Effectiveness of Mindfulness-Based Relapse Prevention in Individuals with Substance Use Disorders: A Systematic Review
Abstract
:1. Introduction
- I
- Do MBRP interventions lead to significant improvements in SUD variables (e.g., cravings, frequency of use) in individuals with SUD?
- II
- Do MBRP interventions lead to significant improvements in other relevant clinical variables (e.g., anxiety, depression, quality of life) in individuals with SUD?
- III
- How do MBRP interventions compare to other evidence-based interventions for individuals with SUD?
2. Materials and Methods
2.1. Research Strategy
2.2. Study Screening and Selection
2.3. Data Extraction and Quality Assessment
2.4. Data Analysis
3. Results
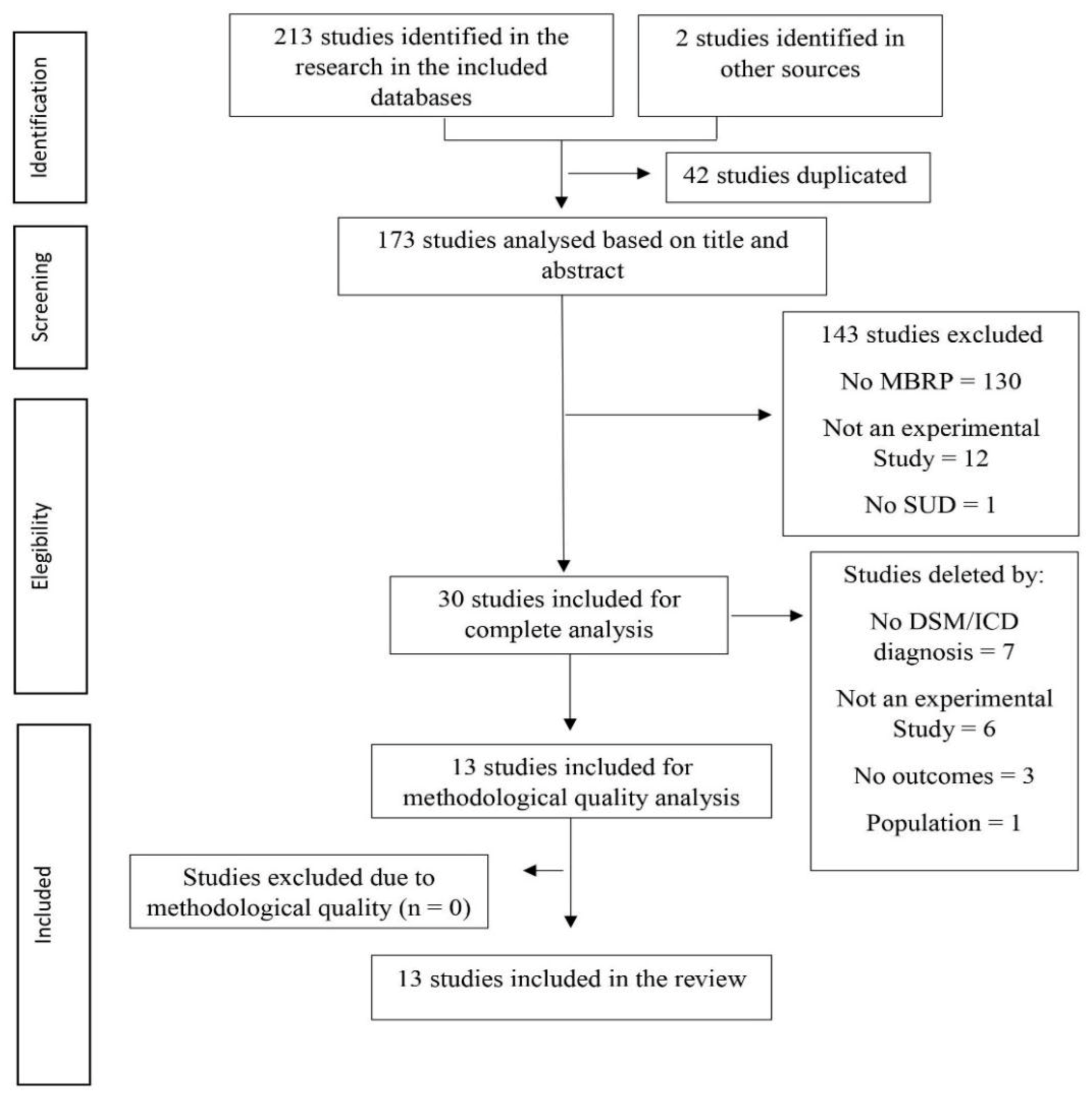
3.1. Search
3.2. Characteristics of Included Studies
3.3. Methodological Quality
3.4. Intervention Characteristics
3.5. Intervention Outcomes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| MBRP | Mindfulness-Based Relapse Prevention |
| RCT | Randomized Controlled Trials |
| SUD | Substance Use Disorders |
| TAU | Treatment as Usual |
Appendix A
| Database | Research Terms |
|---|---|
| Cochrane, Pubmed, Web of Science e Scopus | “Mindfulness-Based Relapse Prevention” OR “MBRP” AND “substance related disorder” OR “Substance dependency” OR “alcohol induced disorders” OR “Chemical Dependency” OR “substance addiction” OR “drug use disorder” OR “street drugs” |
| Study | Country | Participants | Substance Issue |
|---|---|---|---|
| Roos, Bowen, and Witkiewitz, 2020 [28] | USA | 286 participants—38.44 years.; 71.8% male | Substances (alcohol, cocaine, opioids, among others) |
| Zgierska et al., 2019 [29] | USA | 112 Participants—41 years.; 56% male | Alcohol |
| Foroushani, 2019 [31] | Iran | 55 participants—NP | Methadone |
| Witkiewitz et al., 2019 [19] | USA | 84 participants—52.27 years.; 59.5% male | Alcohol |
| Von Hammerstein et al., 2019 [22] | France | 52 participants—49.4 years.; 60% male | Alcohol |
| Yaghubi and Zargar, 2018 [33] | Iran | 70 participants—30.26 years.; 100% male | Methadone |
| Greenfield et al., 2018 [27] | USA | 191 participants—39.04 years.; 71% male | NP |
| Zgierska, Shapiro, Burzinski, Lerner, and Goodman-Strenski, 2017 [20] | USA | 123 participants—41.2 years.; 56.9% male | Alcohol |
| Yaghubi, Zargar, and Akbari, 2017 [32] | Iran | 70 participants—31.73 years.; 100% male | Methadone |
| Zullig et al., 2018 [30] | USA | 16 participants—36 years.; 37.5% male | Opioid |
| Glasner et al., 2017 [26] | USA | 63 participants—45.3 years.; 71% male | Stimulants |
| Zemestani and Ottaviani, 2016 [34] | Iran | 74 participants—30.1 years.; 79.7% male | Substances (methamphetamine, cocaine, heroin, among others) |
