Idiopathic Scoliosis Progression: Presenting Rib and Segmental Rib Index as Predictors—A Literature Review
Abstract
1. Introduction
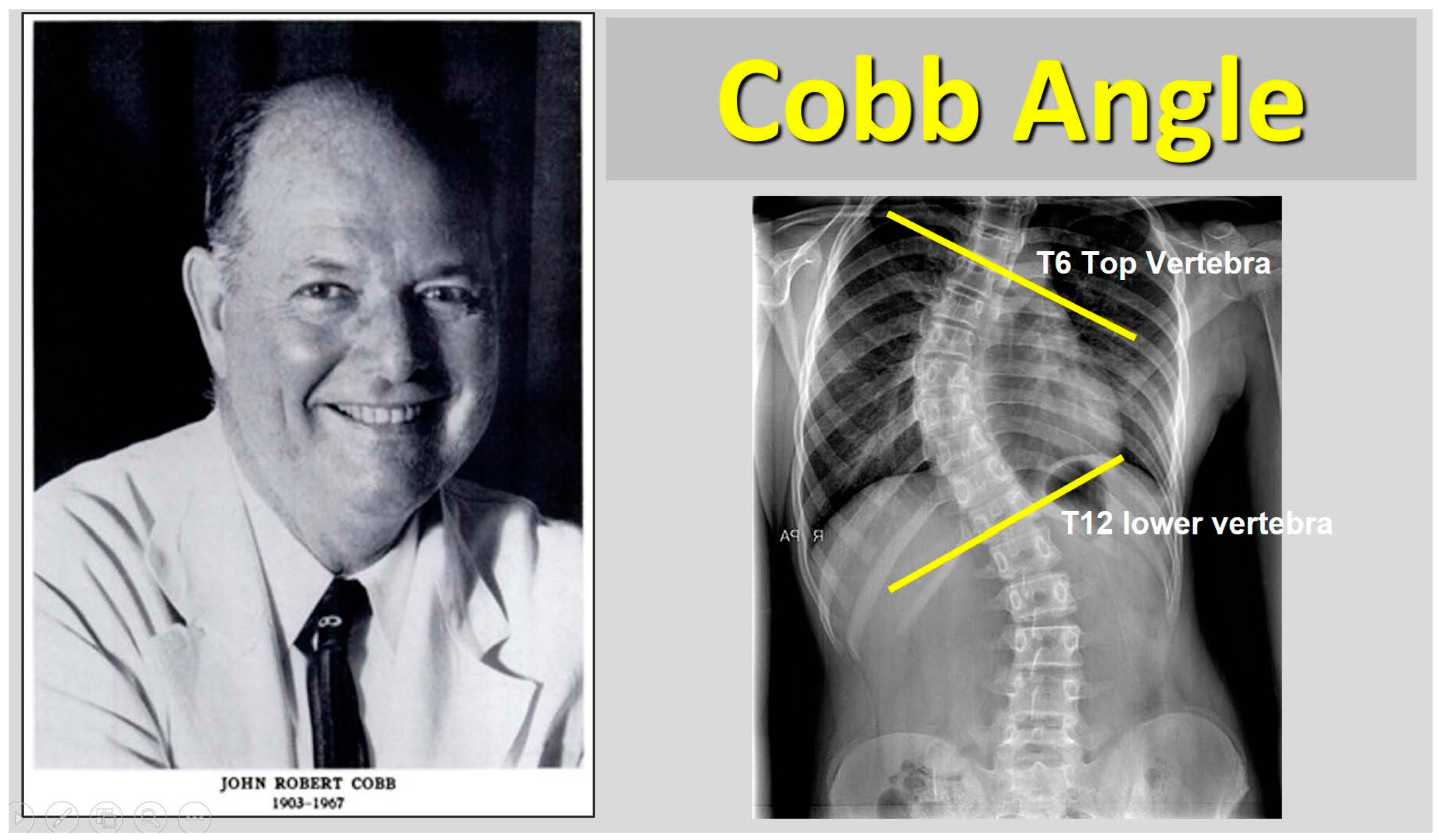
2. Cobb Angle—Rib Hump
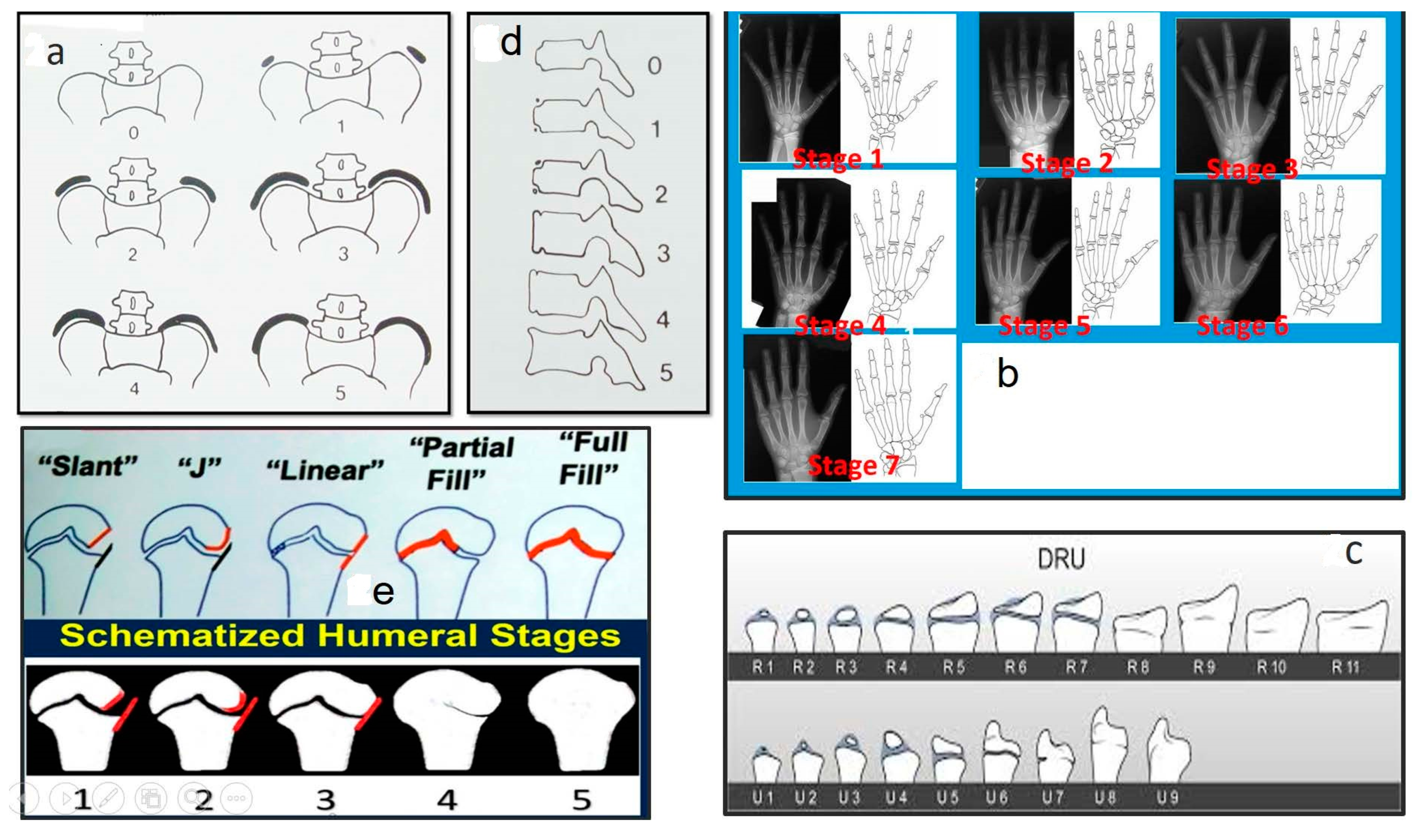
3. Methods for Assessing the Degree of Skeletal Maturity
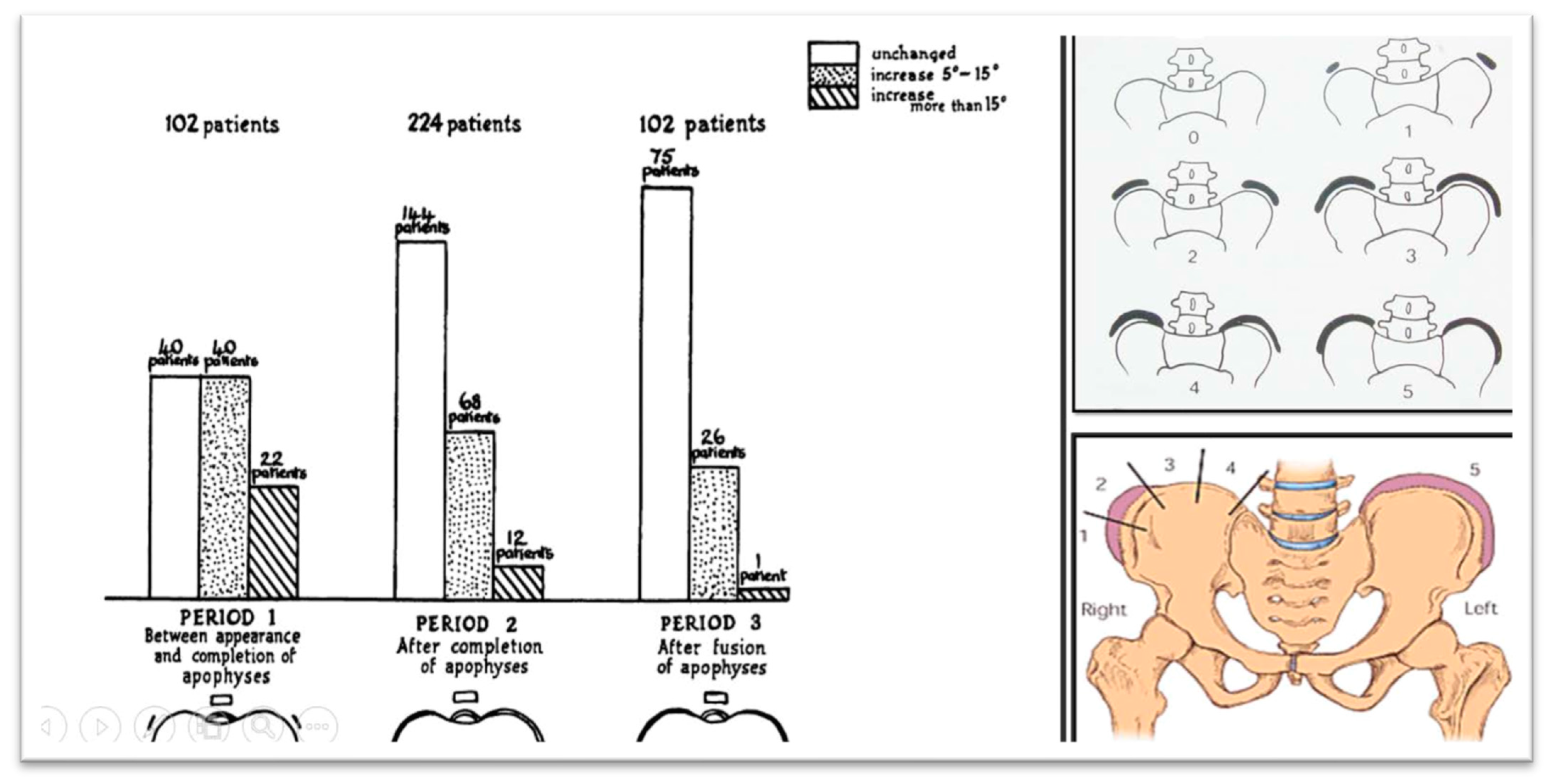
3.1. The Iliac Apophysis and the Evolution of Curves in Scoliosis
3.2. Sanders Skeletal Maturity Staging System
3.3. Distal Radius and Ulna Classification (DRU) Scheme in Predicting Growth Peak and Curve Progression in Idiopathic Scoliosis
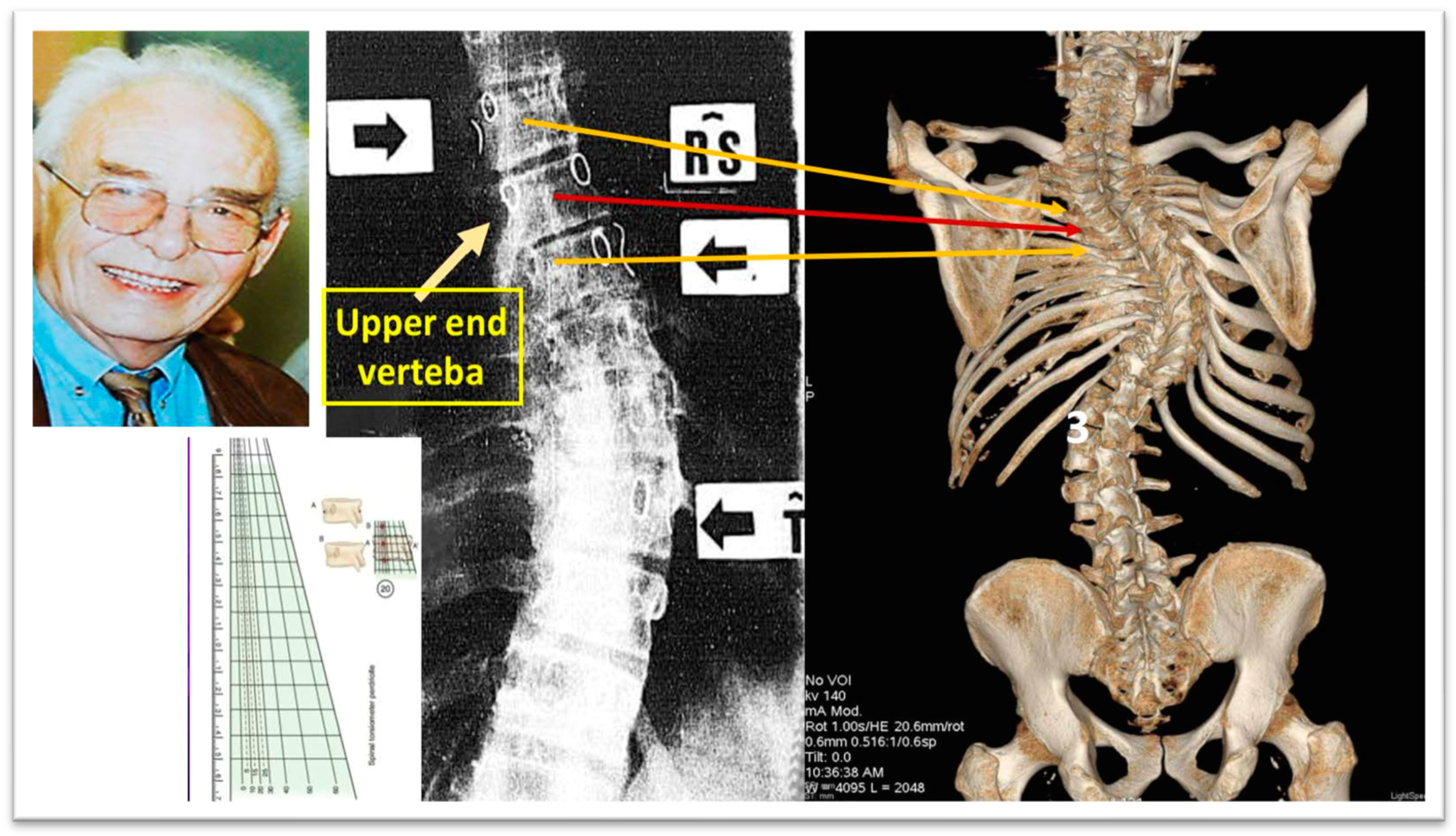
3.4. Ossification of the Vertebral Epiphyseal Rings
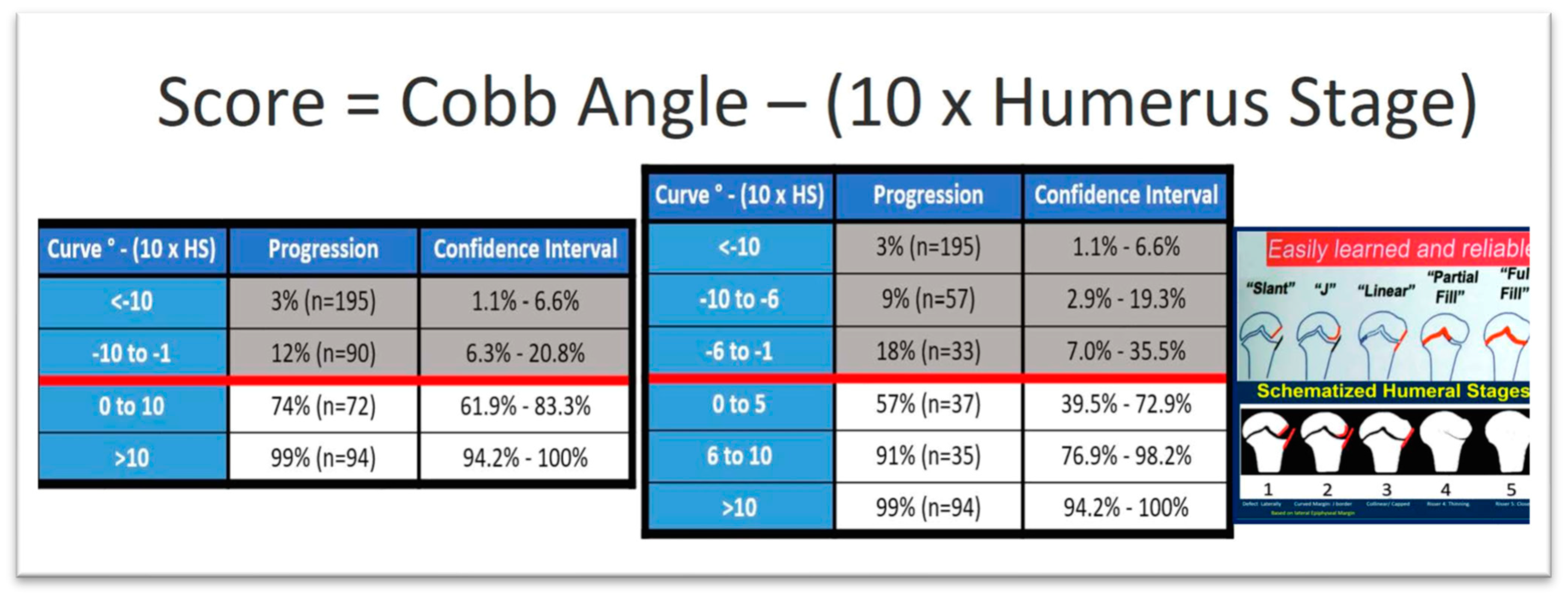
3.5. Ossification of the Humeral Head
3.6. Ossification of Calcaneal Apophysis
4. Prognostic Factors of IS Progression According to the Patient’s Presentation Age
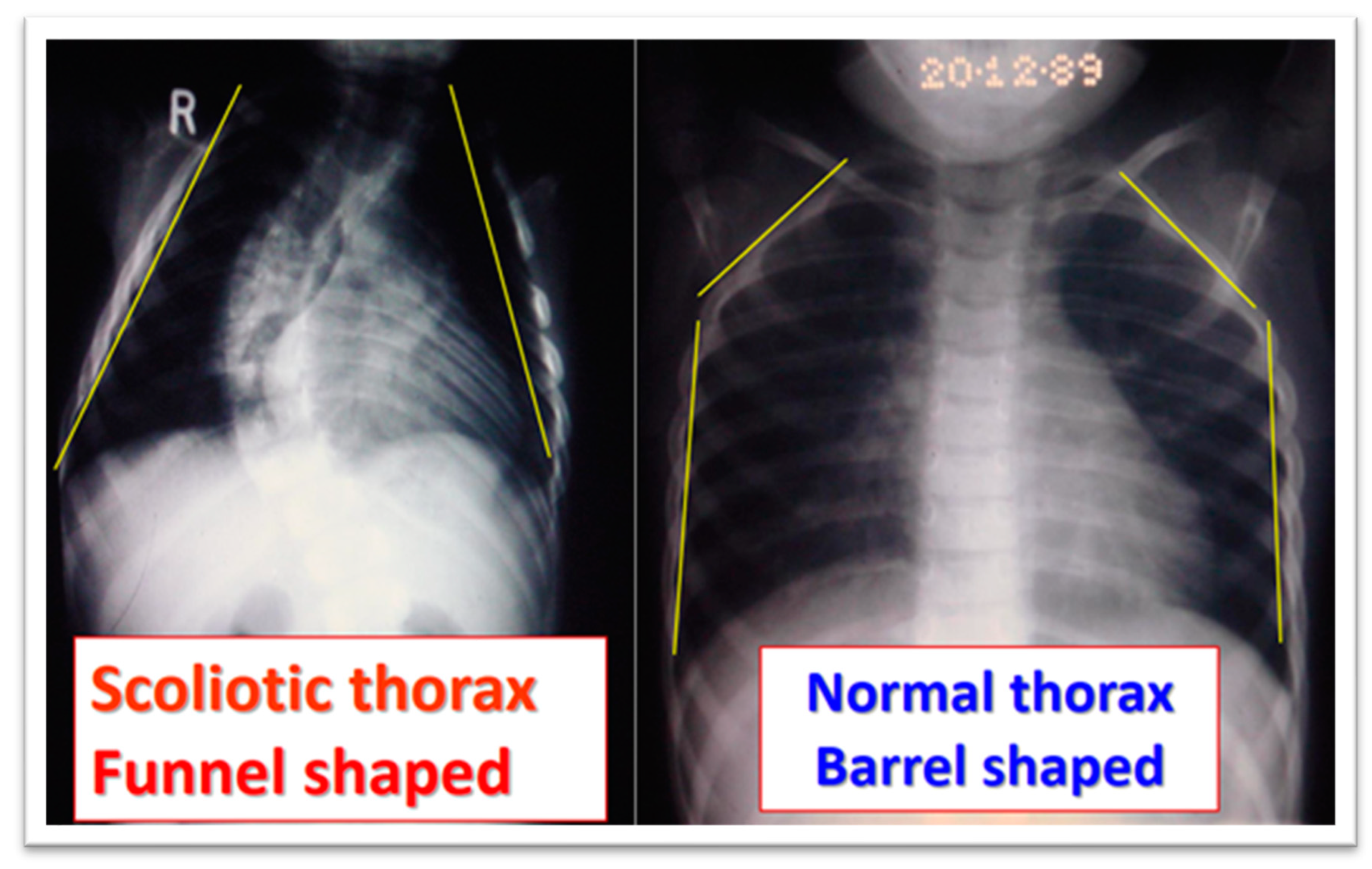
4.1. Infantile Idiopathic Scoliosis (IIS)

4.2. Juvenile Idiopathic Scoliosis—JIS
4.3. Predictors for Progression of Adolescent Idiopathic Scoliosis—AIS
4.4. Predictors for Progression of Braced Adolescent Idiopathic Scoliosis (AIS)
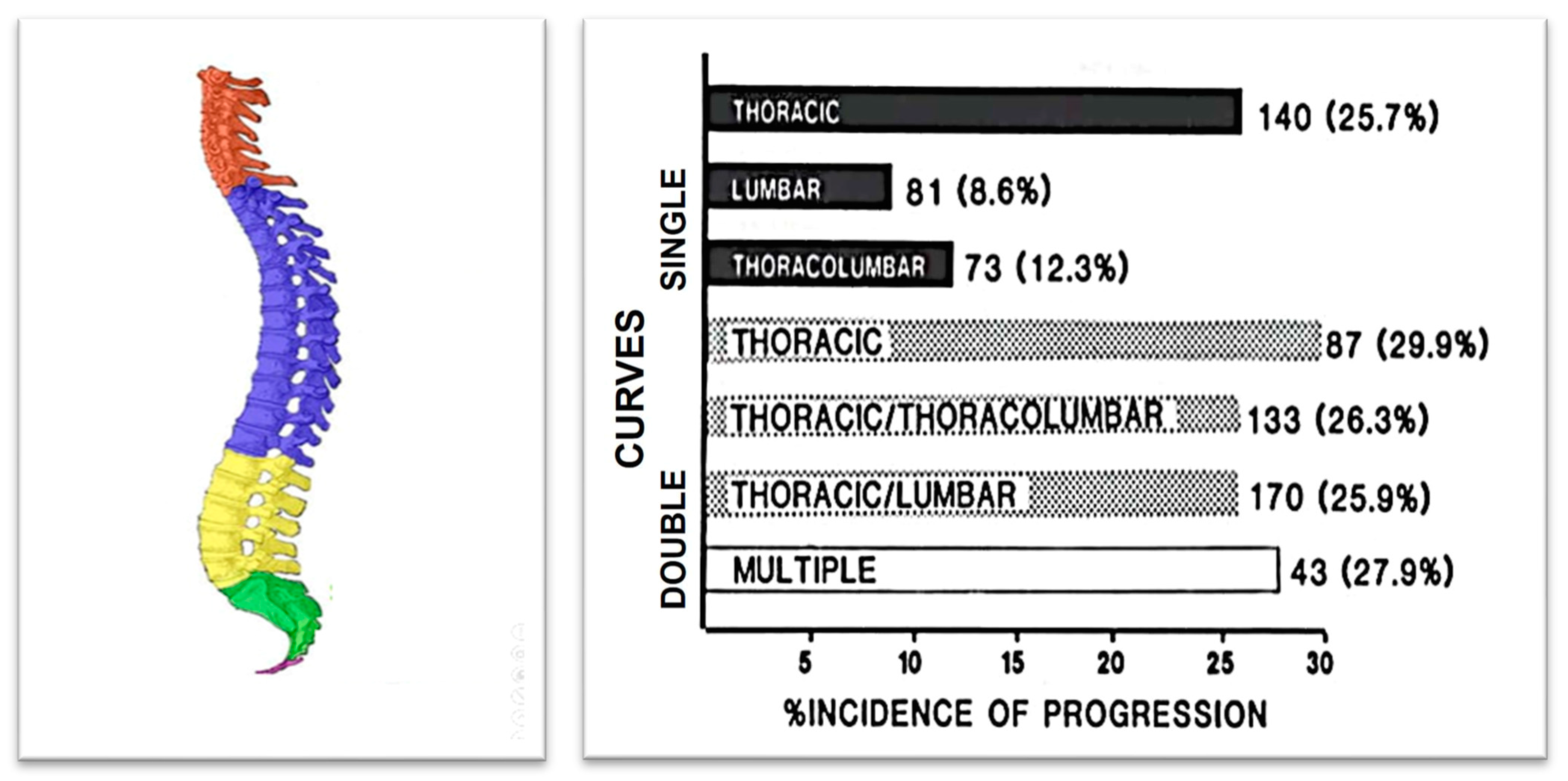
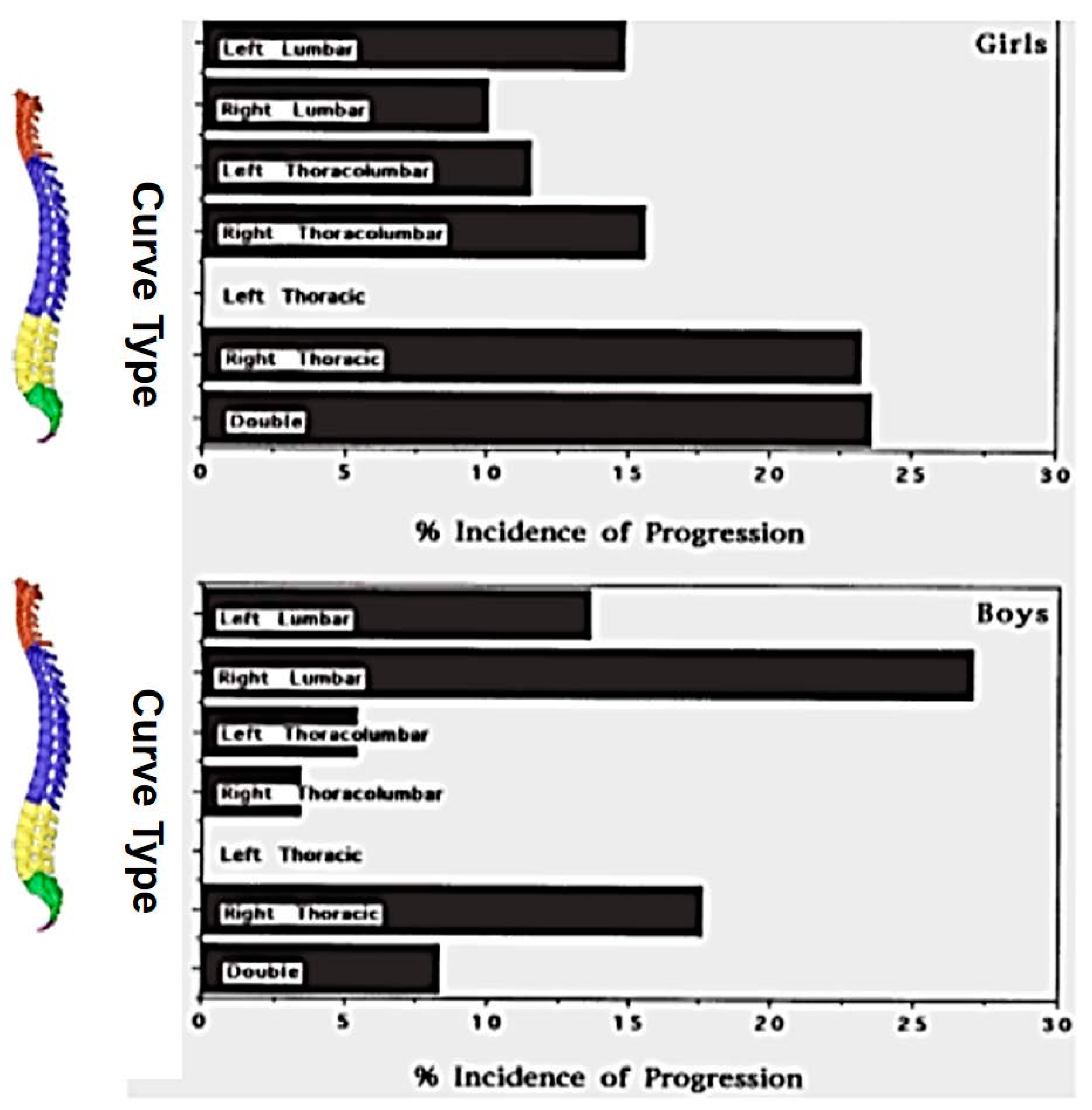
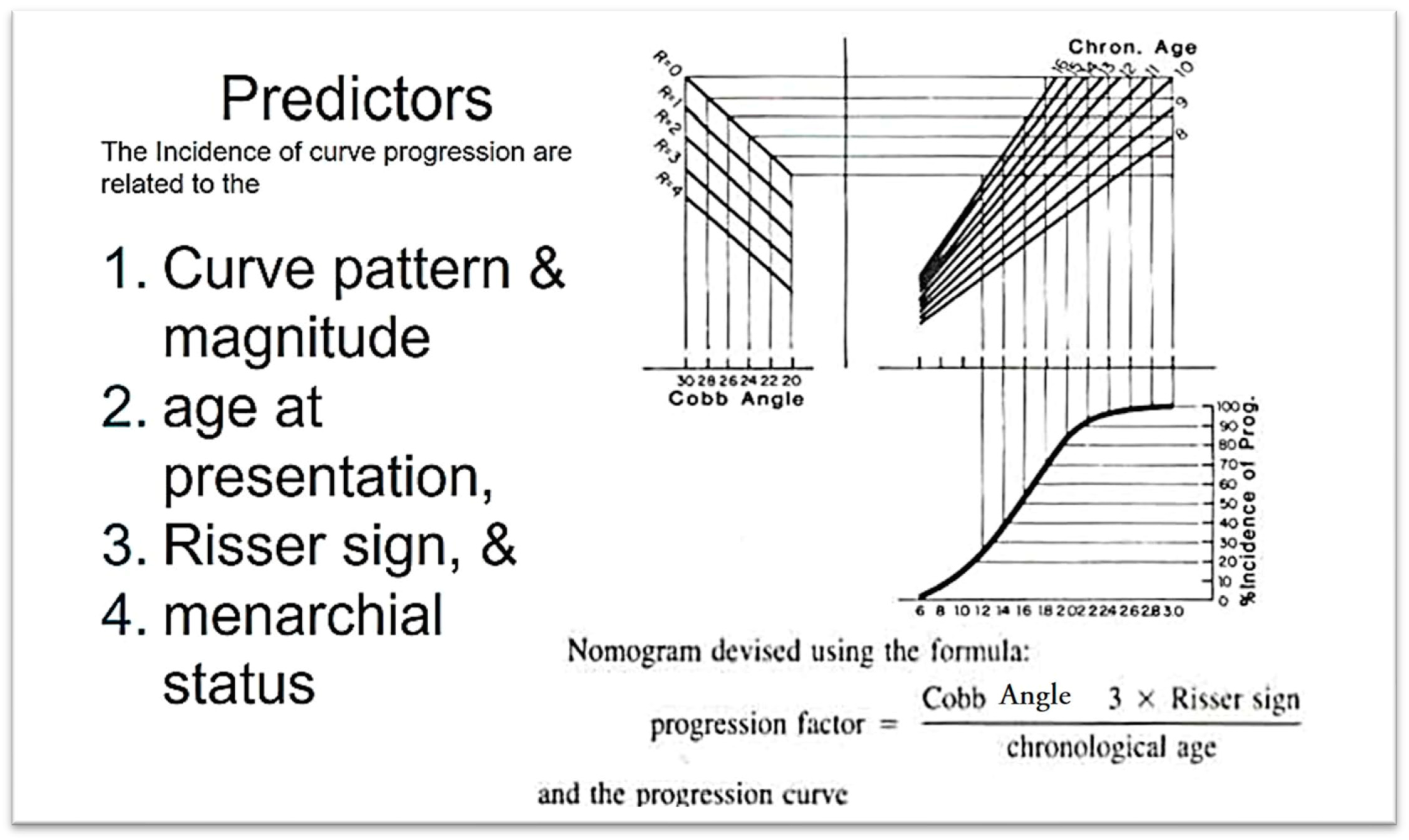
4.5. The Prediction of Curve Progression in Untreated Idiopathic Scoliosis During Growth
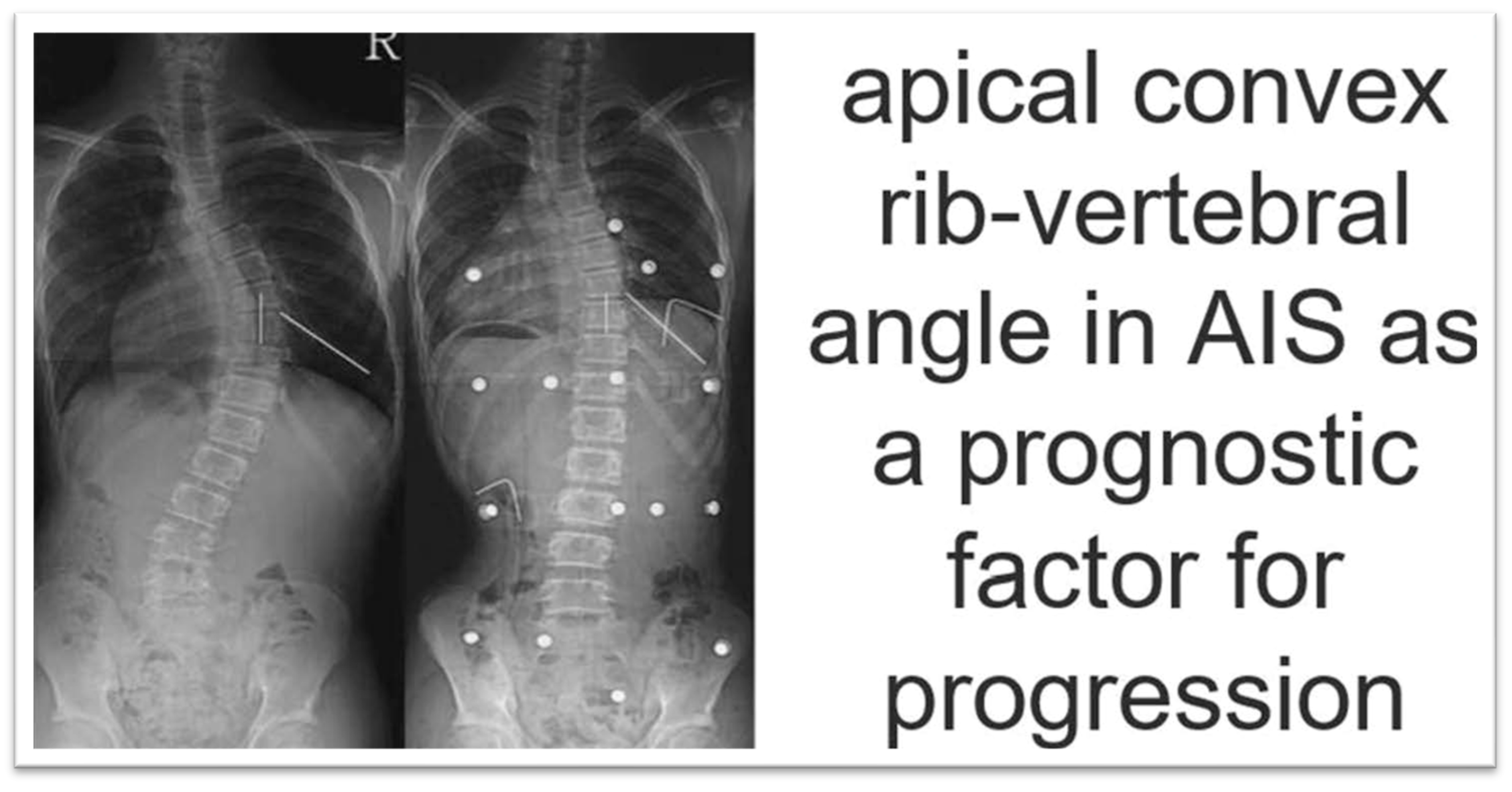
4.6. Apical Convex Rib–Vertebral Angle in AIS as a Prognostic Factor for Progression
5. Predictors for Curve Progression at Skeletal Maturity
6. Models of Prediction of Progression of IS
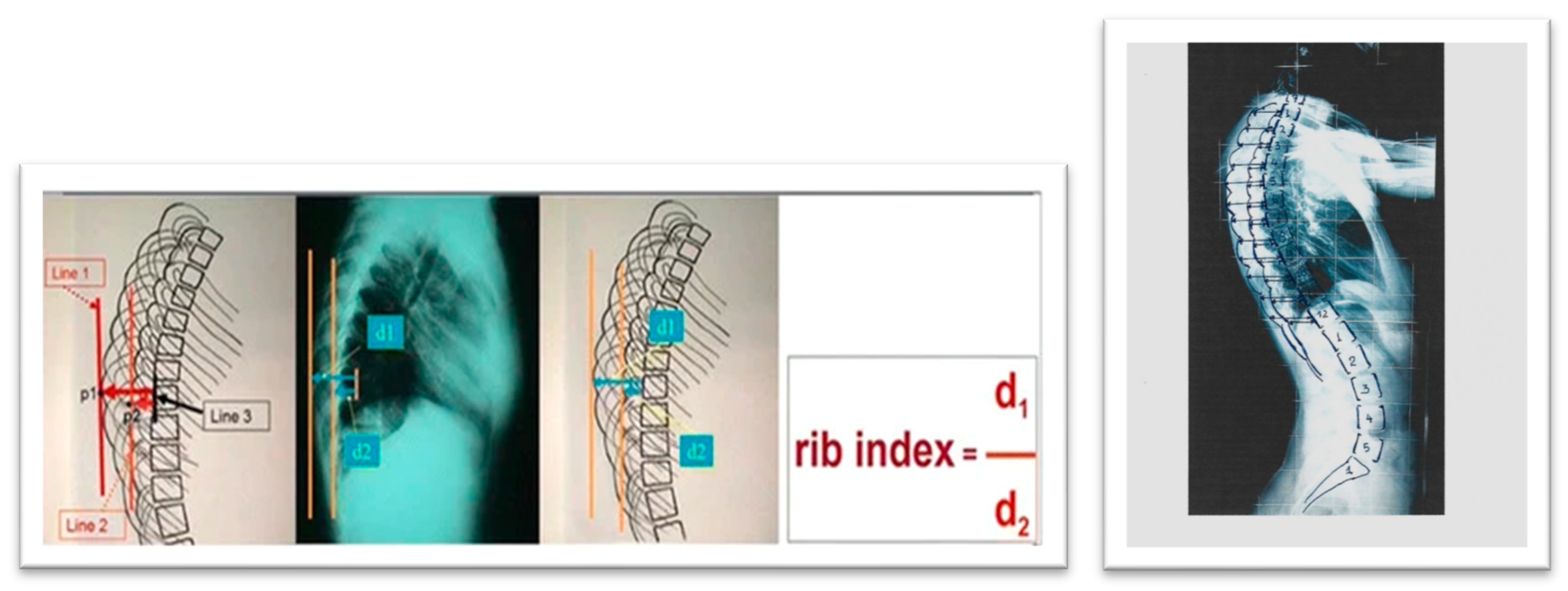
7. Rib Index: A Thoracic Deformity Parameter as Predictor of Progression
8. Critical Opinion
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peterson, L.-E.; Nachemson, A.L. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from The Brace Study of the Scoliosis Research Society. J. Bone Jt. Surg. 1995, 77, 823–827. [Google Scholar] [CrossRef]
- Grivas, T.B.; Vasiliadis, E.; Katzouraki, G.; Lykouris, D.; Sekouris, N.; Mazioti, C.; Mamzeri, A.; Papagianni, D.; Mparka, E.; Kataraxia, E. The multiplane initial skeletal remodeling during scoliogenesis. Acta Orthop. Traumatol. Hell. 2025, accepted. [Google Scholar]
- Noshchenko, A.; Hoffecker, L.; Lindley, E.M.; Burger, E.L.; Cain, C.M.; Patel, V.V.; Bradford, A.P. Predictors of spine deformity progression in adolescent idiopathic scoliosis: A systematic review with meta-analysis. World J. Orthop. 2015, 6, 537–558. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Cheuk, K.Y.; Xu, L.; Wang, Y.; Feng, Z.; Sit, T.; Cheng, K.L.; Nepotchatykh, E.; Lam, T.P.; Liu, Z.; et al. A validated composite model to predict risk of curve progression in adolescent idiopathic scoliosis. eClinicalMedicine 2020, 18, 100236. [Google Scholar] [CrossRef]
- Dansereau, J.; Stokes, I.A.F.; Moreland, M.S. Radiographic reconstruction of 3Dhuman rib cage. In Surface Topography Spinal Deformity; Stokes, I.A.F., Pekelsky, J.R., Moreland, M.S., Eds.; Gustav Fischer: Stuttgart, Germany, 1987; pp. 67–76. [Google Scholar]
