Abstract
Background: Mind-body interventions may support the development of adolescents’ self-regulation and provide a protective effect against maladaptive outcomes, e.g., internalizing and externalizing problems. The present study aimed at evaluating the effects of mindfulness-oriented meditation training (MOM) and autogenic training (AT) on a group of healthy Italian adolescents’ character dimensions, emotional and behavioral difficulties. Methods: 72 adolescents were randomly assigned to MOM/AT conditions and tested before and after the 8-week trainings through self-report measures (Temperament and Character Inventory 125, TCI; Strengths and Difficulties Questionnaire for Adolescents, SDQ-A). Main analyses involved robust and repeated measures ANOVAs, carried out separately for character TCI and SDQ-A scales. Results: After trainings, we found increased levels of cooperativeness and reduced emotional symptoms. Changes in these dimensions were negatively correlated: the more participants increased in their cooperativeness the greater decrease they showed in emotional symptoms. Conclusion: Both MOM and AT enhanced a cooperative attitude in adolescents and helped reducing their emotional problems. Therefore, it may be useful to apply these mind-body interventions in school settings as they can have a protective effect on the well-being and psychosocial adjustment of youths, through fostering their character maturity and helping them to better regulate their emotions.
1. Introduction
Adolescence is a period of development and change for youths across multiple domains [1]. Exposure to some stressors increases as youths age into adolescence [2] and this has been associated with maladaptive outcomes, including internalizing problems, externalizing behaviors, academic difficulties, and health risk behaviors [3,4]. Increasingly, there are calls for further investigation on how to reduce the maladaptive aspects of stress experienced in adolescence which are often related to long-term problems, as well as the risk of developing psychological difficulties in adult life; for example, anxiety, depression and eating disorders typically emerge in mid-late adolescence and tend to become chronic [5,6]. The impact of such determinants can be mitigated by protective factors, such as good adaptive coping and emotion regulation strategies, prosocial behavior and social connectedness, as well as support from schools and mental health services [7,8,9].
School-based prevention programs offer a means of targeting a broad portion of the population at or before the peak emergence of critical conditions, especially with programs offered to all students, thus avoiding the disadvantages of selecting out at-risk individuals, e.g., lack of failsafe screening and potential stigmatization [10,11]. Interventions that reinforce adolescents’ capacity for coping with stressful circumstances, by targeting the emotional and attentional processes associated with stress, may support the development of adolescents’ self-regulation and provide a protective effect against maladaptive outcomes, including internalizing problems and externalizing behaviors [12,13]. Self-regulation (SR) is a psychological construct which encompasses a range of important competencies, including the capacity for controlling one’s emotions, the ability to have positive interactions with others, and the capacity for avoiding inappropriate or aggressive actions [14]. Particularly, SR of negative emotions [15], such as anger and sadness, is related to social and peer acceptance across childhood and adolescence. Emotion regulation is regarded as a fundamental aspect of many kinds of youth psychopathology [16] and a potential mediator of the relationship between exposure to risk and healthy developmental outcomes for minority youth [17]. There is growing evidence that SR and emotion regulation play an important foundational role in development and maintenance of physical health and well-being in childhood and across the lifespan [18,19]. A systematic review and meta-analysis of 49 randomized clinical trials evaluating SR interventions (e.g., curriculum-based, yoga and mindfulness, social and personal skills, and exercise-based interventions), found that these interventions were effective in children and adolescents (0–19 years), contributing to positive outcomes on health and social measures, such as academic achievement, social skills, mental health, reducing behavioral problems, conduct disorders, school suspensions and substance abuse [20].
In particular, mindfulness-based programs have been broadly theorized to improve SR of emotions, behavior, and cognitive processes. Mindfulness has been defined as “paying attention in a particular way: on purpose, in the present moment, and non-judgmentally” [21]. The use of mindfulness meditation practices to reduce suffering and distress has been a feature of many Eastern philosophical traditions (e.g., Buddhism) for hundreds of years, and has been increasingly used in Western medicine for well over 30 years [22,23]. Meditation practices emerged from a body of Buddhist and other contemplative traditions and represent a complementary approach to mental health and well-being that combines psychological approaches to reduce stress and discomfort, including cognitive–behavioral therapies [24,25,26], and relaxation techniques. Most of the research regarding mindfulness approaches has been conducted with adults and in professional or therapeutic contexts [27,28,29]. More recently, mindfulness-based interventions have been embraced and widely disseminated in schools [30,31,32,33], but there are still insufficient methodologically robust studies to make definitive conclusions about efficacy [34,35]. Along with mindfulness there is a wide variety of mind-body interventions that share some common goals and positive outcomes amongst young people, e.g., numerous studies have found that relaxation training correlates with reduced stress, improved symptom management and quality of life [36,37,38] and improvements in externalizing, emotional and behavioral symptoms [39,40]. Until now, few studies were designed to compare the effects of different mind-body approaches in adults or in adolescents and those studies showed contrasting results. For example, some studies [41,42] compared mindfulness meditation and different types of relaxation training (e.g., muscle relaxation, autogenic relaxation), with control groups. One study showed that both types of training had similar beneficial effects in reducing mental distress and improving a positive state of mind, while mindfulness meditation specifically reduced ruminative and distractive thoughts compared to relaxation practices [41]; in contrast, another study found no effects of mindfulness and somatic relaxation in the experience of stress and the use of coping strategies in medical students [42].
To further address this issue, the present study aimed to evaluate the effects of two mind-body interventions on adolescents, namely mindfulness-oriented meditation (MOM) and autogenic training (AT), a relaxation technique first introduced by the German psychiatrist Johannes Heinrich Schultz in 1932. AT consists of a series of relaxation exercises, in conjunction with verbal cues, to learn to regulate physical processes (e.g., breathing and warmth) to induce a state of relaxation. Both programs may positively impact adolescents’ psychosocial adjustment; more specifically, we predict that these types of training will show some beneficial effect in reducing emotional and behavioral problems in youth.