| Biseul, Icick, Seguin, Bellivier, and Scott, 2017 [35] | France | 6 participants—52.5 years.; 67% male | Substances (alcohol, cannabis, heroin, among others) |
| Reporting (0–11) | External Validity (0–3) | Bias (0–7) | Confounding (0–6) | Power (0,1) | Overall (0–28) | |
|---|---|---|---|---|---|---|
| Roos, Bowen, and Witkiewitz, 2020 [28] | 6 | 1 | 3 | 4 | 0 | 14 |
| Zgierska et al., 2019 [29] | 9 | 1 | 4 | 4 | 0 | 18 |
| Foroushani, 2019 [31] | 6 | 1 | 5 | 3 | 0 | 15 |
| Witkiewitz et al., 2019 [19] | 10 | 1 | 7 | 6 | 1 | 25 |
| Von Hammerstein et al., 2019 [22] | 7 | 1 | 3 | 2 | 0 | 13 |
| Yaghubi and Zargar, 2018 [33] | 7 | 2 | 3 | 4 | 1 | 17 |
| Greenfield et al., 2018 [27] | 10 | 1 | 6 | 5 | 0 | 22 |
| Zgierska et al., 2017 [20] | 9 | 1 | 6 | 4 | 1 | 21 |
| Yaghubi, Zargar, and Akbari, 2017 [32] | 7 | 1 | 5 | 5 | 1 | 19 |
| Glasner et al., 2017 [26] | 8 | 1 | 5 | 4 | 0 | 18 |
| Zullig et al., 2018 [30] | 7 | 1 | 3 | 3 | 0 | 14 |
| Biseul et al., 2017 [35] | 5 | 1 | 1 | 3 | 0 | 10 |
| Zemestani and Ottaviani, 2016 [34] | 8 | 3 | 5 | 4 | 0 | 20 |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| - | ? | - | ? | + | + | - | - | - | - | - | - | ? | Roos, Bowen, and Witkiewitz, 2020 [28] |
| - | + | - | + | + | + | - | - | - | - | - | - | - | Zgierska et al., 2019 [29] |
| - | ? | - | + | + | + | - | - | - | - | ? | ? | ? | Foroushani, 2019 [31] |
| - | + | - | - | - | + | - | - | - | - | - | - | - | Witkiewitz et al., 2019 [19] |
| ? | ? | - | ? | ? | ? | - | - | - | - | ? | ? | + | Yaghubi and Zargar, 2018 [33] |
| ? | ? | - | ? | ? | ? | - | - | - | - | - | - | - | Greenfield et al., 2018 [27] |
| - | ? | - | + | ? | ? | - | - | - | - | ? | ? | - | Zgierska et al., 2017 [20] |
| - | + | - | ? | ? | ? | - | - | - | - | - | - | ? | Yaghubi, Zargar, and Akbari, 2017 [32] |
| - | - | - | ? | + | ? | - | - | - | - | - | - | ? | Glasner et al., 2017 [26] |
| - | - | - | - | - | - | - | - | - | - | - | - | - | Zemestani and Ottaviani, 2016 [34] |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | |
|---|---|---|---|---|---|---|---|---|---|
| - | - | ? | + | - | - | - | - | - | Von Hammerstein et al., 2019 [22] |
| - | - | + | + | - | - | - | ? | - | Zullig et al., 2018 [30] |
| - | - | + | + | - | - | - | ? | - | Biseul et al., 2017 [35] |
| Study | Aim | MBRP Program | MBRP Full-Length | MBRP Time p/Session | MBRP Provider | Co-Intervention | Comparator | Follow-Up | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Roos, Bowen, and Witkiewitz, 2020 [28] | Investigate if changes coping may explain the effects of MBRP | Standard (8 sessions) | 16 h | 120 min | Clinical psychologists | No co-intervention | Relapse prevention or TAU | 2nd, 4th, 6th, and 12th month | MBRP showed significant results on heavy drinking days and increased coping over time |
