The Integration of Meditation and Positive Psychology Practices to Relieve Stress in Women Workers (Flourish): Effects in Two Pilot Studies
Abstract
1. Introduction
2. Materials and Methods
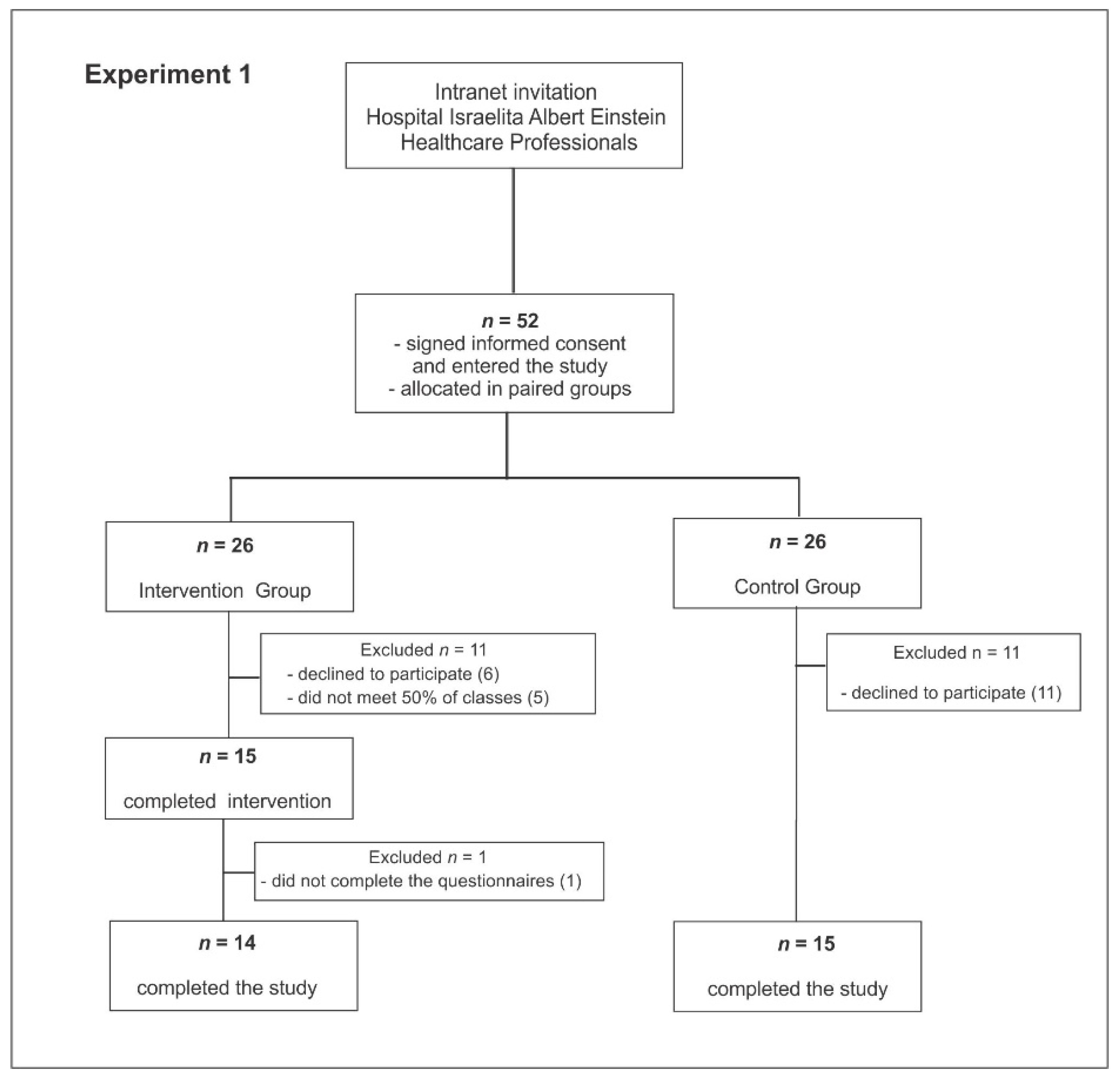
2.1. Experiment 1
2.1.1. Participants
2.1.2. Design
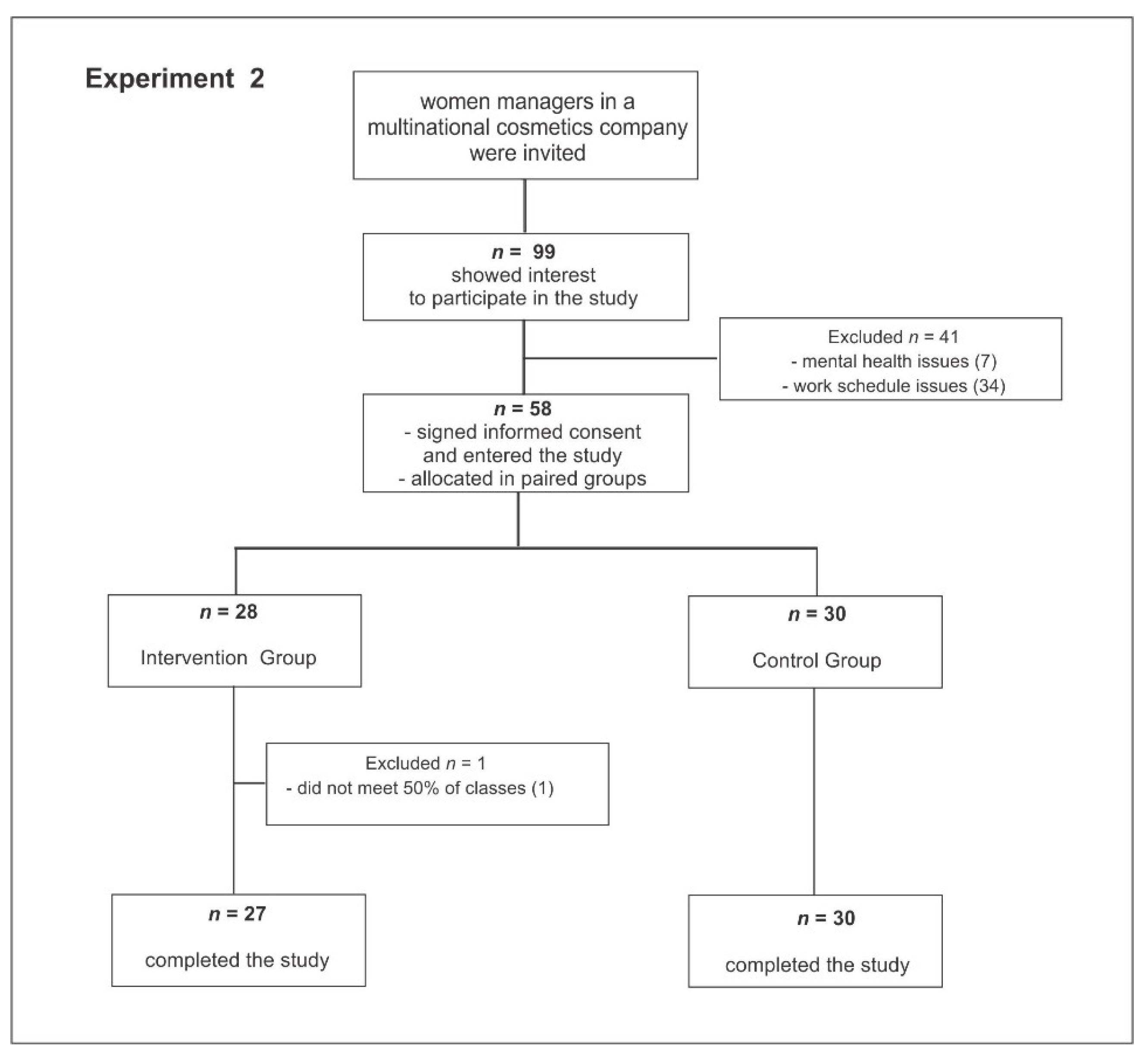
2.2. Experiment 2
2.2.1. Participants
2.2.2. Design
2.3. Intervention (The Same Protocol Was Applied in Experiments 1 and 2)
2.4. Meeting Topics and Activities in the Flourish Program
- 1st Week—Introducing the program. Theory: what is attention and focus. Practices: gratitude diary; counting blessings or reflecting on those aspects of one’s life for which one should be grateful.