Moreover, as shown in previous studies, cognitive, emotional and social experiences could be affected by personality characteristics. In this regard, we built on previous research suggesting the importance of personality traits as protective factors for adolescents’ well-being and psychosocial functioning and the usefulness of assessing these dimensions, especially in the context of interventions that may potentially enhance some character dimensions [43]. According to the well-known temperament and character inventory of personality (TCI; [44,45]), the character, i.e., the maturity of the self, is defined at three levels: at the intrapersonal level by self-directedness (SD; the tendency to be purposeful, responsible and reliable vs. purposeless, blaming and unreliability), at the interpersonal level by cooperativeness (C; the attitude of being helpful, empathic and ethical vs. unhelpful, critical and opportunistic), and at the transpersonal level by self-transcendence (ST; the tendency to be holistic and united with the universe vs. self-centered and unimaginative). A restricted number of studies focusing on character strengths using TCI shows that adolescents who report high levels of persistence and character maturity (high scores in SD and C) [46], report low levels of depressive symptoms [46,47] and decreased risks of developing psychiatric disorders during early adulthood [48]. Previous studies also found that maturation of the self in aspects related to empathy, kindness, and forgiveness (C) was positively associated with pro-social behaviors and more marginally and negatively with total difficulties and externalizing problems [43]. Overall, these data indicate that another key element for understanding well-being and psychosocial adjustment in adolescence seems to involve the possibility to experience satisfying interactions with other individuals [49]. Thus, we took these dispositional factors into consideration; we measured changes in character dimensions and the psychosocial adjustment of adolescents before and after their attendance on a mindfulness-based and an AT course. We predicted finding some positive changes in these measures after the 8-week trainings, as a result of enhanced self-regulatory processes in youth.
2. Materials and Methods
2.1. Procedure
The research study involved seventy-two adolescents aged between 16 and 20 years recruited in two five-year high schools, located in two small cities of approximately 7000 and 14,000 inhabitants in the north-east of Italy (i.e., Lignano Sabbiadoro and Latisana). Students belonged to four classes: the 3rd and 4th grade of a technical high school, and the 3rd and 4th grade of a scientific and linguistic high school. The schools were randomly assigned to a MOM or an AT condition, resulting in one 3rd and one 4th grade class assigned to each training. The training programs were led by two expert instructors of mindfulness meditation and autogenic practices, who were both present in each group meeting (more specifically, one expert conducted the MOM practices and the other conducted the AT practices; they held all group discussions, which took place after the practices, together). The participants were tested twice, before the beginning and after the end of the courses (Session 1: first weeks of March 2017, and Session 2: last weeks of May 2017), through two self-report measures, the TCI and SDQ-A. Questionnaires were administered in groups in participants’ classrooms, in the presence of their teacher and a research psychologist. The courses were designed to be comparable and structurally equivalent; they lasted 8 weeks, during which participants attended a group session once per week. Group sessions for both training programs took place during morning school time, on consecutive days. All the subjects were invited to continue to practice daily at home and to record in a diary each individual session. This study was approved by the Ethics Committee of the University of Udine (Ethical Application Ref: CGPER-2016-11-23-01) and all procedures performed in the study were in accordance with the ethical standards of the 1964 Helsinki declaration and its later amendments.
2.2. Participants
Seventy-two adolescents aged between 16 and 20 years (M = 17.5 ± 0.75; 63.9% females) participated in the study. In total, 69 participants completed the training and the research questionnaires. We thus excluded 3 participants who had not concluded the training or the research questionnaires. All participants were volunteers and were previously informed about the research purposes according to procedures reviewed by their schools. More specifically, the study methodology, aims and procedures were presented to teachers, parents and students in a school general assembly by the experts, with the opportunity to ask questions and seek clarification from the researchers. All recruited participants reported no past history of neurological or mental illness and had no previous experience with MOM and AT training or with the outcome measures used in the study.
2.3. Trainings
The mindfulness-oriented meditation training (MOM) [50,51,52] was an 8-week course in which participants attended a 2 h group session once per week. In each group-session they were taught some theoretical aspects related to mindfulness (e.g., attention regulation, equanimity, defusion, etc.), then they practiced 30 min of meditation (10 min focus on breath, 10 min body scan and 10 min observing contents of the mind), and finally they had a group discussion about meditation practice. The participants were also asked to meditate autonomously at home every day, following an audio-recorded meditation equivalent to that performed during group meetings, and to record each session in a diary. The general purpose of mindfulness-based meditation is to cultivate a state of open, non-judgmental, and not necessarily relaxing, awareness in the present moment.
The autogenic training (AT) [53] was structurally equivalent to the MOM course. In the 2 h group-sessions, participants were invited to use physical processes, in conjunction with verbal cues, to relax and learn to regulate some autonomic activities and internal processes, including breathing and warmth, paying attention to the heartbeat, abdominal sensations, and the coolness of the forehead. After a theoretical introduction lasting up to 30 min and 30 min of guided practice, participants had a group discussion. All the participants were asked to continue to practice daily the same exercises practiced in group and to record each session in a diary. The general purpose of autogenic practice is to enhance a state of calmness and relaxation.
2.4. Self-Report Measures
2.4.1. Temperament and Character Inventory-125
Personality was assessed by the 125-item version of the self-report form of the TCI [45], administered using the Italian adaptation [54]. The TCI-125 operationalizes Cloninger’s personality model [44] with items organized into four temperament scales and three character scales. For the purpose of the present study, we report here the results concerning the character dimensions, namely SD, implying an autonomous self-concept and feelings of hope, honor and self-confidence; C, involving interindividual differences in the acceptance of others, compassion, and charity; and ST, consisting of creative self-forgetfulness, transpersonal identification, and spiritual acceptance. Character traits refer to interindividual differences in the conceptual representation of the self in relation to other people and to the external world and may be related to the functioning of higher cognitive systems [45,55]. Each item requires a True or False response and a higher final score for each scale corresponds to higher levels of SD, CO and ST traits. The three TCI character scales showed good psychometric properties in Italian adolescents: SD α = 0.75, C α = 0.81, ST α = 0.72 [54]. In addition, in our sample the average Cronbach’s alpha of Session 1 and Session 2 was good for SD (α = 0.85), CO (α = 0.82), and ST (α = 0.77).