- Dansereau, J.; Stokes, I.A.F. Measurements of three-dimensional shape of the rib cage. J. Biomech. 1988, 21, 893–901. [Google Scholar] [CrossRef] [PubMed]
- Hierholzer, E.; Hackenberg, L. Three-dimensional shape analysis of the scoliotic spine using MR tomography and rasterstereography. Stud. Health Technol. Inform. 2002, 91, 184–189. [Google Scholar] [PubMed]
- Sangole, A.P.; Aubin, C.E.; Labelle, H.; Stokes, I.A.; Lenke, L.G.; Jackson, R.; Newton, P. Three-dimensional classification of thoracic scoliotic curves. Spine 2009, 34, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Ilharreborde, B.; Steffen, J.S.; Nectoux, E.; Vital, J.M.; Mazda, K.; Skalli, W.; Obeid, I. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine 2011, 36, E1306–E1313. [Google Scholar] [CrossRef]
- Donzelli, S.; Poma, S.; Balzarini, L.; Borboni, A.; Respizzi, S.; Villafane, J.H.; Zaina, F.; Negrini, S. State of the art of current 3-D scoliosis classifications: A systematic review from a clinical perspective. J. Neuroeng. Rehabil. 2015, 12, 91. [Google Scholar] [CrossRef] [PubMed]
- Nault, M.-L.; Mac-Thiong, J.-M.; Roy-Beaudry, M.; Turgeon, I.; de Guise, J.; Labelle, H.; Parent, S. Three-Dimensional Spinal Morphology Can Differentiate Between Progressive and Nonprogressive Patients with Adolescent Idiopathic Scoliosis at the Initial Presentation: A prospective study. Spine 2014, 39, E601–E606. [Google Scholar] [CrossRef]
- Lonstein, J.; Carlson, J. The prediction of curve progression in untreated idiopathic scoliosis. J. Bone Jt. Surg. 1984, 3, 1061–1071. [Google Scholar] [CrossRef]
- Parent, E.C.; Donzelli, S.; Yaskina, M.; Negrini, A.; Rebagliati, G.; Cordani, C.; Zaina, F.; Negrini, S. Prediction of future curve angle using prior radiographs in previously untreated idiopathic scoliosis: Natural history from age 6 to after the end of growth (SOSORT 2022 award winner). Eur. Spine J. 2023, 32, 2171–2184. [Google Scholar] [CrossRef] [PubMed]
- Vergari, C.; Gajny, L.; Courtois, I.; Ebermeyer, E.; Abelin-Genevois, K.; Kim, Y.; Langlais, T.; Vialle, R.; Assi, A.; Ghanem, I.; et al. Quasi-automatic early detection of progressive idiopathic scoliosis from biplanar radiography: A preliminary validation. Eur. Spine J. 2019, 28, 1970–1976. [Google Scholar] [CrossRef] [PubMed]
- Vergari, C.; Gajny, L.; Ebermeyer, E.; Abelin-Genevois, K.; Kim, Y.; Courtois, I.; Langlais, T.; Vialle, R.; Assi, A.; Ghanem, I.; et al. Early detection of progressive idiopathic scoliosis through the quasi-automatic 3D reconstruction of the spine from biplanar radiography. Eur. Spine J. 2019, 28, 2878–2879. [Google Scholar] [CrossRef] [PubMed]
- Lv, Z.; Lv, W.; Wang, L.; Ou, J. Development and validation of machine learning-based models for prediction of adolescent idiopathic scoliosis: A retrospective study. Medicine 2023, 102, e33441. [Google Scholar] [CrossRef]
- Meng, N.; Wong, K.-Y.; Zhao, M.; Cheung, J.P.Y.; Zhang, T. Radiograph comparable image synthesis for spine alignment analysis using deep learning with prospective clinical validation. EClinicalMedicine 2023, 61, 102050. [Google Scholar] [CrossRef]
