Abstract
(1) Background: As of 13 December 2020, Afghanistan reported around 48,952 confirmed COVID-19 cases and 1960 deaths. Lack of knowledge and perceptions among healthcare workers (HCWs) can pose challenges to disease control. Therefore, targeted, timely assessment of knowledge and perceptions are needed to address practices that might hinder efforts to stop the spreading of COVID-19 in Afghanistan. This study aimed to assess COVID-19-related knowledge, perceptions, and risk prevention practices (KPP) among frontline HCWs in Afghanistan; (2) Methods: A cross-sectional study was conducted with the support of field teams who were deployed in Afghanistan, surveyed from 14 to 22 April 2020 in eight provinces in Afghanistan with varying cumulative incidence of COVID-19 cases. A 28-item KPP survey instrument was adapted from other internationally validated questionnaires related to COVID-19. (3) Results: The survey was conducted among 213 frontline HCWs engaged in screening and treating COVID-19 patients. Survey results indicated that basic awareness of COVID-19 was 100% across all the participants. Knowledge and understanding of COVID-19 transmission, symptoms, incubation period and complications associated with COVID-19 are comprehensive and high (>90%), except available treatment for COVID-19 (84%). HCWs’ perceptions towards the prevention and control of COVID-19 were positive. However, only 63% believed that the use of N-95 face masks and disposable and fluid-resistant gowns (76%) could prevent COVID-19 transmission. This survey showed high knowledge and positive perception (72%), and only 48% of frontline HCWs had shown risk prevention practices. Addressing their perceptions and placing additional focus on practices across all health facilities is recommended as a preparedness measure.
1. Introduction
The ongoing global COVID-19 pandemic has been characterized as the global health crisis of our time and the most significant challenge we have faced since World War Two [1]. The first confirmed case in Afghanistan was a young man who came from Iran and was admitted to a government hospital in Herat following symptoms of fever, cough, and dyspnea on 22 February 2020 [2]. There have been 48,952 cumulative cases of COVID-19 as of 13 December 2020 [3]. The Capital City (Kabul) and the Western region (Herat province) of Afghanistan are the main areas of interest with high incidences of COVID-19 [4].
On 13 March 2020, the Afghanistan COVID-19 Emergency Response and Health Systems Preparedness projects were initiated to strengthen the national system for public health preparedness [5]. The overall project goals are for an emergency response to COVID-19, strengthening the healthcare capacity, mitigating social impact, implementing management and monitoring and evaluation of COVID-19 patients, and a contingent emergency response component (CERC) [5]. The Ministry of Public Health (MoPH), in collaboration with the World Health Organisation (WHO), has developed a COVID 19 Response Plan, and the World Bank approved $400 million to sustain Afghanistan’s reforms momentum to mitigate the COVID 19 crisis. The United Nations Office for the Coordination of Humanitarian Affairs (UNOCHA) launched the COVID-19 Multi-sectoral humanitarian country plan with an estimated $108.1 million appeal. Many international NGOs and United Nations (UN) agencies have responded to COVID 19 in the country [6].
The decades of war and political instability in Afghanistan have attenuated the healthcare capacity to detect and control the virus outbreak [7] rapidly. Healthcare workers (HCWs) of all levels are at the frontline of the COVID-19 pandemic response in screening and caring for the infected patients. The occupational risk of exposure to infected individuals and lack of protective measures may pose severe psychological distress; long working hours can lead to fatigue and occupational burnout [8]. A critical aspect of the COVID-19 response was to educate and engage the frontline HCWs in preventing transmission. However, the literature suggests that a poor understanding of the disease can delay the identification and spread of COVID-19 infection [9,10,11]. A study from Italy among the students from life sciences courses showed a higher awareness regarding the infection and the control measures [12]. Another study by Lahner et al. assessed the COVID-19 infection among the health workers in a teaching hospital and found a lower prevalence of COVID-19 than the general population and concluded that high awareness about COVID-19 is mandatory for all, especially for health workers, to safeguard their health and that of patients [13]. Indeed, HCWs’ personal beliefs and experiences can potentially influence patient care during the pandemic period. However, little is known about the personal protection practices such as gloves, surgical face masks, eye protection equipment, and regular hand hygiene activities among HCWs. Therefore, targeted, timely assessment of knowledge and perceptions are needed to address practices that might hinder efforts to stop the spreading of COVID-19 in Afghanistan. Thus, we aimed to assess COVID-19-related knowledge, perceptions, and risk reduction practices (KPP) among HCWs in Afghanistan.
