Experiencing Pregnancy during the COVID-19 Lockdown in Poland: A Cross-Sectional Study of the Mediating Effect of Resiliency on Prenatal Depression Symptoms
Abstract
1. Introduction
- Is the level of prenatal depressive symptoms, pandemic-related pregnancy stress, and traumatic childbirth perception different among women with a low resilience when they are compared to those with high resilience?
- Were traumatic childbirth perceptions and pandemic-related pregnancy stresses related to depression symptoms among pregnant women during the COVID-19 lockdown?
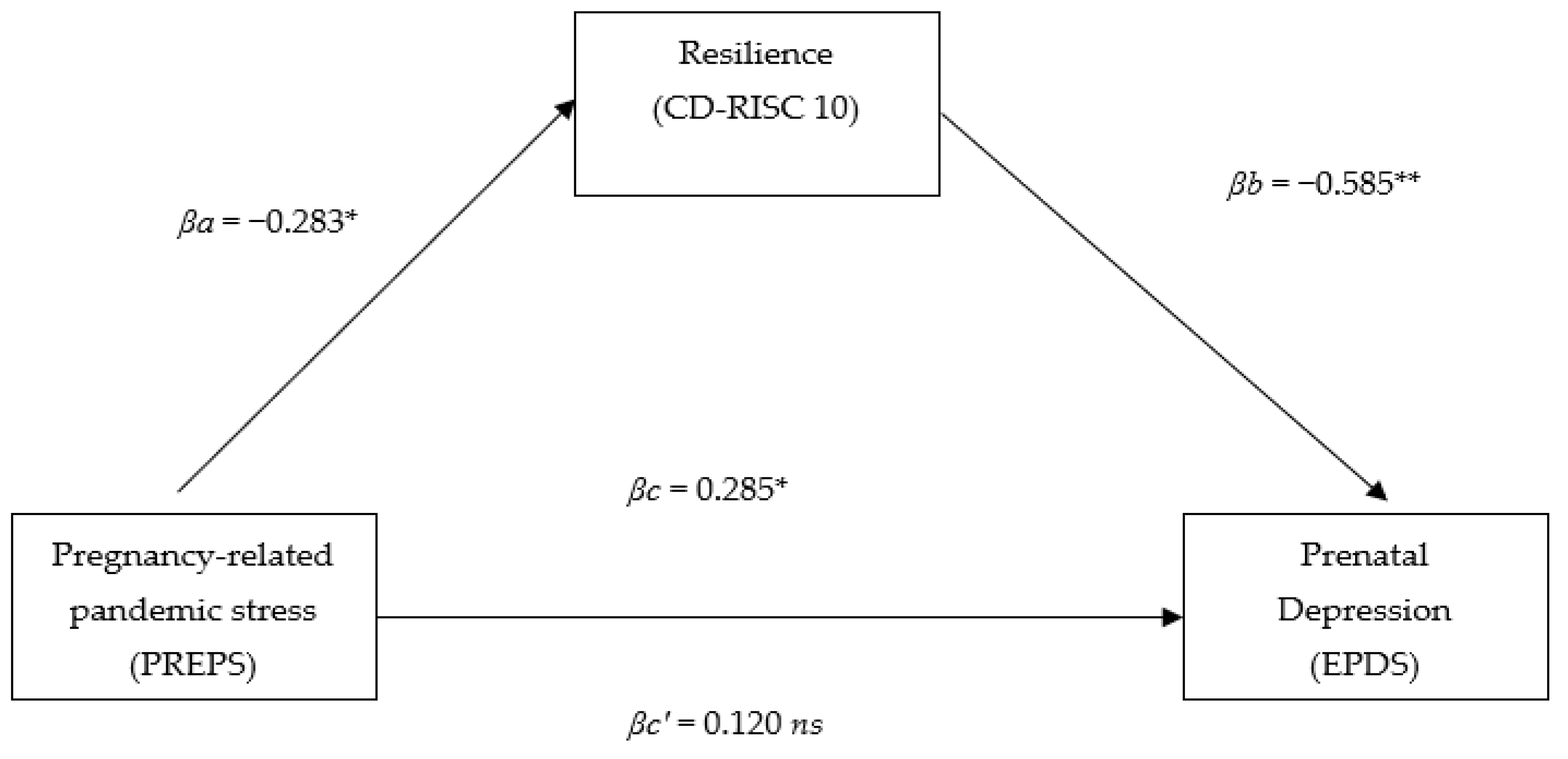
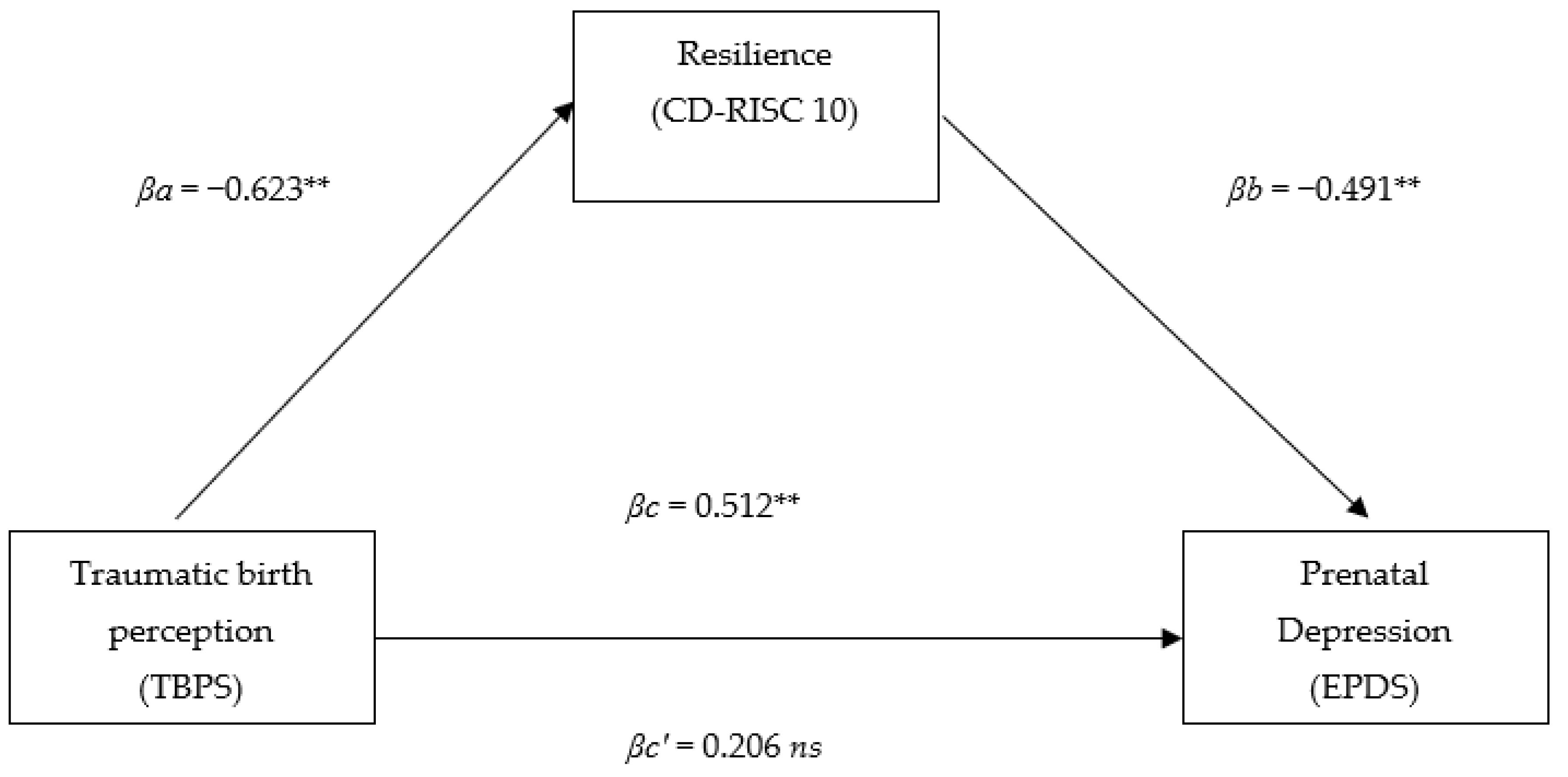
- Does resilience act as a mediator in the relationship between a traumatic childbirth perception and prenatal depressive symptoms, and between pandemic-related pregnancy stress and prenatal depressive symptoms?