- Zhang, T.; Zhu, C.; Zhao, Y.; Zhao, M.; Wang, Z.; Song, R.; Meng, N.; Sial, A.; Diwan, A.; Liu, J.; et al. Deep learning model to classify and monitor idiopathic scoliosis in adolescents using a single smartphone photograph. JAMA Netw. Open 2023, 6, e2330617. [Google Scholar] [CrossRef] [PubMed]
- Bassani, T.; Cina, A.; Galbusera, F.; Cazzato, A.; Pellegrino, M.E.; Albano, D.; Sconfienza, L.M. Feasibility of generating sagittal radiographs from coronal views using GAN-based deep learning framework in adolescent idiopathic scoliosis. Eur. Radiol. Exp. 2025, 9, 11. [Google Scholar] [CrossRef]
- Cobb, J. Outline for the study of scoliosis. Instr. Course Lect. 1948, 5, 261–275. [Google Scholar]
- Adams, W. Lectures on the Pathology and Treatment of Lateral and Other Forms of Curvature of the Spine. Br. Foreign Med. Chir. Rev. 1865, 36, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Duval-Beaupere, G.; Lamireau, T.H. Scoliosis at less than 30~ property of the evolutivity (risk of progression). Spine 1985, 10, 421–424. [Google Scholar] [CrossRef]
- Duval-Beaupère, G. Rib hump and supine angle as prognostic factors for mild scoliosis. Spine 1992, 17, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Manzetti, M.; Ruffilli, A.; Barile, F.; Viroli, G.; Traversari, M.; Vita, F.; Cerasoli, T.; Arceri, A.; Artioli, E.; Mazzotti, A.; et al. Is there a skeletal age index that can predict accurate curve progression in adolescent idiopathic scoliosis? A systematic review. Pediatr. Radiol. 2024, 54, 299–315. [Google Scholar] [CrossRef] [PubMed]
- Risser, J.C. Important Practical Facts in the Treatment of Scoliosis. American Academy of Orthopaedic Surgeons. Instr. Course Lect. 1948, 5, 248. [Google Scholar]
- Sanders, J.O.; Khoury, J.G.; Kishan, S.; Browne, R.H.; Mooney, J.F.I.I.I.; Arnold, K.D.; McConnell, S.J.; Bauman, J.A.; Finegold, D.N. Predicting Scoliosis Progression from Skeletal Maturity: A Simplified Classification During Adolescence. J. Bone Joint Surg. 2008, 90, 540–553. [Google Scholar] [CrossRef] [PubMed]
- Luk, K.D.K.; Saw, L.B.; Grozman, S.; Cheung, K.M.C.; Samartzis, D. Assessment of skeletal maturity in scoliosis patients to determine clinical management: A new classification scheme using distal radius and ulna radiographs. Spine J. 2014, 14, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Mao, S.; Shi, B.; Liu, Z.; Liu, D.; Sun, X.; Qiu, Y.; Zhu, Z. Utilization of distal radius ulna classification scheme in predicting growth peak curve progression in idiopathic scoliosis girls undergoing bracing treatment. Eur. Spine J. 2020, 29, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Makino, T.; Kaito, T.; Sakai, Y.; Kashii, M.; Yoshikawa, H. Asymmetrical ossification in the epiphyseal ring of patients with adolescent idiopathic scoliosis: A retrospective review. Bone Joint J. 2016, 98-B, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, A.D.; Sanders, J.O.; Liu, R.W.; Cooperman, D.R. The relationship of calcaneal apophyseal ossification and Sanders hand scores to the timing of peak height velocity in adolescents. Bone Joint J. 2015, 97-B, 1710–1717. [Google Scholar] [CrossRef]
