Migraine and Neuroticism: A Scoping Review
Abstract
:1. Introduction
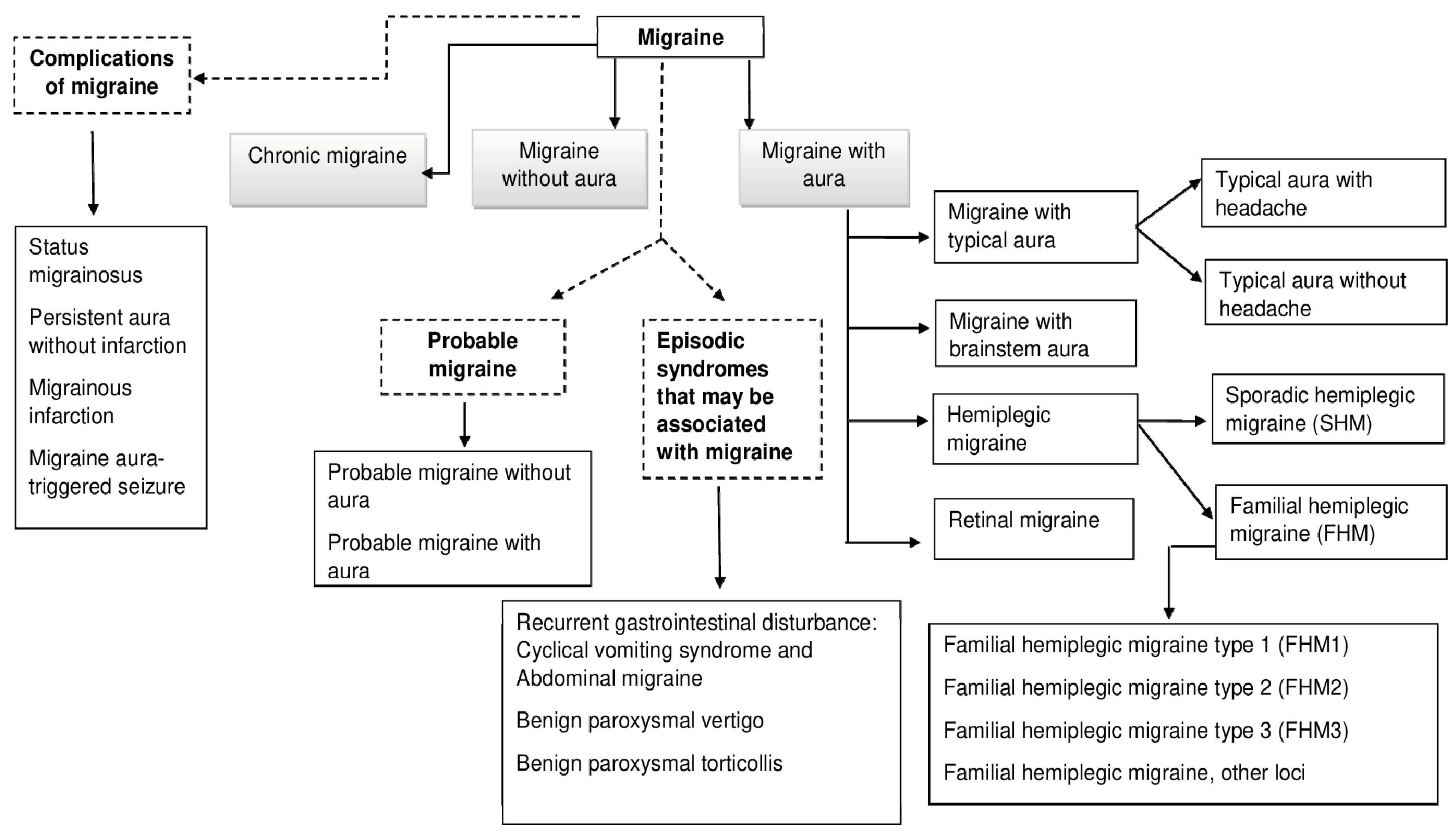
Migraine
2. Methodology
3. Results
3.1. Neuroticism Review’s Findings
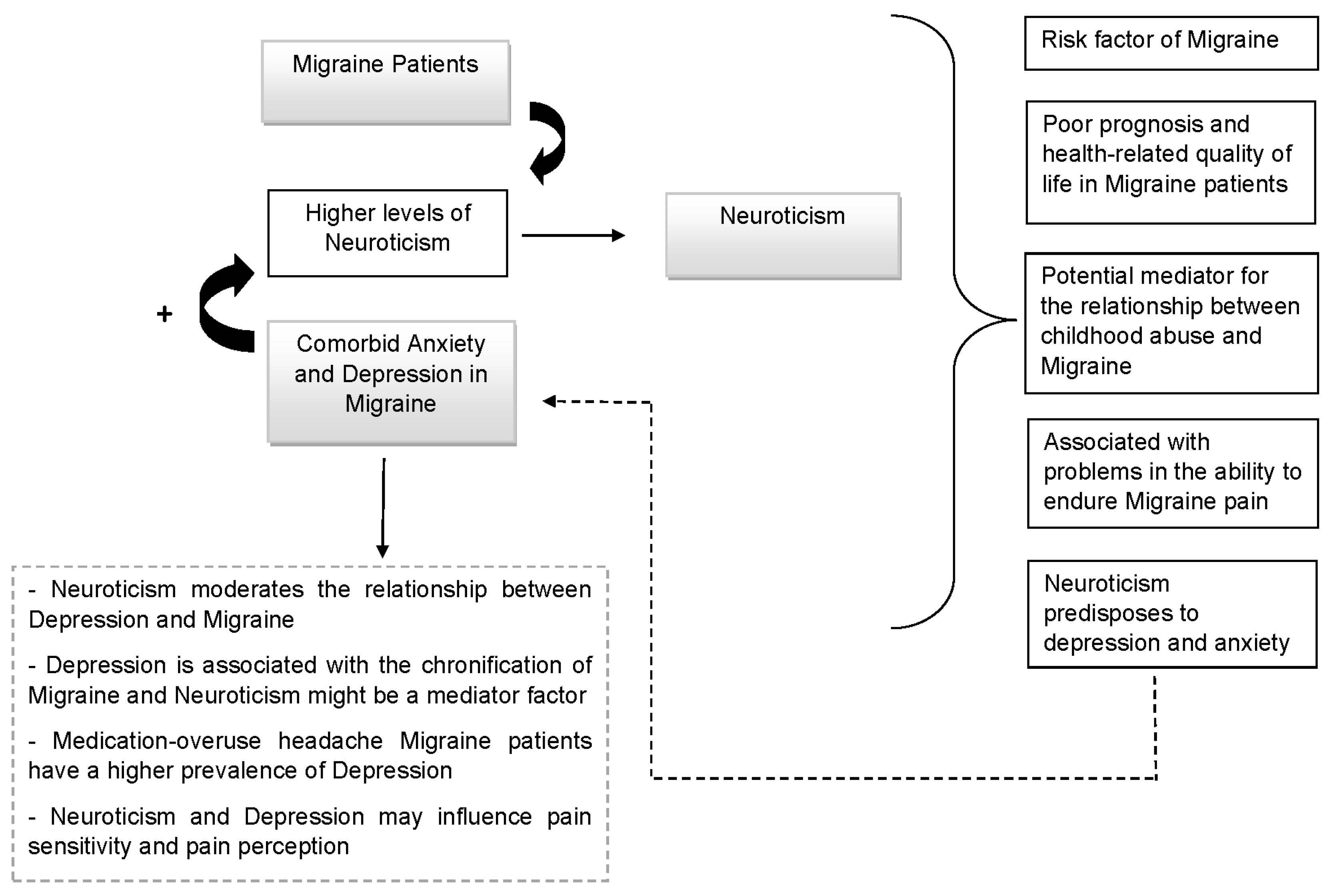
3.2. Migraine and Neuroticism Review’s Findings: Revealing An Important Link
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Deza, L. La Migraña [Migraine]. Acta Med. Per. 2010, 27, 129–136. [Google Scholar]
- Loreto, M. Migraña, un desafío para el médico no especialista [Migraine, a challenge for the general practitioner]. Rev. Med. Clin. Condes. 2019, 30, 407–413. [Google Scholar]
- Pascual, J. Cefalea y Migraña [Headache and Migraine]. Medicine 2019, 12, 4145–4153. [Google Scholar]
- Pérez Pérez, R.; Fajardo Pérez, M.; López Martínez, A.; Orlandi González, N.; Nolasco Cruzata, I. Migraña: Un reto para el médico general integral [Migraine: A challenge for the comprehensive general practitioner]. Rev. Cubana Med. Gen. Integral. 2003, 19, 1–6. [Google Scholar]
- Goadsby, P.J.; Evers, S. Headache Classification Committee of the International Headache Society [IHS]. The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar]
- Steiner, T.J.; Birbeck, G.L.; Jensen, R.; Katsarava, Z.; Martelletti, P.; Stovner, L.J. The Global Campaign, World Health Organization and Lifting The Burden: Collaboration in action. J. Headache Pain 2011, 12, 273–274. [Google Scholar] [CrossRef] [Green Version]
- Galvez-Sánchez, C.M.; Duschek, S.; Reyes Del Paso, G.A. Psychological impact of fibromyalgia: Current perspectives. Psychol. Res. Behav. Manag. 2019, 12, 117–127. [Google Scholar] [CrossRef] [Green Version]
- Davydov, D.M.; Galvez-Sánchez, C.M.; Montoro, C.I.; de Guevara, C.M.L.; Reyes Del Paso, G.A. Personalized behavior management as a replacement for medications for pain control and mood regulation. Sci. Rep. 2021, 11, 20297. [Google Scholar] [CrossRef]
- Montoro, C.I.; del Paso, G.A.R. Personality and fibromyalgia: Relationships with clinical, emotional, and functional variables. Pers. Individ. 2015, 85, 236–244. [Google Scholar] [CrossRef]
- Eysenck, H.J. Genetic and environmental contributions to individual differences: The three major dimensions of personality. J. Pers. 1990, 58, 245–261. [Google Scholar] [CrossRef]
- Lahey, B.B. Public health significance of neuroticism. Am. Psychol. 2009, 64, 24156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, M. The vulnerability status of neuroticism: Over-reporting or genuine complaints? Pers. Individ. Differ. 2003, 35, 877–887. [Google Scholar] [CrossRef]
- Moayedi, M.; Weissman-Fogel, I.; Crawley, A.P.; Goldberg, M.B.; Freeman, B.V.; Tenenbaum, H.C.; Davis, K.D. Contribution of chronic pain and neuroticism to abnormal forebrain gray matter in patients with temporomandibular disorder. Neuroimage 2011, 55, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Affleck, G.; Tennen, H.; Urrows, S.; Higgins, P. Neuroticism and the pain-mood relation in rheumatoid arthritis: Insights from a prospective daily study. J. Consult. Clin. Psychol. 1992, 60, 119–126. [Google Scholar] [CrossRef]