2.4.2. Strengths and Difficulties Questionnaire—Adolescents Version
The self-report form SDQ-A [56,57] was used as a reliable measure covering the most important domains of psychopathology in a normal school-age population. The rationale for the scales was based on nosological criteria from the Diagnostic and Statistical Manual of Mental Disorders (4th ed., DSM-IV) [58]. The SDQ-A is composed of 25 items, organized in five 5-item scales: Emotional symptoms, (EMO, example item: ‘I am often unhappy, depressed or tearful’), Peer problems (PEE, example item: ‘I am usually on my own’), Conduct problems (BEH, example item: ‘I am often accused of lying or cheating’), Hyperactivity/Inattention (HYP, example item: ‘I am restless. I cannot stay still for long’), and Prosocial behaviors (PRO, example item: ‘I am helpful if someone is hurt, upset or feeling ill’). All items are rated on a 3-point rating scale (0 for “not true,” 1 for “somewhat true” and 2 for “certainly true”). The total scores of each scale range from 0 to 10. Higher scores correspond to higher levels of difficulties in EMO, BEH, HYP, PEE scales and to a higher propensity for prosocial behaviors for the PRO scale. The SDQ-A scales showed acceptable psychometric properties in adolescents for EMO (α = 0.66), BEH (α = 0.60), HYP (α = 0.67) and PRO (α = 0.66), while PEE showed poor internal consistency reliability (α = 0.41) [57]. In our sample the mean Cronbach’s alpha of Session 1 and Session 2 was good for EMO (α = 0.77), it was acceptable for HYP (α = 0.62) and PRO (α = 0.64), while it was poor for BEH (α = 0.59) and PEE (α = 0.53).
2.4.3. Daily Practice Diaries
All participants attending the MOM and AT programs were asked to complete diaries on daily practice. More specifically, they were asked to report daily if they practiced individually at home, for how long and at what time of the day. They were also free to report any comments or personal experiences about their practice that they might want to share during the following group discussion.
2.5. Data Analysis
Continuous measures were summarized reporting mean and standard deviation of raw data obtained before and after trainings in the MOM and AT groups (Table 1). One participant of the AT group did not fill in the TCI character scales at Session 1 and one participant of the MOM group did not fill in the PEE scale at Session 2, thus these two subjects were excluded from the relative analyses (TCI character and PEE scales). For all other participants, the response rate was 99.7% for TCI and 99.8% for SDQ-A; scale-mean substitution was used to manage missing items. We compared the rates of group meeting attendance and the mean practice time (reported in minutes) in the MOM and AT groups using two t-tests for independent samples. Then, we tested the distribution of each questionnaire scores for normality with the Shapiro–Wilk’s W test. The main analysis concerned a series of repeated measures 2 × 2 ANOVAs and 2 × 2 ANOVAs using robust M-estimators with 2000 bootstraps for not normally distributed data, carried out separately for the different TCI character scales (SD, C, ST) and the SDQ-A scales (EMO, BEH, HYP, PEE, PRO), with Session (Session 1 and Session 2) as a within-subjects factor and Group (MOM and AT) as a between-subjects factor. Correlational analysis was employed to examine the relationship between post-pre training changes of the TCI and SDQ-A measures where significant differences were observed in the before vs. after training comparison of means. Overall, the conventional level of p < 0.05 was used as a statistical threshold of significance. All analyses were conducted using JASP (version 0.16) and R (version 3.6.3) software.

Table 1.
Descriptive statistics of raw data obtained before and after trainings in the MOM and AT groups and results (main effects and two-way interaction) from ANOVA analyses regarding TCI character and SDQ-A scales.
3. Results
3.1. Training Attendance and Practice Time
Before performing the main analyses, we compared the two groups in terms of attendance at group meetings and individual practice time: participants to the MOM group had, on average, 1.19 absences (sd = 0.90), while the mean for the AT group was 0.59 (sd = 0.93); the total individual practice time accumulated during the training was, on average, 500.69 min (sd = 217.20) for the MOM group, and 600.57 min (sd = 434.36) for the AT group. The MOM group had a significantly higher absence rate (t = −2.691, df = 67, p = 0.009), but the two groups did not differ significantly in total practice time reported by participants (t = 1.179, df = 67, p = 0.24).
3.2. Changes in Character Traits
A Shapiro–Wilk’s test showed that the TCI character scores of C and ST scales were not normally distributed at Session 1 in the AT group (p < 0.05). On the basis of two 2 (Session: Session 1 and Session 2) × 2 (Group: MOM and AT) ANOVAs using robust M-estimator and 2000 bootstraps carried out on C and ST scores, there was a significant main effect of Session for the C scale (Session 2 > Session 1; ψ = −1.1, p = 0.001, see Table 1 and Figure 1). On the basis of a 2 (Session: Session 1 and Session 2) × 2 (Group: MOM and AT) repeated measures ANOVA carried out on SD scores, there was a significant main effect of Group (AT > MOM; F [1,66] = 4.861, p = 0.031; ηp2 = 0.069, see Table 1). No other main effects or interactions were significant (all p > 0.1). Thus, MOM and AT trainings led to higher scores on the cooperativeness scale at Session 2 than at Session 1.
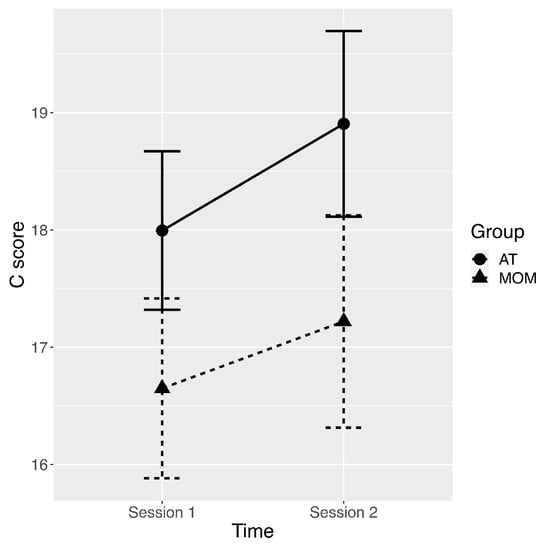
Figure 1.