2. Materials and Methods
2.1. Study Design
2.2. Ethical Consideration
2.3. Inclusion/Exclusion Criteria
2.4. Procedure and Data Collection
2.5. Measures
2.6. Data Analysis
3. Results
3.1. Study Sample Characteristic
3.2. Resilience Level in the Study Sample
3.3. Prenatal Depression Symptoms in a Study Sample
3.4. Pandemic-Related Stress in a Study Sample
3.5. Traumatic Childbirth Perception in a Study Sample
3.6. Relationship between the Traumatic Childbirth Perception, Pandemic-Related Pregnancy Stress, and Prenatal Depression Symptoms
3.7. Resilience as a Mediator between Pandemic-Related Stress/Traumatic Childbirth Perception and Prenatal Depression Symptoms
4. Discussion
4.1. Prenatal Depression
4.2. Traumatic Childbirth Perception
4.3. Pandemic-Related Pregnancy Stress
4.4. Relationship between the Resilience and Prenatal Depression Symptoms, Traumatic Childbirth Perception, and Pandemic-Related Pregnancy Stress
4.5. Strenghts and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tataj-Puzyna, U.; Węgrzynowska, M.; Ryś, M.; Sys, D.; Bączek, G.; Baranowska, B. “This pregnancy makes sense”: Experiences of women who have decided to continue pregnancy after lethal fetal diagnosis. Death Stud. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Young, C.; Ayers, S. Risk and Resilience in Pregnancy and Birth. In Multisystemic Resilience (57-C3.P145); Ungar, M., Ed.; Oxford University Press: New York, NY, USA, 2021. [Google Scholar] [CrossRef]
- Bohren, M.A.; Hofmeyr, G.J.; Sakala, C.; Fukuzawa, R.K.; Cuthbert, A. Continuous support for women during childbirth. Cochrane Database Syst. Rev. 2017, 7, CD003766. [Google Scholar] [CrossRef] [PubMed]
- Türkmen, H.; Yalniz Dİlcen, H.; Özçoban, F.A. Traumatic childbirth perception during pregnancy and the postpartum period and its postnatal mental health outcomes: A prospective longitudinal study. J. Reprod. Infant Psychol. 2021, 39, 422–434. [Google Scholar] [CrossRef] [PubMed]
- Gambin, M.; Sękowski, M.; Woźniak-Prus, M.; Wnuk, A.; Oleksy, T.; Cudo, A.; Hansen, K.; Huflejt-Łukasik, M.; Kubicka, K.; Łyś, A.E.; et al. Generalized anxiety and depressive symptoms in various age groups during the COVID-19 lockdown in Poland. Specific predictors and differences in symptoms severity. Compr. Psychiatry 2021, 105, 152222. [Google Scholar] [CrossRef] [PubMed]
- Ogunkola, I.O.; Adebisi, Y.A.; Imo, U.F.; Odey, G.O.; Esu, E.; Lucero-Prisno, D.E., 3rd. Rural communities in Africa should not be forgotten in responses to COVID-19. Int. J. Health Plan. Manag. 2020, 35, 1302–1305. [Google Scholar] [CrossRef] [PubMed]
- Apaijitt, P.; Wiwanitkit, V. Knowledge of coronavirus disease 2019 (COVID-19) by medical personnel in a rural area of Thailand. Infect. Control Hosp. Epidemiol. 2020, 41, 1243–1244. [Google Scholar] [CrossRef] [PubMed]
- Takashima, R.; Onishi, R.; Saeki, K.; Hirano, M. Perception of COVID-19 Restrictions on Daily Life among Japanese Older Adults: A Qualitative Focus Group Study. Healthcare 2020, 8, 450. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Sano, C. Fears Related to COVID-19 among Rural Older People in Japan. Healthcare 2021, 9, 524. [Google Scholar] [CrossRef]
- Ranscombe, P. Rural areas at risk during COVID-19 pandemic. Lancet Infect. Dis. 2020, 20, 545. [Google Scholar] [CrossRef]
- Kokkinaki, T.; Hatzidaki, E. Covid-19 Pandemic-Related Restrictions: Factors That May Affect Perinatal Maternal Mental Health and Implications for Infant Development. Front. Pediatrics 2022, 10, 846627. [Google Scholar] [CrossRef]
- Węgrzynowska, M.; Doroszewska, A.; Witkiewicz, M.; Baranowska, B. Polish maternity services in times of crisis: In search of quality care for pregnant women and their babies. Health Care Women Int. 2020, 41, 1335–1348. [Google Scholar] [CrossRef]