- Cao, M.; Zhang, S.; Wang, K.; Wang, Y.; Wang, W. Personality traits in migraine and tension-type headaches: A five-factor model study. Psychopathology 2002, 35, 254–258. [Google Scholar] [CrossRef]
- Mose, L.S.; Pedersen, S.S.; Jensen, R.H.; Gram, B. Personality traits in migraine and medication-overuse headache: A comparative study. Acta Neurol. Scand. 2019, 140, 116–122. [Google Scholar] [CrossRef]
- Mateos, V.; García-Moncó, J.C.; Gómez-Beldarrain, M.; Armengol-Bertolín, S.; Larios, C. Factores de personalidad, grado de discapacidad y abordaje terapéutico de los pacientes con migraña atendidos en primera consulta en neurología (estudio Psicomig) [Personality factors, degree of disability and therapeutic approach of patients with migraine seen in the first consultation in neurology (Psicomig study)]. Rev. Neurol. 2011, 52, 131–138. [Google Scholar]
- Merikangas, K.R.; Angst, J.; Isler, H. Migraine and psychopathology. Results of the Zurich cohort study of young adults. Arch. Gen. Psychiatry 1990, 47, 849–853. [Google Scholar] [CrossRef]
- Muñoz, I.; Domínguez, E.; Hernández, M.S.; Ruiz-Piñero, M.; Isidro, G.; Mayor-Toranzo, E.; Sotelo, E.M.; Molina, V.; Uribe, F.; Guerrero-Peral, Á.L. Rasgos de personalidad en migraña crónica: Estudio categorial y dimensional en una serie de 30 pacientes [Personality traits in patients with chronic migraine: A categorial and dimensional study in a series of 30 patients]. Rev. Neurol. 2015, 61, 49–56. [Google Scholar]
- Sevillano-García, M.D.; Manso-Calderón, R.; Cacabelos-Pérez, P. Comorbilidad en la migraña: Depresión, ansiedad, estrés e insomnio [Comorbidity in migraine: Depression, anxiety, stress and insomnia]. Rev. Neurol. 2007, 45, 400–405. [Google Scholar]
- Cassidy, E.M.; Tomkins, E.; Hardiman, O.; O’Keane, V. Factors associated with burden of primary headache in a specialty clinic. Headache 2003, 43, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, A.; Tiraferi, I.; Neri, L.; Sternieri, E. Clinical pharmacology of topiramate in migraine prevention. Expert Opin. Drug Metab. Toxicol. 2011, 7, 1169–1181. [Google Scholar] [CrossRef]
- Aurora, S.K.; Kulthia, A.; Barrodale, P.M. Mechanism of chronic migraine. Curr. Pain Headache Rep. 2011, 15, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Eikermann-Haerter, K.; Can, A.; Ayata, C. Pharmacological targeting of spreading depression in migraine. Expert Rev. Neurother. 2012, 12, 297–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathew, N.T. Pathophysiology of chronic migraine and mode of action of preventive medications. Headache 2011, 51, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Avnon, Y.; Nitzan, M.; Sprecher, E.; Rogowski, Z.; Yarnitsky, D. Different patterns of parasympathetic activation in uni-and bilateral migraineurs. Brain 2003, 126, 1660–1670. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.E.; Jäger, T.; Bäzner, H.; Hennerici, M. Changes in functional vasomotor reactivity in migraine with aura. Cephalalgia 2009, 29, 1156–1164. [Google Scholar] [CrossRef]
- Volcy, M. Pathophysiology of migraine. Acta Neurol. Colomb. 2013, 29, 44–52. [Google Scholar]
