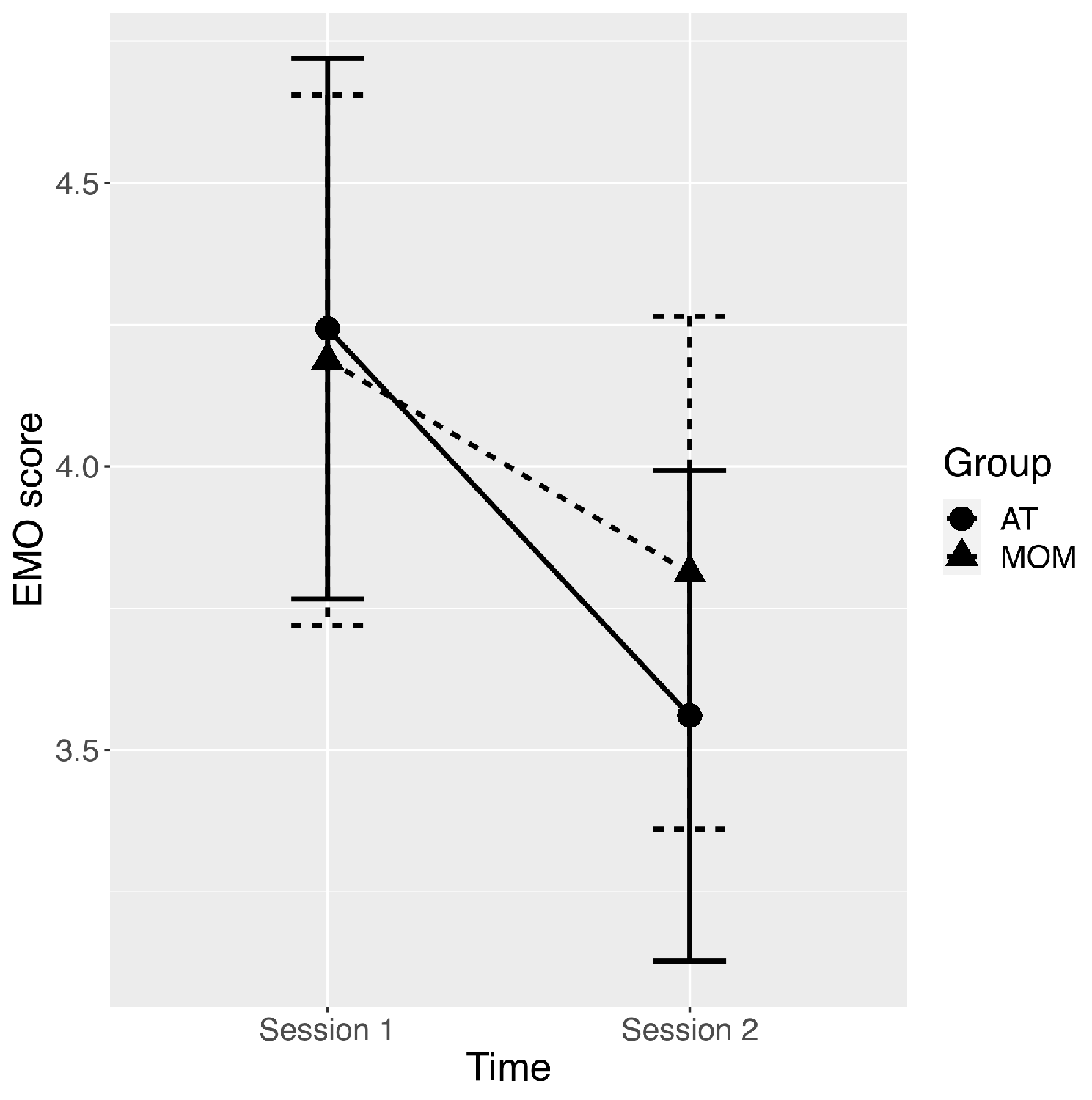
3.3. Changes in Strengths and Difficulties Questionnaire
3.4. Correlations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Paus, T.; Keshavan, M.; Giedd, J.N. Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lambert, S.F.; Copeland-Linder, N.; Ialongo, N.S. Longitudinal associations between community violence exposure and suicidality. J. Adolesc. Health 2008, 43, 380–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burke, C.A. Mindfulness-based approaches with children and adolescents: A preliminary review of current research in an emergent field. J. Child Fam. Stud. 2010, 19, 133–144. [Google Scholar] [CrossRef]
- Grant, K.E.; Compas, B.E.; Thurm, A.E.; McMahon, S.D.; Gipson, P.Y.; Campbell, A.J.; Krochock, K.; Westerholm, R.I. Stressors and child and adolescent psychopathology: Evidence of moderating and mediating effects. Clin. Psychol. Rev. 2006, 26, 257–283. [Google Scholar] [CrossRef] [PubMed]
- Neil, A.L.; Christensen, H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin. Psychol. Rev. 2009, 29, 208–215. [Google Scholar] [CrossRef] [PubMed]
- McGrath, A.P.; Holahan, A. Psychological interventions with children and adolescents: Evidence for their effectiveness in treating chronic pain. Semin. Pain Med. 2003, 1, 99–109. [Google Scholar] [CrossRef]
- Steinberg, L. Adolescent development and juvenile justice. Annu. Rev. Clin. Psychol. 2009, 5, 459–485. [Google Scholar] [CrossRef] [Green Version]
- Dray, J.; Bowman, J.; Campbell, E.; Freund, M.; Wolfenden, L.; Hodder, R.K.; Bailey, J. Systematic review of universal resilience-focused interventions targeting child and adolescent mental health in the school setting. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 813–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organisation (n.d.). Child and Adolescent Mental and Brain Health. 2021. Available online: http://www.who.int/mental_health/maternal_child/child_adolescent/en/ (accessed on 20 November 2021).
- Calear, A.L.; Christensen, H. Systematic review of school-based prevention and early intervention programs for depression. J. Adolesc. 2010, 33, 429–438. [Google Scholar] [CrossRef]
- Nehmy, T.J.; Wade, T.D. Reducing the onset of negative affect in adolescents: Evaluation of a perfectionism program in a universal prevention setting. Behav. Res. Ther. 2015, 67, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.; Ensor, R. Individual differences in growth in executive function across the transition to school predict externalizing and internalizing behaviors and self-perceived academic success at 6 years of age. J. Exp. Child. Psychol. 2011, 108, 663–776. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.; Gauntlett-Gilbert, J. Mindfulness with children and adolescents: Effective clinical application. Clin. Child. Psychol. Psychiatry 2008, 13, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Bronson, M.B. Recognizing and supporting the development of self-regulation in young children. Young Child. 2000, 55, 32–37. [Google Scholar]
- Zeman, J.; Cassano, M.; Perry-Parrish, C.; Stegall, S. Emotion regulation in children and adolescents. J. Dev. Behav. Pediatr. 2006, 27, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Frick, P.J.; Morris, A.S. Temperament and developmental pathways to conduct problems. J. Clin. Child. Adolesc. Psychol. 2004, 33, 54–68. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Galla, B.M.; Duckworth, A.L. More than resisting temptation: Beneficial habits mediate the relationship between self-control and positive life outcomes. J. Pers. Soc. Psychol. 2015, 109, 508–525. [Google Scholar] [CrossRef]