2. Materials and Methods
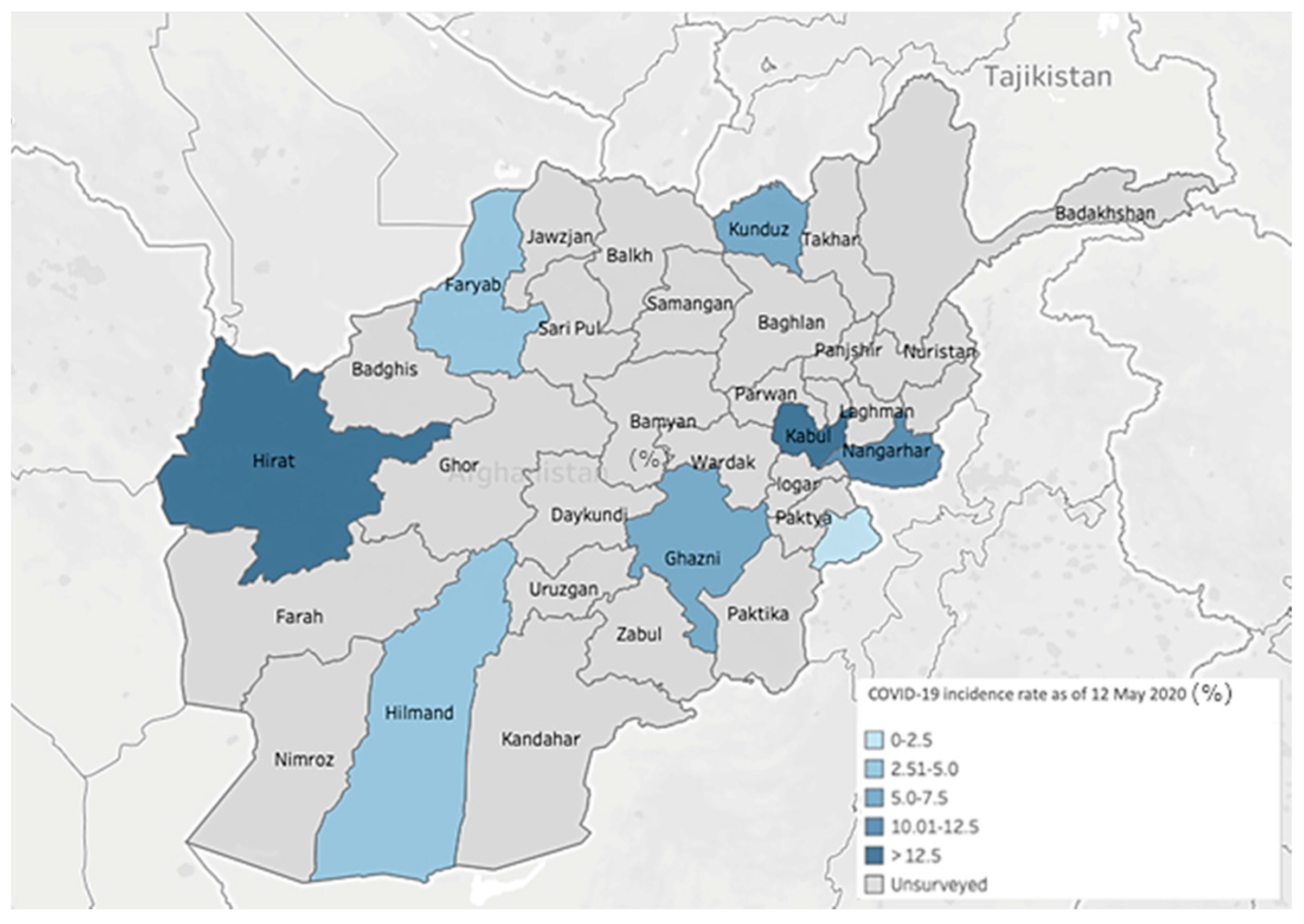
From 14–22 April 2020, a team of trained staff from The Johanniter International Assistance (JIA), in partnership with a locally trained staff of JIA’s partner NGOs, conducted a COVID-19 related KPP cross-sectional survey in eight provinces in Afghanistan (Faryab, Ghazni, Helmand, Herat, Kabul, Khost, Kunduz, and Nangarhar) with varying cumulative incidence of COVID-19 cases per 100,000 population (Figure 1). The selected provinces are stratified based on average incidence rates (12.5 cases) of COVID-19 per 100,000 Afghan population during April 2020. Two of the eight provinces, Herat, and Kabul had high cumulative incidences (≥12.5 cases per 100,000), and the other six provinces had low cumulative incidence rates of COVID-19 (<12.5 cases per 100,000 population). Herat and Kabul reported COVID-19 cases early in the outbreak (March 2020). In early April 2020, JIA and its partners have initiated provisional support to COVID-19-response activities across public health directorates across these eight provinces.