| Zgierska, 2019 [29] | Analyze the effects of MBRP on alcohol use disorder | MBRP-A (8 sessions) | 16 h | 120 min | Therapist with certified mindfulness course | Usual-Care (comparator) | Usual-Care | 8th and 26th week | No significant results were found |
| Foroushani, 2019 [31] | Investigate the impact of the MBRP intervention on cravings, lapse, and mindfulness fostering | Standard (8 sessions) | 16 h | 120 min | NP | No co-intervention | No-comparator | 1st, 2nd, and 3rd month | MBRP showed significant reduction in the desire to use and in the symptoms of dysphoria and withdrawal |
| Witkiewitz et al., 2019 [19] | Evaluate the efficacy of MBRP combined with active or sham tDCS | MBRP modified version (8 sessions) | 12 h | 90 min | Trained therapists in MBRP | Transcranial direct current stimulation (tDCS) | Sham tDCS + MBRP | 2nd, 3rd, 4th and 6th month following baseline | MBRP showed reduction in the nº of drinks per day and a lower percentage of heavy drinking days over time |
| Von Hammerstein et al., 2019 [22] | Evaluate the feasibility and preliminary efficacy of the MBRP in alcohol use disorder | Standard (8 sessions) | 16 h | 120 min | NP | No co-intervention | No-comparator | 6th month | MBRP showed reduction on depression and anxiety levels and on heavy drinking days |
| Yaghubi and Zargar, 2018 [33] | Evaluate the effectiveness of MBRP on QOL and cravings | Standard (8 sessions) | 16 h | 120 min | NP | No co-intervention | No-comparator | 2nd month | MBRP showed significant results on reducing cravings and showed improvements on QoL |
| Greenfield et al., 2018 [27] | Evaluate race/ethnicity and racial/ethnicity group composition has moderators of MBRP; how the relationship between individual minority status vs. group composition can moderate treatment effects | Standard (8 sessions) | 16 h | 120 min | Clinical psychologists in a doctoral training program with master degree | No co-intervention | Relapse prevention (RP) | 12th month | MBRP showed better results in both white and racial/ethnic minorities in substance use; MBRP white group showed a significant reduction on heavy drinking days at 12 months; minorities in the MBRP group showed a significant reduction in drug use days at 12 months |
| Zgierska, Shapiro, Burzinski, Lerner, and Goodman-Strenski, (2017) [20] | Describe the implementation and findings related to fidelity monitoring of MBRP | MBRP-A (8 sessions) | 16 h | 120 min | Trained therapists in Mindfulness Meditation (MM) | Usual-Care (comparator) | Usual-Care | 26th week | Participants revealed overall satisfaction with the intervention, classifying it as helpful for their disorder |