- Zaoussis, A.L.; James, J.I.P. The Iliac Apophysis the Evolution of Curves in Scoliosis. J. Bone Joint Surg. 1948, 40-B, 442–453. [Google Scholar] [CrossRef]
- Lonstein, J.E.; Carlson, J.M. The prediction of curve progression in untreated idiopathic scoliosis during growth. J. Bone Joint Surg. Am. 1984, 66, 1061–1071. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Cui, J.J.; DeVries, S.; Nicholson, A.D.; Li, E.; Petit; Kahan, J.B.; Sanders, J.O.; Liu, R.W.; Cooperman, D.R.; et al. Humeral Head Ossification Predicts Peak Height Velocity Timing and Percentage of Growth Remaining in Children. J. Pediatr. Orthop. 2018, 38, e546–e550. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Blythe, C.S.; Reynolds, M.S.; Gregory, L.S. Quantifying the ossification and fusion of the calcaneal apophysis using computed tomography. J. Anat. 2022, 241, 484–499. [Google Scholar] [CrossRef] [PubMed]
- Harrenstein, R.J. Die Skoliose bei Sauglingen und ihre behandlung. Z. Orthop. Chirurgie 1930, 52, 1–40. [Google Scholar]
- Harrenstein, R.J. Das Entstehen von Skoliose infolge einseitiger Zwerchfellähmung. Ztschr. orthop. Chir. 1932, 56, 101. [Google Scholar]
- Mehta, M.H. The natural history of infantile idiopathic scoliosis. In Scoliosis, Proceedings of a Fifth Symposium Held at the Cardiothoracic Institute Brompton Hospital, London, UK, 21–22 September 1976; Zorab, P.A., Ed.; Academic: London, UK, 1977. [Google Scholar]
- Agadir, M.; Burwell, R.G.; Grivas, T.B.; Moulton, A.; Webb, J.K. Progressive infantile idiopathic scoliosis: A longitudinal radiological study with aetiological implications. Proceedings of British Scoliosis Society, 17th Annual Meeting, Co. Down, UK, 19–21 March 1992. [Google Scholar]
- Agadir, M.; Burwell, R.G.; Grivas, T.B.; Moulton, A.; Webb, J.K.; Wemyss-Holden, S.A. Progressive infantile idiopathic scoliosis: A longitudinal radiological study with aetiological implications. Proceedings of British Association of Clinical Anatomists, Winter Scientific Meeting and the Annual General Meeting 1991, Queen Mary and Westfield College, London, UK, 18 December 1991. [Google Scholar]
- Burwell, R.G.; Cole, A.A.; Cook, T.A.; Grivas, T.B.; Kiel, A.W.; Moulton, A.; Thirlwall, A.S.; Upadhyay, S.S.; Webb, J.K.; Wemyss-Holden, S.A.; et al. Pathogenesis of Idiopathic Scoliosis The Nottingham Concept. Acta Orthop Belgica 1992, 58, 33–58. [Google Scholar]
- Burwell, R.G.; Dangerfield, P.H. Etiologic theories of idiopathic scoliosis: Neurodevelopmental concepts to be evaluated. Stud. Health Technol. Inform. 2002, 91, 15–19. [Google Scholar] [PubMed]
- Mehta, M.H. The rib-vertebra angle in the early diagnosis between resolving and progressive infantile scoliosis. J. Bone Jt. Surg. Br. Vol. 1972, 54, 230–243. [Google Scholar] [CrossRef]
- Kristmundsdottir, F.; Burwell, R.G.; James, I. The rib-vertebra angles on the convexity and concavity of the spinal curve in infantile idiopathic scoliosis. Clin. Orthop. Relat. Res. 1985, 201, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; Burwell, R.G.; Webb, J.K. The funnel-shaped upper chest of progressive infantile idiopathic scoliosis (lIS): Significance for rib growth patterns, rib dysplasia and aetiology of the spinal deformity (IIS). Clin. Anat. 1991, 4, 73. [Google Scholar]