- Muller, M.; Marziniak, M. The linear behavior of the system middle cerebral artery flow velocity and blood pressure in patients with migraine. Lack of autonomic control? Stroke 2005, 36, 1886–1890. [Google Scholar] [CrossRef] [Green Version]
- Zaninovic, V. Migrañas: Fisiopatología y tratamiento. Colomb. Med. 2001, 32, 86–88. [Google Scholar]
- Sarchielli, P.; Granella, F.; Prudenzano, M.P.; Pini, L.A.; Guidetti, V.; Bono, G.; Pinessi, L.; Alessandri, M.; Antonaci, F.; Fanciullacci, M.; et al. Italian guidelines for primary headaches: 2012 revised version. J. Headache Pain 2012, 13, S31–S70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Visens, L.S. Actualización en la prevención y tratamiento de la migraña [Update on the prevention and treatment of migraine]. Medicina 2014, 74, 147–157. [Google Scholar] [PubMed]
- Geppetti, P.; De Cesaris, F.; Nicoletti, P.; Benemei, S. Chronic headaches and medication overuse. Intern. Emerg. Med. 2010, 5, S7–S11. [Google Scholar] [CrossRef] [PubMed]
- Widiger, T.A.; Livesley, W.J.; Clark, L.A. An integrative dimensional classification of personality disorder. Psychol. Assess 2009, 21, 243–255. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.; Snell, W.E., Jr. Goldberg’s bipolar measure of the Big-Five personality dimensions: Reliability and validity. Eur. J. Pers. 1996, 10, 283–299. [Google Scholar] [CrossRef]
- McCrae, R. Creativity, Divergent Thinking, and Openness to Experience. J. Pers. Soc. Psychol. 1987, 52, 1258–1265. [Google Scholar] [CrossRef]
- Eysenck, H.J. Personality: Biological foundations. In The Neuropsychology of Individual Differences; Vernon, P.A., Ed.; Academic Press: Cambridge, MA, USA, 1994; pp. 151–207. [Google Scholar]
- Bear, M.F.; Connors, B.W.; Paradiso, M.A. Neuroscience: Exploring the Brain; Wolter Kluwer: Philadelphia, PA, USA, 2016. [Google Scholar]
- Snell, R.S. Clinical Neuroanatomy, 7th ed.; Wolter Kluwer: Philadelphia, PA, USA, 2010. [Google Scholar]
- Kadimpati, S.; Zale, E.L.; Hooten, M.W.; Ditre, J.W.; Warner, D.O. Associations between Neuroticism and Depression in Relation to Catastrophizing and Pain-Related Anxiety in Chronic Pain Patients. PLoS ONE 2015, 10, e0126351. [Google Scholar]
- Wu, D.; Yin, H.; Xu, S.; Zhao, Y. Risk factors for posttraumatic stress reactions among Chinese students following exposure to a snowstorm disaster. BMC Public Health 2011, 12, 1196. [Google Scholar] [CrossRef] [Green Version]
- Engelhard, I.M.; van den Hout, M.A.; Schouten, E.G. Neuroticism and low educational level predict the risk of posttraumatic stress disorder in women after miscarriage or stillbirth. Gen. Hosp. Psychiatry 2006, 28, 414–417. [Google Scholar] [CrossRef]
- Kuljic, B.; Miljanovic, B.; Svicevic, R. Posttraumatic stress disorder in Bosnian war veterans: Analysis of stress events and risk factors. Vojnosanit. Pregl. 2004, 61, 283–289. [Google Scholar] [CrossRef]