Plot of average scores in Cooperativeness with error bars representing standard errors of the mean for pre-training assessment (Session 1) and post-training assessment (Session 2), and for AT (autogenic training) and MOM (mindfulness-oriented meditation) groups.
3.3. Changes in Strengths and Difficulties Questionnaire
A Shapiro–Wilk’s test showed that at Session 1, the SDQ-A scores of the BEH, HYP, PRO scales in the MOM group, as well as the PEE scores in the AT group, were not normally distributed (all p < 0.05). Furthermore, at Session 2, the SDQ-A scores of the EMO scale were not normally distributed for the AT group (p < 0.05).
On the basis of five 2 (Session: Session 1 and Session 2) × 2 (Group: MOM and AT) ANOVAs using robust M-estimators and 2000 bootstraps carried out on each SDQ-A scale score (EMO, BEH, HYP, PRE, PRO), there was a significant main effect of Session for the EMO scale (Session 1 > Session 2; ψ = 0.8, p = 0.002, see Table 1 and Figure 2). No other main effects or interactions reached the significance threshold (all p > 0.06). Thus, after MOM and AT trainings, participants showed lower scores on the emotional symptoms scale.
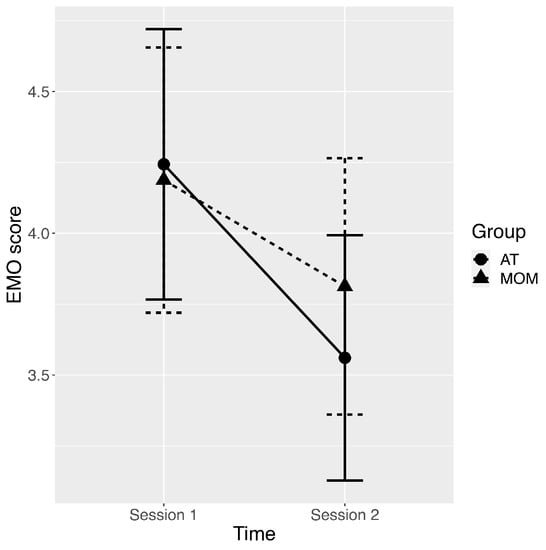
Figure 2.
Plot of average scores in Emotional symptoms with error bars representing standard errors of the mean for pre-training assessment (Session 1) and post-training assessment (Session 2), and for AT (autogenic training) and MOM (mindfulness-oriented meditation) groups.
3.4. Correlations
With regard to correlations between the indexes of Session 2 minus Session 1 changes in cooperativeness (C) and emotional symptoms (EMO), we obtained a significant negative correlation between changes in C and changes in EMO (Rho = −0.319, p = 0.008). The more participants increased in cooperativeness after the training the greater decrease they showed in emotional symptoms.
4. Discussion
The aim of this study was to investigate the effect of two 8-week mind-body interventions, namely MOM and AT, on adolescents’ character dimensions, emotional and behavioral difficulties. This was done by asking a sample of healthy late adolescents—recruited in two Italian five-year high-schools—to self-report their character traits and psychosocial adjustment (TCI and SDQ-A), before and after the trainings. Globally after both training programs, we found an increased level of cooperativeness, involving the acceptance of others, compassion and forgiveness. Alongside these changes, after the trainings, both groups showed decreased emotional symptoms, such as often feeling unhappy and downhearted. Moreover, the change in cooperativeness was negatively correlated with reduction in emotional problems: the more participants increased in their cooperativeness the more they showed a decrease in emotional symptoms after training.
Our study sample had already been investigated, at the “baseline” Session 1, in a previous study [43] that shed light on the relationship between temperament and character dimensions and different aspects of well-being and psychosocial functioning in adolescents. This study found that self-directness had a widespread protective effect on emotional and behavioral problems and that immaturity of the character (a combination of low self-directedness and low cooperativeness) showed a marked association with low psychological well-being and poor psychosocial adjustment. In line with the findings of the study by Crescentini et al. [43], we found that maturation of the self in aspects related to empathy and kindness was associated with enhanced psychological wellbeing in terms of a reduction in emotional problems. Overall, these data indicate the importance of considering personality traits, and character maturity in particular, as being closely connected to psychological adjustment and emotional regulation in youth.
Mindfulness and relaxation-based interventions based on autogenic training produced similar beneficial outcomes despite the different aims and techniques on which they focused, i.e., mindful awareness and relaxation practices, respectively. Similar findings emerged also in some previous studies [59,60]. The MOM and AT courses we used shared some important features: attendees of both training programs were encouraged to control their attention, to maintain a non-judgmental and non-reactive attitude, and to focus on breath and other physical sensations; moreover, the adolescents involved took an active role in the training through their daily individual practice and received support by sharing their challenges and successes with instructors and peers during the group meetings. It is possible that these common features of the two mind-body interventions were some of the key ingredients that promoted self-regulation, emotional well-being and changes in cooperativeness [61,62].
In general, the present results are consistent with what has emerged in previous research; implementing mind-body programs in schools can be an effective method to enhance positive intra- and interpersonal changes [63,64,65], such as self-regulation, coping, resilience [66,67,68] and emotional well-being [69,70], empathy, compassion and greater connection with others [71,72]. An emerging field of study—social and emotional learning (SEL)—highlights the importance of improving socio-emotional functioning and psychosocial adjustment in students, including recognition and management of emotions, empathy, and maintenance of positive interpersonal relationships, in order to support and maintain adolescents’ well-being [73,74,75] and to create a more pleasant and favorable school setting [74]. Thus, our research findings offer support to the field of SEL, showing that mind-body interventions, such as MOM and AT, can have a positive impact on socioemotional outcomes. Moreover, these interventions offer a means of targeting a broad section of the young population at or before the peak emergence of critical conditions, because they can, in theory, be offered to all students [10,11].
