Pediatric Medication Prescribing Across Urgent Care Visits: An Epidemiologic View from a Primary Care Setting in the Kingdom of Saudi Arabia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Ethical Considerations
2.3. Study Participants
2.4. Data Collection Tool
2.5. Data Management and Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics According to Medication Prescriptions
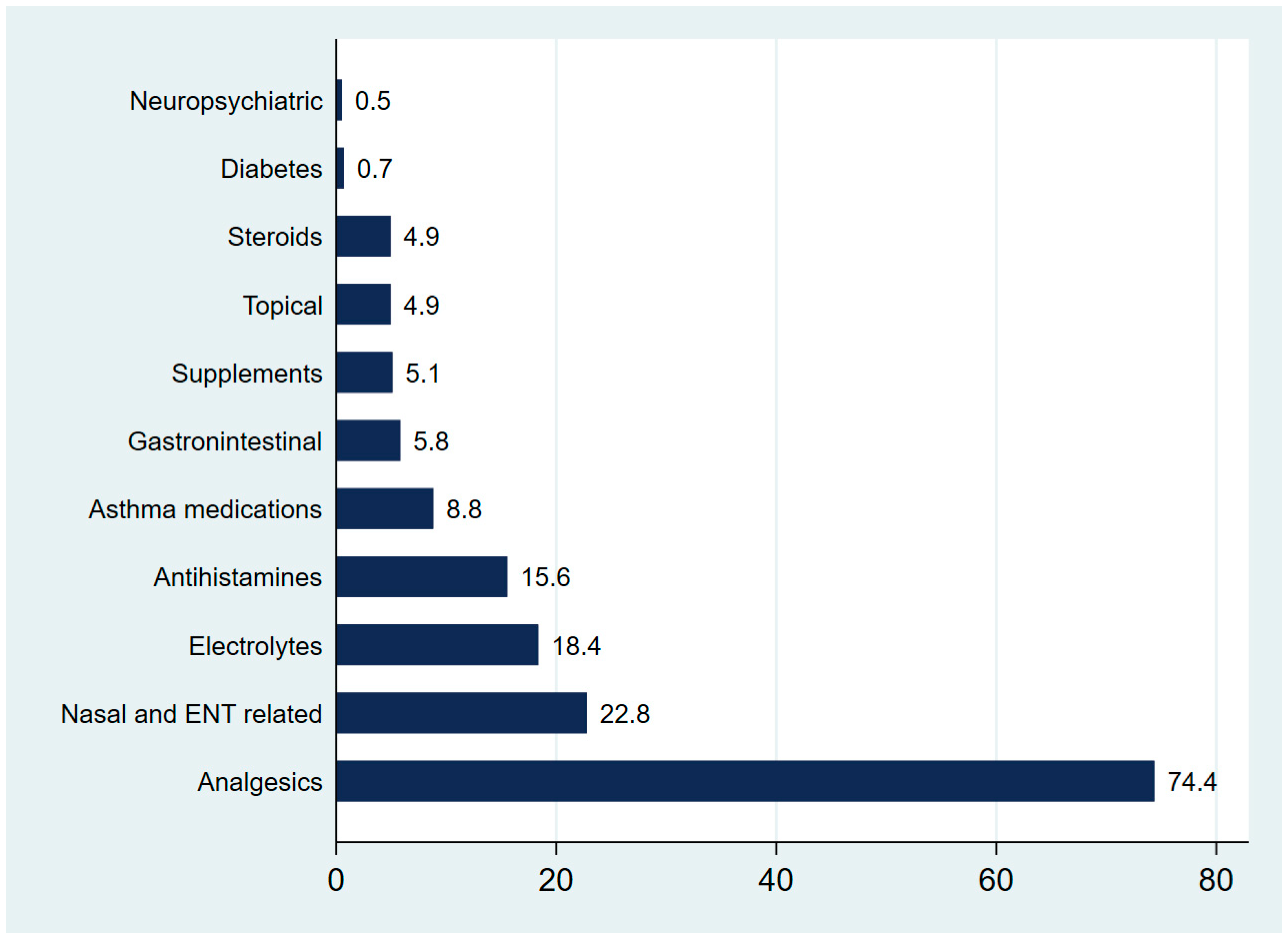
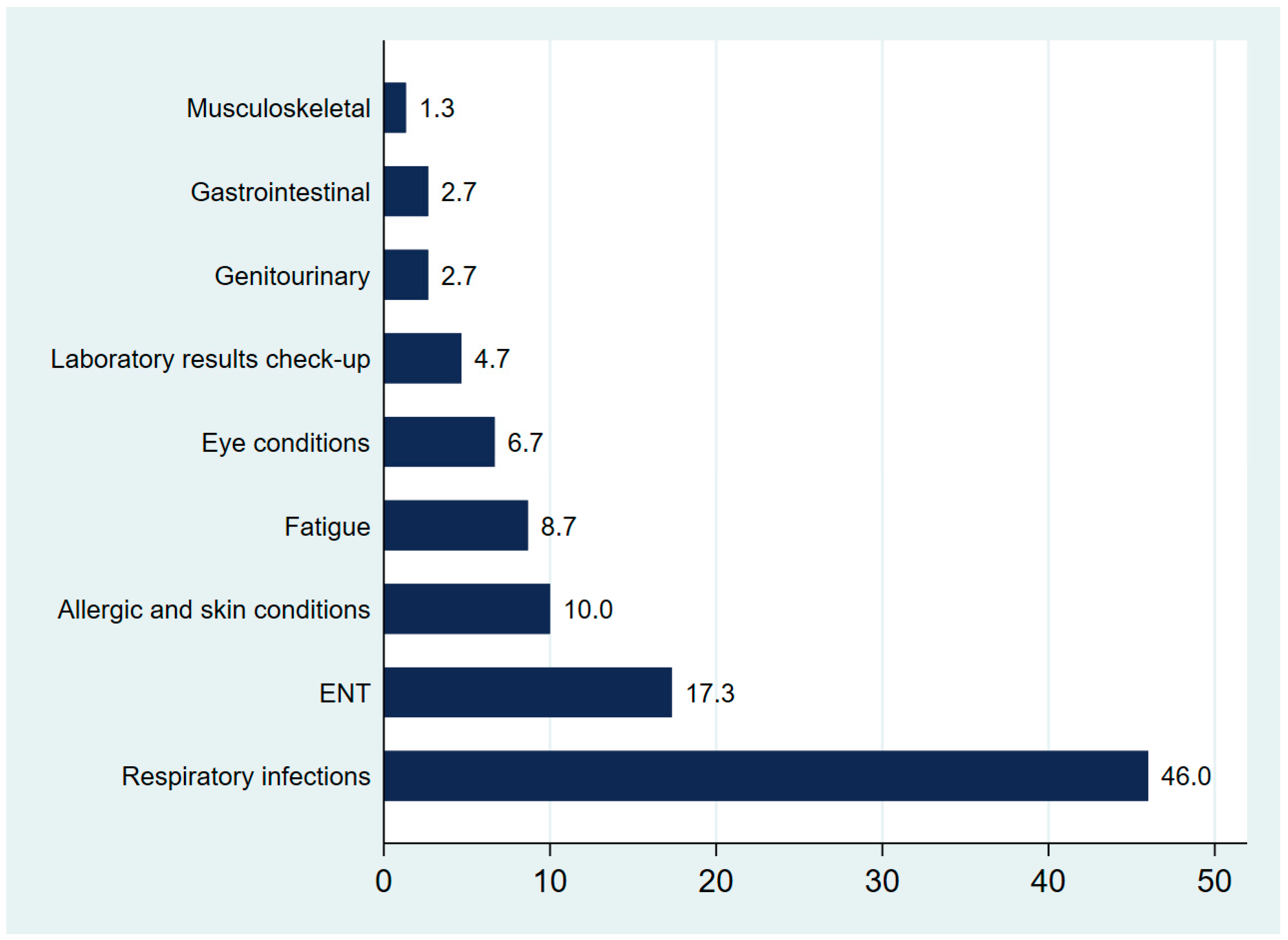
3.2. Visit Characteristics According to Medication Prescriptions
3.3. Patterns of Antibiotic Prescriptions by Class
3.4. Multivariable Logistic Regression of Prescriptions in Urgent Care Pediatric Visits
4. Discussion
4.1. Visit Characteristics According to Medication Prescriptions
4.2. Patterns of Antibiotic Prescriptions by Class
4.3. Implications and Recommendations
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| UCC | Urgent care clinic |
| ED | Emergency department |
| KSA | Kingdom of Saudi Arabia |
| MoH | Ministry of Health |
| CTAS | Canadian Triage and Acuity Scale |
| PHC | Primary healthcare |
| OR | Odds ratio |
| CI | Confidence interval |
References
- AAUCM. What Is Urgent Care Medicine? Orlando: The American Academy of Urgent Care Medicine. 2025. Available online: https://aaucm.org/what-is-urgent-care-medicine/ (accessed on 25 July 2025).