Figure 1.
Cumulative incidence of COVID-19 in the surveyed regions-Afghanistan, as of 12 May 2020.
The present KPP survey is a part of COVID-19 response and preparedness activities in Afghanistan. A snowball sampling design was used in the study by recruiting the frontline HCWs engaged in COVID-19-response activities. Survey areas were selected based on communities with a higher number of newly diagnosed COVID-19 cases and health facilities prepared for treating COVID-19 patients. Across eight provinces, more than 50 survey areas were identified.
Survey Instrument
The survey questionnaire was adopted from previous studies on the knowledge and perceptions of COVID-19 [9,10,11]. The authors included additional questions about the risk reduction practices of COVID-19 adopted from the WHO interim guidelines on risk assessment and management of COVID-19 [14]. The initial questionnaire was checked for clarity, wordiness, and double-ended questions and was validated for content and relevance by authors and subject experts (public health researchers) using face and content validation methods. The revised questionnaire was assessed for internal reliability, and consistency in a pilot tested on 20 randomly selected HCWs who were not included in the study. The questionnaire had a reliability correlation coefficient of ≥0.76. The internal consistency was assessed by calculating the Cronbach alpha of the knowledge section (0.813), perception section (0.763), and risk reduction practice (0.781) parts in this study.
The 28-item structured questionnaire consisted of questions that covered several areas: (1) sociodemographic data (3 items: age, gender, occupation); (2) source of information (4 statements/4-point Likert scale: 1-least used to 4-most used); (3) COVID-19 knowledge (7 multiple-choice questions designed to gauge HCWs understanding of COVID-19 symptoms (2 items), transmission (2 items), precautions and risk prevention (3 items)); (4) perceptions of COVID-19 (7 true/false items); (5) risk reduction practices such as the use of personal protective equipment (PPEs) at health facilities and screening sites of COVID-19 patients (7 items; yes/no questions).
Respondents were considered to have “good” knowledge if they provided “correct” responses to at least four of seven questions related to COVID-19 knowledge and “positive” perception if five out of seven statements are correct. Responses related to the use of risk reduction practices were considered high (≥6 of 7) and low (0–5).
Subject matter experts reviewed the survey’s content before it was administered and pilot-tested the surveys. Surveyors were instructed to share accurate information about COVID-19 after the survey. The field team approached the HCWs at their workplace, and telephone interviews were conducted among those working in high incidence areas. Surveys were identical for all survey regions and administered in the English language. High-level precautions were taken while conducting the survey when approaching HCWs at their workplace.
