Serum Chloride Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Clinical Characteristics
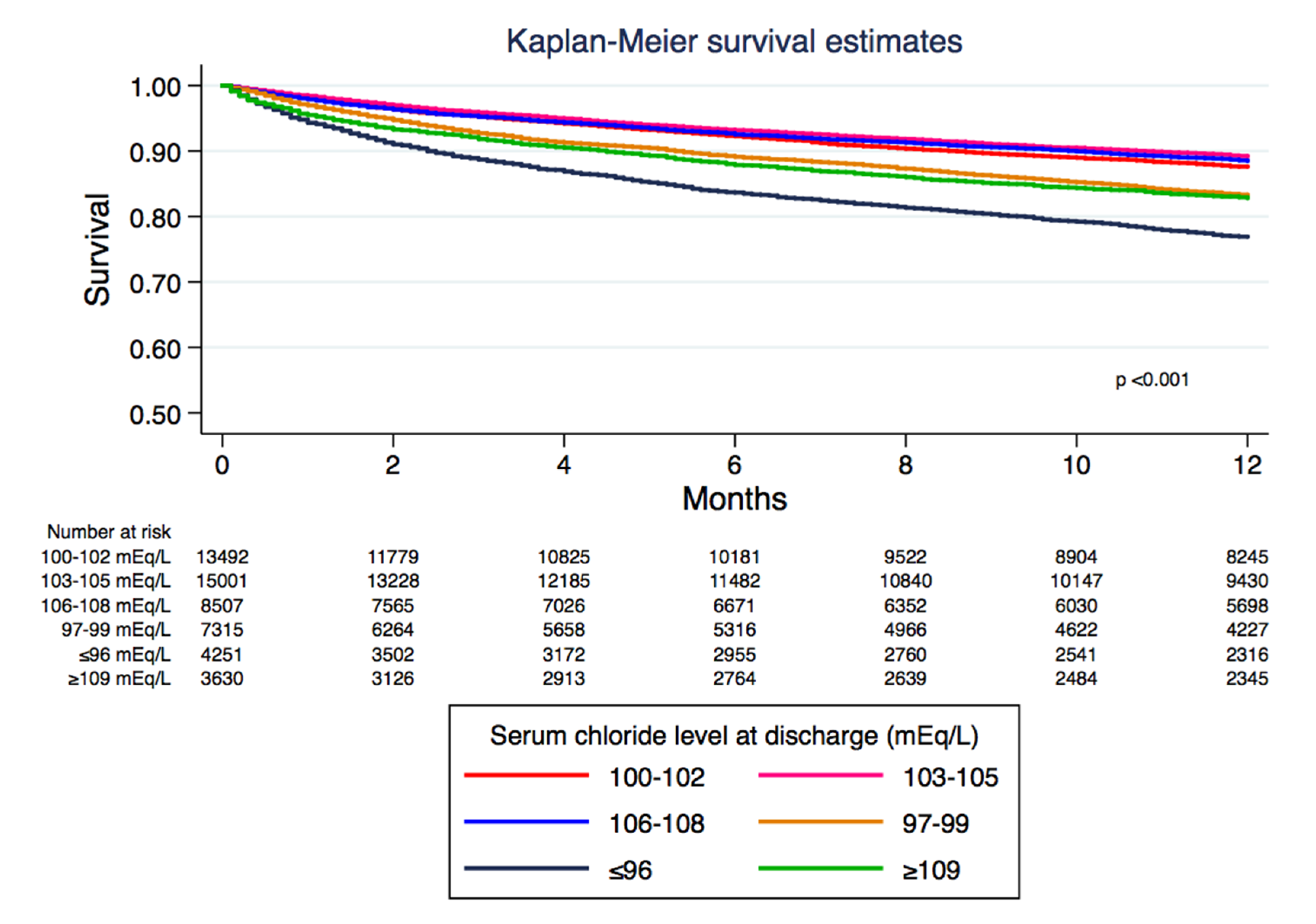
3.2. Discharge Serum Chloride and One-Year Mortality
3.3. Stratified Analysis Based on Admission Serum Chloride
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bandak, G.; Kashani, K.B. Chloride in intensive care units: A key electrolyte. F1000Research 2017, 6, 1930. [Google Scholar] [CrossRef] [PubMed]
- Pfortmueller, C.A.; Uehlinger, D.; Von Haehling, S.; Schefold, J.C. Serum chloride levels in critical illness-the hidden story. Intensive Care Med. Exp. 2018, 6, 10. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, A.H.; Cox, E.F.; Francis, S.T.; Lobo, D.N. A randomized, controlled, double-blind crossover study on the effects of 2-L infusions of 0.9% saline and plasma-lyte(R) 148 on renal blood flow velocity and renal cortical tissue perfusion in healthy volunteers. Ann. Surg. 2013, 258, 1118. [Google Scholar] [CrossRef]
- Wilcox, C.S. Regulation of Renal Blood Flow by Plasma Chloride. J. Clin. Investig. 1983, 71, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, C.S.; Peart, W.S. Release of renin and angiotensin II into plasma and lymph during hyperchloremia. Am. J. Physiol. 1987, 253, F734–F741. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-F.; Wang, J.-L.; Zhang, M.-Z.; McKanna, J.A.; Harris, R.C. Role of p38 in the regulation of renal cortical cyclooxygenase-2 expression by extracellular chloride. J. Clin. Investig. 2000, 106, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Huang, L.Y.; Zeng, D.Y.; Huang, E.W.; Liang, S.J.; Tang, Y.B.; Su, Y.X.; Tao, J.; Shang, F.; Wu, Q.Q.; et al. Decrease of intracellular chloride concentration promotes endothelial cell inflammation by activating nuclear factor-kB pathway. Hypertension 2012, 60, 1287–1293. [Google Scholar] [CrossRef]
- Shao, M.; Li, G.; Sarvottam, K.; Wang, S.; Thongprayoon, C.; Dong, Y.; Gajic, O.; Kashani, K. Dyschloremia Is a Risk Factor for the Development of Acute Kidney Injury in Critically Ill Patients. PLoS ONE 2016, 11, e0160322. [Google Scholar] [CrossRef]
- Suetrong, B.; Pisitsak, C.; Boyd, J.H.; Russell, J.A.; Walley, K.R. Hyperchloremia and moderate increase in serum chloride are associated with acute kidney injury in severe sepsis and septic shock patients. Crit. Care 2016, 20, 315. [Google Scholar] [CrossRef]
- Tani, M.; Morimatsu, H.; Takatsu, F.; Morita, K. The Incidence and Prognostic Value of Hypochloremia in Critically Ill Patients. Sci. World J. 2012, 2012, 474185–474187. [Google Scholar] [CrossRef]