- Allen, L.; Cummings, J.R.; Hockenberry, J.M. The impact of urgent care centers on nonemergent emergency department visits. Health Serv. Res. 2021, 56, 721–730. [Google Scholar] [CrossRef] [PubMed]
- AAFP. Primary Care Defintion: American Academy of Family Physicians. 2025. Available online: https://www.aafp.org/about/policies/all/primary-care.html (accessed on 25 July 2025).
- MoH. Urgent Care Center Standard Policy; Ministry of Health: Riyadh, Saudi Arabia, 2025.
- Albalahi, N.M.; Al Bargawi, M.; Kofi, M. Awareness and utilization of urgent care services among patients attending Al-Wazarat PHCC in Riyadh, Saudi Arabia 2020. J. Fam. Med. Prim. Care 2021, 10, 4452–4462. [Google Scholar] [CrossRef]
- Mudd, S.S.; Alvarado, S.M.; Otaru, S.; Canares, T. Urgent Care Utilization in a Pediatric Population With Private Health Insurance. J. Pediatr. Health Care 2020, 34, e21–e27. [Google Scholar] [CrossRef]
- King, L.M.; Tsay, S.V.; Hicks, L.A.; Bizune, D.; Hersh, A.L.; Fleming-Dutra, K. Changes in outpatient antibiotic prescribing for acute respiratory illnesses, 2011 to 2018. Antimicrob. Steward. Healthc. Epidemiol. 2021, 1, 1–8. [Google Scholar] [CrossRef]
- Sohn, M.; Pontefract, B.; Dahal, K.; Klepser, M. Outpatient antibiotic stewardship during the COVID-19 era: Analysis of prescribing trends and guideline compliance. Antimicrob. Steward. Healthc. Epidemiol. 2025, 5, e168. [Google Scholar] [CrossRef] [PubMed]
- STATA. StataCorp: Stata Statistical Software: Release 16; StataCorp LLC: College Station, TX, USA, 2017. [Google Scholar]
- Nedved, A.; Fung, M.; Bizune, D.; Liu, C.M.; Obremskey, J.; Fleming-Dutra, K.E.; Hamdy, R.F.; Montalbano, A. A Multisite Collaborative to Decrease Inappropriate Antibiotics in Urgent Care Centers. Pediatrics 2022, 150, e2021051806. [Google Scholar] [CrossRef]
- Poole, N.M.; Shapiro, D.J.; Fleming-Dutra, K.E.; Hicks, L.A.; Hersh, A.L.; Kronman, M.P. Antibiotic Prescribing for Children in United States Emergency Departments: 2009–2014. Pediatrics 2019, 143, e20181056. [Google Scholar] [CrossRef]
- Lau, J.; Islam, S.; Polischuk, E. Appropriateness and Accuracy of Antimicrobial Prescriptions at Pediatric Emergency Department Discharge. Clin. Pediatr. 2022, 61, 461–464. [Google Scholar] [CrossRef]
- Hagedoorn, N.N.; Borensztajn, D.; Nijman, R.G.; Nieboer, D.; Herberg, J.A.; Balode, A.; von Both, U.; Carrol, E.; Eleftheriou, I.; Emonts, M.; et al. Development and validation of a prediction model for invasive bacterial infections in febrile children at European Emergency Departments: MOFICHE, a prospective observational study. Arch. Dis. Child. 2021, 106, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Covino, M.; Buonsenso, D.; Gatto, A.; Morello, R.; Curatole, A.; Simeoni, B.; Franceschi, F.; Chiaretti, A. Determinants of antibiotic prescriptions in a large cohort of children discharged from a pediatric emergency department. Eur. J. Pediatr. 2022, 181, 2017–2030. [Google Scholar] [CrossRef]
- Kissler, S.M.; Wang, B.; Mehrotra, A.; Barnett, M.; Grad, Y.H. Prescribing of antibiotics and other drugs to children from birth to age 5 in the United States: An observational study. medRxiv 2021. [Google Scholar] [CrossRef]
- López-Valverde, L.; Domènech, È.; Roguera, M.; Gich, I.; Farré, M.; Rodrigo, C.; Montané, E. Spontaneous Reporting of Adverse Drug Reactions in a Pediatric Population in a Tertiary Hospital. J. Clin. Med. 2021, 10, 5531. [Google Scholar] [CrossRef]
- Walkowiak, M.P.; Walkowiak, J.; Walkowiak, D. Respiratory Diagnoses Year-Round: Unraveling the Multifaceted Pediatric Infection Cycles. Influenza Other Respir. Viruses 2024, 18, e70037. [Google Scholar] [CrossRef] [PubMed]