The collected responses were summarized by region, based on COVID-19 incidences (high (Herat and Kabul) versus low (Nangarha, Faryab, Ghazni, Helmand, Khost, and Kunduz)). Categorical variables were presented as absolute numbers and percentages. Continuous variables as mean ± standard deviations (SD) or median (range). To test the differences among the variables, we used the χ2 test, or Fisher’s exact test was used for categorical data. Wilcoxon ran-sum tests were used for ordinal data. Univariate analysis was performed to assess the differences between knowledge, perceptions, and practices among participants’ administrative region; 95% confidence intervals were generated for overall and regional data. Comparisons of survey responses of HCWs between COVID-19 regions described as high-incidence and low-incidence were conducted using the Chi-square (nominal/ordinal data) and Mann–Whitney (continuous variables) tests. We also calculated Cohen’s d, a standardized effect size estimation, by taking the differences between two means and dividing them by the pooled standard deviation of the two groups. The differences between the effect estimates were considered small when Cohen’s d score (between 0.20 and 0.49), medium (0.5–0.79), and large (≥0.80).
3. Results
Overall, there were 213 HCW respondents from eight provinces (Kabul (n = 33), Nangarhar (n = 27), 26 each from Faryab, Ghazni, Herat, Khost, and Kunduz, and Helmand (n = 23). Although no official records were kept, the average response rate was estimated at >90%, based on the field teams’ experience with the refusal rate of HCWs approached. Among all HCWs, 82 (38%) were women, between 26 and 40 years (51%). Around one-third of them are medical doctors and work in tertiary care hospitals (31%). Everyone (100%) reported that they had heard of COVID-19 before the KPP survey questions about COVID-19 were administered. The summary of respondents’ sociodemographic characteristics is presented in Table 1.

Table 1.
Sociodemographic characteristics of healthcare workers surveyed on COVID-19 in Afghanistan.
3.1. Knowledge of COVID-19 Cause, Transmission, Signs, and Symptoms