Our findings also show the importance of continuing to assess personality traits and their relation to well-being and psychosocial functioning in adolescence [72]. More specifically, it would be interesting for future studies to further investigate the effects of mind-body interventions on cooperative orientation. Recent research [76] involving five studies across different forms of cooperation, in both distributive and integrative negotiation contexts, and experimentally induced mindfulness, found substantial evidence that mindfulness is an effective intervention for increasing cooperation. Yet, these, and our, results are initial evidence that should be further investigated especially in youth. A larger body of evidence is available about the effects of mindfulness and relaxation on emotion regulation. Mindfulness has been shown to be effective in its regulatory function of targeting low positive emotionality, poor mood regulation and negative self-concept, which are risk factors implicated in the onset, development, and maintenance of depressive symptoms [77]. Several models, for example Shapiro’s [78] and Hölzel’s [79,80], outline both cognitive and experiential processes that enable emotional regulation through mindfulness meditation. Cognitive processes, for example, are involved in purposeful focusing of attention and reappraisal that allow for a new way of understanding and observing the transitory nature of emotional experience. With respect to AT, the existing literature is mainly focused on this kind of practice as a first intervention in therapeutic settings for children and adolescence. For example, some previous studies demonstrated how AT can be a valid self-help technique for adjustment disorders in young people, by diminishing the effects of, and easing the adaptation to, stress, and helping with recovery [81,82]. Other studies showed the effectiveness of AT in reducing anxiety and stress disorders [37,83]. A recent study [84] focused on how AT could help youth to cope with the pandemic; it reported strong beneficial effects of this practice on adolescents’ physical, psychological and relational health, recommending the practice of AT to people who experience anxiety, are afraid of illness, or feel that they have to improve the quality of their relationships with others.
Notwithstanding these promising results, more studies are needed to clearly define the specific effects and processes of the action of autogenic and mindfulness training in young people. Deepening this line of research will help tailor more effective programs for specific age groups and conditions, e.g., evaluating which delivery aspects of mind-body programs, such as duration of training, level of expertise of teacher training, environmental aspects, home practice, etc., induce the largest effects. Training should also be specifically adapted for use with youth, by shortening practice periods, making language appropriate for youth, and selecting age-appropriate activities, but further research is required to identify the optimal age, content and length of programs. These further investigations could be helpful to increase our knowledge on how to implement mind-body interventions in school settings with the aim of improving or preserving adolescents’ psychosocial functioning and well-being, which is becoming more and more important considering the challenges our society is facing and will face in the future.
The present findings should be interpreted in the context of some limitations. First, the exclusive use of self-report measures can be susceptible to socially desirable responding and these are sometimes considered less reliable than more objective measures, such as observation, in detecting, for instance, externalizing behaviors [85,86]. Other studies have showed that behavioral problems can reliably be assessed using self-reports [87], but it is advisable in the future to use multiple informants (e.g., adolescents, parents and teachers) to assess externalizing behaviors and to include implicit measures of personality which are more difficult to control or fake (e.g., the Implicit Association Test [50]). Moreover, we relied on daily diaries for the estimation of participants’ home practice, which is a common method used in mindfulness intervention studies [88], despite leaving unclear the extent to which this kind of measure relates to participants’ actual individual practice. Another limitation is that our results refer to a sample of adolescents living in the north-east of Italy and may not be generalizable to the larger population. Additionally, we lacked a passive, or waiting-list control group, which could have been useful to collect more informative data on the specific effects of the MOM and AT training. More studies are thus needed that include active and structurally equivalent control conditions to test training effects on specific mental health outcomes and behavioral change mechanisms in adolescents.
5. Conclusions
The aim of the present research was to investigate the impact of different mind-body interventions, specifically MOM and AT, on a group of Italian adolescents, by detecting potential changes in character dimensions, emotional and behavioral difficulties. Both training programs were effective in increasing participants’ level of cooperativeness, and in decreasing their emotional symptoms. These findings support the importance of implementing mind-body programs in schools as a valid method to enhance positive intra- and interpersonal changes in students. To conclude, it is suggested that consideration of the outcomes of this research could inspire future studies to further investigate the effectiveness and the underlying mechanisms of mindfulness and relaxation practices in young people, with the aim of promoting their healthy and harmonious growth.
Author Contributions
C.C. and A.P. were involved in the realization of the training and data acquisition; S.F. and A.M. analyzed the data and prepared the table; S.F. and S.P. wrote the original draft of the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the local Institutional Review Board of the University of Udine (Ethical Application Ref: CGPER-2016-11-23-01).
Informed Consent Statement
Informed consent was obtained from all subjects, or from their parents in the case of underage volunteers, involved in the study.
Data Availability Statement
Data supporting the results are available from the corresponding author [SF], upon request.
Acknowledgments
We thank the schools and the municipality of Lignano Sabbiadoro and Latisana for their contribution and support to this project, and G. Lucilli (ISIS E. Mattei) for his assistance and help in coordinating the courses.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Paus, T.; Keshavan, M.; Giedd, J.N. Why do many psychiatric disorders emerge during adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lambert, S.F.; Copeland-Linder, N.; Ialongo, N.S. Longitudinal associations between community violence exposure and suicidality. J. Adolesc. Health 2008, 43, 380–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burke, C.A. Mindfulness-based approaches with children and adolescents: A preliminary review of current research in an emergent field. J. Child Fam. Stud. 2010, 19, 133–144. [Google Scholar] [CrossRef]
- Grant, K.E.; Compas, B.E.; Thurm, A.E.; McMahon, S.D.; Gipson, P.Y.; Campbell, A.J.; Krochock, K.; Westerholm, R.I. Stressors and child and adolescent psychopathology: Evidence of moderating and mediating effects. Clin. Psychol. Rev. 2006, 26, 257–283. [Google Scholar] [CrossRef] [PubMed]
- Neil, A.L.; Christensen, H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin. Psychol. Rev. 2009, 29, 208–215. [Google Scholar] [CrossRef] [PubMed]
- McGrath, A.P.; Holahan, A. Psychological interventions with children and adolescents: Evidence for their effectiveness in treating chronic pain. Semin. Pain Med. 2003, 1, 99–109. [Google Scholar] [CrossRef]
- Steinberg, L. Adolescent development and juvenile justice. Annu. Rev. Clin. Psychol. 2009, 5, 459–485. [Google Scholar] [CrossRef] [Green Version]
- Dray, J.; Bowman, J.; Campbell, E.; Freund, M.; Wolfenden, L.; Hodder, R.K.; Bailey, J. Systematic review of universal resilience-focused interventions targeting child and adolescent mental health in the school setting. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 813–824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organisation (n.d.). Child and Adolescent Mental and Brain Health. 2021. Available online: http://www.who.int/mental_health/maternal_child/child_adolescent/en/ (accessed on 20 November 2021).
