Assessment of Oral Hygiene Behavioral and Demographic Risk Factors for Extrahepatic Manifestations of Hepatitis C
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Patients Examination
2.3. Statistical Analysis
3. Results
3.1. General Characteristics of Study Participants
3.2. Prevalence of Oral Hygiene Habits in Patients with EHC Manifestations
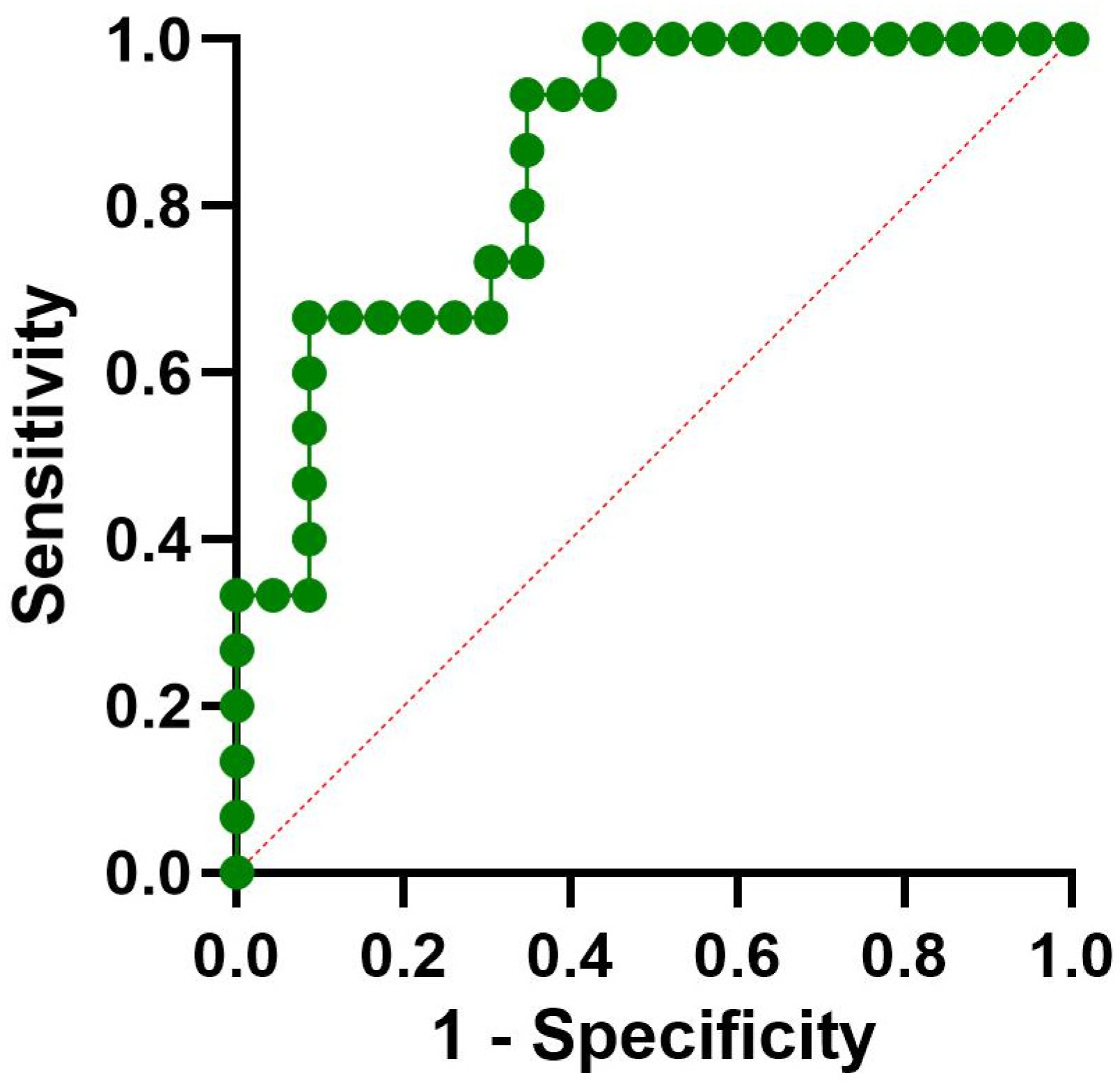