| Yaghubi, Zargar, and Akbari, 2017 [32] | Compare the effectives of MBRP vs. TAU on impulsivity and relapse | Standard (8 sessions) | 16 h | 120 min | Clinical Psychologist | No co-intervention | TAU | 2nd month | MBRP showed significant reductions on impulsivity levels and on the probability of relapse |
| Zullig et al., 2018 [30] | Compare the effectiveness of MBRP in an outpatient setting | Standard (8 sessions) | 16 h | 120 min | NP | Medication-assisted treatment (MAT) | MAT | No follow-up | MBRP showed significant reductions in depression |
| Glasner, 2017 [26] | Investigate the efficacy and outcomes of MBRP in comparison to a health education (HE) control | MBRP modified version (8 sessions) | 10 h | 75 min | Therapist with certified mindfulness course | Contingency Management (CM) | HE + CM | 1st month | MBRP has demonstrated significant results in improving depressive symptoms and general psychiatric severity |
| Zemestani and Ottaviani, 2016 [34] | Examine the efficacy of MBRP vs. TAU in reducing cravings and depressive, anxious symptomatology | Standard | 16 h | 120 min | Clinical Psychologist with PhD | No co-intervention | TAU | 2nd month | MBRP showed significant results in reducing depression, cravings, and anxiety |
| Biseul, Icick, Seguin, Bellivier, and Scott, 2017 [35] | Evaluate the feasibility and acceptability of HABIT (CBT + MBRP) | Standard | 16 h | 120 min | Psychologist trained in MBCT | Cognitive Behavioural therapy (CBT) | No-comparator | After intervention | HABIT showed significant results in reducing depressive symptoms and substance misuse |
References
- United Nations Office on Drugs and Crime. (n.d.) World Drug Report 2019: 35 million People Worldwide Suffer from Drug Use Disorders While Only 1 in 7 People Receive Treatment. Available online: https://www.unodc.org/unodc/en/frontpage/2019/June/world-drug-report-2019_-35-million-people-worldwide-suffer-from-drug-use-disorders-while-only-1-in-7-people-receive-treatment.html (accessed on 5 August 2021).
- Mayo Clinic. Drug Addiction (Substance Use Disorder). 2017. Available online: https://www.mayoclinic.org/diseases-conditions/drug-addiction/symptoms-causes/syc-20365112?p=1 (accessed on 8 August 2021).
- Volkow, N.D.; Michaelides, M.; Baler, R. The neuroscience of drug reward and addiction. Physiol. Rev. 2019, 99, 2115–2140. [Google Scholar] [CrossRef] [PubMed]
- DSM 5 Criteria for Substance Use Disorders. Available online: https://www.verywellmind.com/dsm-5-criteria-for-substance-use-disorders-21926 (accessed on 5 August 2021).