- Thongprayoon, C.; Cheungpasitporn, W.; Cheng, Z.; Qian, Q. Chloride alterations in hospitalized patients: Prevalence and outcome significance. PLoS ONE 2017, 12, e0174430. [Google Scholar] [CrossRef] [PubMed]
- Boniatti, M.M.; Cardoso, P.R.; Castilho, R.K.; Vieira, S.R. Is hyperchloremia associated with mortality in critically ill patients? A prospective cohort study. J. Crit. Care 2011, 26, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Marttinen, M.; Wilkman, E.; Petäjä, L.; Suojaranta-Ylinen, R.; Pettilä, V.; Vaara, S.T. Association of plasma chloride values with acute kidney injury in the critically ill - a prospective observational study. Acta Anaesthesiol. Scand. 2016, 60, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Neyra, J.A.; Canepa-Escaro, F.; Li, X.; Manllo, J.; Adams-Huet, B.; Yee, J.; Yessayan, L. Acute Kidney Injury in Critical Illness Study Group Association of Hyperchloremia With Hospital Mortality in Critically Ill Septic Patients. Crit. Care Med. 2015, 43, 1938–1944. [Google Scholar] [CrossRef] [PubMed]
- Terzano, C.; Di Stefano, F.; Conti, V.; Di Nicola, M.; Paone, G.; Petroianni, A.; Ricci, A. Mixed Acid-Base Disorders, Hydroelectrolyte Imbalance and Lactate Production in Hypercapnic Respiratory Failure: The Role of Noninvasive Ventilation. PLoS ONE 2012, 7, e35245. [Google Scholar] [CrossRef]
- Zhang, Z.; Xu, X.; Fan, H.; Li, D.; Deng, H. Higher serum chloride concentrations are associated with acute kidney injury in unselected critically ill patients. BMC Nephrol. 2013, 14, 235. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A. Estimating GFR Using the CKD Epidemiology Collaboration (CKD-EPI) Creatinine Equation: More Accurate GFR Estimates, Lower CKD Prevalence Estimates, and Better Risk Predictions. Am. J. Kidney Dis. 2010, 55, 622–627. [Google Scholar] [CrossRef]
- Lee, J.Y.; Hong, T.H.; Lee, K.W.; Jung, M.J.; Gil Lee, J.; Lee, S.H. Hyperchloremia is associated with 30-day mortality in major trauma patients: A retrospective observational study. Scand. J. Trauma Resusc. Emerg. Med. 2016, 24, 117. [Google Scholar] [CrossRef]
- McClusky, S.; Karkouti, K.; Wijeysundera, D.N.; Minkovich, L.; Tait, G.; Beattie, W.S. Hyperchloremia After Noncardiac Surgery Is Independently Associated with Increased Morbidity and Mortality. Anesthesia Analg. 2013, 117, 412–421. [Google Scholar] [CrossRef]
- Sadan, O.; Singbartl, K.; Kandiah, P.A.; Martin, K.S.; Samuels, O.B. Hyperchloremia Is Associated With Acute Kidney Injury in Patients With Subarachnoid Hemorrhage. Crit. Care Med. 2017, 45, 1382–1388. [Google Scholar] [CrossRef]