3.3. Logistic Regression for OLP
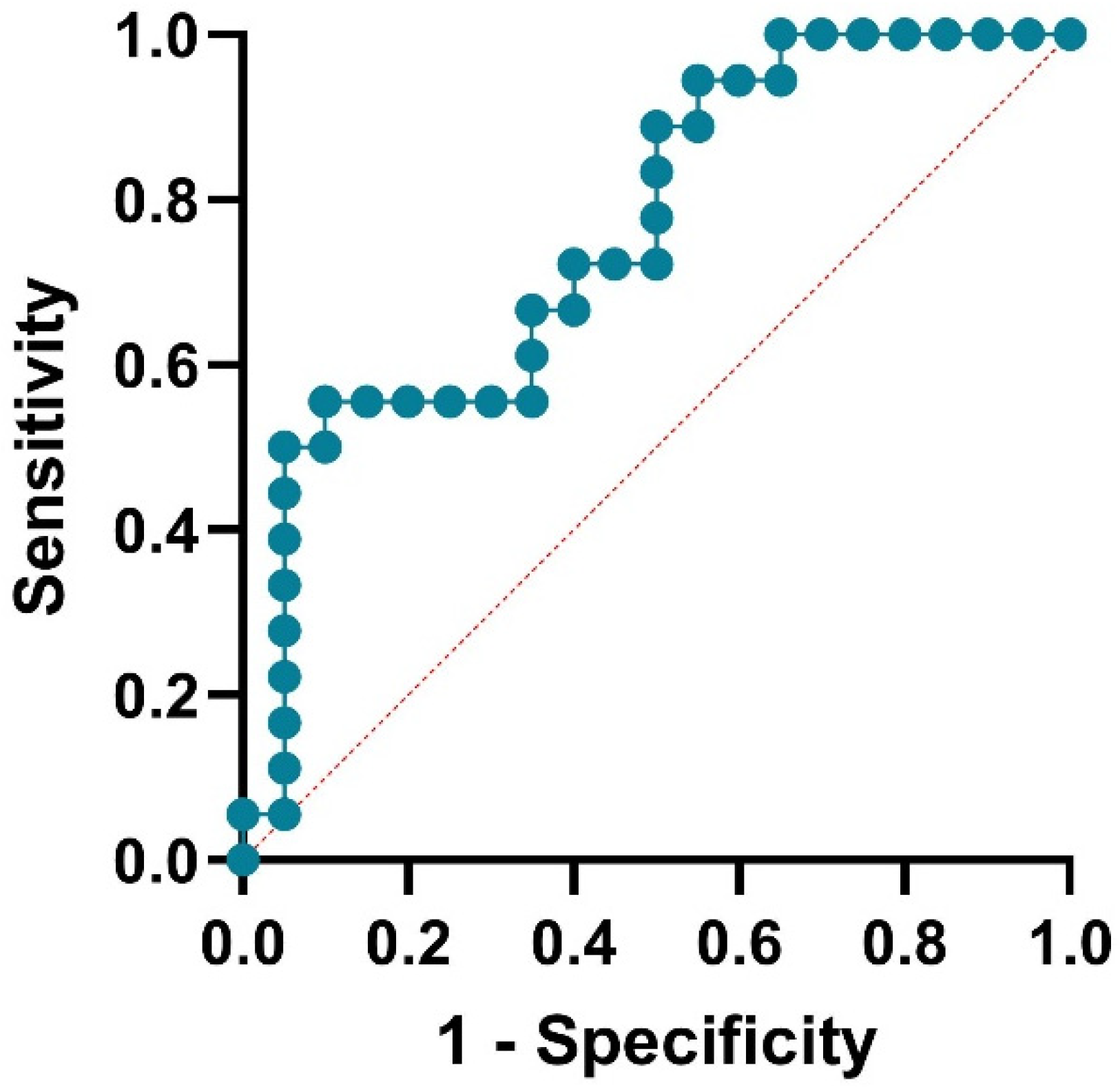
3.4. Logistic Regression for Xerostomia
3.5. Logistic Regression for Sjögren Syndrome-like
3.6. Alluvial Diagram Analysis for OLP, Xerostomia, and Sjögren Syndrome-like
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Hepatitis. Available online: https://www.who.int/data/gho/data/themes/chronic-viral-hepatitis (accessed on 1 October 2025).