- Grivas, T.B.; Burwell, G.R.; Vasiliadis, E.S.; Webb, J.K. A segmental radiological study of the spine and rib--cage in children with progressive infantile idiopathic scoliosis. Scoliosis 2006, 1, 17. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; Burwell, R.G.; Purdue, M.; Webb, J.K.; Moulton, A. The Rib-Cage deformity in infantile idiopathic scoliosis-the funnel-shaped upper chest in relation to specific rotation as a prognostic factor An evaluation of thoracic shape in progressive scoliosis control children during growth. In Faculdade Ciencias Medicas Surface Topography and Spinal Deformity VI; Drerup, A., Hierholzer, Eds.; Gustav Fischer Verlag: Stuttgart, Germany; Jena, Germany; New York, NY, USA, 1992; pp. 93–109. [Google Scholar]
- Perdriolle, R.; Vidal, J. Thoracic idiopathic scoliosis curve evolution and prognosis. Spine 1985, 10, 785–791. [Google Scholar] [CrossRef]
- Grivas, T.B.; Webb, J.K.; Burwell, R.G. Arrest of curve progression by epiphysiodesis and rodding for early onset scoliosis. Proceedings of British Association of Clinical Anatomists Meeting, London, UK, 5 January 1990. [Google Scholar]
- Grivas, T.B.; Webb, J.K.; Burwell, R.G. The effects of epiphysiodesis and rodding for early onset scoliosis. In Proceedings of the 15th Annual Meeting of the British Scoliosis Society, Southampton, UK, 22–24 March 1990. [Google Scholar]
- Grivas, T.B.; Webb, J.K.; Burwell, R.G. Progressive infantile idiopathic scoliosis: A comparison of three methods and the derotation of a combined procedure. In Proceedings of the 25th Annual Meeting of the Scoliosis Research Society, Honolulu, HI, USA, 25–27 September 1990; p. 73. [Google Scholar]
- Coillard, C.; Circo, A.B.; Rivard, C.H. SpineCor treatment for juvenile idiopathic scoliosis: SOSORT award 2010 winner. Scoliosis 2010, 5, 25. [Google Scholar] [CrossRef] [PubMed]
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J. Child Orthop. 2012, 7, 3–9. [Google Scholar] [CrossRef]
- Charles, Y.P.; Daures, J.P.; de Rosa, V.; Diméglio, A. Progression risk of idiopathic juvenile scoliosis during pubertal growth. Spine 2006, 31, 1933–1942. [Google Scholar] [CrossRef]
- Sitoula, P.; Verma, K.; Holmes, L., Jr.; Gabos, P.G.; Sanders, J.O.; Yorgova, P.; Neiss, G.; Rogers, K.; Shah, S.A. Prediction of Curve Progression in Idiopathic Scoliosis: Validation of the Sanders Skeletal Maturity Staging System. Spine 2015, 40, 1006–1013. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.J.; Moe, M.M.; Vaithinathan, R.; Wong, H.K. Curve progression in idiopathic scoliosis: Follow-up study to skeletal maturity. Spine 2009, 34, 697–700. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.P.Y.; Cheung, P.W.H.; Yeng, W.C.; Chan, L.C.K. Does Curve Regression Occur During Underarm Bracing in Patients with Adolescent Idiopathic Scoliosis? Clin. Orthop. Relat. Res. 2020, 478, 334–345. [Google Scholar] [CrossRef]