Most of the HCWs from high incidence COVID-19-affected regions (Herat and Kabul) and also the Southern region (Helmand) showed a higher level of knowledge levels than those from the East (Khost and Nangarhar) and Northern region (Faryab and Kunduz) (Table 2). Overall, 67% (95% CI: 60.3–73%, p = 0.002) of the HCWs perceived the cause/origin of COVID-19 to be bats. Most HCWs knew that COVID-19 is transmitted by contact, air, and fecal-oral routes (91%, p = 0.003). Concerning symptoms, 97% of respondents were aware of headache, fever, cough, sore throat, and flu-like symptoms of COVID-19 infection and knew that COVID-19 symptom onset ranges from 2 to 14 days (97%, p < 0.007*), and also reported that COVID-19 could cause pneumonia, respiratory failure, and death. Knowledge about COVID-19 treatment and prevention was high among HCWs such that 84% of respondents expressed that currently, supportive care is the only available treatment for COVID-19.

Table 2.
Knowledge, perception, and practices related to COVID-19 in healthcare workers in Afghanistan (n = 213).
3.2. Source of Receiving COVID-19-Related Information
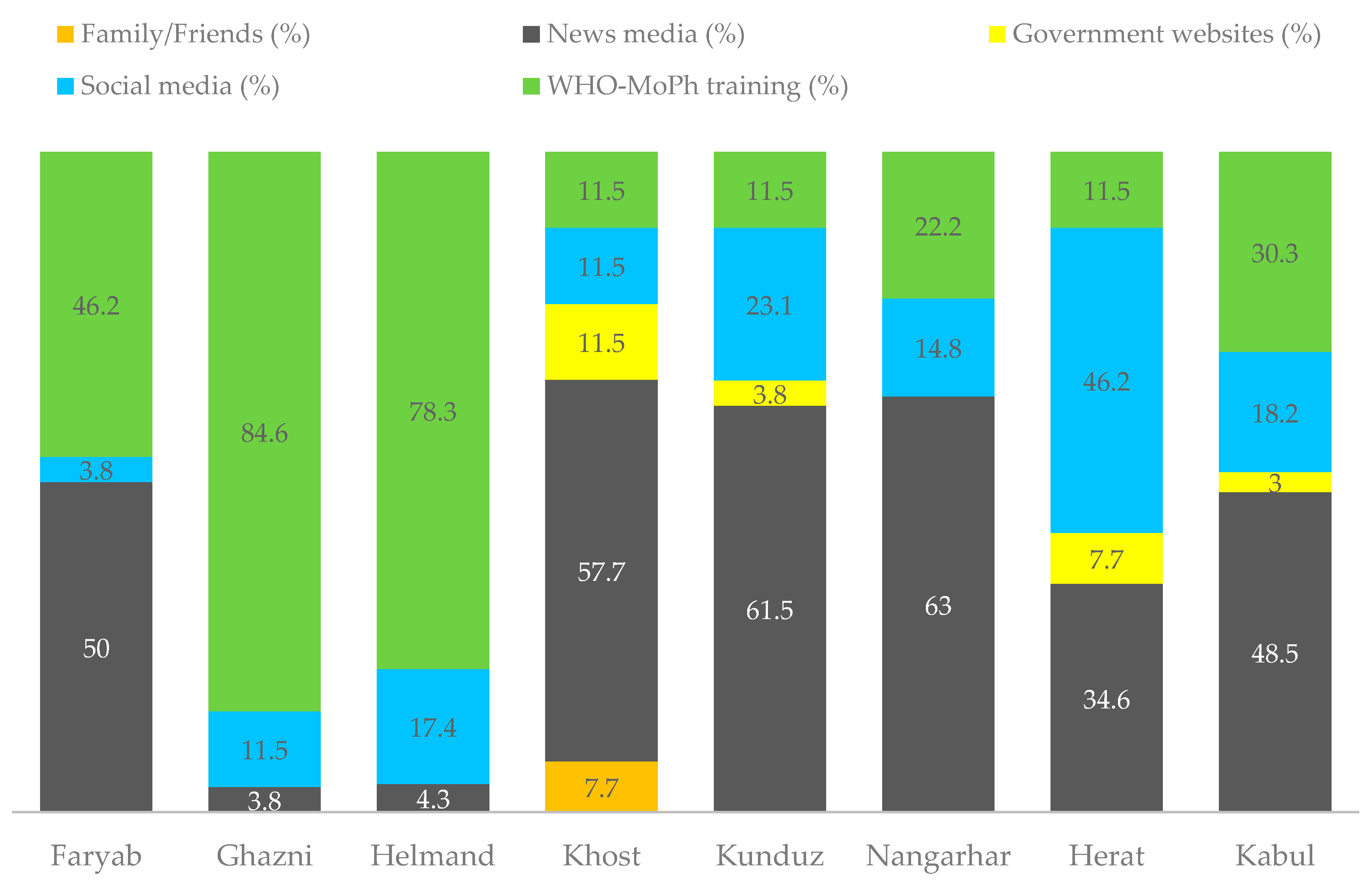
Training from WHO and MoPH was the primary COVID-19 information channel mentioned by HCWs from Ghazni (84.6%) and Helmand (78.3%) region. The most trusted information source on COVID-19 was the news media in Nangarhar (63%), Kunduz (61.5%), Khost (57.7%), Faryab (50%), and Kabul (48.5%). However, social media is the major source of information in Herat (46.2%) (Figure 2).
Figure 2.
Source of receiving COVID-19-related information.
3.3. Perception of COVID-19 Risk and Prevention
Overall, >90% of HCWs reported that COVID-19 is not fatal (98%), patients should report their travel history first (96%), symptoms appear in 2–14 days (94%), and the flu vaccine is not sufficient for prevention of COVID-19. A vast majority of the respondents also expressed that eating well-cooked meat is safe (89%), and equipment used in the wet market should be disinfected every day (90%). Besides, almost all agreed (99%) that washing hands with soap and water can prevent transmission of COVID-19 (Table 2).
3.4. COVID-19-Related Risk Prevention Practices
The majority of participants across all regions (95%) indicated that using gloves (98%), surgical face masks (98%), and regular hand hygiene (95%) practices can prevent the risk of COVID-19 transmission. However, only 63% believed that N-95 face masks and disposable and fluid-resistant gowns (76%) could prevent COVID-19 transmission (Table 2).