- Soler-Ferrería, F.B.; Sánchez Meca, J.; López Navarro, J.M.; Navarro Mateu, F. Neuroticismo y trastorno por estrés postraumático: Un estudio metaanalítico [Neuroticism and post-traumatic stress disorder: A meta-analytic study]. Rev. Esp. Salud. Pública 2014, 88, 17–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asghari, A.; Nicholas, M.K. Personality and Pain-Related Beliefs/Coping Strategies: A Prospective Study. Clin. J. Pain 2006, 22, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Martínez, M.P.; Sánchez, A.I.; Miró, E.; Medina, A.; Lami, M.J. The relationship between the fear-avoidance model of pain and personality traits in fibromyalgia patients. J. Clin. Psychol. Med. Settings 2011, 18, 380–391. [Google Scholar] [CrossRef] [PubMed]
- Ramírez Maestre, C.; Esteve Zarazaga, R.; López Martínez, A.E. Neuroticismo, afrontamiento y dolor crónico [Neuroticism, coping and chronic pain]. An. Psicol. 2001, 17, 129–137. [Google Scholar]
- Bolger, N. Coping as a personality process: A prospective study. J. Pers. Soc. Psychol. 1990, 59, 525–537. [Google Scholar] [CrossRef]
- Gracely, R.H.; Geisser, M.E.; Giesecke, T.; Grant, M.A.; Petzke, F.; Williams, D.A.; Clauw, D.J. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain 2004, 127, 835–843. [Google Scholar] [CrossRef] [Green Version]
- Galvez-Sánchez, C.M.; Montoro, C.I.; Duschek, S.; Del Paso, G.A.R. Pain catastrophizing mediates the negative influence of pain and trait-anxiety on health-related quality of life in fibromyalgia. Qual. Life Res. 2020, 29, 1871–1881. [Google Scholar] [CrossRef]
- Mathur, V.A.; Moayedi, M.; Keaser, M.L.; Khan, S.A.; Hubbard, C.S.; Goyal, M.; Seminowicz, D.A. High Frequency Migraine Is Associated with Lower Acute Pain Sensitivity and Abnormal Insula Activity Related to Migraine Pain Intensity, Attack Frequency, and Pain Catastrophizing. Front. Hum. Neurosci. 2016, 10, 489. [Google Scholar] [CrossRef]
- Barral, E.; Buonanotte, F. Catastrofización ante el dolor y abuso de analgésicos en pacientes con migraña crónica [Pain catastrophizing and medication overuse in patients with chronic migraine]. Rev. Neurol. 2020, 70, 282–286. [Google Scholar]
- Farris, S.G.; Thomas, J.G.; Kibbey, M.M.; Pavlovic, J.M.; Steffen, K.J.; Bond, D.S. Treatment effects on pain catastrophizing and cutaneous allodynia symptoms in women with migraine and overweight/obesity. Health Psychol. 2020, 39, 927–933. [Google Scholar] [CrossRef]
- Vallejo-Sánchez, B.; Pérez-García, A.M. Contribución del Neuroticismo, Rasgos Patológicos de Personalidad y Afrontamiento en la Predicción de la Evolución Clínica: Estudio de Seguimiento a los 5 Años de una Muestra de Pacientes con Trastorno Adaptativo [Contribution of neuroticism, pathological personality traits comorbidity, and coping to the prediction of clinical evolution: A five-year follow-up study of a sample of patients with adjustment disorder]. Clin. Salud. 2018, 29, 58–62. [Google Scholar]
- Kristoffersen, E.S.; Aaseth, K.; Grande, R.B.; Lundqvist, C.; Russell, M.B. Psychological distress, neuroticism and disability associated with secondary chronic headache in the general population-the Akershus study of chronic headache. J. Headache Pain 2018, 19, 62. [Google Scholar] [CrossRef] [PubMed]
- Mccrae, R.R.; John, O.P. An introduction to the five-factor model and its applications. J. Pers. 1992, 60, 175–215. [Google Scholar] [CrossRef] [PubMed]