- Cheung, J.P.Y.; Cheung, P.W.H. Supine flexibility predicts curve progression for patients with adolescent idiopathic scoliosis undergoing underarm bracing. Bone Joint J. 2020, 102-B, 254–260. [Google Scholar] [CrossRef]
- Wong, L.P.K.; Cheung, P.W.H.; Cheung, J.P.Y. Supine correction index as a predictor for brace outcome in adolescent idiopathic scoliosis. Bone Joint J. 2022, 104-B, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Khodaei, M.; Parent, E.C.; Wong, J.; Chan, A.; Coutts, B.; Dlikan, M.; Fehr, B.; Logithasan, V.; Sayed, T.; Mendoza, A.; et al. Identifying predictors of brace treatment outcomes for adolescents or adults with idiopathic scoliosis: A systematic review. Eur. Spine J. 2025. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, A.; Farì, G.; Maccagnano, G.; Riondino, A.; Covelli, I.; Bianchi, F.P.; Tafuri, S.; Piazzolla, A.; Moretti, B. Teenagers’ perceptions of their scoliotic curves. An observational study of comparison between sports people and non- sports people. Muscles Ligaments Tendons J. 2019, 9, 225–235. [Google Scholar] [CrossRef]
- Soucacos, P.N.; Zacharis, K.; Gelalis, J.; Soultanis, K.; Kalos, N.; Beris, A.; Xenakis, T.; Johnson, E.O. Assessment of curve progression in idiopathic scoliosis. Eur. Spine J. 1998, 7, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Modi, H.N.; Suh, S.W.; Song, H.R.; Yang, J.H.; Ting, C.; Hazra, S. Drooping of apical convex rib-vertebral angle in adolescent idiopathic scoliosis of more than 40 degrees: A prognostic factor for progression. J. Spinal Disord. Tech. 2009, 22, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Agabegi, S.S.; Kazemi, N.; Sturm, P.F.; Mehlman, C.T. Natural History of Adolescent Idiopathic Scoliosis in Skeletally Mature Patients: A Critical Review. J. Am. Acad. Orthop. Surg. 2015, 23, 714–723. [Google Scholar] [CrossRef] [PubMed]
- Ohashi, M.; Watanabe, K.; Hirano, T.; Hasegawa, K.; Katsumi, K.; Shoji, H.; Mizouchi, T.; Endo, N. Predicting Factors at Skeletal Maturity for Curve Progression and Low Back Pain in Adult Patients Treated Nonoperatively for Adolescent Idiopathic Scoliosis With Thoracolumbar/Lumbar Curves: A Mean 25-year Follow-up. Spine 2018, 43, E1403–E1411. [Google Scholar] [CrossRef] [PubMed]
- Shea, G.K.-H.; Ng, S.Y.-L.; Zhang, C.; Wang, G. Prognosticating accelerated deterioration in skeletally mature adolescent idiopathic scoliosis curves of 40–50° using uniplanar radiographic measures of axial rotation. Spine Deform. 2024, 12, 1729–1734. [Google Scholar] [CrossRef]
- Dolan, L.A.; Weinstein, S.L.; Abel, M.F.; Bosch, P.P.; Dobbs, M.B.; Farber, T.O.; Halsey, M.F.; Hresko, M.T.; Krengel, W.F.; Mehlman, C.T.; et al. Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Spine Deform. 2019, 7, 890–898e4. [Google Scholar] [CrossRef]
- Wan, H.T.; Wong, D.L.; To, C.H.; Meng, N.; Zhang, T.; Cheung, J.P. 3D prediction of curve progression in adolescent idiopathic scoliosis based on biplanar radiological reconstruction. Bone Jt. Open 2024, 5, 243–251. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ferrero, E.; Lafage, R.; Vira, S.; Rohan, P.Y.; Oren, J.; Delsole, E.; Guigui, P.; Schwab, F.; Lafage, V.; Skalli, W. Three-dimensional reconstruction using stereoradiography for evaluating adult spinal deformity: A reproducibility study. Eur. Spine J. 2017, 26, 2112–2120. [Google Scholar] [CrossRef]