- Huiban, L.; Stanciu, C.; Muzica, C.M.; Cuciureanu, T.; Chiriac, S.; Zenovia, S.; Burduloi, V.M.; Petrea, O.; Sîngeap, A.M.; Gîrleanu, I.; et al. Hepatitis C Virus Prevalence and Risk Factors in a Village in Northeastern Romania—A Population-Based Screening—The First Step to Viral Micro-Elimination. Healthcare 2021, 9, 651. [Google Scholar] [CrossRef] [PubMed]
- Goto, K.; Roca Suarez, A.A.; Wrensch, F.; Baumert, T.F.; Lupberger, J. Hepatitis C Virus and Hepatocellular Carcinoma: When the Host Loses Its Grip. Int. J. Mol. Sci. 2020, 21, 3057. [Google Scholar] [CrossRef]
- Di Stasio, D.; Guida, A.; Romano, A.; Petruzzi, M.; Marrone, A.; Fiori, F.; Lucchese, A. Hepatitis C Virus (HCV) Infection: Pathogenesis, Oral Manifestations, and the Role of Direct-Acting Antiviral Therapy—A Narrative Review. J. Clin. Med. 2024, 13, 4012. [Google Scholar] [CrossRef]
- Nagao, Y.; Hanada, S.; Shishido, S.; Ide, T.; Kumashiro, R.; Ueno, T.; Sata, M. Incidence of Sjögren’s Syndrome in Japanese Patients with Hepatitis C Virus Infection. J. Gastroenterol. Hepatol. 2003, 18, 258–266. [Google Scholar] [CrossRef]
- World Health Organization. Number of Persons Living with Chronic Hepatitis. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/hepatitis---number-of-persons-living-with-chronic-hepatitis (accessed on 2 October 2025).
- World Health Organization. Prevalence of Chronic Hepatitis Among the General Population. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/hepatitis---prevalence-of-chronic-hepatitis-among-the-general-population (accessed on 2 October 2025).
- García-Pola, M.; Rodríguez-Fonseca, L.; Suárez-Fernández, C.; Sanjuán-Pardavila, R.; Seoane-Romero, J.; Rodríguez-López, S. Bidirectional Association between Lichen Planus and Hepatitis C—An Updated Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 5777. [Google Scholar] [CrossRef]
- Millsop, J.W.; Wang, E.A.; Fazel, N. Etiology, Evaluation, and Management of Xerostomia. Clin. Dermatol. 2017, 35, 468–476. [Google Scholar] [CrossRef]
- Nawito, Z.; Amin, A.; El-Fadl, S.A.; Abu El-Einen, K. Sicca Complex among Egyptian Patients with Chronic Hepatitis C Virus Infection. Clin. Rheumatol. 2011, 30, 1299–1304. [Google Scholar] [CrossRef]
- Di Stasio, D.; Lucchese, A.; Romano, A.; Adinolfi, L.E.; Serpico, R.; Marrone, A. The Clinical Impact of Direct-Acting Antiviral Treatment on Patients Affected by Hepatitis C Virus-Related Oral Lichen Planus: A Cohort Study. Clin. Oral Investig. 2022, 26, 5409–5417. [Google Scholar] [CrossRef]
- Mariette, X.; Criswell, L.A. Primary Sjögren’s Syndrome. N. Engl. J. Med. 2018, 378, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Shiboski, C.H.; Shiboski, S.C.; Seror, R.; Criswell, L.A.; Labetoulle, M.; Lietman, T.M.; Rasmussen, A.; Scofield, H.; Vitali, C.; Bowman, S.J. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren’s Syndrome: A Consensus and Data-Driven Methodology Involving Three International Patient Cohorts. Arthritis Rheumatol. 2017, 69, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.O.; Beach, M.E.; Wang, Y.; Perez, P.; Yin, H.; Pelayo, E.; Fowler, S.; Alevizos, I.; Grisius, M.; Baer, A.N.; et al. HCV Infection Alters Salivary Gland Histology and Saliva Composition. J. Dent. Res. 2022, 101, 534–541. [Google Scholar] [CrossRef] [PubMed]
- European Commission. National Low-Risk Drinking Recommendations (Drinking Guidelines). Available online: https://knowledge4policy.ec.europa.eu/health-promotion-knowledge-gateway/national-low-risk-drinking-recommendations-drinking-guidelines_en (accessed on 2 October 2025).