- 2nd week—Theory: life is relationship, interdependence and a sense of belonging. Practices: sharing or talking about the gratitude diary, body scanning, mindful attention focused on corporeal experience.
- 3rd week—Theory: cultivating positive emotions and empathy. Practices: awareness of the breathing act (mindful breathing) and body scanning.
- 4th week—Theory: cultivating compassion. Practice: loving-kindness meditation and mindful breathing.
- 5th week—Theory: gratitude, reflecting on personal life aspects for which to be grateful. Practice: sharing the gratitude diary and empathetic joy meditation.
- 6th week—Theory: PERMA model (positive emotion, engagement, meaning, positive relationships and achievement). Practices: mindful breathing, loving-kindness meditation and sharing the gratitude diary.
- 7th week—Theory: character strengths: identifying and using them. Practices: sharing character strengths; empathetic joy meditation.
- 8th week—Theory: hope, expectations in life. Review of the contents and carried-out practices. Practice: mindful breathing.
2.5. Instruments (The Same Were Used for Both Experiments)
2.6. Statistical Analysis
3. Results
3.1. Experiment 1
3.1.1. Baseline Characteristics
3.1.2. Changes in Perceived Stress after the Intervention
3.1.3. Changes in Other Variables Studied after the Intervention
3.2. Experiment 2
3.2.1. Baseline Characteristics
3.2.2. Changes in Perceived Stress after the Intervention
3.2.3. Changes in Other Variables Studied after the Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychological Association. Stress in America: The State of Our Nation. In Stress in America Survey. 2017. Available online: https://www.apa.org/news/press/releases/stress/2017/uncertainty-health-care.pdf (accessed on 5 January 2021).
- Medina-Inojosa, J.R.; Vinnakota, S.; Garcia, M.; Calle, M.A.; Mulvagh, S.L.; Lopez-Jimenez, F.; Bhagra, A. Role of Stress and Psychosocial Determinants on Women’s Cardiovascular Risk and Disease Development. J. Women’s Health 2019, 28, 483–489. [Google Scholar] [CrossRef]
- Weinberg, A.; Creed, F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet 2000, 355, 533–537. [Google Scholar] [CrossRef]
- Preston, S.D.; Buchanan, T.W.; Stansfield, R.B.; Bechara, A. Effects of anticipatory stress on decision making in a gambling task. Behav. Neurosci. 2007, 121, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Spickard, J.A.; Gabbe, S.G.; Christensen, J.F. Mid-Career Burnout in Generalist and Specialist Physicians. JAMA 2002, 288, 1447. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Bradley, K.A.; Wipf, J.E.; Back, A.L. Burnout and Self-Reported Patient Care in an Internal Medicine Residency Program. Ann. Intern. Med. 2002, 136, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Causes and consequences of occupational stress in emergency nurses, a longitudinal study. J. Nurs. Manag. 2015, 23, 346–358. [Google Scholar] [CrossRef] [PubMed]
- Brett, J.M.; Stroh, L.K. Working 61 plus hours a week: Why do managers do it? J. Appl. Psychol. 2003, 88, 67–78. [Google Scholar] [CrossRef]