- Garg, B.; Mehta, N.; Bansal, T.; Malhotra, R. EOS imaging: Concept and current applications in spinal disorders. J. Clin. Orthop. Trauma 2020, 11, 786–793. [Google Scholar] [CrossRef] [PubMed]
- Dufvenberg, M.; Charalampidis, A.; Diarbakerli, E.; Öberg, B.; Tropp, H.; Aspberg Ahl, A.; Wezenberg, D.; Hedevik, H.; Möller, H.; Gerdhem, P.; et al. Prognostic model development for risk of curve progression in adolescent idiopathic scoliosis: A prospective cohort study of 127 patients. Acta Orthop. 2024, 95, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Alfraihat, A.; Samdani, A.F.; Balasubramanian, S. Predicting curve progression for adolescent idiopathic scoliosis using random forest model. PLoS ONE 2022, 17, e0273002. [Google Scholar] [CrossRef]
- Grivas, T.B.; Dagas, S.; Lafogianni, S.; Samelis, P.; Polyzois, D. The double rib contour sign (DRCS) of the hemithoracic ribs in the lateral vertebral radiographs Is there a causal relationship with scoliosis? In Proceedings of the 25th Anniversary Symposium on Spine Diseases of "N. Giannestras, P. Smyrnis" Meeting, Patras, Greece, 21–23 May 1999; p. 39. [Google Scholar]
- Grivas, T.B.; Daggas, S.; Polyzois, B.; Samelis, P. The Double Rib Contour Sign (DRCS) in lateral spinal radiographs: Aetiologic implications for scoliosis. Proceeding of the International Research Society of Spinal Deformities Meeting, Clermont, France, 23–26 May 2000; p. 9. [Google Scholar]
- Grivas, T.B.; Dangas, S.; Polyzois, B.D.; Samelis, P. The Double Rib Contour Sign (DRCS) in lateral spinal radiographs: Aetiologic implications for scoliosis. Stud. Health Technol. Inform. 2002, 88, 38–43. [Google Scholar] [PubMed]
- Grivas, T.B. Rib index. Scoliosis 2014, 9, 20. [Google Scholar] [CrossRef] [PubMed]
- Lykissas, M.G.; Sharma, V.; Jain, V.V.; Crawford, A.H. Assessment of Rib Hump Deformity Correction in Adolescent Idiopathic Scoliosis with or Without Costoplasty Using the Double Rib Contour Sign. J. Spinal Disord. Tech. 2015, 28, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; Jevtic, N.; Ljubojevic, D.; Pjanic, S.; Golic, F.; Mazioti, C.; Papagianni, D.; Mamzari, A. Vasiliadis ERib index is a strong surrogate of scoliometric reading in idiopathic scoliosis. Eur. Spine J. 2024, 33, 2451–2456. [Google Scholar] [CrossRef] [PubMed]
- Lebel, A.; Lebel, V. Rib index an objective measure to document changes of the rib hump deformity in a Risser 4 progressive AISpatient treated with the Schroth method. Scoliosis 2014, 9 (Suppl. 1), O18. [Google Scholar] [CrossRef]
- Grivas, T.B. Chapter: Radiological appraisal of thoracic deformity—Improvement or deterioration using the convex/concave rib-hump index (‘double rib contour sign’) in curves Lenke Type 1, 3, 5 and 6. In Scoliosis Research Society • Half-Day Courses; Scoliosis Research Society, Ed.; SRS 2012-2013; Education Committee; pp. 29–30.