- Lipsett, S.C.; Monuteaux, M.C.; Fine, A.M. Seasonality of Common Pediatric Infectious Diseases. Pediatr. Emerg. Care 2021, 37, 82–85. [Google Scholar] [CrossRef]
- Aguilar, A.G.; Canals, P.C.; Tian, M.; Miller, K.A.; Piper, B.J. Decreases and Pronounced Geographic Variability in Antibiotic Prescribing in Medicaid. Pharmacy 2024, 12, 46. [Google Scholar] [CrossRef]
- Burvenich, R.; De Boodt, S.; Lowie, L.; Janssens, A.; Beerten, S.G.; Vaes, B.; Toelen, J.; Verbakel, J.Y. Temporal trends in antibiotic prescribing and serious and nonserious infections in children presenting to general practice: A registry-based longitudinal cohort study of 162507 individuals. J. Antimicrob. Chemother. 2024, 79, 1397–1406. [Google Scholar] [CrossRef] [PubMed]
- Altaş, U.; Söğütlü, Y.; Altaş, Z.M.; Özkars, M.Y. Seasonal pattern of emergency department visits by children with asthma. East Mediterr Health J. 2023, 29, 789–795. [Google Scholar] [CrossRef]
- Serletti, L.; Dutcher, L.; Degnan, K.O.; Szymczak, J.E.; Cluzet, V.; David, M.Z.; Cressman, L.; Glassman, L.W.; Hamilton, K.W.; Centers for Disease Control and Prevention (CDC) Prevention Epicenters Program. Analysis of seasonal variation of antibiotic prescribing for respiratory tract diagnoses in primary care practices. Antimicrob. Steward. Healthc. Epidemiol. 2023, 3, e147. [Google Scholar] [CrossRef] [PubMed]
- AbdEl-Aty, M.A.; Amin, M.T.; Ahmed, S.M.; Elsedfy, G.O.; El-Gazzar, A.F. Exploring factors for antibiotic over-prescription in children with acute upper respiratory tract infections in Assiut, Egypt: A qualitative study. Antimicrob. Resist. Infect. Control 2024, 13, 2. [Google Scholar] [CrossRef]
- Wushouer, H.; Du, K.; Yu, J.; Zhang, W.; Hu, L.; Ko, W.; Fu, M.; Zheng, B.; Shi, L.; Guan, X. Outpatient Antibiotic Prescribing Patterns in Children among Primary Healthcare Institutions in China: A Nationwide Retrospective Study, 2017–2019. Antibiotics 2024, 13, 70. [Google Scholar] [CrossRef]
- Al-Baghli, N.A.; Al Saif, A.Z.; Al Dorazi, S.A.; Zainaldeen, M.H.; Alameer, A.H.; Albaghli, S.; Al-Dawood, A.M.; Buhelaiga, S.M.; Alsalim, B.S.; A Rabaan, A.; et al. Antibiotic-Prescribing Patterns Among Patients With Respiratory Symptoms in the Eastern Province, Kingdom of Saudi Arabia. Cureus 2023, 15, e44298. [Google Scholar] [CrossRef]
- Krueger, C.; Alqurashi, W.; Barrowman, N.; Litwinska, M.; Le Saux, N. The long and the short of pediatric emergency department antibiotic prescribing: A retrospective observational study. Am. J. Emerg. Med. 2024, 75, 131–136. [Google Scholar] [CrossRef]
- Almutairi, A.M.; Alwehaibi, S.A.; Almousa, A.Y.; Alanazi, S.; Bin Muaibed, R.R.; Althobaiti, R.; Alkheraiji, A.M.; Alamrani, H.A. A Multicenter Retrospective Chart Review Study Estimating the Prevalence of Iron Deficiency Anemia Among Infants, Toddlers, and Children in Riyadh, Saudi Arabia. Cureus 2024, 16, e70031. [Google Scholar] [CrossRef]
- Alhamed, M.S.; Alharbi, F.; Al Joher, A.; Dhahry, S.; Fallatah, A.A.; Alanazi, O.H.; Almutiri, J.M.; Albaradie, S.S.; Al Enezi, B.A.A.; Albishi, M.S. Vitamin D Deficiency in Children and Adolescents in Saudi Arabia: A Systematic Review. Cureus 2024, 16, e52040. [Google Scholar] [CrossRef]
- Meesters, K.; Buonsenso, D. Antimicrobial Stewardship in Pediatric Emergency Medicine: A Narrative Exploration of Antibiotic Overprescribing, Stewardship Interventions, and Performance Metrics. Children 2024, 11, 276. [Google Scholar] [CrossRef]
- NICE. Fever in Under 5s: Assessment and Initial Management. NICE Guideline [NG143]. 2019. Available online: https://www.nice.org.uk/guidance/ng143 (accessed on 25 July 2025).