- Calear, A.L.; Christensen, H. Systematic review of school-based prevention and early intervention programs for depression. J. Adolesc. 2010, 33, 429–438. [Google Scholar] [CrossRef]
- Nehmy, T.J.; Wade, T.D. Reducing the onset of negative affect in adolescents: Evaluation of a perfectionism program in a universal prevention setting. Behav. Res. Ther. 2015, 67, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.; Ensor, R. Individual differences in growth in executive function across the transition to school predict externalizing and internalizing behaviors and self-perceived academic success at 6 years of age. J. Exp. Child. Psychol. 2011, 108, 663–776. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.; Gauntlett-Gilbert, J. Mindfulness with children and adolescents: Effective clinical application. Clin. Child. Psychol. Psychiatry 2008, 13, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Bronson, M.B. Recognizing and supporting the development of self-regulation in young children. Young Child. 2000, 55, 32–37. [Google Scholar]
- Zeman, J.; Cassano, M.; Perry-Parrish, C.; Stegall, S. Emotion regulation in children and adolescents. J. Dev. Behav. Pediatr. 2006, 27, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Frick, P.J.; Morris, A.S. Temperament and developmental pathways to conduct problems. J. Clin. Child. Adolesc. Psychol. 2004, 33, 54–68. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Galla, B.M.; Duckworth, A.L. More than resisting temptation: Beneficial habits mediate the relationship between self-control and positive life outcomes. J. Pers. Soc. Psychol. 2015, 109, 508–525. [Google Scholar] [CrossRef]
- Moffitt, T.E.; Arseneault, L.; Belsky, D.; Dickson, N.; Hancox, R.J.; Harrington, H.; Houts, R.; Poulton, R.; Roberts, B.W.; Ross, S.; et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc. Natl. Acad. Sci. USA 2011, 108, 2693–2698. [Google Scholar] [CrossRef] [Green Version]
- Pandey, A.; Hale, D.; Das, S.; Goddings, A.L.; Blakemore, S.J.; Viner, R.M. Effectiveness of Universal Self-Regulation-Based Interventions in Children and Adolescents: A Systematic Review and Meta-analysis. JAMA Pediatr. 2018, 172, 566–575. [Google Scholar] [CrossRef] [Green Version]
- Kabat-Zinn, J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life; Hyperion: New York, NY, USA, 1994. [Google Scholar]
- Kabat-Zinn, J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 1982, 4, 33–47. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J.; Lipworth, L.; Burney, R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J. Behav. Med. 1985, 8, 163–190. [Google Scholar] [CrossRef] [PubMed]
- De Vibe, M.; Solhaug, I.; Tyssen, R.; Friborg, O.; Rosenvinge, J.H.; Sørlie, T.; Bjørndal, A. Mindfulness training for stress management: A randomised controlled study of medical and psychology students. BMC Med. Educ. 2013, 13, 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Segal, Z.V.; Williams, J.G.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse; Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Shapiro, S.L.; Brown, K.W.; Thoresen, C.; Plante, T.G. The moderation of Mindfulness-based stress reduction effects by trait mindfulness: Results from a randomized controlled trial. J. Clin. Psychol. 2011, 67, 267–277. [Google Scholar] [CrossRef] [PubMed]
- Krasner, M.S.; Epstein, R.M.; Beckman, H.; Suchman, A.L.; Chapman, B.; Mooney, C.J.; Quill, T.E. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009, 302, 1284–1293.19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olson, K.; Kemper, K.J. Factors associated with well-being and confidence in providing compassionate care. J. Evid.-Based Complementary Altern. Med. 2014, 19, 292–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, S.L.; Shapiro, D.E.; Schwartz, G.E. Stress management in medical education: A review of the literature. Acad. Med. 2000, 75, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Dobkin, P.L.; Hutchinson, T.A. Teaching mindfulness in medical school: Where are we now and where are we going? Med. Educ. 2013, 47, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Erogul, M.; Singer, G.; McIntyre, T.; Stefanov, D.G. Abridged mindfulness intervention to support wellness in first-year medical students. Teach. Learn. Med. 2014, 26, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Malpass, A.; Binnie, K.; Robson, L. Medical Students’ Experience of Mindfulness Training in the UK: Well-Being, Coping Reserve, and Professional Development. Educ Res. Int. 2019, 2019, 4021729. [Google Scholar] [CrossRef]
- Semple, R.J.; Droutman, V.; Reid, B.A. Mindfulness goes to school: Things learned (so far) from research and real-word experience. Psychol. Sch. 2017, 54, 29–52. [Google Scholar] [CrossRef] [Green Version]
- Johnson, C.; Burke, C.; Brinkman, S.; Wade, T. A randomized controlled evaluation of a secondary school mindfulness program for early adolescents: Do we have the recipe right yet? Behav. Res. Ther. 2017, 99, 37–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry-Parrish, C.; Copeland-Linder, N.; Webb, L.; Shields, A.H.; Sibinga, E.M. Improving self-regulation in adolescents: Current evidence for the role of mindfulness-based cognitive therapy. Adolesc. Health Med. Ther. 2016, 7, 101–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fortney, L.; Luchterhand, C.; Zakletskaia, L.; Zgierska, A.; Rakel, D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: A pilot study. Ann. Fam. Med. 2013, 11, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, G.M.; Pagnini, F.; Castelnuovo, G.; Molinari, E. Relaxation training for anxiety: A ten-years systematic review with meta-analysis. BMC Psychiatry 2008, 8, 41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Institutes of Health. Relaxation Techniques: What You Need to Know. National Center for Complementary and Integrative Health. 2021. Available online: https://www.nccih.nih.gov/health/relaxation-techniques-what-you-need-to-know. (accessed on 20 November 2021).