- Boz, C.; Velioglu, S.; Ozmenoglu, M.; Sayar, K.; Alioglu, Z.; Yalman, B.; Topbas, M. Temperament and character profiles of patients with tension-type headache and migraine. Psychiatry Clin. Neurosci. 2004, 58, 536–543. [Google Scholar] [CrossRef] [PubMed]
- Brandt, J.; Celentano, D.; Stewart, W.; Linet, M.; Folstein, M.F. Personality and emotional disorder in a community sample of migraine headache sufferers. Am. J. Psychiatry 1990, 147, 303–308. [Google Scholar]
- Breslau, N.; Lipton, R.B.; Stewart, W.F.; Schultz, L.R.; Welch, K.M. Comorbidity of migraine and depression: Investigating potential etiology and prognosis. Neurology 2003, 60, 1308–1312. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, B.K. Migraine and tension-type headache in a general population: Psychosocial factors. Int. J. Epidemiol. 1992, 21, 1138–1143. [Google Scholar] [CrossRef]
- Sances, G.; Galli, F.; Anastasi, S.; Ghiotto, N.; De Giorgio, G.; Guidetti, V.; Nappi, G. Medication-overuse headache and personality: A controlled study by means of the MMPI-2. Headache 2010, 50, 198–209. [Google Scholar] [CrossRef] [PubMed]
- Sala, I.; Roig, C.; Amador-Campos, J.A.; Garcia-Sanchez, C.; Rodriguez, A.; Diaz, C.; Gich, I. Síntomas psicopatológicos en pacientes afectos de cefalea crónica con o sin fibromialgia [Psychopathological symptoms in patients with chronic headache with or without fibromyalgia]. Rev. Neurol. 2009, 49, 281–287. [Google Scholar]
- Huber, D.; Henrich, G. Personality traits and stress sensitivity in migraine patients. Behav. Med. 2003, 29, 4–13. [Google Scholar] [CrossRef]
- Persson, B. Growth environment and personality in adult migraineurs and their migraine-free siblings. Headache 1997, 37, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Treglown, L.; Green, A.; Chapman, B.P.; Κornilaki, E.N.; Furnham, A. Childhood onset of migraine, gender, parental social class, and trait neuroticism as predictors of the prevalence of migraine in adulthood. J. Psychosom. Res. 2016, 88, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Ligthart, L.; Boomsma, D.I. Causes of comorbidity: Pleiotropy or causality? Shared genetic and environmental influences on migraine and neuroticism. Twin Res. Hum. Genet. 2012, 15, 158–165. [Google Scholar] [CrossRef]
- Costa, P.T., Jr.; McCrae, R.R. Domains and facets: Hierarchical personality assessment using the revised NEO personality inventory. J. Pers. Assess 1995, 64, 21–50. [Google Scholar] [CrossRef] [Green Version]
- Lampl, C.; Thomas, H.; Tassorelli, C.; Katsarava, Z.; Laínez, J.M.; Lantéri-Minet, M.; Rastenyte, D.; Ruiz de la Torre, E.; Stovner, L.J.; Andrée, C.; et al. Headache, depression and anxiety: Associations in the Eurolight project. J. Headache Pain 2016, 17, 59. [Google Scholar] [CrossRef] [Green Version]
- Silberstein, S.D.; Lipton, R.B.; Breslau, N. Migraine: Association with personality characteristics and psychopathology. Cephalalgia 1995, 15, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Svedberg, P.; Bardage, C.; Sandin, S.; Pedersen, N.L. A prospective study of health, life-style and psychosocial predictors of self-rated health. Eur. J. Epidemiol. 2006, 21, 767–776. [Google Scholar] [CrossRef]