- Chumpitazi, C.E.; Chang, C.; Atanelov, Z.; Dietrich, A.M.; Lam, S.H.; Rose, E.; Ruttan, T.; Shahid, S.; Stoner, M.J.; Sulton, C.; et al. Managing acute pain in children presenting to the emergency department without opioids. J. Am. Coll. Emerg. Physicians Open 2022, 3, e12664. [Google Scholar] [CrossRef]
- Satir, A.N.; Pfiffner, M.; Meier, C.R.; Caduff Good, A. Prescribing Patterns in Pediatric General Wards and Their Association with Prescribing Errors: A Retrospective Observational Study. Drugs Real World Outcomes 2023, 10, 619–629. [Google Scholar] [CrossRef]
- Leung, A.K.; Hon, K.L. Paediatrics: How to manage viral gastroenteritis. Drugs Context 2021, 10, 1–11. [Google Scholar] [CrossRef]
- Parisi, G.F.; Licari, A.; Papale, M.; Manti, S.; Salpietro, C.; Marseglia, G.L.; Leonardi, S. Antihistamines: ABC for the pediatricians. Pediatr. Allergy Immunol. 2020, 31 (Suppl. 24), 34–36. [Google Scholar] [CrossRef]
- Galistiani, G.F.B.R.; Babarczy, B.; Papp, R.; Hajdu, Á.; Szabó, É.H.; Viola, R.; Papfalvi, E.; Visnyovszki, Á.; Matuz, M. Prescribing Patterns and Variations of Antibiotic Use for Children in Ambulatory Care: A Nationwide Study. Antibiotics 2022, 11, 189. [Google Scholar] [CrossRef]
- Al-Shatnawi, S.F.; Al-Hosban, S.Y.; Altawalbeh, S.M.; Khasawneh, R.A. Antibiotic prescribing patterns for childhood infections in ambulatory settings in Jordan. Int. J. Clin. Pract. 2021, 75, e14740. [Google Scholar] [CrossRef] [PubMed]
- Yehualaw, A.; Taferre, C.; Bantie, A.T.; Demsie, D.G. Appropriateness and Pattern of Antibiotic Prescription in Pediatric Patients at Adigart General Hospital, Tigray, Ethiopia. BioMed Res. Int. 2021, 2021, 6640892. [Google Scholar] [CrossRef] [PubMed]
- Jahan, S.; Al-Saigul, A.M.; Hamdelsseed, S.A. Primary health care physicians’ prescribing patterns for children under five in Qassim, Saudi Arabia. Prim. Health Care Res. Dev. 2019, 20, e89. [Google Scholar] [CrossRef]
- El-Dahiyat, F.; Salah, D.; Alomari, M.; Elrefae, A.; Jairoun, A.A. Antibiotic Prescribing Patterns for Outpatient Pediatrics at a Private Hospital in Abu Dhabi: A Clinical Audit Study. Antibiotics 2022, 11, 1676. [Google Scholar] [CrossRef]