- Moffitt, T.E.; Arseneault, L.; Belsky, D.; Dickson, N.; Hancox, R.J.; Harrington, H.; Houts, R.; Poulton, R.; Roberts, B.W.; Ross, S.; et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc. Natl. Acad. Sci. USA 2011, 108, 2693–2698. [Google Scholar] [CrossRef] [Green Version]
- Pandey, A.; Hale, D.; Das, S.; Goddings, A.L.; Blakemore, S.J.; Viner, R.M. Effectiveness of Universal Self-Regulation-Based Interventions in Children and Adolescents: A Systematic Review and Meta-analysis. JAMA Pediatr. 2018, 172, 566–575. [Google Scholar] [CrossRef] [Green Version]
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion: New York, NY, USA, 1994. [Google Scholar]
- Kabat-Zinn, J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 1982, 4, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J.; Lipworth, L.; Burney, R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J. Behav. Med. 1985, 8, 163–190. [Google Scholar] [CrossRef] [PubMed]
- De Vibe, M.; Solhaug, I.; Tyssen, R.; Friborg, O.; Rosenvinge, J.H.; Sørlie, T.; Bjørndal, A. Mindfulness training for stress management: A randomised controlled study of medical and psychology students. BMC Med. Educ. 2013, 13, 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Segal, Z.V.; Williams, J.G.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse; Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Shapiro, S.L.; Brown, K.W.; Thoresen, C.; Plante, T.G. The moderation of Mindfulness-based stress reduction effects by trait mindfulness: Results from a randomized controlled trial. J. Clin. Psychol. 2011, 67, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Krasner, M.S.; Epstein, R.M.; Beckman, H.; Suchman, A.L.; Chapman, B.; Mooney, C.J.; Quill, T.E. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009, 302, 1284–1293.19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olson, K.; Kemper, K.J. Factors associated with well-being and confidence in providing compassionate care. J. Evid.-Based Complementary Altern. Med. 2014, 19, 292–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, S.L.; Shapiro, D.E.; Schwartz, G.E. Stress management in medical education: A review of the literature. Acad. Med. 2000, 75, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Dobkin, P.L.; Hutchinson, T.A. Teaching mindfulness in medical school: Where are we now and where are we going? Med. Educ. 2013, 47, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Erogul, M.; Singer, G.; McIntyre, T.; Stefanov, D.G. Abridged mindfulness intervention to support wellness in first-year medical students. Teach. Learn. Med. 2014, 26, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Malpass, A.; Binnie, K.; Robson, L. Medical Students’ Experience of Mindfulness Training in the UK: Well-Being, Coping Reserve, and Professional Development. Educ Res. Int. 2019, 2019, 4021729. [Google Scholar] [CrossRef]
- Semple, R.J.; Droutman, V.; Reid, B.A. Mindfulness goes to school: Things learned (so far) from research and real-word experience. Psychol. Sch. 2017, 54, 29–52. [Google Scholar] [CrossRef] [Green Version]