3.5. KPP in High and Low-Incidence Regions
The knowledge areas where high-incidence provinces scored lower were related to the questions of COVID-19 origin, its transmission, and treatment for COVID-19 patients (Table 3). More HCWs from low-incidence provinces believed that the COVID-19 originated from bats (80% versus 62%), and transmission (100% versus 87%), compared with those from high-incidence provinces. Among respondents from all eight provinces, >90% perceived that COVID-19 symptoms onset in 2–14 days, sick patients should share their recent travel history, and washing hands with soap can prevent COVID-19 transmission. However, respondents from low-incidence regions were not confident in their ability to identify that COVID-19 is not fatal (83%), the flu vaccine is ineffective (83%), and equipment used in the wet market should be disinfected (86%). One statistically significant difference in risk prevention practice between high-and low-incidence regions was use of eye protection glasses (79% (high-incidence) and 93% (low-incidence), p = 0.015) (Table 3).

Table 3.
Healthcare workers responses to knowledge, perception, and risk prevention practices based on COVID-19 incidences in Afghanistan (n = 213).
Overall, HCWs answered a median of 7 (4–7) of 7 COVID-19 knowledge questions correctly, with a slight variation in their knowledge levels between high-incidence regions (median= 7; range: 5–7) versus low-incidence regions (median= 6; range: 4–7). The correct responses for perceptions (median = 6 of 7 questions correctly; range = 4–7), and risk reduction practices (median = 5 of 7 questions correct; range: 0–7) were also moderate, and their scores differed slightly by region. The overall COVID-19-related knowledge was high (98.6%), with moderate perceptions (71.4%) and poor-risk prevention practices (48%) among HCWs, based on cut-off values in each section of the KPP survey. However, a considerable proportion of the frontline HCWs from high-incidence regions reported negative perceptions and poor-risk prevention practices (Table 4). We calculated a Cohen’s d of 0.280 (p = 0.076) for knowledge scores, 0.012 (p = 0.935) for perception scores, and 0.034 (p = 0.804) for risk perception practices to prevent COVID-19.

Table 4.
Summary results of the knowledge, perceptions, and practices survey—Afghanistan, 14–22 April 2020.
4. Discussion
The assessment was the first national-level quantitative evaluation of COVID-19-related knowledge, perceptions, and risk reduction practices among frontline HCWs during a period of ongoing COVID-19 transmission. Overall, COVID-19 knowledge was high, 72% had a positive perception, and only 48% had shown risk prevention practices, based on the correct responses for the 21 statements in the sections of the KPP survey. Simultaneously, this survey revealed several key areas of concern as Afghanistan has recorded a many COVID-19 cases and hundreds of frontline HCWs infected with COVID-19 [15]. Across all regions, HCWs were somewhat less able to correctly recognize the origins of the virus, recommended treatment for COVID-19, use of disposable fluid-resistant gowns, and N-95 face masks to reduce the risk of exposure from COVID-19 infection. The lack of recognition of the origin of COVID-19 might be partially explained by the fact that there is considerable debate on the origin of the causative agent. Given the similarity of SARS-CoV-2 to SARS-CoV, coronaviruses that are ~96% identical, it is likely that bats serve as reservoirs of COVID-19 [16,17]. Yet, questions about the origin of COVID-19 are still unclear. Besides, a quarter (22%) of the frontline HCWs from the low-incidence region and 13% from the high-incidence region believed that COVID-19 patients can be treated with antivirals and that there is a vaccine available. Currently, there is no validated treatment for COVID-19, although some drugs are under investigation and supportive treatment was the only strategy. The targeted educational messages state “that there is no standard treatment for COVID-19, and supportive treatment should be prioritized.” The WHO and MoPH guidelines say that all the frontline HCWs preparing to access suspected or confirmed COVID-19 patients should wear full PPE, including long-sleeved disposable gowns and N95 masks, to protect them against infection [18]. The passiveness risk prevention practices among HCWs in Afghanistan can be due to PPE shortage during the pandemic period. However, the current ongoing COVID-19 epidemic in Afghanistan reinforces the need to practice risk reduction practices among frontline HCWs.