- Bei, H.-Z.; You, S.-J.; Zheng, D.; Zhong, C.-K.; Du, H.-P.; Zhang, Y.; Lu, T.-S.; Cao, L.-D.; Dong, X.-F.; Cao, Y.-J.; et al. Prognostic role of hypochloremia in acute ischemic stroke patients. Acta Neurol. Scand. 2017, 136, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Kubota, K.; Sakaguchi, Y.; Hamano, T.; Oka, T.; Yamaguchi, S.; Shimada, K.; Matsumoto, A.; Hashimoto, N.; Mori, D.; Matsui, I.; et al. Prognostic value of hypochloremia versus hyponatremia among patients with chronic kidney disease—A retrospective cohort study. Nephrol. Dial. Transplant. 2018. [Google Scholar] [CrossRef]
- Ferreira, J.P.; Girerd, N.; Duarte, K.; Coiro, S.; McMurray, J.J.; Dargie, H.J.; Pitt, B.; Dickstein, K.; Testani, J.M.; Zannad, F.; et al. Serum Chloride and Sodium Interplay in Patients With Acute Myocardial Infarction and Heart Failure With Reduced Ejection Fraction. Circ. Heart Fail. 2017, 10, e003500. [Google Scholar] [CrossRef] [PubMed]
- Grodin, J.L.; Verbrugge, F.H.; Ellis, S.G.; Mullens, W.; Testani, J.M.; Tang, W.H.W. Importance of Abnormal Chloride Homeostasis in Stable Chronic Heart Failure. Circ. Heart Fail. 2016, 9, e002453. [Google Scholar] [CrossRef] [PubMed]
- McCallum, L.; Jeemon, P.; Hastie, C.E.; Patel, R.K.; Williamson, C.; Redzuan, A.M.; Dawson, J.; Sloan, W.; Muir, S.; Morrison, D.S.; et al. Serum Chloride Is an Independent Predictor of Mortality in Hypertensive Patients. Hypertension 2013, 62, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Hansrivijit, P.; Thirunavukkarasu, S.; Chewcharat, A.; Medaura, J.A.; Mao, A.; Kashani, K. Association of serum chloride level alterations with in-hospital mortality. Postgrad. Med. J. 2020. [Google Scholar] [CrossRef] [PubMed]

| Variables | All | Discharge Serum Chloride Level (mmoL/L) | p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| ≤96 | 97–99 | 100–102 | 103–105 | 106–108 | ≥109 | |||
| N | 56,907 | 5065 | 8017 | 14,576 | 16,204 | 9129 | 3916 | |
| Age (year) | 63 ± 17 | 67 ± 16 | 64 ± 17 | 62 ± 17 | 62 ± 17 | 63 ± 18 | 63 ± 18 | <0.001 |
| Male | 30,447 (54) | 2675 (53) | 4646 (58) | 8319 (57) | 8689 (54) | 4398 (48) | 1720 (44) | <0.001 |
| Caucasian | 52,947 (93) | 4736 (94) | 7493 (93) | 13,495 (93) | 15,096 (93) | 8509 (93) | 3618 (92) | 0.04 |
| eGFR (mL/min/1.73 m2) | 79 ± 28 | 72 ± 31 | 77 ± 30 | 81 ± 27 | 81 ± 27 | 79 ± 28 | 72 ± 31 | <0.001 |
| Principal Diagnosis | <0.001 | |||||||
| - Cardiovascular | 14,537 (26) | 1713 (34) | 2417 (30) | 4051 (28) | 4056 (25) | 1803 (20) | 497 (13) | |
| - Endocrine/Metabolic | 1677 (3) | 224 (4) | 212 (3) | 354 (2) | 411 (3) | 294 (3) | 182 (5) | |