- Mongini, F.; Ibertis, F.; Barbalonga, E.; Raviola, F. MMPI-2 profiles in chronic daily headache and their relationship to anxiety levels and accompanying symptoms. Headache 2000, 40, 466–472. [Google Scholar] [CrossRef]
- Merikangas, K.R.; Stevens, D.E.; Angst, J. Headache and personality: Results of a community sample of young adults. J. Psychiatr. Res. 1993, 27, 187–196. [Google Scholar] [CrossRef]
- Ashina, S.; Bendtsen, L.; Buse, D.C.; Lyngberg, A.C.; Lipton, R.B.; Jensen, R. Neuroticism, depression and pain perception in migraine and tension-type headache. Acta Neurol. Scand. 2017, 136, 470–476. [Google Scholar] [CrossRef]
- Shiomi, K. Relations of pain threshold and pain tolerance in cold water with scores on Maudsley Personality Inventory and Manifest Anxiety Scale. Percept. Mot. Skills 1978, 47, 1155–1158. [Google Scholar] [CrossRef] [PubMed]
- Goubert, L.; Crombez, G.; Van, D.S. The role of neuroticism, pain catastrophizing and pain-related fear in vigilance to pain: A structural equations approach. Pain 2004, 107, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.R.; Stride, E. The varying response to pain in psychiatric disorders: A study in abnormal psychology. Br. J. Med. Psychol. 1954, 27, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Stengel, E.; Oldham, A.J.; Ehrenberg, A.S. Reactions to pain in various abnormal mental states. J. Ment. Sci. 1955, 101, 52–69. [Google Scholar] [CrossRef] [PubMed]
- Bond, M.R. The relation of pain to the Eysenck personality inventory, Cornell medical index and Whiteley index of hypochondriasis. Br. J. Psychiatry 1971, 119, 671–678. [Google Scholar] [CrossRef]
- Lipton, R.B.; Bigal, M.E.; Ashina, S.; Burstein, R.; Silberstein, S.; Reed, M.L.; Serrano, D.; Stewart, W.F.; American Migraine Prevalence Prevention Advisory Group. Cutaneous allodynia in the migraine population. Ann. Neurol. 2008, 63, 148–158. [Google Scholar] [CrossRef]
- Ashina, S.; Serrano, D.; Lipton, R.B.; Maizels, M.; Manack, A.N.; Turkel, C.C.; Reed, M.L.; Buse, D.C. Depression and risk of transformation of episodic to chronic migraine. J. Headache Pain 2012, 13, 615–624. [Google Scholar] [CrossRef] [Green Version]
- Sair, A.; Sair, Y.B.; Akyol, A.; Sevincok, L. Affective temperaments and lifetime major depression in female migraine patients. Women Health 2020, 60, 1218–1228. [Google Scholar] [CrossRef]
- Breslau, N.; Andreski, P. Migraine, personality, and psychiatric comorbidity. Headache 1995, 35, 382–386. [Google Scholar] [CrossRef] [Green Version]
- Furnham, A. Personality and Intelligence at Work; Routledge: London, UK, 2008. [Google Scholar]
- Cheng, H.; Furnham, A. Personality, self-esteem, and demographic predictions of happiness and depression. Pers. Individ. Differ. 2003, 34, 921–942. [Google Scholar] [CrossRef]
- Beck, A.T. Cognitive Therapy and the Emotional Disorders; Penguin Books: New York, NY, USA, 1979. [Google Scholar]