Although we included various regions with low-and high-incidences of COVID-19, most participants in this geographically diverse sample understood the principal aspects of COVID-19 transmission, prevention, and risk reduction actions to reduce the risk of acquiring COVID-19. This indicates that frontline HCWs may use safe case management and practices to prevent the spreading of COVID-19 in Afghanistan. Regional variations in the epidemic and related response activities might have resulted in the regional differences in knowledge and perceptions, suggesting that targeting health communication at the district level might be more effective than a uniform, national approach. Underlying differences in the cultures, healthcare infrastructure, and education level across different HCWs might have contributed to regional variations in perceptions and behavior, especially regarding risk prevention practices.
The findings of this study have some limitations. First, the selection of HCWs within the regions was non-random; thus, mostly men and medical doctors participated in the survey. However, healthcare facilities were selected based on the MoPH approved centers for COVID-19 at the time. As a result, the survey covered areas with varying levels of COVID-19 incidence. Second, the survey was conducted during the ongoing epidemic; questions related to risk prevention practices were not validated. Second, a standardized questionnaire was used for the survey, but none of the responses was open-ended. Therefore, limited information was available beyond the binary yes/no or agree/disagree responses. Third, some participants might have provided socially desirable responses aligned to government recommendations rather than actual opinions. Fourth, the sample size was not calculated due to the adoption of a nonprobability sampling technique. Finally, due to physical distancing and some conflicting regions, we conducted our survey as a telephonic or in-person interview with the list of frontline HCWs provided by the MoPH. Thus, we cannot provide more information about the extent of training preparedness and response actions for COVID-19.
Despite these limitations, the data made it possible to generate preliminary findings that can be shared with several organizations in Afghanistan and the world within a few days of the COVID-19 epidemic. This information can guide the ongoing response and health communication efforts, which can contribute to controlling the epidemic. KPP surveys during an outbreak can provide valuable information for health communication efforts that can contribute to controlling the outbreak at its source, and thereby enhance COVID-19 containment efforts.
5. Conclusions
This survey, conducted at a time when case counts were rapidly increasing in Afghanistan, showed that COVID-19 knowledge among frontline HCWs was high, 72% had a positive perception, and only 48% had shown risk prevention practices. Addressing their perceptions and placing additional focus on practices across all health facilities is recommended as a preparedness measure.
Author Contributions
Conceptualization, V.R.R. and A.A.; methodology, A.S.B., V.R.R. and A.A.; software, A.S.B.; validation, A.A. and D.S.; formal analysis, A.S.B. and V.K.C.; investigation, A.S.B., A.A. and V.R.R.; resources, V.R.R.; data curation, D.S., A.A. and A.S.B.; writing—original draft preparation, A.S.B.; writing—review and editing, V.K.C.; supervision, V.R.R.; project administration, V.R.R. and A.A.; funding acquisition, V.R.R. All authors have read and agreed to the published version of the manuscript.
Funding
The project was supported by Johanniter International Assistance.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Johanniter International Assistance Research Committee (JUH-2020-002) on 14 March 2020.
Informed Consent Statement
Oral consent was obtained from the participants.
Data Availability Statement
Data is available on contacting the corresponding author or first authors requesting with valid reason.
Acknowledgments
The authors would like to thank Head of Desk and Director, The Johanniter International Assistance, its staff and partner NGOs’ staff for their excellent support in fulfilling the research work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- United Nations Development Programme. COVID-19 Pandemic, Humanity Needs Leadership and Solidarity to Defeat the Coronavirus. Available online: https://www.undp.org/content/undp/en/home/coronavirus.html (accessed on 24 May 2020).
- Mousavi, S.H.; Shah, J.; Giang, H.T.N.; Al-Ahdal, T.M.A.; Zahid, S.U.; Temory, F.; Paikan, F.M.; Karimzadeh, S.; Huy, N.T. The first COVID-19 case in Afghanistan acquired from Iran. Lancet Infect. Dis. 2020, 20, 657–658. [Google Scholar] [CrossRef]
- World Health Organization. Weekly Operational Update on COVID-19. Available online: https://covid19.who.int/region/emro/country/af (accessed on 14 December 2020).
- World Health Organization Coronavirus Disease (COVID-19) Situation Dashboard. Available online: https://covid19.who.int/region/emro/country/af.html (accessed on 24 May 2020).