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Periodontol. 2018, 89 (Suppl. S1), S159–S172, Erratum in: J. Periodontol. 2018, 89, 1475. [Google Scholar] [CrossRef]
- Abdel-Gawad, M.; Nour, M.; El-Raey, F.; Nagdy, H.; Almansoury, Y.; El-Kassas, M. Gender Differences in Prevalence of Hepatitis C Virus Infection in Egypt: A Systematic Review and Meta-Analysis. Sci. Rep. 2023, 13, 2499. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Hepatitis C—Annual Epidemiological Report for 2022. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/HEPC_AER_2022.pdf (accessed on 2 October 2025).
- Jin, F.; Dore, G.J.; Matthews, G.; Luhmann, N.; Macdonald, V.; Bajis, S.; Baggaley, R.; Mathers, B.; Verster, A.; Grulich, A.E. Prevalence and Incidence of Hepatitis C Virus Infection in Men Who Have Sex with Men: A Systematic Review and Meta-Analysis. Lancet Gastroenterol. Hepatol. 2021, 6, 39–56. [Google Scholar] [CrossRef]
- Adolfsson, A.; Lener, F.; Marklund, B.; Mossberg, K.; Cevik-Aras, H. Prevalence of Dry Mouth in Adult Patients in Primary Health Care. Acta Odontol. Scand. 2022, 80, 605–610. [Google Scholar] [CrossRef]
- Guo, X.; Hou, L.; Peng, X.; Tang, F. The Prevalence of Xerostomia among E-Cigarette or Combustible Tobacco Users: A Systematic Review and Meta-Analysis. Tob. Induc. Dis. 2023, 21, 22. [Google Scholar] [PubMed]
- Brito-Zerón, P.; Retamozo, S.; Ramos-Casals, M. Sjögren Syndrome. Med. Clin. 2023, 160, 163–171. [Google Scholar] [CrossRef] [PubMed]
- El-Ghitany, E. Hepatitis C Virus Infection in Egypt: Current Situation and Future Perspective. J. High Inst. Public Health 2019, 49, 1–9. [Google Scholar] [CrossRef][Green Version]
- Ismail, R.M.; Elansary, A.R.; Ezzatt, O.M.; Hamed, M.G.; Gamil, Y. Hepatitis C-Associated Oral Lesions: A Hospital-Based Retrospective Case-Control Study in Egypt. J. Int. Oral Health 2023, 15, 52–58. [Google Scholar] [CrossRef]
- Nagao, Y.; Tsuji, M. Effects of Hepatitis C Virus Elimination by Direct-Acting Antiviral Agents on the Occurrence of Oral Lichen Planus and Periodontal Pathogen Load: A Preliminary Report. Int. J. Dent. 2021, 2021, 8925879. [Google Scholar] [CrossRef] [PubMed]
- Stone, S.J.; Heasman, P.A.; Staines, K.S.; McCracken, G.I. The impact of structured plaque control for patients with gingival manifestations of oral lichen planus: A randomized controlled study. J. Clin. Periodontol. 2015, 42, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Mergoni, G.; Magnani, V.; Goldoni, M.; Vescovi, P.; Manfredi, M. Effects of oral healthcare motivation in patients with gingival oral lichen planus: A randomized controlled trial. Oral Dis. 2019, 25, 1335–1343. [Google Scholar] [CrossRef] [PubMed]