- Johnson, C.; Burke, C.; Brinkman, S.; Wade, T. A randomized controlled evaluation of a secondary school mindfulness program for early adolescents: Do we have the recipe right yet? Behav. Res. Ther. 2017, 99, 37–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry-Parrish, C.; Copeland-Linder, N.; Webb, L.; Shields, A.H.; Sibinga, E.M. Improving self-regulation in adolescents: Current evidence for the role of mindfulness-based cognitive therapy. Adolesc. Health Med. Ther. 2016, 7, 101–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fortney, L.; Luchterhand, C.; Zakletskaia, L.; Zgierska, A.; Rakel, D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: A pilot study. Ann. Fam. Med. 2013, 11, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.M.; Pagnini, F.; Castelnuovo, G.; Molinari, E. Relaxation training for anxiety: A ten-years systematic review with meta-analysis. BMC Psychiatry 2008, 8, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institutes of Health. Relaxation Techniques: What You Need to Know. National Center for Complementary and Integrative Health. 2021. Available online: https://www.nccih.nih.gov/health/relaxation-techniques-what-you-need-to-know. (accessed on 20 November 2021).
- Dunning, D.L.; Griffiths, K.; Kuyken, W.; Crane, C.; Foulkes, L.; Parker, J.; Dalgleish, T. Research Review: The effects of mindfulness-based interventions on cognition and mental health in children and adolescents—A meta-analysis of randomized controlled trials. J. Child. Psychol. Psychiatry 2019, 60, 244–258. [Google Scholar] [CrossRef] [Green Version]
- Goldbeck, L.; Schmid, K. Effectiveness of autogenic relaxation training on children and adolescents with behavioral and emotional problems. J. Am. Acad. Child. Adolesc. Psychiatry 2003, 42, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Shapiro, S.L.; Swanick, S.; Roesch, S.C.; Mills, P.J.; Bell, I.; Schwartz, G.E.R. A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Ann. Behav. Med. 2007, 33, 11–21. [Google Scholar] [CrossRef]
- Kuhlmann, S.M.; Huss, M.; Bürger, A.; Hammerle, F. Coping with stress in medical students: Results of a randomized controlled trial using a mindfulness-based stress prevention training (MediMind) in Germany. BMC Med. Educ. 2016, 16, 316. [Google Scholar] [CrossRef] [Green Version]
- Crescentini, C.; Garzitto, M.; Paschetto, A.; Brambilla, P.; Fabbro, F. Temperament and character effects on late adolescents’ well-being and emotional-behavioural difficulties. PeerJ 2018, 6, e4484. [Google Scholar] [CrossRef] [Green Version]
- Cloninger, C.R.; Svrakic, D.M.; Przybeck, T.R. A psychobiological model of temperament and character. Arch. Gen. Psychiatry 1993, 50, 975–990. [Google Scholar] [CrossRef] [PubMed]
- Cloninger, C.R. The Temperament and Character Inventory (TCI): A Guide to Its Development and Use; Centre for Psychobiology of Personality, Washington University: St Louis, MO, USA, 1994. [Google Scholar]
- Garcia, D.; Moradi, S. Adolescents’ Temperament and Character: A Longitudinal Study on Happiness. J. Happiness Stud. 2012, 13, 931–946. [Google Scholar] [CrossRef]
- Gillham, J.; Adams-Deutsch, Z.; Werner, J.; Reivich, K.; Coulter-Heindl, V.; Linkins, M.; Winder, B.; Peterson, C.; Park, N.; Abenavoli, R.; et al. Character strengths predict subjective well-being during adolescence. J. Posit. Psychol. 2011, 6, 31–44. [Google Scholar] [CrossRef]
- Bromley, E.; Johnson, J.G.; Cohen, P. Personality strengths in adolescence and decreased risk of developing mental health problems in early adulthood. Compr. Psychiatry 2006, 47, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Garcia, D. Two models of personality and well-being among adolescents. Personal. Individ. Differ. 2011, 50, 1208–1212. [Google Scholar] [CrossRef]