- Kim, C.; Kabbani, S.; Dube, W.C.; Neuhauser, M.; Tsay, S.; Hersh, A.; Marcelin, J.R.; Hicks, L.A. Health Equity and Antibiotic Prescribing in the United States: A Systematic Scoping Review. Open Forum Infect. Dis. 2023, 10, ofad440. [Google Scholar] [CrossRef]
- Waterlow, N.R.; Ashfield, T.; Knight, G.M. Observational study of antibiotic prescribing patterns by age and sex in primary care in England: Why we need to take this variation into account to evaluate antibiotic stewardship and predict AMR variation. JAC Antimicrob. Resist. 2025, 7, dlae210. [Google Scholar] [CrossRef]
| Characteristics | N (%) 1016 (100.00) | Medications Prescribed | p-Value | |
|---|---|---|---|---|
| Yes N (%) 635 (62.50) | No N (%) 381 (37.50) | |||
| Sex | 0.627 | |||
| Males | 506 (49.80) | 320 (63.24) | 186 (36.76) | |
| Females | 510 (50.20) | 315 (61.76) | 195 (38.24) | |
| Age group | <0.007 | |||
| Infants | 49 (4.82) | 20 (40.82) | 29 (59.18) | |
| Toddlers | 115 (11.32) | 65 (56.52) | 50 (43.48) | |
| Preschoolers | 263 (25.89) | 169 (64.26) | 94 (35.74) | |
| Schoolers | 448 (44.09) | 285 (63.62) | 163 (36.38) | |
| Adolescents | 141 (13.88) | 96 (68.09) | 45 (31.91) | |
| Nationality | 0.21 | |||
| Saudi | 710 (69.88) | 435 (61.27) | 275 (38.73) | |
| Non-Saudi | 306 (30.12) | 200 (65.36) | 106 (34.64) | |
| Characteristics | N (%) 1016 (100.00) | Medications Prescribed | p-Value | |
|---|---|---|---|---|
| Yes N (%) 635 (62.50) | No N (%) 381 (37.50) | |||
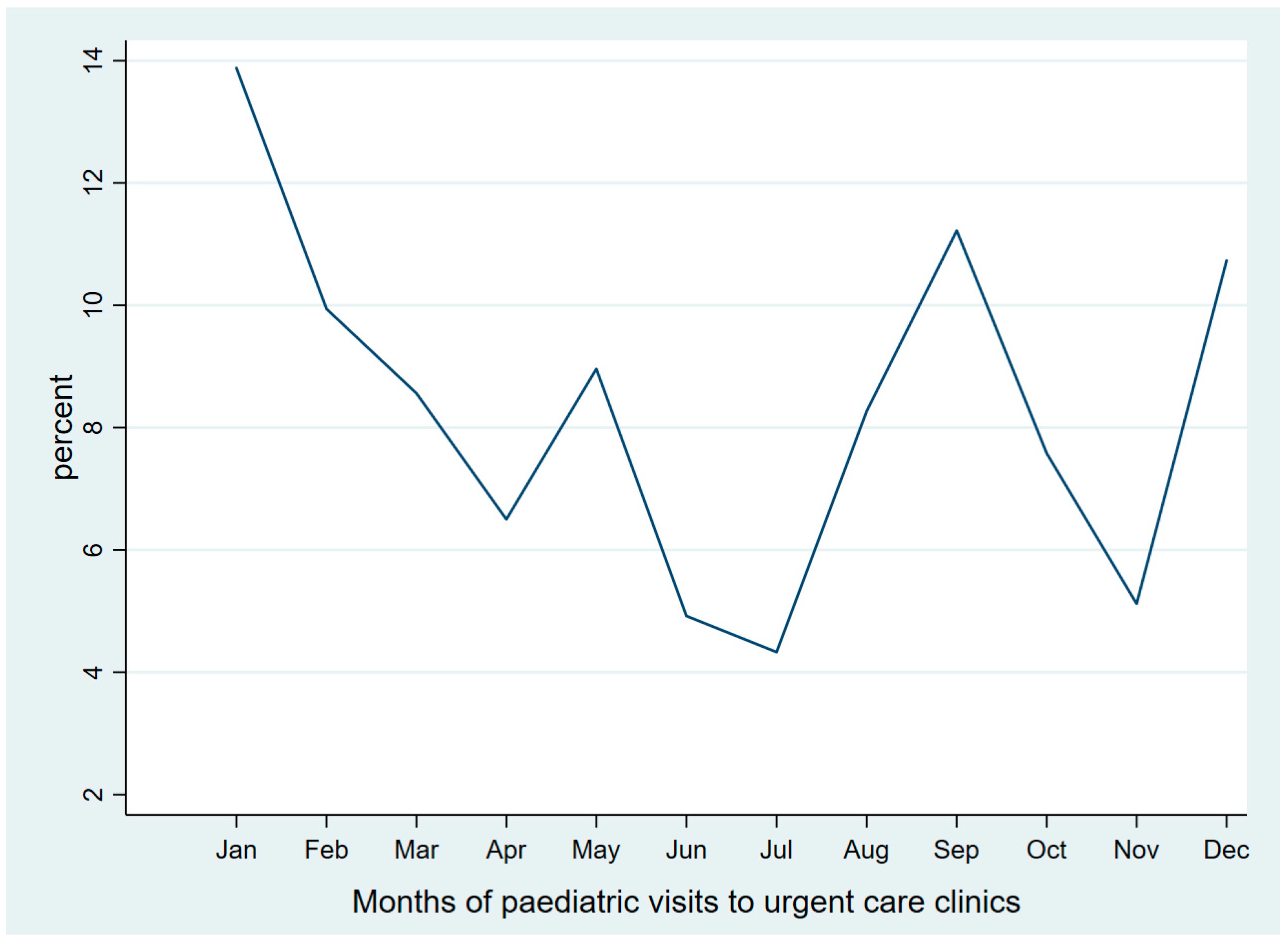
| Season | <0.001 | |||
| Winter | 351 (34.55) | 249 (70.94) | 102 (29.06) | |
| Spring | 244 (24.02) | 124 (50.82) | 120 (49.18) | |
| Summer | 178 (17.52) | 89 (50.00) | 89 (50.00) | |
| Autumn | 243 (23.92) | 173 (71.19) | 70 (28.81) | |
| Primary diagnosis | <0.001 | |||
| Respiratory infections | 402 (39.57) | 322 (79.90) | 81 (20.10) | |
| Routine check-up | 262 (25.79) | 76 (29.12) | 185 (70.88) | |
| Unspecified (e.g., general fatigue) | 72 (7.09) | 48 (66.67) | 24 (33.33) | |
| Allergic and skin conditions | 71 (6.99) | 52 (73.24) | 19 (26.76) | |
| Gastrointestinal | 55 (5.41) | 34 (61.82) | 21 (38.18) | |
| Musculoskeletal and orthopedics | 45 (4.43) | 31 (68.89) | 14 (31.11) | |
| ENT | 41 (4.02) | 33 (80.49) | 8 (19.51) | |
| Eye conditions | 30 (2.95) | 21 (70.00) | 9 (30.00) | |