- Dunning, D.L.; Griffiths, K.; Kuyken, W.; Crane, C.; Foulkes, L.; Parker, J.; Dalgleish, T. Research Review: The effects of mindfulness-based interventions on cognition and mental health in children and adolescents—A meta-analysis of randomized controlled trials. J. Child. Psychol. Psychiatry 2019, 60, 244–258. [Google Scholar] [CrossRef] [Green Version]
- Goldbeck, L.; Schmid, K. Effectiveness of autogenic relaxation training on children and adolescents with behavioral and emotional problems. J. Am. Acad. Child. Adolesc. Psychiatry 2003, 42, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Shapiro, S.L.; Swanick, S.; Roesch, S.C.; Mills, P.J.; Bell, I.; Schwartz, G.E.R. A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Ann. Behav. Med. 2007, 33, 11–21. [Google Scholar] [CrossRef]
- Kuhlmann, S.M.; Huss, M.; Bürger, A.; Hammerle, F. Coping with stress in medical students: Results of a randomized controlled trial using a mindfulness-based stress prevention training (MediMind) in Germany. BMC Med. Educ. 2016, 16, 316. [Google Scholar] [CrossRef] [Green Version]
- Crescentini, C.; Garzitto, M.; Paschetto, A.; Brambilla, P.; Fabbro, F. Temperament and character effects on late adolescents’ well-being and emotional-behavioural difficulties. PeerJ 2018, 6, e4484. [Google Scholar] [CrossRef] [Green Version]
- Cloninger, C.R.; Svrakic, D.M.; Przybeck, T.R. A psychobiological model of temperament and character. Arch. Gen. Psychiatry 1993, 50, 975–990. [Google Scholar] [CrossRef] [PubMed]
- Cloninger, C.R. The Temperament and Character Inventory (TCI): A Guide to Its Development and Use; Centre for Psychobiology of Personality, Washington University: St Louis, MO, USA, 1994. [Google Scholar]
- Garcia, D.; Moradi, S. Adolescents’ Temperament and Character: A Longitudinal Study on Happiness. J. Happiness Stud. 2012, 13, 931–946. [Google Scholar] [CrossRef]
- Gillham, J.; Adams-Deutsch, Z.; Werner, J.; Reivich, K.; Coulter-Heindl, V.; Linkins, M.; Winder, B.; Peterson, C.; Park, N.; Abenavoli, R.; et al. Character strengths predict subjective well-being during adolescence. J. Posit. Psychol. 2011, 6, 31–44. [Google Scholar] [CrossRef]
- Bromley, E.; Johnson, J.G.; Cohen, P. Personality strengths in adolescence and decreased risk of developing mental health problems in early adulthood. Compr. Psychiatry 2006, 47, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Garcia, D. Two models of personality and well-being among adolescents. Personal. Individ. Differ. 2011, 50, 1208–1212. [Google Scholar] [CrossRef]
- Crescentini, C.; Urgesi, C.; Campanella, F.; Eleopra, R.; Fabbro, F. Effects of an 8-week meditation program on the implicit and explicit attitudes toward religious/spiritual self-representations. Conscious. Cogn. 2014, 30, 266–280. [Google Scholar] [CrossRef] [PubMed]
- Fabbro, F.; Crescentini, C. La meditazione orientata alla mindfulness (mom) nella ricerca psicologica. Ric. Psicol. 2017, 457–472. [Google Scholar] [CrossRef] [Green Version]
- Matiz, A.; Fabbro, F.; Crescentini, C. Single vs. Group Mindfulness Meditation: Effects on Personality, Religiousness/Spirituality, and Mindfulness Skills. Mindfulness 2018, 9, 1236–1244. [Google Scholar] [CrossRef]
- Schultz, J.H.; Luthe, W. Autogenic Training: A Psychophysiologic Approach to Psychotherapy; Grune & Stratton: New York, USA, 1959. [Google Scholar]
- Delvecchio, G.; Garzitto, M.; Fagnani, C.; Fornasari, L.; Stazi, M.A.; Picardi, A.; Ciappolino, V.; Fabbro, F.; Altamura, A.C.; Brambilla, P. Normative data and effects of age and gender on temperament and character dimensions across the lifespan in an Italian population: A cross-sectional validation study. J. Affect. Disord. 2016, 204, 83–91. [Google Scholar] [CrossRef]
- Svrakic, D.M.; Whitehead, C.; Przybeck, T.R.; Cloninger, C.R. Differential diagnosis of personality disorders by the seven-factor model of temperament and character. Arch. Gen. Psychiatry 1993, 50, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Publishing, Inc.: Washington, DC, USA, 1994. [Google Scholar]
- Hashim, H.A.; Hanafi Ahmad Yusof, H. The effects of progressive muscle relaxation and autogenic relaxation on young soccer players’ mood states. Asian J. Sports Med. 2011, 2, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Kemper, K.J.; Khirallah, M. Acute Effects of Online Mind-Body Skills Training on Resilience, Mindfulness, and Empathy. J. Evid.-Based Complementary Altern Med. 2015, 20, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Pepper, E.; Harvey, R.; Lin, I.M. Mindfulness training has elements common to other techniques. Biofeedback 2019, 47, 50–57. [Google Scholar] [CrossRef]
- Berry, D.R.; Cairo, A.H.; Goodman, R.J.; Quaglia, J.T.; Green, J.D.; Brown, K.W. Mindfulness increases prosocial responses toward ostracized strangers through empathic concern. J. Exp. Psychol. Gen. 2018, 147, 93–112. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, E.K.; Chin, B.; Greco, K.M.; Young, S.; Brown, K.W.; Wright, A.G.C.; Smyth, J.M.; Burkett, D.; Creswell, J.D. How mindfulness training promotes positive emotions: Dismantling acceptance skills training in two randomized controlled trials. J. Pers. Soc. Psychol. 2018, 115, 944–973. [Google Scholar] [CrossRef]
- Vago, D.R.; Silbersweig, D.A. Self-awareness, self-regulation, and self-transcendence (S-ART): A framework for understanding the neurobiological mechanisms of mindfulness. Front. Hum. Neurosci. 2012, 6, 296. [Google Scholar] [CrossRef] [Green Version]