- Wszolek, K.; Pruski, D.; Tomczyk, K.; Kampioni, M.; Chmaj-Wierzchowska, K.; Przybylski, M.; Wilczak, M. Women’s Healthcare Services since the COVID-19 Pandemic Outbreak in Poland. Int. J. Environ. Res. Public Health 2021, 19, 180. [Google Scholar] [CrossRef]
- Feduniw, S.; Modzelewski, J.; Kajdy, A.; Sys, D.; Kwiatkowski, S.; Makomaska-Szaroszyk, E.; Rabijewski, M. Anxiety of pregnant women in time of catastrophic events, including COVID-19 pandemic: A systematic review and meta-analysis. J. Psychosom. Obstet. Gynecol. 2021, 1–11. [Google Scholar] [CrossRef]
- Preis, H.; Mahaffey, B.; Lobel, M. Psychometric properties of the Pandemic-Related Pregnancy Stress Scale (PREPS). J. Psychosom. Obstet. Gynecol. 2020, 41, 191–197. [Google Scholar] [CrossRef]
- Romero-Gonzalez, B.; Puertas-Gonzalez, J.A.; Mariño-Narvaez, C.; Peralta-Ramirez, M.I. Confinement variables by COVID-19 predictors of anxious and depressive symptoms in pregnant women [Variables del confinamiento por COVID-19 predictoras de sintomatología ansiosa y depresiva en mujeres embarazadas]. Med. Clin. 2021, 156, 172–176. [Google Scholar] [CrossRef]
- Masten, A.S. Ordinary magic. Resilience processes in development. Am. Psychol. 2001, 56, 227–238. [Google Scholar] [CrossRef]
- Young, C.; Roberts, R.; Ward, L. Application of resilience theories in the transition to parenthood: A scoping review. J. Reprod. Infant Psychol. 2019, 37, 139–160. [Google Scholar] [CrossRef]
- Masten, A.S.; Powell, J.L. A resilience framework for research, policy, and practice. In Resilience and Vulnerability: Adaptation in the Context of Childhood Adversities; Cambridge University Press: Cambridge, UK, 2003; pp. 1–25. [Google Scholar] [CrossRef]
- Luo, Z.; Shen, Y.; Yuan, J.; Zhao, Y.; Liu, Z.; Shangguan, F. Perceived Stress, Resilience, and Anxiety among Pregnant Chinese Women during the COVID-19 Pandemic: Latent Profile Analysis and Mediation Analysis. Front. Psychol. 2021, 12, 2851. [Google Scholar] [CrossRef]
- Tam, C.C.; Li, X.; Benotsch, E.G.; Lin, D. A Resilience-Based Intervention Programme to Enhance Psychological Well-Being and Protective Factors for Rural-to-Urban Migrant Children in China. Appl. Psychol. Health Well-Being 2020, 12, 53–76. [Google Scholar] [CrossRef]
- Ma, X.; Wang, Y.; Hu, H.; Tao, X.G.; Zhang, Y.; Shi, H. The impact of resilience on prenatal anxiety and depression among pregnant women in Shanghai. J. Affect. Disord. 2019, 250, 57–64. [Google Scholar] [CrossRef]
- Pinar, G.; Avsar, F.; Aslantekin, F. Evaluation of the Impact of Childbirth Education Classes in Turkey on Adaptation to Pregnancy Process, Concerns About Birth, Rate of Vaginal Birth, and Adaptation to Maternity: A Case-Control Study. Clin. Nurs. Res. 2018, 27, 315–342. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- British Psychological Society. Ethics Guidelines for Internet-Mediated Research; The British Psychological Society: London, UK, 2017. [Google Scholar]
- Ilska, M.; Kołodziej-Zaleska, A.; Brandt-Salmeri, A.; Preis, H.; Lobel, M. Pandemic-related pregnancy stress assessment-Psychometric properties of the Polish PREPS and its relationship with childbirth fear. Midwifery 2021, 96, 102940. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Levis, B.; Negeri, Z.; Sun, Y.; Benedetti, A.; Thombs, B.D. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: Systematic review and meta-analysis of individual participant data. BMJ (Clin. Res. Ed.) 2020, 371, m4022. [Google Scholar] [CrossRef]