- Chan, F.; Cardoso, E.D.S.; Chronister, J.A. Understanding Psychosocial Adjustment to Chronic Illness and Disability: A Handbook for Evidence-Based Practitioners in Rehabilitation; Springer Publishing Company: Berlin/Heidelberg, Germany, 2009. [Google Scholar]
- Karmakar, M.; Elhai, J.D.; Amialchuk, A.A.; Tietjen, G.E. Do Personality Traits Mediate the Relationship Between Childhood Abuse and Migraine? An Exploration of the Relationships in Young Adults Using the Add Health Dataset. Headache 2018, 58, 243–259. [Google Scholar] [CrossRef] [PubMed]
- Li, X.B.; Wang, Z.M.; Hou, Y.Z.; Wang, Y.; Liu, J.T.; Wang, C.Y. Effects of childhood trauma on Headache 15 personality in a sample of Chinese adolescents. Child Abuse Negl. 2014, 38, 788–796. [Google Scholar] [CrossRef]
- Spinhoven, P.; Elzinga, B.M.; Van Hemert, A.M.; de Rooij, M.; Penninx, B.W. Childhood maltreatment, maladaptive personality types and level and course of psychological distress: A six-year longitudinal study. J. Affect Disord. 2016, 191, 100–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gamble, S.A.; Talbot, N.L.; Duberstein, P.R.; Conner, K.R.; Franus, N.; Beckman, A.M.; Conwell, Y. Childhood sexual abuse and depressive symptom severity: The role of neuroticism. J. Nerv. Ment. Dis. 2006, 194, 382–385. [Google Scholar] [CrossRef] [PubMed]
- Schwandt, M.L.; Heilig, M.; Hommer, D.W.; George, D.T.; Ramchandani, V.A. Childhood trauma exposure and alcohol dependence severity in adulthood: Mediation by emotional abuse severity and neuroticism. Alcohol Clin. Exp. Res. 2013, 37, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, Y.; Okamoto, Y.; Takagaki, K.; Okada, G.; Toki, S.; Inoue, T.; Tanabe, H.; Kobayakawa, M.; Yamawaki, S. Direct and indirect influences of childhood abuse on depression symptoms in patients with major depressive disorder. BMC Psychiatry 2015, 15, 244. [Google Scholar] [CrossRef] [Green Version]
- Hovens, J.G.F.M.; Giltay, E.J.; van Hemert, A.M.; Penninx, B.W.J.H. Childhood maltreatment and the course of depressive and anxiety disorders: The contribution of personality characteristics. Depress. Anxiety 2016, 33, 27–34. [Google Scholar] [CrossRef]
- Martin-Blanco, A.; Soler, J.; Villalta, L.; Feliu-Soler, A.; Elices, M.; Pérez, V.; Arranz, M.J.; Ferraz, L.; Alvarez, E.; Pascual, J.C. Exploring the interaction between childhood maltreatment and temperamental traits on the severity of borderline personality disorder. Compr. Psychiat. 2014, 55, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Vinkers, C.H.; Joels, M.; Milaneschi, Y.; Kahn, R.S.; Penninx, B.W.J.H.; Boks, M.P.M. Stress exposure across the life span cumulatively increases depression risk and is moderated by neuroticism. Depress. Anxiety 2014, 31, 737–745. [Google Scholar] [CrossRef]
- Brents, L.K.; Tripathi, S.P.; Young, J.; James, G.A.; Kilts, C.D. The role of childhood maltreatment in the altered trait and global expression of personality in cocaine addiction. J. Psychiatr. Res. 2015, 64, 23–31. [Google Scholar] [CrossRef] [Green Version]
- Eisenberger, N.I. The neural bases of social pain: Evidence for shared representations with physical pain. Psychosom. Med. 2012, 74, 126–135. [Google Scholar] [CrossRef] [Green Version]