- Grivas, T.B.; Triantafyllopoulos, G.; Mazioti, C. Assessment of early RH deformity correction in adolescent idiopathic scoliosis treated with a dynamic derotation brace using the double rib contour sign. Scoliosis 2013, 8 (Suppl. 2), O54. [Google Scholar] [CrossRef]
- Stavropoulos, N.A.; Soultanis, K.C.; Grivas, T.Β.; Starantzis, K.A.; Tsiavos, K.; Sarlikiotis, T.; Mimidis, G.; Papagelopoulos, P.J. Measurement of rib hump deformity correction in adolescent idiopathic scoliosis treated with full screw or hybrid constructs using the double rib contour sign. In Proceedings of the 7o Panhellenic Spinal Meeting, Thessaloniki, Greece, 31 October–2 November 2013. [Google Scholar]
- Hwang, S.W.; Samdani, A.F.; Marks, M.; Bastrom, T.; Garg, H.; Lonner, B.; Bennett, J.T.; Pahys, J.; Shah, S.; Miyanji, F.; et al. Five-year clinical and radiographic outcomes using pedicle screw only constructs in the treatment of adolescent idiopathic scoliosis. Eur. Spine J. 2013, 22, 1292–1299. [Google Scholar] [CrossRef] [PubMed]
- Haber, L.L.; Hughes, J.D.; Womack, E.D.; Roberson, R.M.; Wrigh, P.B. Screw versus hybrid constructs for flexible thoracic curves in adolescent idiopathic scoliosis: A prospective, randomized study. Spine Deform. 2014, 2, 367–373. [Google Scholar] [CrossRef]
- Stavropoulos, N.A.; Soultanis, K.C.; Grivas, T.B.; Tsiavos, K.; Starantzis, K.; Sarlikiotis, T.; Karamanis, E.; Papagelopoulos, P.J. Measurement of RH Deformity Correction in Adolescent Idiopathic Scoliosis Treated with Full Screw or Hybrid Constructs Using the Double Rib Contour Sign; 15th EFORT Congress: London, UK, 2014. [Google Scholar]
- Igoumenou, V.G.; Megaloikonomos, P.D.; Tsiavos, K.; Georgopoulos, G.; Liontos, M.; Mavrogenis, A.F.; Grivas, T.B.; Soultanis, K.; Papagelopoulos, P.J. Postoperative rib hump deformity correction in patients with adolescent idiopathic scoliosis. Comparison of a three generations spinal fusion systems. In Proceedings of the Combined Meeting of the International Research Society of Spinal Deformities and the Society on Scoliosis Orthopaedic and Rehabilitation Treatment, Banff, AB, Canada, 25–28 May 2016. [Google Scholar]
- Igoumenou, V.G.; Melamud, E.; Vazifehdan, F.; Megaloikonomos, P.D.; Grivas, T.B.; Mavrogenis, A.F.; Papagelopoulos, P.J.; Soultanis, K. Rib Hump Deformity Correction in Patients with Adolescent Idiopathic Scoliosis: A Comparison of Three Spinal Fusion Systems. J. Long Term Eff. Med. Implant. 2021, 31, 81–87. [Google Scholar] [CrossRef]
- Easwar, T.R.; Hong, J.-Y.; Yang, J.H.; Suh, S.W.; Modi, H.N. Does lateral vertebral translation correspond to Cobb angle and relate in the same way to axial vertebral rotation and rib hump index? A radiographic analysis on idiopathic scoliosis. Eur. Spine J. 2011, 20, 1095–1105. [Google Scholar]
- Harris, J.A.; Mayer, O.H.; Shah, S.A.; Campbell, R.M., Jr.; Balasubramanian, S. A comprehensive review of thoracic deformity parameters in scoliosis. Eur. Spine J. 2014, 23, 2594–2602. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; Jevtic, N.; Ljubojevic, D.; Pjanic, S.; Golic, F.; Vasiliadis, E. Segmental Rib Index and Spinal Deformity: Scoliogenic Implications. Healthcare 2023, 11, 3004. [Google Scholar] [CrossRef] [PubMed]
- Soultanis, K.C.; Stavropoulos, N.A.; Grivas, T.B.; Tsiavos, K.; Starantzis, K.; Papagelopoulos, P.J. Rib hump deformity assessment using the rib index in adolescent idiopathic scoliotics treated with full screw or hybrid constructs: Aetiological implications. Scoliosis 2015, 10 (Suppl. S2), S10. [Google Scholar] [CrossRef] [PubMed]
- Sevastik, J.A.; Aaro, S.; Normelli, H. Scoliosis: Experimental and clinical studies. Clin. Orthop. Relat. Res. 1984, 191, 27–34. [Google Scholar] [CrossRef]
- Normelli, H.; Sevastik, J.; Wallberg, H. The thermal emission from the skin and the vascularity of the breasts in normal and scoliotic girls. Spine 1986, 11, 405–408. [Google Scholar] [CrossRef]
- Sevastik, J.A.; Aaro, S.; Lindholm, S.T.; Dalhborn, M. Experimental scoliosis in growing rabbits by operations on the rib cage. Clin. Orthop. Relat. Res. 1987, 136, 282–286. [Google Scholar]
- Agadir, M.; Sevastik, B.; Sevastik, J.A.; Persson, A.; Isberg, B. Induction of scoliosis in the growing rabbit by unilateral rib-growth stimulation. Spine 1988, 13, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Normelli, H.; Sevastik, J.A.; Ljung, G.; Jönsson-Söderström, A.M. The symmetry of the breasts in normal and scoliotic girls. Spine 1986, 11, 749–752. [Google Scholar] [CrossRef]
- Sevastik, J.; Agadir, M.; Sevastik, B. Effects of rib elongation on the spine: I. Distortion of the vertebral alignment in the rabbit. Spine 1990, 15, 822–825. [Google Scholar] [CrossRef] [PubMed]
- Sevastik, J.; Agadir, M.; Sevastik, B. Effects of rib elongation on the spine: II. Correction of scoliosis in the rabbit. Spine 1990, 15, 826–829. [Google Scholar] [CrossRef]
- Agadir, M.; Sevastik, B.; Reinholt, F.P.; Perbeck, L.; Sevastik, J. Vascular Changes in the Chest Wall After Unilateral Resection of the Intercostal Nerves in the Growing Rabbit. J. Orthop. Res. 1990, 8, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Sevastik, B.; Xiong, B.; Lundberg, A.; Sevastik, J.A. In vitro opto-electronic analysis of 3-D segmental vertebral movements during gradual rib lengthening in the pig. Acta Orthop. Belg. 1995, 61, 218–225. [Google Scholar]
- Gréalou, L.; Aubin, C.E.; Sevastik, J.A.; Labelle, H. Simulations of rib cage surgery for the management of scoliotic deformities. Stud. Health Technol. Inform. 2002, 88, 345–349. [Google Scholar]
- Sevastik, J.A. Dysfunction of the autonomic nerve system (ANS) in the aetiopathogenesis of adolescent idiopathic scoliosis. Stud. Health Technol. Inform. 2002, 88, 20–23. [Google Scholar]
- Sevastik, J.A.; Burwell, R.G.; Dangerfild, P.H. A new concept for the etiopathogenesis of the thoracospinal deformity of idiopathic scoliosis: Summary of an electronic focus group debate of the IBSE. Eur. Spine J. 2003, 12, 440–450. [Google Scholar] [CrossRef]
- Sevastik, J.A. Right convex thoracic female adolescent scoliosis in the light of the thoracospinal concept. Stud. Health Technol. Inform. 2006, 123, 552–558. [Google Scholar]
- Grivas, T.B.; Vasiliadis, E.S.; Mihas, C.; Savvidou, O. The effect of growth on the correlation between the spinal and rib cage deformity: Implications on idiopathic scoliosis pathogenesis. Scoliosis 2007, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- Doi, T.; Matsumoto, Y.; Tono, O.; Tarukado, K.; Harimaya, K.; Okada, S.; Kubota, K.; Hayashida, M.; Iwamoto, Y. A shallow chest correlates with the aortic position in the normal spine: Features resembling those observed in structural scoliosis. Scoliosis 2014, 9, 14. [Google Scholar] [CrossRef] [PubMed]


| Cobb Degrees | 0–10 + hump | 11–15 | 16–20 | 21–25 | 26–30 | 31–35 | 36–40 | 41–45 | 46–50 | Over 50 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Infantile | Min | Ob6 | Ob6 | Ob3 | SSB | SSB | SSB | SSB | SSB | PTRB | FTRB | |
| Max | Ob3 | Ob3 | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Juvenile | Min | Ob3 | Ob3 | Ob3 | SSB | SSB | SSB | PTRB | PTRB | PTRB | FTRB | |
| Max | PSE | PSE | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Adolescent | Risser 0 | Min | Ob6 | Ob6 | Ob3 | PSE | PSE | SSB | PTRB | PTRB | PTRB | FTRB |
| Max | Ob3 | PSE | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Risser 1 | Min | Ob6 | Ob6 | Ob3 | PSE | PSE | SSB | PTRB | PTRB | PTRB | FTRB | |
| Max | Ob3 | PSE | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Risser 2 | Min | Ob8 | Ob6 | Ob3 | PSE | PSE | SSB | SSB | SSB | SSB | FTRB | |
| Max | Ob6 | PSE | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Risser 3 | Min | Ob12 | Ob6 | Ob6 | Ob6 | PSE | SSB | SSB | SSB | SSB | FTRB | |
| Max | Ob6 | PSE | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Risser 4 | Min | No | Ob6 | Ob6 | Ob6 | Ob6 | Ob6 | Ob6 | Ob6 | SSB | FTRB | |
| Max | Ob12 | PSE | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Risser 4–5 | Min | No | Ob6 | Ob6 | Ob6 | Ob6 | Ob6 | Ob6 | Ob6 | SSB | FTRB | |
| Max | Ob12 | PSE | PTRB | FTRB | FTRB | FTRB | FTRB | FTRB | Su | Su | ||
| Adult | No pain | Min | No | No | No | No | No | No | No | No | Ob12 | Ob12 |
| Max | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob6 | Ob6 | ||
| Chronic Pain | Min | No | PSE | PSE | PSE | PSE | PSE | PSE | PSE | PSE | PSE | |
| Max | PTRB | PTRB | PTRB | PTRB | PTRB | Su | Su | Su | Su | Su | ||
| Elderly | No pain | Min | No | No | No | No | No | No | No | No | Ob12 | Ob12 |
| Max | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob12 | Ob6 | Ob6 | ||
| Chronic Pain | Min | No | PSE | PSE | PSE | PSE | PSE | PSE | PSE | PSE | PSE | |
| Max | PTRB | PTRB | PTRB | PTRB | PTRB | PTRB | PTRB | PTRB | Su | Su | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grivas, T.B.; Vasiliadis, E.; Soultanis, K.; Lykissas, M.; Katzouraki, G.; Sekouris, N.; Lykouris, D.; Mazioti, C.; Mamzeri, A.; Papagianni, D.; et al. Idiopathic Scoliosis Progression: Presenting Rib and Segmental Rib Index as Predictors—A Literature Review. Med. Sci. 2025, 13, 62. https://doi.org/10.3390/medsci13020062
Grivas TB, Vasiliadis E, Soultanis K, Lykissas M, Katzouraki G, Sekouris N, Lykouris D, Mazioti C, Mamzeri A, Papagianni D, et al. Idiopathic Scoliosis Progression: Presenting Rib and Segmental Rib Index as Predictors—A Literature Review. Medical Sciences. 2025; 13(2):62. https://doi.org/10.3390/medsci13020062
Chicago/Turabian StyleGrivas, Theodoros B., Elias Vasiliadis, Konstantinos Soultanis, Marios Lykissas, Galateia Katzouraki, Nikolaos Sekouris, Dimitrios Lykouris, Christina Mazioti, Aristea Mamzeri, Despina Papagianni, and et al. 2025. "Idiopathic Scoliosis Progression: Presenting Rib and Segmental Rib Index as Predictors—A Literature Review" Medical Sciences 13, no. 2: 62. https://doi.org/10.3390/medsci13020062
APA StyleGrivas, T. B., Vasiliadis, E., Soultanis, K., Lykissas, M., Katzouraki, G., Sekouris, N., Lykouris, D., Mazioti, C., Mamzeri, A., Papagianni, D., Potamiti, E., Kastrinis, A., & Theodosopoulos, E. (2025). Idiopathic Scoliosis Progression: Presenting Rib and Segmental Rib Index as Predictors—A Literature Review. Medical Sciences, 13(2), 62. https://doi.org/10.3390/medsci13020062