| - Gastrointestinal | 5886 (10) | 384 (8) | 667 (8) | 1276 (9) | 1638 (10) | 1191 (13) | 730 (19) | |
| - Hematology/Oncology | 7686 (14) | 652 (13) | 1218 (15) | 2062 (14) | 2158 (13) | 1147 (13) | 449 (11) | |
| - Infectious Disease | 2097 (4) | 155 (3) | 230 (3) | 471 (3) | 532 (3) | 439 (5) | 270 (7) | |
| - Respiratory | 2595 (5) | 369 (7) | 469 (6) | 632 (4) | 662 (4) | 307 (3) | 156 (4) | |
| - Genitourinary | 1854 (3) | 119 (2) | 191 (2) | 334 (2) | 492 (3) | 393 (4) | 325 (8) | |
| - Injury/poisoning | 8737 (15) | 644 (13) | 1163 (15) | 2308 (16) | 2517 (16) | 1472 (16) | 633 (16) | |
| - Other | 11,838 (21) | 805 (16) | 1450 (18) | 3088 (21) | 3738 (23) | 2083 (23) | 674 (17) | |
| Charlson Score | 1.9 ± 2.4 | 2.4 ± 2.6 | 2.1 ± 2.5 | 1.9 ± 2.4 | 1.8 ± 2.3 | 1.9 ± 2.4 | 2.2 ± 2.5 | <0.001 |
| Comorbidities | ||||||||
| - Coronary artery disease | 4788 (8) | 566 (11) | 715 (9) | 1200 (8) | 1274 (8) | 724 (8) | 309 (8) | <0.001 |
| - Congestive heart failure | 4648 (8) | 792 (16) | 874 (11) | 1158 (8) | 1024 (6) | 528 (6) | 272 (7) | <0.001 |
| - Peripheral vascular disease | 2042 (4) | 268 (5) | 352 (4) | 513 (4) | 460 (3) | 302 (3) | 147 (4) | <0.001 |
| - Stroke | 4649 (8) | 516 (10) | 630 (8) | 1121 (8) | 1271 (8) | 764 (8) | 347 (9) | <0.001 |
| - Diabetes mellitus | 12,438 (22) | 1469 (29) | 2018 (25) | 3319 (23) | 3088 (19) | 1695 (19) | 849 (22) | <0.001 |
| - Chronic obstructive pulmonary disease | 5453 (10) | 832 (16) | 1016 (13) | 1327 (9) | 1300 (8) | 672 (7) | 306 (8) | <0.001 |
| - Cirrhosis | 1632 (3) | 171 (3) | 219 (2) | 373 (3) | 371 (2) | 303 (3) | 195 (5) | <0.001 |
| Acute myocardial infarction | 2762 (5) | 237 (5) | 342 (4) | 729 (5) | 887 (5) | 447 (5) | 120 (3) | <0.001 |
| Acute kidney injury | 8420 (15) | 1316 (26) | 1552 (19) | 2106 (14) | 1907 (12) | 998 (11) | 541 (14) | <0.001 |
| Renal replacement therapy | 1180 (2) | 379 (7) | 325 (4) | 248 (2) | 133 (1) | 51 (1) | 44 (1) | <0.001 |
| Mechanical ventilation | 9418 (17) | 1250 (25) | 1933 (24) | 2764 (19) | 2209 (14) | 921 (10) | 341 (9) | <0.001 |
| Vasopressor use | 5282 (9) | 832 (16) | 1113 (14) | 1496 (10) | 1147 (7) | 485 (5) | 209 (5) | <0.001 |
| Admission serum chloride (mmoL/L) | 103 ± 5 | 98 ± 7 | 101 ± 5 | 103 ± 5 | 104 ± 4 | 105 ± 4 | 107 ± 5 | <0.001 |
| Discharge serum sodium (mmoL/L) | 138 ± 3 | 134 ± 4 | 136 ± 3 | 138 ± 2 | 139 ± 2 | 141 ± 2 | 142 ± 3 | <0.001 |
| Discharge serum bicarbonate (mmoL/L) | 26 ± 3 | 29 ± 4 | 28 ± 3 | 27 ± 3 | 26 ± 3 | 25 ± 3 | 22 ± 3 | <0.001 |