- Gardiner, M.; Tiggemann, M. Gender differences in leadership style, job stress and mental health in male- and female-dominated industries. J. Occup. Organ. Psychol. 1999, 72, 301–315. [Google Scholar] [CrossRef]
- Gleichgerrcht, E.; Decety, J. Empathy in Clinical Practice: How Individual Dispositions, Gender, and Experience Moderate Empathic Concern, Burnout, and Emotional Distress in Physicians. PLoS ONE 2013, 8, e61526. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Mindfulness-based Interventions in Context: Past, Present, and Future. Clin. Psychol. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Burton, A.; Burgess, C.; Dean, S.; Koutsopoulou, G.Z.; Hugh-Jones, S. How Effective Are Mindfulness-Based Interventions for Reducing Stress among Healthcare Professionals? A Systematic Review and Meta-Analysis: Mindfulness Interventions for Stress Reduction. Stress Health 2017, 33, 3–13. [Google Scholar] [CrossRef]
- Lacerda, S.S.; Little, S.W.; Kozasa, E.H. A Stress Reduction Program Adapted for the Work Environment: A Randomized Controlled Trial With a Follow-Up. Front. Psychol. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Irving, J.A.; Dobkin, P.L.; Park, J. Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction (MBSR). Complement. Ther. Clin. Pract. 2009, 15, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, S.G.; Grossman, P.; Hinton, D.E. Loving-kindness and compassion meditation: Potential for psychological interventions. Clin. Psychol. Rev. 2011, 31, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Boellinghaus, I.; Jones, F.W.; Hutton, J. The Role of Mindfulness and Loving-Kindness Meditation in Cultivating Self-Compassion and Other-Focused Concern in Health Care Professionals. Mindfulness 2014, 5, 129–138. [Google Scholar] [CrossRef]
- dos Santos, T.M.; Kozasa, E.H.; Carmagnani, I.S.; Tanaka, L.H.; Lacerda, S.S.; Nogueira-Martins, L.A. Positive Effects of a Stress Reduction Program Based on Mindfulness Meditation in Brazilian Nursing Professionals: Qualitative and Quantitative Evaluation. Explore 2016, 12, 90–99. [Google Scholar] [CrossRef]
- Seligman, M.E.; Csikszentmihalyi, M. Positive Psychology. An Introduction. Am. Psychol. 2000, 55, 5–14. [Google Scholar] [CrossRef]
- Seligman, M.E.P.; Peterson, C. Positive Clinical Psychology. In A Psychology of Human Strengths: Fundamental Questions and Future Directions for a Positive Psychology; American Psychological Association: Washington, DC, USA, 2003; pp. 305–317. [Google Scholar]
- Linley, P.A.; Joseph, S. (Eds.) Positive Psychology in Practice: Linley/Positive; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004. [Google Scholar]
- Seligman, M.E.P.; Steen, T.A.; Park, N.; Peterson, C. Positive Psychology Progress: Empirical Validation of Interventions. Am. Psychol. 2005, 60, 410–421. [Google Scholar] [CrossRef]
- Sin, N.L.; Lyubomirsky, S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. J. Clin. Psychol. 2009, 65, 467–487. [Google Scholar] [CrossRef]
- Bolier, L.; Haverman, M.; Westerhof, G.J.; Riper, H.; Smit, F.; Bohlmeijer, E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health 2013, 13, 119. [Google Scholar] [CrossRef]