- SEP Afghanistan COVID-19 Clean for Negs. Available online: https://moph.gov.af/sites/default/files/2020-03/SEP_Afghanistan%20COVID-19_clean_For%20Negs.pdf (accessed on 24 May 2020).
- COVID-19 Response across Afghanistan. Available online: http://www.emro.who.int/afg/afghanistan-news/covid-19-response-across-the-country-in-afghanistan.html (accessed on 24 April 2020).
- The Lancet. Peace and health in Afghanistan. Lancet 2020, 395, 921. [Google Scholar] [CrossRef]
- World Health Organisation Coronavirus Disease (COVID-19) Outbreak: Rights, Roles and Responsibilities of Health Workers, Including Key Considerations for Occupational Safety and Health. 2020. Available online: www.who.int/publications-detail/coronavirus-disease-(covid-19)-outbreak-rights-roles-and-responsibilities-of-health-workers-including-key-considerations-for-occupational-safety-and-health (accessed on 20 March 2020).
- Olum, R.; Chekwech, G.; Wekha, G.; Nassozi, D.R.; Bongomin, F. Coronavirus Disease-2019: Knowledge, Attitude, and Practices of Health Care Workers at Makerere University Teaching Hospitals, Uganda. Front. Public Health 2020, 8, 181. [Google Scholar] [CrossRef] [PubMed]
- Modi, P.D.; Nair, G.; Uppe, A.; Modi, J.; Tuppekar, B.; Gharpure, A.S.; Langade, D. COVID-19 Awareness among Healthcare Students and Professionals in Mumbai Metropolitan Region: A Questionnaire-Based Survey. Cureus 2020, 12, e7514. [Google Scholar] [CrossRef] [PubMed]
- Bhagavathula, A.S.; AlDhaleei, W.A.; Rahmani, J.; Mahabadi, M.A.; Bandari, D.K. Knowledge and Perceptions of COVID-19 among Health Care Workers: Cross-Sectional Study. JMIR Public Health Surveill. 2020, 6, e19160. [Google Scholar] [CrossRef] [PubMed]
- Gallé, F.; Sabella, E.A.; Da Molin, G.; De Giglio, O.; Caggiano, G.; Di Onofrio, V.; Ferracuti, S.; Montagna, M.T.; Liguori, G.; Orsi, G.B.; et al. Understanding Knowledge and Behaviors Related to CoViD–19 Epidemic in Italian Undergraduate Students: The EPICO Study. Int. J. Environ. Res. Public Health 2020, 17, 3481. [Google Scholar] [CrossRef] [PubMed]
- Lahner, E.; Dilaghi, E.; Prestigiacomo, C.; Alessio, G.; Marcellini, L.; Simmaco, M.; Santino, I.; Orsi, G.B.; Anibaldi, P.; Marcolongo, A.; et al. Prevalence of Sars-Cov-2 Infection in Health Workers (HWs) and Diagnostic Test Performance: The Experience of a Teaching Hospital in Central Italy. Int. J. Environ. Res. Public Health 2020, 17, 4417. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Risk Assessment and Management of Exposure of Health Care Workers in the Context of COVID-19: Interim Guidance, 19 March 2020. World Health Organization, 2020. Available online: https://apps.who.int/iris/handle/10665/331496 (accessed on 25 March 2020).
- Google News, Coronavirus (COVID-19) Afghanistan. Available online: https://news.google.com/covid19/map?hl=en-US&gl=US&ceid=US%3Aen&mid=%2Fm%2F02qzd9 (accessed on 25 May 2020).
- Medics Infected with Coronavirus in Western Afghanistan amid Iran Exodus. Available online: https://www.reuters.com/article/us-health-coronavirus-afghanistan/medics-infected-with-coronavirus-in-western-afghanistan-amid-iran-exodus.html (accessed on 28 April 2020).
- Andersen, K.G.; Rambaut, A.; Lipkin, W.I.; Holmes, E.C.; Garry, R.F. The proximal origin of SARS-CoV-2. Nat. Med. 2020, 26, 450–452. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19): Interim Guidance, 27 February 2020. World Health Organization. Available online: https://extranet.who.int/iris/restricted/handle/10665/331215 (accessed on 12 March 2020).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).