- McNeely, J.; Troxel, A.B.; Kunins, H.V.; Shelley, D.; Lee, J.D.; Walley, A.; Weinstein, Z.M.; Billings, J.; Davis, N.J.; Marcello, R.K.; et al. Study protocol for a pragmatic trial of the Consult for Addiction Treatment and Care in Hospitals (CATCH) model for engaging patients in opioid use disorder treatment. Addict. Sci. Clin. Pract. 2019, 14, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tai, B.; Volkow, N.D. Treatment for Substance Use Disorder: Opportunities and Challenges under the Affordable Care. Act. Soc. Work Public Health 2013, 28, 165–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brandon, T.H.; Vidrine, J.I.; Litvin, E.B. Relapse and relapse prevention. Annu. Rev. Clin. Psychol. 2007, 3, 257–284. [Google Scholar] [CrossRef] [PubMed]
- Marlatt, G.A.; Donovan, D.M. (Eds.) Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors, 2nd ed.; The Guilford Press: New York, NY, USA, 2005. [Google Scholar]
- Li, W.; Howard, M.O.; Garland, E.L.; McGovern, P.; Lazar, M. Mindfulness treatment for substance misuse: A systematic review and meta-analysis. J. Subst. Abus. Treat. 2017, 75, 62–96. [Google Scholar] [CrossRef] [PubMed]
- Priddy, S.E.; Howard, M.O.; Hanley, A.W.; Riquino, M.R.; Friberg-Felsted, K.; Garland, E.L. Mindfulness meditation in the treatment of substance use disorders and preventing future relapse: Neurocognitive mechanisms and clinical implications. Subst. Abus. Rehabil. 2018, 9, 103–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khanna, S.; Greeson, J.M. A narrative review of yoga and mindfulness as complementary therapies for addiction. Complement. Ther. Med. 2013, 21, 244–252. [Google Scholar] [CrossRef] [Green Version]
- Crane, R.S.; Brewer, J.; Feldman, C.; Kabat-Zinn, J.; Santorelli, S.; Williams, J.M.G.; Kuyken, W. What defines mindfulness-based programs? The warp and the weft. Psychol. Med. 2017, 47, 990–999. [Google Scholar] [CrossRef] [Green Version]
- Holas, P.; Draps, M.; Kowalewska, E.; Lewczuk, K.; Gola, M. A pilot study of mindfulness-based relapse prevention for compulsive sexual behaviour disorder. J. Behav. Addict. 2020, 9, 1088–1092. [Google Scholar] [CrossRef]
- Garland, E.L.; Howard, M.O. Mindfulness-based treatment of addiction: Current state of the field and envisioning the next wave of research. Addict. Sci. Clin. Pract. 2018, 13, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Witkiewitz, K.; Bowen, S.; Douglas, H.; Hsu, S.H. Mindfulness-based relapse prevention for substance craving. Addict. Behav. 2013, 38, 1563–1571. [Google Scholar] [CrossRef] [Green Version]
- Bowen, S.; Witkiewitz, K.; Clifasefi, S.L.; Grow, J.; Chawla, N.; Hsu, S.H.; Carroll, H.A.; Harrop, E.; Collins, S.E.; Lustyk, M.K.; et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders. JAMA Psychiatry 2014, 71, 547–556. [Google Scholar] [CrossRef]
- Penberthy, J.K.; Konig, A.; Gioia, C.J.; Rodríguez, V.M.; Starr, J.A.; Meese, W.; Worthington-Stoneman, D.; Kersting, K.; Natanya, E. Mindfulness-based relapse prevention: History, mechanisms of action, and effects. Mindfulness 2015, 6, 151–158. [Google Scholar] [CrossRef]
- Weber, B.; Sala, L.; Gex-Fabry, M.; Docteur, A.; Gorwood, P.; Cordera, P.; Bondolfi, G.; Jermann, F.; Aubry, J.M.; Mirabel-Sarron, C. Self-reported long-term benefits of mindfulness-based cognitive therapy in patients with bipolar disorder. J. Altern. Complement. Med. 2017, 23, 534–540. [Google Scholar] [CrossRef]