- Yalniz, H.; Canan, F.; Genc, R.E.; Kuloglu, M.M.; Gecici, Ö. Development of a scale of traumatic childbirth perception. Turk. J. Med. Sci. 2016, 8, 81–88. [Google Scholar]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2013. [Google Scholar] [CrossRef]
- McCabe-Beane, J.E.; Segre, L.S.; Perkhounkova, Y.; Stuart, S.; O’Hara, M.W. The identification of severity ranges for the Edinburgh Postnatal Depression Scale. J. Reprod. Infant Psychol. 2016, 34, 293–303. [Google Scholar] [CrossRef]
- Gotlib, J.; Baranowska, B.; Rzońca, E.; Pawlicka, P.; Tataj-Puzyna, U.; Cieślak, I.; Jaworski, M.; Panczyk, M. Changes in maternity care in Poland perceived by midwives working in the SARS-CoV-2 pandemic. A preliminary study. Nurs. Probl. 2021, 29, 116–123. [Google Scholar] [CrossRef]
- Spinola, O.; Liotti, M.; Speranza, A.M.; Tambelli, R. Effects of COVID-19 Epidemic Lockdown on Postpartum Depressive Symptoms in a Sample of Italian Mothers. Front. Psychiatry 2020, 11, 589916. [Google Scholar] [CrossRef] [PubMed]
- Horsch, A.; Lalor, J.; Downe, S. Moral and mental health challenges faced by maternity staff during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, S141–S142. [Google Scholar] [CrossRef] [PubMed]
- Kajdy, A.; Feduniw, S.; Ajdacka, U.; Modzelewski, J.; Baranowska, B.; Sys, D.; Pokropek, A.; Pawlicka, P.; Kaźmierczak, M.; Rabijewski, M.; et al. Risk factors for anxiety and depression among pregnant women during the COVID-19 pandemic: A web-based cross-sectional survey. Medicine 2020, 99, e21279. [Google Scholar] [CrossRef] [PubMed]
- Wszolek, K.M.; Chmaj-Wierzchowska, K.; Wilczak, M. Management of birth, postpartum care and breastfeeding—Polish recommendations and guidelines during SARS-CoV-2 pandemic. Ginekol. Pol. 2021, 92, 387–391. [Google Scholar] [CrossRef]
- Thapa, S.B.; Mainali, A.; Schwank, S.E.; Acharya, G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet. Gynecol. Scand. 2020, 99, 817–818. [Google Scholar] [CrossRef]
- Khedmat, L.; Mohaghegh, P.; Veysizadeh, M.; Hosseinkhani, A.; Fayazi, S.; Mirzadeh, M. Pregnant women and infants against the infection risk of COVID-19: A review of prenatal and postnatal symptoms, clinical diagnosis, adverse maternal and neonatal outcomes, and available treatments. Arch. Gynecol. Obstet. 2022, 306, 323–335. [Google Scholar] [CrossRef]
- Rubertsson, C.; Wickberg, B.; Gustavsson, P.; Rådestad, I. Depressive symptoms in early pregnancy, two months and one year postpartum-prevalence and psychosocial risk factors in a national Swedish sample. Arch. Women’s Ment. Health 2005, 8, 97–104. [Google Scholar] [CrossRef]
- Ryff, C.D.; Singer, B. Flourishing under fire: Resilience as a prototype of challenged thriving. In Flourishing: Positive Psychology and the Life Well-Lived; American Psychological Association: Worcester, MA, USA, 2003; pp. 15–36. [Google Scholar] [CrossRef]
- Skrove, M.; Romundstad, P.; Indredavik, M.S. Resilience, lifestyle and symptoms of anxiety and depression in adolescence: The Young-HUNT study. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 407–416. [Google Scholar] [CrossRef]
- Wu, Y.; Sang, Z.; Zhang, X.-C.; Margraf, J. The Relationship between Resilience and Mental Health in Chinese College Students: A Longitudinal Cross-Lagged Analysis. Front. Psychol. 2020, 11, 108. [Google Scholar] [CrossRef]
- Hain, S.; Oddo-Sommerfeld, S.; Bahlmann, F.; Louwen, F.; Schermelleh-Engel, K. Risk and protective factors for antepartum and postpartum depression: A prospective study. J. Psychosom. Obstet. Gynaecol. 2016, 37, 119–129. [Google Scholar] [CrossRef]
- Mautner, E.; Stern, C.; Avian, A.; Deutsch, M.; Fluhr, H.; Greimel, E. Maternal Resilience and Postpartum Depression at the Neonatal Intensive Care Unit. Front. Pediatrics 2022, 10, 864373. [Google Scholar] [CrossRef]