| Discharge Serum Chloride (mmoL/L) | One-Year Mortality | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p | Adjusted HR * (95% CI) | p | ||
| ≤96 | 24.2% | 2.46 (2.26–2.66) | <0.001 | 1.94 (1.72–2.19) | <0.001 |
| 97–99 | 17.0% | 1.61 (1.49–1.75) | <0.001 | 1.45 (1.32–1.59) | <0.001 |
| 100–102 | 12.7% | 1.17 (1.08–1.25) | <0.001 | 1.07 (0.99–1.15) | 0.09 |
| 103–105 | 11.0% | 1 (ref) | - | 1 (ref) | - |
| 106–108 | 11.8% | 1.09 (0.99–1.18) | 0.06 | 1.01 (0.93–1.10) | 0.81 |
| ≥109 | 17.9% | 1.75 (1.59–1.92) | <0.001 | 1.41 (1.26–1.58) | <0.001 |
| Discharge Serum Chloride (mEq/L) | One-Year Mortality (%) | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|---|
| HR (95% CI) | p | Adjusted HR * (95% CI) | p | ||
| Admission serum chloride ≤99 mmoL/L | |||||
| ≤99 | 26.4% | 1.50 (1.38–1.64) | <0.001 | 1.25 (1.11–1.41) | <0.001 |
| 100–108 | 18.6% | 1 (ref) | - | 1 (ref) | - |
| ≥109 | 37.5% | 2.31 (1.82–2.92) | <0.001 | 2.06 (1.60–2.66) | <0.001 |
| Admission serum chloride 100–108 mmoL/L | |||||
| ≤99 | 15.1% | 1.43 (1.32–1.55) | <0.001 | 1.37 (1.23–1.52) | <0.001 |
| 100–108 | 10.9% | 1 (ref) | - | 1 (ref) | - |
| ≥109 | 16.1% | 1.58 (1.41–1.77) | <0.001 | 1.24 (1.09–1.42) | 0.002 |
| Admission serum chloride ≥109 mmoL/L | |||||
| ≤99 | 8.9% | 0.90 (0.67–1.17) | 0.45 | 1.32 (0.94–1.84) | 0.10 |
| 100–108 | 9.8% | 1 (ref) | - | 1 (ref) | - |
| ≥109 | 17.6% | 1.94 (1.62–2.32) | <0.001 | 1.10 (0.86–1.40) | 0.46 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petnak, T.; Thongprayoon, C.; Cheungpasitporn, W.; Bathini, T.; Vallabhajosyula, S.; Chewcharat, A.; Kashani, K. Serum Chloride Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients. Med. Sci. 2020, 8, 22. https://doi.org/10.3390/medsci8020022
Petnak T, Thongprayoon C, Cheungpasitporn W, Bathini T, Vallabhajosyula S, Chewcharat A, Kashani K. Serum Chloride Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients. Medical Sciences. 2020; 8(2):22. https://doi.org/10.3390/medsci8020022
Chicago/Turabian StylePetnak, Tananchai, Charat Thongprayoon, Wisit Cheungpasitporn, Tarun Bathini, Saraschandra Vallabhajosyula, Api Chewcharat, and Kianoush Kashani. 2020. "Serum Chloride Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients" Medical Sciences 8, no. 2: 22. https://doi.org/10.3390/medsci8020022
APA StylePetnak, T., Thongprayoon, C., Cheungpasitporn, W., Bathini, T., Vallabhajosyula, S., Chewcharat, A., & Kashani, K. (2020). Serum Chloride Levels at Hospital Discharge and One-Year Mortality among Hospitalized Patients. Medical Sciences, 8(2), 22. https://doi.org/10.3390/medsci8020022