- Stankeviciene, I.; Stangvaltaite-Mouhat, L.; Aleksejuniene, J.; Mieliauskaite, D.; Talijuniene, I.; Butrimiene, I.; Bendinskaite, R.; Puriene, A. Oral health status, related behaviours and perceived stress in xerostomia, Sicca and Sjögren’s syndromes patients—A cross-sectional study. BMC Oral Health 2024, 24, 454. [Google Scholar] [CrossRef] [PubMed]
- Attin, T.; Hornecker, E. Tooth brushing and oral health: How frequently and when should tooth brushing be performed? Oral Health Prev. Dent. 2005, 3, 135–140. [Google Scholar] [PubMed]
- Lertpimonchai, A.; Rattanasiri, S.; Arj-Ong Vallibhakara, S.; Attia, J.; Thakkinstian, A. The association between oral hygiene and periodontitis: A systematic review and meta-analysis. Int. Dent. J. 2017, 67, 332–343. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Albuquerque-Souza, E.; Sahingur, S.E. Periodontitis, Chronic Liver Diseases, and the Emerging Oral–Gut–Liver Axis. Periodontology 2000 2022, 89, 125–141. [Google Scholar] [CrossRef]


| Characteristics | Frequency N = 38 |
|---|---|
| Age, years mean ± standard deviation median (interquartile range) range | 56.47 ± 8.6 59.5 (52.5–63) 38–67 |
| Gender, male | 22 (57.9%) |
| Frequency of Dental Brushing | |
| Less than daily | 7 (18.4%) |
| Daily | 22 (57.9%) |
| Twice daily | 9 (23.7%) |
| Professional Dental Hygiene Visits | |
| Less than 6 months | 6 (15.8%) |
| At 1 year | 23 (60.5%) |
| More than 1 year | 9 (23.7%) |
| Smoking | |
| No | 10 (26.3%) |
| Less than 10 cigarettes/day | 16 (42.1%) |
| More than 10 cigarettes/day | 12 (31.6%) |
| OLP | 15 (39.5%) |
| Xerostomia | 18 (47.4%) |
| Sjögren syndrome-like | 6 (15.8%) |
| Predictors | Xerostomia | OLP | SS-like |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Frequency of Dental Brushing | |||
| Less daily | 6 (33.33) | 4 (26.66) | 2 (33.33) |
| Daily | 10 (55.55) | 9 (60) | 3 (50) |
| Twice daily | 2 (11.11) | 2 (13.33) | 1 (16.66) |
| Professional Dental Hygiene Visits | |||
| Less than 6 mo | 6 (33.33) | 5 (33.33) | 3 (50) |
| 1 year | 8 (44.44) | 9 (60) | 2 (33.33) |
| More 1 y | 4 (22.22) | 1 (6.66) | 1 (16.66) |
| Predictors | VIF (Multicollinearity) | OR (95% CI) | p-Value |
|---|---|---|---|
| Gender (female vs. male) | 1.354 | 10.61 (1.78–94.45) | 0.0086 |
| Age | 1.518 | 0.95 (0.84–1.06) | 0.3401 |
| Frequency of Dental Brushing | |||
| Daily vs. less than daily | 4.59 | 3.19 (0.1–118.5) | 0.5028 |
| Twice daily vs. less than daily | 4.24 | 2.56 (0.04–247.1) | 0.66 |
| Professional Dental Hygiene Visits | |||
| 1 year vs. less than 6 mo | 4.10 | 1.79 (0.02–211.4) | 0.7975 |