- Nie, C.; Dai, Q.; Zhao, R.; Dong, Y.; Chen, Y.; Ren, H. The impact of resilience on psychological outcomes in women with threatened premature labor and spouses: A cross-sectional study in Southwest China. Health Qual. Life Outcomes 2017, 15, 26. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, X.; Zhao, J.; Zhang, W.; Cui, C.; Yang, F.; Ma, R.; Jia, Y. Prevalence of Prenatal Depression among Pregnant Women and the Importance of Resilience: A Multi-Site Questionnaire-Based Survey in Mainland China. Front. Psychiatry 2020, 11, 374. [Google Scholar] [CrossRef]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef]
- Mandar, O.; Idrees, M.B.; Ahmed, A.; ALhabardi, N.; Hassan, B.; Adam, I. Prevalence and associated factors of fear for childbirth among pregnant women in eastern Sudan. J. Reprod. Infant Psychol. 2021. [Google Scholar] [CrossRef]
- O’Connell, M.A.; Leahy-Warren, P.; Kenny, L.C.; O’Neill, S.M.; Khashan, A.S. The prevalence and risk factors of fear of childbirth among pregnant women: A cross-sectional study in Ireland. Acta Obstet. Gynecol. Scand. 2019, 98, 1014–1023. [Google Scholar] [CrossRef]
- Nilsson, C.; Hessman, E.; Sjöblom, H.; Dencker, A.; Jangsten, E.; Mollberg, M.; Patel, H.; Sparud-Lundin, C.; Wigert, H.; Begley, C. Definitions, measurements and prevalence of fear of childbirth: A systematic review. BMC Pregnancy Childbirth 2018, 18, 28. [Google Scholar] [CrossRef]
- Wijma, K.; Wijma, B.; Zar, M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J. Psychosom. Obstet. Gynecol. 1998, 19, 84–97. [Google Scholar] [CrossRef]
- Yalnız, H.; Genc, R. The effects of Psychoeducation on the Traumatic Perception of the Birth Phenomenon in women with Substance-use Disorders. Subst. Use Misuse 2019, 54, 2066–2074. [Google Scholar] [CrossRef]
- Putyński, L.; Paciorek, M. Kwestionariusz Lęku Porodowego (KLP II) wersja zrewidowana–konstrukcja i właściwości psychometryczne. Acta Univ. Lodz. Folia Psychol. 2008, 12, 129–133. [Google Scholar]
- Kaźmierczak, M.; Sołdyńska, M.; Gierszewska, M.; Gebuza, G.; Mieczkowska, E. Assessment of fear in women before childbirth. Nurs. Public Health 2017, 7, 69–75. [Google Scholar] [CrossRef][Green Version]
- Davydov, D.M.; Stewart, R.; Ritchie, K.; Chaudieu, I. Resilience and mental health. Clin. Psychol. Rev. 2010, 30, 479–495. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Huang, J.; Li, Y.; Liao, B. The prevalence and predictors of fear of childbirth among pregnant Chinese women: A hierarchical regression analysis. BMC Pregnancy Childbirth 2021, 21, 643. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Silva, J.; Caracuel, A.; Lozano-Ruiz, A.; Alderdice, F.; Lobel, M.; Perra, O.; Caparros-Gonzalez, R.A. Pandemic-related pregnancy stress among pregnant women during the COVID-19 pandemic in Spain. Midwifery 2021, 103, 103163. [Google Scholar] [CrossRef]
- Schaal, N.K.; La Marca-Ghaemmaghami, P.; Preis, H.; Mahaffey, B.; Lobel, M.; Amiel Castro, R. The German version of the pandemic-related pregnancy stress scale: A validation study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 256, 40–45. [Google Scholar] [CrossRef]
- Dikmen-Yildiz, P.; Ayers, S.; Phillips, L. Longitudinal trajectories of post-traumatic stress disorder (PTSD) after birth and associated risk factors. J. Affect. Disord. 2018, 229, 377–385. [Google Scholar] [CrossRef]
- Brown, A.; Nielsen, J.D.J.; Russo, K.; Ayers, S.; Webb, R. The Journey towards resilience following a traumatic birth: A grounded theory. Midwifery 2022, 104, 103204. [Google Scholar] [CrossRef]