- Crescentini, C.; Urgesi, C.; Campanella, F.; Eleopra, R.; Fabbro, F. Effects of an 8-week meditation program on the implicit and explicit attitudes toward religious/spiritual self-representations. Conscious. Cogn. 2014, 30, 266–280. [Google Scholar] [CrossRef] [PubMed]
- Fabbro, F.; Crescentini, C. La meditazione orientata alla mindfulness (mom) nella ricerca psicologica. Ric. Psicol. 2017, 457–472. [Google Scholar] [CrossRef] [Green Version]
- Matiz, A.; Fabbro, F.; Crescentini, C. Single vs. Group Mindfulness Meditation: Effects on Personality, Religiousness/Spirituality, and Mindfulness Skills. Mindfulness 2018, 9, 1236–1244. [Google Scholar] [CrossRef]
- Schultz, J.H.; Luthe, W. Autogenic Training: A Psychophysiologic Approach to Psychotherapy; Grune & Stratton: New York, USA, 1959. [Google Scholar]
- Delvecchio, G.; Garzitto, M.; Fagnani, C.; Fornasari, L.; Stazi, M.A.; Picardi, A.; Ciappolino, V.; Fabbro, F.; Altamura, A.C.; Brambilla, P. Normative data and effects of age and gender on temperament and character dimensions across the lifespan in an Italian population: A cross-sectional validation study. J. Affect. Disord. 2016, 204, 83–91. [Google Scholar] [CrossRef]
- Svrakic, D.M.; Whitehead, C.; Przybeck, T.R.; Cloninger, C.R. Differential diagnosis of personality disorders by the seven-factor model of temperament and character. Arch. Gen. Psychiatry 1993, 50, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Publishing, Inc.: Washington, DC, USA, 1994. [Google Scholar]
- Hashim, H.A.; Hanafi Ahmad Yusof, H. The effects of progressive muscle relaxation and autogenic relaxation on young soccer players’ mood states. Asian J. Sports Med. 2011, 2, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Kemper, K.J.; Khirallah, M. Acute Effects of Online Mind-Body Skills Training on Resilience, Mindfulness, and Empathy. J. Evid.-Based Complementary Altern Med. 2015, 20, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Pepper, E.; Harvey, R.; Lin, I.M. Mindfulness training has elements common to other techniques. Biofeedback 2019, 47, 50–57. [Google Scholar] [CrossRef]
- Berry, D.R.; Cairo, A.H.; Goodman, R.J.; Quaglia, J.T.; Green, J.D.; Brown, K.W. Mindfulness increases prosocial responses toward ostracized strangers through empathic concern. J. Exp. Psychol. Gen. 2018, 147, 93–112. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, E.K.; Chin, B.; Greco, K.M.; Young, S.; Brown, K.W.; Wright, A.G.C.; Smyth, J.M.; Burkett, D.; Creswell, J.D. How mindfulness training promotes positive emotions: Dismantling acceptance skills training in two randomized controlled trials. J. Pers. Soc. Psychol. 2018, 115, 944–973. [Google Scholar] [CrossRef]
- Vago, D.R.; Silbersweig, D.A. Self-awareness, self-regulation, and self-transcendence (S-ART): A framework for understanding the neurobiological mechanisms of mindfulness. Front. Hum. Neurosci. 2012, 6, 296. [Google Scholar] [CrossRef] [Green Version]
- Pidgeon, A.M.; Ford, L.; Klaassen, F. Evaluating the effectiveness of enhancing resilience in human service professionals using a retreat-based Mindfulness with Metta Training Program: A randomised control trial. Psychol. Health Med. 2014, 19, 355–364. [Google Scholar] [CrossRef]