- Hendriks, T.; Schotanus-Dijkstra, M.; Hassankhan, A.; De Jong, J.; Bohlmeijer, E. The Efficacy of Multi-component Positive Psychology Interventions: A Systematic Review and Meta-analysis of Randomized Controlled Trials. J. Happiness Stud. 2020, 21, 357–390. [Google Scholar] [CrossRef]
- Ivtzan, I.; Young, T.; Martman, J.; Jeffrey, A.; Lomas, T.; Hart, R.; Eiroa-Orosa, F.J. Integrating Mindfulness into Positive Psychology: A Randomised Controlled Trial of an Online Positive Mindfulness Program. Mindfulness 2016, 7, 1396–1407. [Google Scholar] [CrossRef]
- Shapiro, S.L.; Carlson, L.E.; Astin, J.A.; Freedman, B. Mechanisms of mindfulness. J. Clin. Psychol. 2006, 62, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, S.L. The integration of mindfulness and psychology. J. Clin. Psychol. 2009, 65, 555–560. [Google Scholar] [CrossRef]
- Jazaieri, H.; Jinpa, G.T.; McGonigal, K.; Rosenberg, E.L.; Finkelstein, J.; Simon-Thomas, E.; Cullen, M.; Doty, J.R.; Gross, J.J.; Goldin, P.R. Enhancing Compassion: A Randomized Controlled Trial of a Compassion Cultivation Training Program. J. Happiness Stud. 2012, 14, 1113–1126. [Google Scholar] [CrossRef]
- Dodds, S.E.; Pace, T.W.W.; Bell, M.L.; Fiero, M.; Negi, L.T.; Raison, C.L.; Weihs, K.L. Erratum to: Feasibility of Cognitively-Based Compassion Training (CBCT) for breast cancer survivors: A randomized, wait list controlled pilot study. Support. Care Cancer 2015, 23, 3609–3611. [Google Scholar] [CrossRef] [PubMed]
- Neff, K.D.; Germer, C.K. A Pilot Study and Randomized Controlled Trial of the Mindful Self-Compassion Program: A Pilot and Randomized Trial of MSC Program. J. Clin. Psychol. 2013, 69, 28–44. [Google Scholar] [CrossRef]
- Coelhoso, C.C.; Tobo, P.R.; Lacerda, S.S.; Lima, A.H.; Barrichello, C.R.C.; Jr, E.A.; Kozasa, E.H. A New Mental Health Mobile App for Well-Being and Stress Reduction in Working Women: Randomized Controlled Trial. J. Med Internet Res. 2019, 21, e14269. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Luft, C.D.B.; de Sanches, S.O.; Mazo, G.Z.; Andrade, A. Brazilian version of the Perceived Stress Scale: Translation and validation for the elderly. Rev. Saude Publica 2007, 41, 606–615. [Google Scholar] [CrossRef]
- Mari, J.D.J.; Williams, P. A Validity Study of a Psychiatric Screening Questionnaire (SRQ-20) in Primary Care in the city of Sao Paulo. Br. J. Psychiatry 1986, 148, 23–26. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A. Internal consistencies of the original and revised beck depression inventory. J. Clin. Psychol. 1984, 40, 1365–1367. [Google Scholar] [CrossRef]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An Inventory for Measuring Clinical Anxiety: Psychometric Properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- João, K.A.D.R.; Becker, N.B.; Jesus, S.D.N.; Martins, R.I.S. Validation of the Portuguese version of the Pittsburgh Sleep Quality Index (PSQI-PT). Psychiatry Res. 2017, 247, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Felton, J.S. Burnout as a clinical entity—its importance in health care workers. Occup. Med. 1998, 48, 237–250. [Google Scholar] [CrossRef] [PubMed]
- Ruotsalainen, J.; Serra, C.; Marine, A.; Verbeek, J. Systematic review of interventions for reducing occupational stress in health care workers. Scand. J. Work. Environ. Heal. 2008, 34, 169–178. [Google Scholar] [CrossRef]