- Barzilay, R.; Moore, T.M.; Greenberg, D.M.; DiDomenico, G.E.; Brown, L.A.; White, L.K.; Gur, R.C.; Gur, R.E. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl. Psychiatry 2020, 10, 291. [Google Scholar] [CrossRef]
- Kumar, S.; Lee, N.K.; Pinkerton, E.; Wroblewski, K.E.; Lengyel, E.; Tobin, M. Resilience: A mediator of the negative effects of pandemic-related stress on women’s mental health in the USA. Arch. Women’s Ment. Health 2022, 25, 137–146. [Google Scholar] [CrossRef]
- King, S.; Laplante, D.P. Using natural disasters to study prenatal maternal stress in humans. Adv. Neurobiol. 2015, 10, 285–313. [Google Scholar] [CrossRef]
- Kossakowska, K. Incidence and determinants of postpartum depression among healthy pregnant women and high-risk pregnant women. Postępy Psychiatr. Neurol. 2016, 25, 1–21. [Google Scholar] [CrossRef]
- Sim, A.; Bowes, L.; Gardner, F. The Promotive Effects of Social Support for Parental Resilience in a Refugee Context: A Cross-Sectional Study with Syrian Mothers in Lebanon. Prev. Sci. Off. J. Soc. Prev. Res. 2019, 20, 674–683. [Google Scholar] [CrossRef]
- Young, C.; Roberts, R.; Ward, L. Enhancing resilience in the transition to parenthood: A thematic analysis of parents’ perspectives. J. Reprod. Infant Psychol. 2021, 39, 358–370. [Google Scholar] [CrossRef]
- Andrews, D.; Nonnecke, B.; Preece, J. Electronic Survey Methodology: A Case Study in Reaching Hard-to-Involve Internet Users. Int. J. Hum. Comput. Interact. 2003, 16, 185–210. [Google Scholar] [CrossRef]
| Variable | n (%) | EPDS Scores | |||||
|---|---|---|---|---|---|---|---|
| M | SD | Mean Rank | U/H | p | |||
| Education | 551.000 | 0.747 | |||||
| High school and lower | 19 (23.8) | 8.6 | 5.1 | 39.0 | |||
| University degree | 61 (76.3) | 9.7 | 6.4 | 41.0 | |||
| Place of residence | 2.118 | 0.347 | |||||
| Rural | 10 (12.5) | 10.5 | 6.5 | 44.5 | |||
| Small city | 18 (22.5) | 7.4 | 5.4 | 33.6 | |||
| Large city | 52 (65.0) | 9.9 | 6.2 | 42.1 | |||
| Marital status | 570.500 | 0.919 | |||||
| Marital | 61 (76.3) | 9.4 | 5.9 | 40.7 | |||
| Partnership | 19 (23.8) | 9.5 | 6.7 | 40.0 | |||
| Children | 1.509 | 0.470 | |||||
| None | 31 (38.9) | 9.1 | 6.3 | 39.0 | |||
| One | 26 (32.5) | 8.7 | 5.9 | 37.9 | |||
| Two | 23 (28.7) | 10.7 | 6.1 | 45.5 | |||
| Economic situation | 0.695 | 0.706 | |||||
| Very good | 14 (17.5) | 10.7 | 7.9 | 44.1 | |||
| Good | 48 (60.0) | 9.4 | 5.7 | 49.7 | |||
| Average | 18 (22.5) | 8.4 | 5.9 | 37.3 | |||
| Current pregnancy status | 419.000 | 0.069 | |||||
| High risk | 19 (23.8) | 7.5 | 6.8 | 32.1 | |||
| Health | 61 (76.3) | 10.0 | 5.8 | 43.1 | |||
| Previous fertility problems | 458.500 | 0.251 | |||||
| Yes | 18 (22.5) | 8.4 | 7.3 | 35.0 | |||
| No | 62 (77.5) | 9.7 | 5.8 | 42.1 | |||
| Planned pregnancy | 300.000 | 0.077 | |||||
| Yes | 67 (83.8) | 9.0 | 6.4 | 38.5 | |||
| No | 13 (16.3) | 11.4 | 4.3 | 50.9 | |||
| COVID-19 impact on the family’s economic situation | |||||||
| Improved | 3 (3.8) | 7.7 | 4.0 | 34.5 | 2.827 | 0.243 | |
| Not changed | 56 (70.0) | 8.8 | 6.2 | 38.1 | |||
| Worsened | 21 (26.3) | 11.3 | 6.1 | 47.7 | |||
| Variable | Lower Resilience n = 41 | Higher Resilience n = 39 | Χ2 | df | p | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Education | 2.070 | 1 | 0.150 | |||||
| High school and lower | 7 | 17.1 | 12 | 30.8 | ||||
| University degree | 34 | 82.9 | 27 | 69.2 | ||||
| Place of residence | 3.044 | 2 | 0.218 | |||||
| Rural | 6 | 14.6 | 4 | 10.3 | ||||
| Small city | 6 | 14.6 | 12 | 30.8 | ||||
| Large city | 29 | 70.7 | 23 | 59.0 | ||||
| Marital status | 0.150 | 1 | 0.698 | |||||
| Marital | 32 | 78.0 | 29 | 74.4 | ||||
| Partnership | 9 | 22.0 | 10 | 25.6 | ||||
| Children | 0.438 | 2 | 0.803 | |||||
| None | 17 | 41.5 | 14 | 35.9 | ||||