| Genitourinary and puberty-related | 21 (2.07) | 7 (33.33) | 14 (66.67) | |
| Neurological disorders | 7 (0.69) | 3 (42.86) | 4 (57.14) | |
| Endocrine disorders and diabetes | 4 (0.39) | 3 (75.00) | 1 (25.00) | |
| Nutritional deficiencies | 4 (0.39) | 4 (100.00) | 0 | |
| Developmental, psychiatric, and behavioral | 2 (0.20) | 1 (50.00) | 1 (50.00) | |
| Characteristics of Antibiotic Prescribed Patients ¥‡ | Penicillins N (%) 107 (71.33) | Macrolides N (%) 14 (9.33) | Fluoroquinolones N (%) 9 (6.00) | Aminoglycosides N (%) 6 (4.00) | Nitroimidazoles N (%) 13 (8.67) |
|---|---|---|---|---|---|
| Males (n = 74) | 53 (71.62) | 8 (10.81) | 6 (8.11) | 4 (5.41) | 4 (5.41) |
| Females (n = 76) | 54 (71.05) | 6 (7.89) | 3 (3.95) | 2 (2.63) | 9 (11.84) |
| All age groups | |||||
| Infants (n = 6) | 1 (16.67) | 2 (33.33) | 0 | 0 | 3 (50.00) |
| Toddlers (n = 12) | 7 (58.33) | 2 (16.67) | 0 | 3 (25.00) | 0 |
| Preschoolers (n = 42) | 35 (83.33) | 3 (7.14) | 1 (2.38) | 2 (4.76) | 1 (2.38) |
| Schoolers (n = 75) | 54 (72.00) | 7 (9.33) | 7 (9.33) | 1 (1.33) | 7 (9.33) |
| Adolescents (n = 15) | 10 (66.67) | 0 | 1 (6.67) | 0 | 2 (13.33) |
| Characteristic | Odds of Prescribing | |||
|---|---|---|---|---|
| p-Value | Unadjusted Odds (95% CI) | p-Value | Adjusted Odds (95% CI) | |
| Sex | ||||
| Males | 0.62 | 1.06 (0.82–1.37) | 0.78 | 1.04 (0.78–1.40) |
| Females | Ref | |||
| Age group | ||||
| Infants | 0.002 | 0.39 (0.21–0.71) | 0.001 | 0.30 (0.15–0.61) |
| Toddlers | 0.16 | 0.74 (0.49–1.12) | 0.10 | 0.66 (0.40–1.08) |
| Preschoolers | 0.86 | 1.02 (0.74–1.41) | 0.06 | 0.70 (0.48–1.01) |
| Schoolers | Ref | |||
| Adolescents | 0.33 | 1.22 (0.81–1.82) | 0.03 | 1.67 (1.04–2.67) |
| Seasons | ||||
| Winter | Ref | |||
| Spring | <0.001 | 0.42 (0.30–0.59) | 0.001 | 0.52 (0.35–0.77) |
| Summer | <0.001 | 0.40 (0.28–0.59) | 0.005 | 0.54 (0.35–0.83) |
| Autumn | 0.94 | 1.01 (0.70–1.45) | 0.87 | 0.96 (0.64–1.44) |
| Primary diagnosis | ||||
| Respiratory infections | Ref | |||
| Routine check-up | <0.001 | 0.10 (0.07–0.14) | <0.001 | 0.10 (0.06–0.14) |
| Unspecified (e.g., general fatigue) | 0.01 | 0.50 (0.29–0.86) | 0.01 | 0.47 (0.27–0.84) |
| Allergic and skin conditions | 0.20 | 0.68 (0.38–1.22) | 0.25 | 0.23 (0.38–1.26) |