- Suyi, Y.; Meredith, P.; Khan, A. Effectiveness of Mindfulness Intervention in Reducing Stress and Burnout for Mental Health Professionals in Singapore. Explore 2017, 13, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Beckman, H.B.; Wendland, M.; Mooney, C.; Krasner, M.S.; Quill, T.E.; Suchman, A.L.; Epstein, R.M. The Impact of a Program in Mindful Communication on Primary Care Physicians. Acad. Med. 2012, 87, 815–819. [Google Scholar] [CrossRef]
- Chakhssi, F.; Kraiss, J.T.; Sommers-Spijkerman, M.; Bohlmeijer, E.T. The effect of positive psychology interventions on well-being and distress in clinical samples with psychiatric or somatic disorders: A systematic review and meta-analysis. BMC Psychiatry 2018, 18, 1–17. [Google Scholar] [CrossRef]
- Kim, H.; Doiron, K.; Warren, M.A.; Donaldson, S.I. The international landscape of positive psychology research: A systematic review. Int. J. Wellbeing 2018, 8, 50–70. [Google Scholar] [CrossRef]
- Cheng, S.-T.; Tsui, P.K.; Lam, J.H.M. Improving mental health in health care practitioners: Randomized controlled trial of a gratitude intervention. J. Consult. Clin. Psychol. 2015, 83, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Mccullough, M.E.; Emmons, R.A.; Tsang, J.-A. The Grateful Disposition: A Conceptual and Empirical Topography. J. Pers. Soc. Psychol. 2002, 82, 112–127. [Google Scholar] [CrossRef] [PubMed]
- Pang, D.; Willibald, R. Fusing character strengths and mindfulness interventions: Benefits for job satisfaction and performance. J. Occup. Health Psychol. 2019, 24, 150. [Google Scholar] [CrossRef] [PubMed]
| Control Group (n = 15) | Intervention Group (n = 14) | Value (df) | p Value | |
|---|---|---|---|---|
| Mean (SD)/n (%) | Mean (SD)/n (%) | |||
| Age | 36.07 (7.60) | 40.20 (6.74) | −1.58 (27) | 0.126 |
| Marital status | ||||
| Single | 2 (13.33%) | 5 (35.71%) | 3.18 (4) | 0.528 c |
| Married | 8 (53.34%) | 5 (35.71%) | ||
| Partnered | 2 (13.33%) | 2 (14.29%) | ||
| Divorced | 2 (13.33%) | 2 (14.29%) | ||
| Other | 1 (6.67%) | 0 (0%) | ||
| Religion | ||||
| No religion | 4 (26.67%) | 2 (14.29%) | 9.11 (4) | 0.058 c |
| Catholic | 5 (33.33%) | 4 (28.57%) | ||
| Evangelical | 5 (33.33%) | 1 (7.14%) | ||
| Spiritist | 1 (6.67%) | 5 (35.71%) | ||
| Other | 0 (0%) | 2 (14.29%) | ||
| PSS | 23.20 (4.36) | 26.43 (5.64) | −1.01 (27) | 0.320 t |
| SRQ | 9.27 (3.86) | 10.86 (2.90) | −0.73 (27) | 0.470 t |
| BDI | 19.27 (9.84) | 20.50 (8.05) | 0.04 (27) | 0.970 t |
| BAI | 11.93 (7.00) | 17.93 (8.04) | −1.74 (27) | 0.093 t |
| PSQI | 8.93 (3.28) | 9.00 (3.40) | 0.31 (27) | 0.758 t |
| Control Group (n = 15) | Intervention Group (n = 14) | Time Effect | Group Effect | Time* Group Effect | |||
|---|---|---|---|---|---|---|---|
| Baseline | After 8 Weeks | Baseline | After 8 Weeks | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| PSS | 23.20 (4.36) | 22.13 (7.92) | 26.43 (5.64) | 21.07 (5.50) | 0.003 ** | 0.594 | 0.036 * |
| SRQ | 9.27 (3.86) | 9.40 (4.40) | 10.86 (2.90) | 8.50 (5.18) | 0.077 | 0.811 | 0.050 |
| BDI | 19.27 (9.84) | 15.73 (10.27) | 20.50 (8.05) | 15.07 (11.47) | 0.016 * | 0.931 | 0.591 |