| One | 12 | 29.3 | 14 | 35.9 | ||||
| Two | 12 | 29.3 | 11 | 28.2 | ||||
| Economic situation | 2.066 | 2 | 0.356 | |||||
| Very good | 9 | 22.0 | 5 | 12.8 | ||||
| Good | 25 | 61.0 | 23 | 59.0 | ||||
| Average | 7 | 17.1 | 11 | 28.2 | ||||
| Current pregnancy status | 0.150 | 1 | 0.698 | |||||
| High risk | 9 | 22.0 | 10 | 25.6 | ||||
| Health | 32 | 78.0 | 29 | 74.4 | ||||
| Previous fertility problems | 0.015 | 1 | 0.904 | |||||
| Yes | 9 | 22.0 | 9 | 23.1 | ||||
| No | 32 | 78.0 | 30 | 76.9 | ||||
| Planned pregnancy | 1.016 | 1 | 0.313 | |||||
| Yes | 36 | 87.8 | 31 | 79.5 | ||||
| No | 5 | 12.2 | 8 | 20.5 | ||||
| COVID-19 impact on the family’s economic situation | 0.998 | 2 | 0.607 | |||||
| Improved | 2 | 4.9 | 1 | 2.6 | ||||
| Not changed | 30 | 73.2 | 26 | 66.7 | ||||
| Worsened | 9 | 22.0 | 12 | 30.8 | ||||
| Variable | Lower Resilience | Higher Resilience | t | p | Cohen’s d | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Infection stress | 12.0 | 5.3 | 10.8 | 6.1 | 0.986 | 0.327 | NA |
| Preparedness stress | 24.6 | 8.1 | 19.9 | 8.6 | 2.448 | 0.017 * | 0.56 |
| Positive appraisal | 6.3 | 2.6 | 7.2 | 3.5 | −1.179 | 0.242 | NA |
| Pandemic-related pregnancy stress (total PREPS) | 36.6 | 12.1 | 30.7 | 13.9 | 2.007 | 0.048 * | 0.45 |
| Variables | M | SD | Range of Scores | LL; UL 95% CI | Skewness | Kurtosis |
|---|---|---|---|---|---|---|
| Prenatal depression (EPDS) | 9.43 | 6.12 | 0–23 | 8.06; 10.79 | 0.46 | 0.53 |
| Resilience (CD-RISK) | 19.95 | 8.60 | 0–36 | 18.04; 21.86 | −0.23 | −0.65 |
| Perinatal Infection Stress (PREPS) | 2.28 | 1.14 | 1–5 | 2.03; 2.54 | 0.16 | −0.74 |
| Preparedness Stress (PREPS) | 3.19 | 1.23 | 1–5 | 2.91; 2.46 | −0.47 | −0.78 |
| Positive Appraisal (PREPS) | 2.25 | 1.03 | 1–5 | 2.02; 2.47 | 0.32 | −0.53 |
| Pandemic-related stress (total PREPS) | 2.81 | 1.10 | 1–5 | 2.57; 3.06 | −0.38 | −0.76 |
| Traumatic childbirth perception (TPBS) | 57.30 | 26.21 | 11–112 | 51.47; 63.13 | 0.27 | −0.76 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Prenatal depression (EPDS) | 1 | |||||
| 2. Resilience (CD-RISK) | −0.62 ** | 1 | ||||
| 3. Perinatal Infection Stress (PREPS) | 0.09 | −0.12 | 1 | |||
| 4. Preparedness Stress (PREPS) | 0.38 ** | −0.36 ** | 0.70 ** | 1 | ||
| 5. Positive Appraisal (PREPS) | −0.18 | 0.10 | 0.21 | 0.23 * | 1 | |
| 6. Pregnancy-related stress (total PREPS) | 0.29 * | −0.28 * | 0.89 ** | 0.95 ** | 0.24 | 1 |
| 7. Traumatic birth perception (TBPS) | 0.51 ** | −0.62 ** | 0.14 | 0.42 ** | 0.07 | 0.34 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Studniczek, A.; Kossakowska, K. Experiencing Pregnancy during the COVID-19 Lockdown in Poland: A Cross-Sectional Study of the Mediating Effect of Resiliency on Prenatal Depression Symptoms. Behav. Sci. 2022, 12, 371. https://doi.org/10.3390/bs12100371
Studniczek A, Kossakowska K. Experiencing Pregnancy during the COVID-19 Lockdown in Poland: A Cross-Sectional Study of the Mediating Effect of Resiliency on Prenatal Depression Symptoms. Behavioral Sciences. 2022; 12(10):371. https://doi.org/10.3390/bs12100371
Chicago/Turabian StyleStudniczek, Anna, and Karolina Kossakowska. 2022. "Experiencing Pregnancy during the COVID-19 Lockdown in Poland: A Cross-Sectional Study of the Mediating Effect of Resiliency on Prenatal Depression Symptoms" Behavioral Sciences 12, no. 10: 371. https://doi.org/10.3390/bs12100371
APA StyleStudniczek, A., & Kossakowska, K. (2022). Experiencing Pregnancy during the COVID-19 Lockdown in Poland: A Cross-Sectional Study of the Mediating Effect of Resiliency on Prenatal Depression Symptoms. Behavioral Sciences, 12(10), 371. https://doi.org/10.3390/bs12100371