- Gelaye, B.; Do, N.; Avila, S.; Carlos Velez, J.; Zhong, Q.Y.; Sanchez, S.E.; Peterlin, B.L.; Williams, M.A. Childhood abuse, intimate partner violence and risk of migraine among pregnant women: An epidemiologic study. Headache 2016, 56, 976–986. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tietjen, G.E.; Brandes, J.L.; Peterlin, B.L.; Eloff, A.; Dafer, R.M.; Stein, M.R.; Drexler, E.; Martin, V.T.; Hutchinson, S.; Aurora, S.K.; et al. Childhood maltreatment and migraine [part II]. Emotional abuse as a risk factor for headache chronification. Headache 2010, 50, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Juang, K.D.; Wang, S.J.; Fuh, J.L.; Lu, S.R.; Chen, Y.S. Association between adolescent chronic daily headache and childhood adversity: A community-based study. Cephalalgia Int. J. Headache 2004, 24, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Fuller-Thomson, E.; Baker, T.M.; Brennenstuhl, S. Investigating the association between childhood physical abuse and migraine. Headache 2010, 50, 749–760. [Google Scholar] [CrossRef] [PubMed]
- Fuh, J.L.; Wang, S.J.; Juang, K.D.; Lu, S.R.; Liao, Y.C.; Chen, S.P. Relationship between childhood physical maltreatment and migraine in adolescents. Headache 2010, 50, 761–768. [Google Scholar] [CrossRef]
- Tietjen, G.E.; Buse, D.C.; Fanning, K.M.; Serrano, D.; Reed, M.L.; Lipton, R.B. Recalled maltreatment, migraine, and tension-type hedache: Results of the AMPP study. Neurology 2015, 84, 132–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brennenstuhl, S.; Fuller-Thomson, E. The painful legacy of childhood violence: Migraine headaches among adult survivors of adverse childhood experiences. Headache 2015, 55, 973–983. [Google Scholar] [CrossRef]
- Tietjen, G.E.; Karmakar, M.; Amialchuk, A.A. Emotional abuse history and migraine among young adults: A retrospective cross-sectional analysis of the add health dataset. Headache 2017, 57, 45–59. [Google Scholar] [CrossRef]
- Mattsson, P.; Ekselius, L. Migraine, major depression, panic disorder, and personality traits in women aged 40–74 years: A population-based study. Cephalalgia 2002, 22, 543–551. [Google Scholar] [CrossRef]
- Masaro, E.J. (Ed.) Ageing: Current concepts. In Handbook of Physiology, Section 11: Ageing; Oxford University Press: New York, NY, USA, 1993; pp. 3–33. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galvez-Sánchez, C.M.; Montoro Aguilar, C.I. Migraine and Neuroticism: A Scoping Review. Behav. Sci. 2022, 12, 30. https://doi.org/10.3390/bs12020030
Galvez-Sánchez CM, Montoro Aguilar CI. Migraine and Neuroticism: A Scoping Review. Behavioral Sciences. 2022; 12(2):30. https://doi.org/10.3390/bs12020030
Chicago/Turabian StyleGalvez-Sánchez, Carmen M., and Casandra I. Montoro Aguilar. 2022. "Migraine and Neuroticism: A Scoping Review" Behavioral Sciences 12, no. 2: 30. https://doi.org/10.3390/bs12020030
APA StyleGalvez-Sánchez, C. M., & Montoro Aguilar, C. I. (2022). Migraine and Neuroticism: A Scoping Review. Behavioral Sciences, 12(2), 30. https://doi.org/10.3390/bs12020030