| BAI | 11.93 (7.00) | 12.87 (9.47) | 17.93 (8.04) | 12.43 (7.61) | 0.102 | 0.310 | 0.025 * |
| PSQI | 8.93 (3.28) | 6.40 (3.87) | 9.00 (3.40) | 7.29 (3.97) | 0.002 ** | 0.696 | 0.510 |
| Control Group (n = 30) | Intervention Group (n = 27) | Value (df) | p Value | |
|---|---|---|---|---|
| Mean (SD)/n (%) | Mean (SD)/n (%) | |||
| Age | 40.93 (8.17) | 46.07 (7.87) | −2.46 (56) | 0.017 t |
| Marital status | ||||
| Single | 2 (6.68%) | 3 (10.71%) | 2.16 (3) | 0.539 c |
| Married | 16 (53.32%) | 16 (60.71%) | ||
| Partnered | 6 (20.00%) | 2 (7.14%) | ||
| Divorced | 6 (20.00%) | 6 (21.43%) | ||
| Religion | ||||
| No religion | 8 (26.68%) | 4 (14.81%) | 3.62 (5) | 0.604 c |
| Catholic | 14 (46.68%) | 14 (51.85%) | ||
| Protestant | 0 (0%) | 1 (3.70%) | ||
| Evangelical | 1 (3.33%) | 3 (11.11%) | ||
| Spiritist | 4 (13.33%) | 4 (14.81%) | ||
| Other | 3 (10.00%) | 1 (3.72%) | ||
| PSS | 21.03 (7.04) | 19.82 (7.45) | 0.64 (56) | 0.527 t |
| SRQ | 6.00 (3.50) | 6.35 (3.88) | −0.37 (56) | 0.714 t |
| BDI | 12.60 (6.45) | 13.57 (9.26) | −0.47 (56) | 0.643 t |
| BAI | 9.17 (6.68) | 9.18 (6.57) | −0.01 (56) | 0.995 t |
| PSQI | 7.17 (3.19) | 7.96 (4.17) | −0.79 (56) | 0.431 t |
| Control Group (n = 30) | Intervention Group (n = 27) | Time Effect | Group Effect | Time* Group Effect | |||
|---|---|---|---|---|---|---|---|
| Baseline | After 8 Weeks | Baseline | After 8 Weeks | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| PSS | 21.03 (7.04) | 21.46 (6.10) | 19.82 (7.45) | 17.39 (8.14) | 0.369 | 0.093 | 0.019 * |
| SRQ | 6.00 (3.50) | 6.33 (4.35) | 6.36 (3.89) | 4.93 (4.43) | 0.173 | 0.355 | 0.007 * |
| BDI | 12.60 (6.45) | 11.73 (6.68) | 13.57 (9.26) | 10.68 (11.33) | 0.229 | 0.466 | 0.161 |
| BAI | 9.17 (6.68) | 8.43 (7.71) | 9.18 (6.57) | 7.92 (7.42) | 0.418 | 0.465 | 0.980 |
| PSQI | 7.17 (3.19) | 7.34 (3.54) | 7.96 (4.17) | 6.35 (3.91) | 0.294 | 0.257 | 0.019 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, F.R.M.d.; Lacerda, S.S.; Coelhoso, C.C.; Barrichello, C.R.; Tobo, P.R.; Kozasa, E.H. The Integration of Meditation and Positive Psychology Practices to Relieve Stress in Women Workers (Flourish): Effects in Two Pilot Studies. Behav. Sci. 2021, 11, 43. https://doi.org/10.3390/bs11040043
Santos FRMd, Lacerda SS, Coelhoso CC, Barrichello CR, Tobo PR, Kozasa EH. The Integration of Meditation and Positive Psychology Practices to Relieve Stress in Women Workers (Flourish): Effects in Two Pilot Studies. Behavioral Sciences. 2021; 11(4):43. https://doi.org/10.3390/bs11040043
Chicago/Turabian StyleSantos, Fabio R. M. dos, Shirley S. Lacerda, Cassia C. Coelhoso, Carla R. Barrichello, Patricia R. Tobo, and Elisa H. Kozasa. 2021. "The Integration of Meditation and Positive Psychology Practices to Relieve Stress in Women Workers (Flourish): Effects in Two Pilot Studies" Behavioral Sciences 11, no. 4: 43. https://doi.org/10.3390/bs11040043
APA StyleSantos, F. R. M. d., Lacerda, S. S., Coelhoso, C. C., Barrichello, C. R., Tobo, P. R., & Kozasa, E. H. (2021). The Integration of Meditation and Positive Psychology Practices to Relieve Stress in Women Workers (Flourish): Effects in Two Pilot Studies. Behavioral Sciences, 11(4), 43. https://doi.org/10.3390/bs11040043