- Pidgeon, A.M.; Ford, L.; Klaassen, F. Evaluating the effectiveness of enhancing resilience in human service professionals using a retreat-based Mindfulness with Metta Training Program: A randomised control trial. Psychol. Health Med. 2014, 19, 355–364. [Google Scholar] [CrossRef]
- Kuyken, W.; Weare, K.; Ukoumunne, O.C.; Vicary, R.; Motton, N.; Burnett, R.; Cullen, C.; Hennelly, S.; Huppert, F. Effectiveness of the Mindfulness in Schools Programme: Non-randomised controlled feasibility study. Br. J. Psychiatry 2013, 203, 126–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry-Parrish, C.; Copeland-Linder, N.; Webb, L.; Sibinga, E.M. Mindfulness-Based Approaches for Children and Youth. Curr. Probl. Pediatr. Adolesc. Health Care 2016, 46, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Raes, F.; Griffith, J.W.; Gucht, K.V.; Williams, J.M. School-Based Prevention and Reduction of Depression in Adolescents: A Cluster-Randomized Controlled Trial of a Mindfulness Group Program. Mindfulness 2014, 5, 477–486. [Google Scholar] [CrossRef]
- Condon, P.; Desbordes, G.; Miller, W.B.; De Steno, D. Meditation increases compassionate responses to suffering. Psychol. Sci. 2013, 24, 2125–2127. [Google Scholar] [CrossRef] [PubMed]
- Donald, J.N.; Sahdra, B.K.; Van Zanden, B.; Duineveld, J.J.; Atkins, P.W.B.; Marshall, S.L.; Ciarrochi, J. Does your mindfulness benefit others? A systematic review and meta-analysis of the link between mindfulness and prosocial behaviour. Br. J. Psychol. 2019, 110, 101–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Durlak, J.A.; Weissberg, R.P.; Dymnicki, A.B.; Taylor, R.D.; Schellinger, K.B. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child Dev. 2011, 82, 405–432. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.; Burke, C.; Brinkman, S.; Wade, T. Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behav. Res. Ther. 2016, 81, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Cloninger, C.R. Feeling good: The Science of Well-Being; Oxford University Press: Oxford, UK, 2008; p. 374. [Google Scholar]
- Greenberg, M.T.; Weissberg, R.P.; O’Brien, M.U.; Zins, J.E.; Fredericks, L.; Resnik, H.; Elias, M.J. Enhancing school-based prevention and youth development through coordinated social, emotional, and academic learning. Am. Psychol. 2003, 58, 466–474. [Google Scholar] [CrossRef]
- Sibinga, E.M.; Kemper, K.J. Complementary, holistic, and integrative medicine: Meditation practices for pediatric health. Pediatr. Rev. 2010, 31, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Masters-Waage, T.; Nai, J.; Reb, J.; Sim, S.; Narayanan, J.; Tan, N. Going far together by being here now: Mindfulness increases cooperation in negotiations. Organ. Behav. Hum. Decis. Processes 2021, 167, 189–205. [Google Scholar] [CrossRef]
- Lindsay, E.K.; Creswell, J.D. Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clin. Psychol. Rev. 2017, 51, 48–59. [Google Scholar] [CrossRef] [Green Version]
- Shapiro, S.L.; Carlson, L.E.; Astin, J.A.; Freedman, B. Mechanisms of mindfulness. J. Clin. Psychol. 2006, 62, 373–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hölzel, B.K.; Carmody, J.; Vangel, M.; Congleton, C.; Yerramsetti, S.M.; Gard, T.; Lazar, S.W. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011, 191, 36–43. [Google Scholar] [CrossRef] [Green Version]
- Hölzel, B.K.; Lazar, S.W.; Gard, T.; Schuman-Olivier, Z.; Vago, D.R.; Ott, U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action from a Conceptual and Neural Perspective. Perspect. Psychol. Sci. 2011, 6, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Jojić, B.R.; Leposavić, L.M. Autogenic training as a therapy for adjustment disorder in adolescents. Srp. Arh. Celok. Lek. 2005, 133, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Klott, O. Autogenic Training—A self-help technique for children with emotional and behavioural problems. Therapeutic Communities: Int. J. Ther. Communities 2013, 34, 152–158. [Google Scholar] [CrossRef]
- Kanji, N.; White, A.; Ernst, E. Autogenic training to reduce anxiety in nursing students: Randomized controlled trial. J. Adv. Nurs. 2006, 53, 729–735. [Google Scholar] [CrossRef] [PubMed]
- De Rivera, L.; Ozamiz-Etxebarria, N.; Dosil-Santamaría, M.; De Rivera-Monterrey, L. Autogenic Training Improves the Subjective Perception of Physical and Psychological Health and of Interpersonal Relational Abilities: An Electronic Field Survey During the COVID-19 Crisis in Spain. Front. Psychol. 2021, 12. [Google Scholar] [CrossRef]
- Hinshaw, S.P.; Han, S.S.; Erhardt, D.; Huber, A. Internalizing and externalizing behavior problems in preschool children: Correspondence among parent and teacher ratings and behavior observations. J. Clin. Child Psychol. 1992, 21, 115–122. [Google Scholar] [CrossRef]
- Perry-Parrish, C.; Waasdorp, T.E.; Bradshaw, C.P. Peer Nominations of Emotional Expressivity among Urban Children: Social and Psychological Correlates. Soc. Dev. 2012, 21, 88–108. [Google Scholar] [CrossRef] [Green Version]
- Bartels, M.; Van de Aa, N.; Van Beijsterveldt, C.E.; Middeldorp, C.M.; Boomsma, D.I. Adolescent self-report of emotional and behavioral problems: Interactions of genetic factors with sex and age. J. Can. Acad. Child. Adolesc. Psychiatry 2011, 20, 35–52. [Google Scholar]
- Parsons, C.E.; Crane, C.; Parsons, L.J.; Fjorback, L.O.; Kuyken, W. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav. Res. Ther. 2017, 95, 29–41. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).