- Witkiewitz, K.; Stein, E.R.; Votaw, V.R.; Wilson, A.D.; Roos, C.R.; Gallegos, S.J.; Clark, V.P.; Claus, E.D. Mindfulness-Based Relapse Prevention and Transcranial Direct Current Stimulation to Reduce Heavy Drinking: A Double-Blind Sham-Controlled Randomized Trial. Alcohol Clin. Exp. Res. 2019, 43, 1296–1307. [Google Scholar] [CrossRef]
- Zgierska, A.E.; Shapiro, J.; Burzinski, C.A.; Lerner, F.; Goodman-Strenski, V. Maintaining Treatment Fidelity of Mindfulness-Based Relapse Prevention Intervention for Alcohol Dependence: A Randomized Controlled Trial Experience. Evid Based Complement. Altern. Med. 2017, 2017, 9716586. [Google Scholar] [CrossRef] [Green Version]
- Bowen, S.; Chawla, N.; Collins, S.E.; Witkiewitz, K.; Hsu, S.; Grow, J.; Clifasefi, S.; Garner, M.; Douglass, A.; Larimer, M.E.; et al. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Subst. Abus. 2009, 30, 295–305. [Google Scholar] [CrossRef]
- Von Hammerstein, C.; Khazaal, Y.; Dupuis, M.; Aubin, H.J.; Benyamina, A.; Luquiens, A.; Romo, L. Feasibility, acceptability and preliminary outcomes of a mindfulness-based relapse prevention program in a naturalistic setting among treatment-seeking patients with alcohol use disorder: A prospective observational study. BMJ Open 2019, 95, e026839. [Google Scholar] [CrossRef]
- Grant, S.; Colaiaco, B.; Motala, A.; Shanman, R.; Booth, M.; Sorbero, M.; Hempel, S. Mindfulness-based Relapse Prevention for Substance Use Disorders: A Systematic Review and Meta-analysis. J. Addict. Med. 2017, 11, 386–396. [Google Scholar] [CrossRef] [Green Version]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Livingston, J.D.; Milne, T.; Fang, M.L.; Amari, E. The effectiveness of interventions for reducing stigma related to substance use disorders: A systematic review. Addiction 2012, 107, 39–50. [Google Scholar] [CrossRef] [Green Version]
- Glasner, S.; Mooney, L.J.; Ang, A.; Garneau, H.C.; Hartwell, E.; Brecht, M.L.; Rawson, R.A. Mindfulness-Based Relapse Prevention for Stimulant Dependent Adults: A Pilot Randomized Clinical Trial. Mindfulness 2017, 8, 126–135. [Google Scholar] [CrossRef]
- Greenfield, B.L.; Roos, C.; Hagler, K.J.; Stein, E.; Bowen, S.; Witkiewitz, K.A. Race/ethnicity and racial group composition moderate the effectiveness of mindfulness-based relapse prevention for substance use disorder. Addict. Behav. 2018, 81, 96–103. [Google Scholar] [CrossRef]
- Roos, C.; Bowen, S.; Witkiewitz, K. Approach Coping and Substance Use Outcomes Following Mindfulness-Based Relapse Prevention Among Individuals with Negative Affect Symptomatology. Mindfulness 2020, 11, 2397–2410. [Google Scholar] [CrossRef]
- Zgierska, A.E.; Burzinski, C.A.; Mundt, M.P.; McClintock, A.S.; Cox, J.; Coe, C.L.; Miller, M.M.; Fleming, M.F. Mindfulness-based relapse prevention for alcohol dependence: Findings from a randomized controlled trial. J. Subst. Abus. Treat. 2019, 100, 8–17. [Google Scholar] [CrossRef]
- Zullig, K.J.; Lander, L.R.; Sloan, S.; Brumage, M.R.; Hobbs, G.R.; Faulkenberry, L. Mindfulness-Based Relapse Prevention with Individuals Receiving Medication-Assisted Outpatient Treatment for Opioid Use Disorder. Mindfulness 2018, 9, 423–429. [Google Scholar] [CrossRef]
- Foroushani, N. The impact of mindfulness-based relapse prevention on craving, lapse and mindfulness fostering in addicted patients in Methadone Maintenance Treatment. Heroin Addict. Relat. Clin. Probl. 2019, 21, 33–40. [Google Scholar]