- Kuyken, W.; Weare, K.; Ukoumunne, O.C.; Vicary, R.; Motton, N.; Burnett, R.; Cullen, C.; Hennelly, S.; Huppert, F. Effectiveness of the Mindfulness in Schools Programme: Non-randomised controlled feasibility study. Br. J. Psychiatry 2013, 203, 126–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry-Parrish, C.; Copeland-Linder, N.; Webb, L.; Sibinga, E.M. Mindfulness-Based Approaches for Children and Youth. Curr. Probl. Pediatr. Adolesc. Health Care 2016, 46, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Raes, F.; Griffith, J.W.; Gucht, K.V.; Williams, J.M. School-Based Prevention and Reduction of Depression in Adolescents: A Cluster-Randomized Controlled Trial of a Mindfulness Group Program. Mindfulness 2014, 5, 477–486. [Google Scholar] [CrossRef]
- Condon, P.; Desbordes, G.; Miller, W.B.; De Steno, D. Meditation increases compassionate responses to suffering. Psychol. Sci. 2013, 24, 2125–2127. [Google Scholar] [CrossRef] [PubMed]
- Donald, J.N.; Sahdra, B.K.; Van Zanden, B.; Duineveld, J.J.; Atkins, P.W.B.; Marshall, S.L.; Ciarrochi, J. Does your mindfulness benefit others? A systematic review and meta-analysis of the link between mindfulness and prosocial behaviour. Br. J. Psychol. 2019, 110, 101–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durlak, J.A.; Weissberg, R.P.; Dymnicki, A.B.; Taylor, R.D.; Schellinger, K.B. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child Dev. 2011, 82, 405–432. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.; Burke, C.; Brinkman, S.; Wade, T. Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behav. Res. Ther. 2016, 81, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Cloninger, C.R. Feeling good: The Science of Well-Being; Oxford University Press: Oxford, UK, 2008; p. 374. [Google Scholar]
- Greenberg, M.T.; Weissberg, R.P.; O’Brien, M.U.; Zins, J.E.; Fredericks, L.; Resnik, H.; Elias, M.J. Enhancing school-based prevention and youth development through coordinated social, emotional, and academic learning. Am. Psychol. 2003, 58, 466–474. [Google Scholar] [CrossRef]
- Sibinga, E.M.; Kemper, K.J. Complementary, holistic, and integrative medicine: Meditation practices for pediatric health. Pediatr. Rev. 2010, 31, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Masters-Waage, T.; Nai, J.; Reb, J.; Sim, S.; Narayanan, J.; Tan, N. Going far together by being here now: Mindfulness increases cooperation in negotiations. Organ. Behav. Hum. Decis. Processes 2021, 167, 189–205. [Google Scholar] [CrossRef]
- Lindsay, E.K.; Creswell, J.D. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clin. Psychol. Rev. 2017, 51, 48–59. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, S.L.; Carlson, L.E.; Astin, J.A.; Freedman, B. Mechanisms of mindfulness. J. Clin. Psychol. 2006, 62, 373–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hölzel, B.K.; Carmody, J.; Vangel, M.; Congleton, C.; Yerramsetti, S.M.; Gard, T.; Lazar, S.W. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011, 191, 36–43. [Google Scholar] [CrossRef] [Green Version]
- Hölzel, B.K.; Lazar, S.W.; Gard, T.; Schuman-Olivier, Z.; Vago, D.R.; Ott, U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action from a Conceptual and Neural Perspective. Perspect. Psychol. Sci. 2011, 6, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Jojić, B.R.; Leposavić, L.M. Autogenic training as a therapy for adjustment disorder in adolescents. Srp. Arh. Celok. Lek. 2005, 133, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Klott, O. Autogenic Training—A self-help technique for children with emotional and behavioural problems. Therapeutic Communities: Int. J. Ther. Communities 2013, 34, 152–158. [Google Scholar] [CrossRef]