| More than 1 y vs. less than 6 mo | 2.05 | 3.07 (0.23–93.36) | 0.4148 |
| Smoking | |||
| Less 10 vs. More 10 | 3.23 | 0.24 (0.007–4.73) | 0.344 |
| No vs. More 10 | 2.44 | 0.15 (0.004–2.72) | 0.211 |
| Predictors | VIF (Multicollinearity) | OR (95% CI) | p-Value |
|---|---|---|---|
| Gender (female vs. male) | 1.354 | 2.18 (0.43–12.17) | 0.0345 |
| Age | 1.518 | 0.99 (0.89–1.12) | 0.989 |
| Frequency of Dental Brushing Daily vs. less than daily Twice daily vs. less than daily | 4.59 4.24 | 0.2 (0.004–4.96) 0.09 (0.001–3.46) | 0.331 0.21 |
| Professional Dental Hygiene Visits 1 year vs. less than 6 mo More than 1 y vs. less than 6 mo | 4.102 2.045 | 0.97 (0.03–30.29) 0.37 (0.04–2.89) | 0.99 0.34 |
| Smoking Less 10 vs. More 10 No vs. More 10 | 3.23 2.44 | 1.73 (0.14–28.14) 0.67 (0.05–10.60) | 0.057 0.36 |
| Predictors | VIF (Multicollinearity) | OR (95% CI) | p-Value |
|---|---|---|---|
| Gender (female vs. male) | 1.204 | 0.49 (0.05–4.23) | 0.515 |
| Age | 1.286 | 1.101 (0.98–1.26) | 0.103 |
| Frequency of Dental Brushing | |||
| Daily vs. less than daily | 2.323 | 0.948 (0.068–10.58) | 0.966 |
| Twice daily vs. less than daily | 2.254 | 1.094 (0.042–38.28) | 0.956 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oprea, M.; Cândea, A.; Roman, A.; Rogoveanu, I.; Pitru, A.R.; Ionele, C.M.; Gheorghe, D.N.; Nicolae, F.M.; Popescu, D.M.; Turcu-Stiolica, A.; et al. Assessment of Oral Hygiene Behavioral and Demographic Risk Factors for Extrahepatic Manifestations of Hepatitis C. Med. Sci. 2025, 13, 298. https://doi.org/10.3390/medsci13040298
Oprea M, Cândea A, Roman A, Rogoveanu I, Pitru AR, Ionele CM, Gheorghe DN, Nicolae FM, Popescu DM, Turcu-Stiolica A, et al. Assessment of Oral Hygiene Behavioral and Demographic Risk Factors for Extrahepatic Manifestations of Hepatitis C. Medical Sciences. 2025; 13(4):298. https://doi.org/10.3390/medsci13040298
Chicago/Turabian StyleOprea, Mihai, Andreea Cândea, Alexandra Roman, Ion Rogoveanu, Allma Roxana Pitru, Claudiu Marinel Ionele, Dorin Nicolae Gheorghe, Flavia Mirela Nicolae, Dora Maria Popescu, Adina Turcu-Stiolica, and et al. 2025. "Assessment of Oral Hygiene Behavioral and Demographic Risk Factors for Extrahepatic Manifestations of Hepatitis C" Medical Sciences 13, no. 4: 298. https://doi.org/10.3390/medsci13040298
APA StyleOprea, M., Cândea, A., Roman, A., Rogoveanu, I., Pitru, A. R., Ionele, C. M., Gheorghe, D. N., Nicolae, F. M., Popescu, D. M., Turcu-Stiolica, A., Ciobanu, S., & Surlin, P. (2025). Assessment of Oral Hygiene Behavioral and Demographic Risk Factors for Extrahepatic Manifestations of Hepatitis C. Medical Sciences, 13(4), 298. https://doi.org/10.3390/medsci13040298