- Yaghubi, M.; Zargar, F.; Akbari, H. Comparing Effectiveness of Mindfulness-Based Relapse Prevention with Treatment as Usual on Impulsivity and Relapse for Methadone-Treated Patients: A Randomized Clinical Trial. Addict. Health 2017, 9, 156–165. [Google Scholar]
- Yaghubi, M.; Zargar, F. Effectiveness of Mindfulness-based Relapse Prevention on Quality of Life and Craving in Methadone-treated Patients: A Randomized Clinical Trial. Addict. Health 2018, 10, 250–259. [Google Scholar] [CrossRef]
- Zemestani, M.; Ottaviani, C. Effectiveness of Mindfulness-Based Relapse Prevention for Co-occurring Substance Use and Depression Disorders. Mindfulness 2016, 7, 1347–1355. [Google Scholar] [CrossRef]
- Biseul, I.; Icick, R.; Seguin, P.; Bellivier, F.; Scott, J. Feasibility and Acceptability of the ‘HABIT’ Group Programme for Comorbid Bipolar and Alcohol and Substance use Disorders. Clin. Psychol. Psychother. 2017, 24, 887–898. [Google Scholar] [CrossRef] [PubMed]
- Hölzel, B.K.; Lazar, S.W.; Gard, T.; Schuman-Olivier, Z.; Vago, D.R.; Ott, U. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect. Psychol. Sci. 2011, 6, 537–559. [Google Scholar] [CrossRef] [PubMed]
- Vago, D.R.; Silbersweig, D.A. Self-awareness, self-regulation, and self-transcendence (S-ART): A framework for understanding the neurobiological mechanisms of mindfulness. Front. Hum. Neurosci. 2012, 6, 296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiesa, A.; Serretti, A.; Jakobsen, J.C. Mindfulness: Top-down or bottom-up emotion regulation strategy? Clin. Psychol. Rev. 2013, 33, 82–96. [Google Scholar] [CrossRef]
- Grecucci, A.; Pappaianni, E.; Siugzdaite, R.; Theuninck, A.; Job, R. Mindful Emotion Regulation: Exploring the Neurocognitive Mechanisms behind Mindfulness. Biomed. Res. Int. 2015, 2015, 670724. [Google Scholar] [CrossRef] [Green Version]
- Riggs, N.R.; Greenberg, M.T.; Dvorakova, K. A Role for Mindfulness and Mindfulness Training in Substance Use Prevention. In Proceedings of the Third International Conference, MOD, Volterra, Italy, 10–13 September 2019; pp. 335–346. [Google Scholar] [CrossRef]
- Palazidou, E. The neurobiology of depression. Br. Med. Bull. 2012, 101, 127–145. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramadas, E.; Lima, M.P.d.; Caetano, T.; Lopes, J.; Dixe, M.d.A. Effectiveness of Mindfulness-Based Relapse Prevention in Individuals with Substance Use Disorders: A Systematic Review. Behav. Sci. 2021, 11, 133. https://doi.org/10.3390/bs11100133
Ramadas E, Lima MPd, Caetano T, Lopes J, Dixe MdA. Effectiveness of Mindfulness-Based Relapse Prevention in Individuals with Substance Use Disorders: A Systematic Review. Behavioral Sciences. 2021; 11(10):133. https://doi.org/10.3390/bs11100133
Chicago/Turabian StyleRamadas, Eduardo, Margarida Pedroso de Lima, Tânia Caetano, Jessica Lopes, and Maria dos Anjos Dixe. 2021. "Effectiveness of Mindfulness-Based Relapse Prevention in Individuals with Substance Use Disorders: A Systematic Review" Behavioral Sciences 11, no. 10: 133. https://doi.org/10.3390/bs11100133
APA StyleRamadas, E., Lima, M. P. d., Caetano, T., Lopes, J., & Dixe, M. d. A. (2021). Effectiveness of Mindfulness-Based Relapse Prevention in Individuals with Substance Use Disorders: A Systematic Review. Behavioral Sciences, 11(10), 133. https://doi.org/10.3390/bs11100133