- Kanji, N.; White, A.; Ernst, E. Autogenic training to reduce anxiety in nursing students: Randomized controlled trial. J. Adv. Nurs. 2006, 53, 729–735. [Google Scholar] [CrossRef] [PubMed]
- De Rivera, L.; Ozamiz-Etxebarria, N.; Dosil-Santamaría, M.; De Rivera-Monterrey, L. Autogenic Training Improves the Subjective Perception of Physical and Psychological Health and of Interpersonal Relational Abilities: An Electronic Field Survey During the COVID-19 Crisis in Spain. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef]
- Hinshaw, S.P.; Han, S.S.; Erhardt, D.; Huber, A. Internalizing and externalizing behavior problems in preschool children: Correspondence among parent and teacher ratings and behavior observations. J. Clin. Child Psychol. 1992, 21, 115–122. [Google Scholar] [CrossRef]
- Perry-Parrish, C.; Waasdorp, T.E.; Bradshaw, C.P. Peer Nominations of Emotional Expressivity among Urban Children: Social and Psychological Correlates. Soc. Dev. 2012, 21, 88–108. [Google Scholar] [CrossRef] [Green Version]
- Bartels, M.; Van de Aa, N.; Van Beijsterveldt, C.E.; Middeldorp, C.M.; Boomsma, D.I. Adolescent self-report of emotional and behavioral problems: Interactions of genetic factors with sex and age. J. Can. Acad. Child. Adolesc. Psychiatry 2011, 20, 35–52. [Google Scholar]
- Parsons, C.E.; Crane, C.; Parsons, L.J.; Fjorback, L.O.; Kuyken, W. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav. Res. Ther. 2017, 95, 29–41. [Google Scholar] [CrossRef] [Green Version]
| MOM Group (N = 32) | AT Group (N = 37) | 2 × 2 Anova | ||||||
|---|---|---|---|---|---|---|---|---|
| Session 1 Mean SD | Session 2 Mean SD | Session 1 Mean SD | Session 2 Mean SD | Group ψ/F † p | Session ψ/F † p | Group: Session ψ/F † p | ||
| TCI (Character) | SD | 13.50 5.45 | 12.81 5.91 | 15.43 5.51 | 16.42 5.50 | 4.86 † 0.031 * | 0.08 † 0.77 | 2.62 † 0.11 |
| C | 16.65 4.33 | 17.22 5.12 | 17.99 4.05 | 18.90 4.75 | 1.9 0.20 | −1.1 0.001 * | −0.1 0.90 | |
| ST | 6.97 3.55 | 6.75 3.33 | 6.36 3.23 | 6.45 3.39 | −0.4 0.66 | 0.0 0.81 | −0.5 0.19 | |
| SDQ-A | EMO | 4.19 2.64 | 3.81 2.56 | 4.24 2.90 | 3.56 2.63 | 0.3 0.71 | 0.8 0.002 * | 0.7 0.12 |
| BEH | 2.87 2.07 | 2.75 1.74 | 2.70 1.91 | 2.24 1.92 | −0.6 0.16 | 0.1 0.48 | 0.4 0.24 | |
| HYP | 4.56 1.56 | 4.59 2.17 | 3.95 2.01 | 3.73 1.91 | −0.6 0.17 | −0.1 0.59 | 0.1 0.80 | |
| PEE | 2.97 2.10 | 3.29 2.30 | 2.78 2.00 | 2.62 1.30 | −0.7 0.16 | −0.2 0.44 | 0.0 0.96 | |
| PRO | 7.59 1.96 | 8.00 1.87 | 6.95 2.08 | 7.32 2.08 | −1.0 0.06 | −0.2 0.24 | 0.1 0.67 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feruglio, S.; Pascut, S.; Matiz, A.; Paschetto, A.; Crescentini, C. Effects of Mind-Body Interventions on Adolescents’ Cooperativeness and Emotional Symptoms. Behav. Sci. 2022, 12, 33. https://doi.org/10.3390/bs12020033
Feruglio S, Pascut S, Matiz A, Paschetto A, Crescentini C. Effects of Mind-Body Interventions on Adolescents’ Cooperativeness and Emotional Symptoms. Behavioral Sciences. 2022; 12(2):33. https://doi.org/10.3390/bs12020033
Chicago/Turabian StyleFeruglio, Susanna, Stefania Pascut, Alessio Matiz, Andrea Paschetto, and Cristiano Crescentini. 2022. "Effects of Mind-Body Interventions on Adolescents’ Cooperativeness and Emotional Symptoms" Behavioral Sciences 12, no. 2: 33. https://doi.org/10.3390/bs12020033
APA StyleFeruglio, S., Pascut, S., Matiz, A., Paschetto, A., & Crescentini, C. (2022). Effects of Mind-Body Interventions on Adolescents’ Cooperativeness and Emotional Symptoms. Behavioral Sciences, 12(2), 33. https://doi.org/10.3390/bs12020033