| Gastrointestinal | 0.003 | 0.40 (0.22–0.73) | 0.009 | 0.43 (0.23–0.80) |
| Musculoskeletal and orthopedics | 0.09 | 0.55 (0.28–1.09) | 0.04 | 0.48 (0.23–0.97) |
| ENT | 0.92 | 1.03 (0.46–2.33) | 0.86 | 1.05 (0.46–2.41) |
| Eye conditions | 0.20 | 0.58 (0.25–1.33) | 0.37 | 0.67 (0.29–1.58) |
| Genitourinary and puberty-related | <0.001 | 0.12 (0.04–0.32) | <0.001 | 0.12 (0.04–0.32) |
| Neurological disorders | 0.03 | 0.18 (0.04–0.85) | 0.04 | 0.19 (0.04–0.93) |
| Endocrine disorders and diabetes | 0.80 | 0.75 (0.07–7.35) | 0.62 | 0.55 (0.05–6.01) |
| Developmental, psychiatric, and behavioral | 0.33 | 0.25 (0.01–4.06) | 0.42 | 0.31 (0.01–5.27) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlOmar, R.S.; AlShamlan, N.A.; Al Yateem, A.A.; Al-Abdulazeem, A.A.; Al-Turki, A.M.; Alghamdi, R.J.; Alhamed, N.A.; Motabgani, S.; Aldhawyan, A.F.; Al Shammari, M.A. Pediatric Medication Prescribing Across Urgent Care Visits: An Epidemiologic View from a Primary Care Setting in the Kingdom of Saudi Arabia. Med. Sci. 2025, 13, 177. https://doi.org/10.3390/medsci13030177
AlOmar RS, AlShamlan NA, Al Yateem AA, Al-Abdulazeem AA, Al-Turki AM, Alghamdi RJ, Alhamed NA, Motabgani S, Aldhawyan AF, Al Shammari MA. Pediatric Medication Prescribing Across Urgent Care Visits: An Epidemiologic View from a Primary Care Setting in the Kingdom of Saudi Arabia. Medical Sciences. 2025; 13(3):177. https://doi.org/10.3390/medsci13030177
Chicago/Turabian StyleAlOmar, Reem S., Nouf A. AlShamlan, Ahmed A. Al Yateem, Abdulrahman A. Al-Abdulazeem, Ahmed M. Al-Turki, Reema J. Alghamdi, Najla A. Alhamed, Sameerah Motabgani, Adam F. Aldhawyan, and Malak A. Al Shammari. 2025. "Pediatric Medication Prescribing Across Urgent Care Visits: An Epidemiologic View from a Primary Care Setting in the Kingdom of Saudi Arabia" Medical Sciences 13, no. 3: 177. https://doi.org/10.3390/medsci13030177
APA StyleAlOmar, R. S., AlShamlan, N. A., Al Yateem, A. A., Al-Abdulazeem, A. A., Al-Turki, A. M., Alghamdi, R. J., Alhamed, N. A., Motabgani, S., Aldhawyan, A. F., & Al Shammari, M. A. (2025). Pediatric Medication Prescribing Across Urgent Care Visits: An Epidemiologic View from a Primary Care Setting in the Kingdom of Saudi Arabia. Medical Sciences, 13(3), 177. https://doi.org/10.3390/medsci13030177







