Exploring Treatment Protocol Adherence and Variations in Paroxysmal Supraventricular Tachycardia in the Emergency Department: A Multi-Center Cohort Study
Abstract
1. Background
2. Methods
2.1. Study Design and Setting
2.2. Inclsion and Exclusion Criteria
2.3. Major Outcomes
2.4. Statistical Analysis
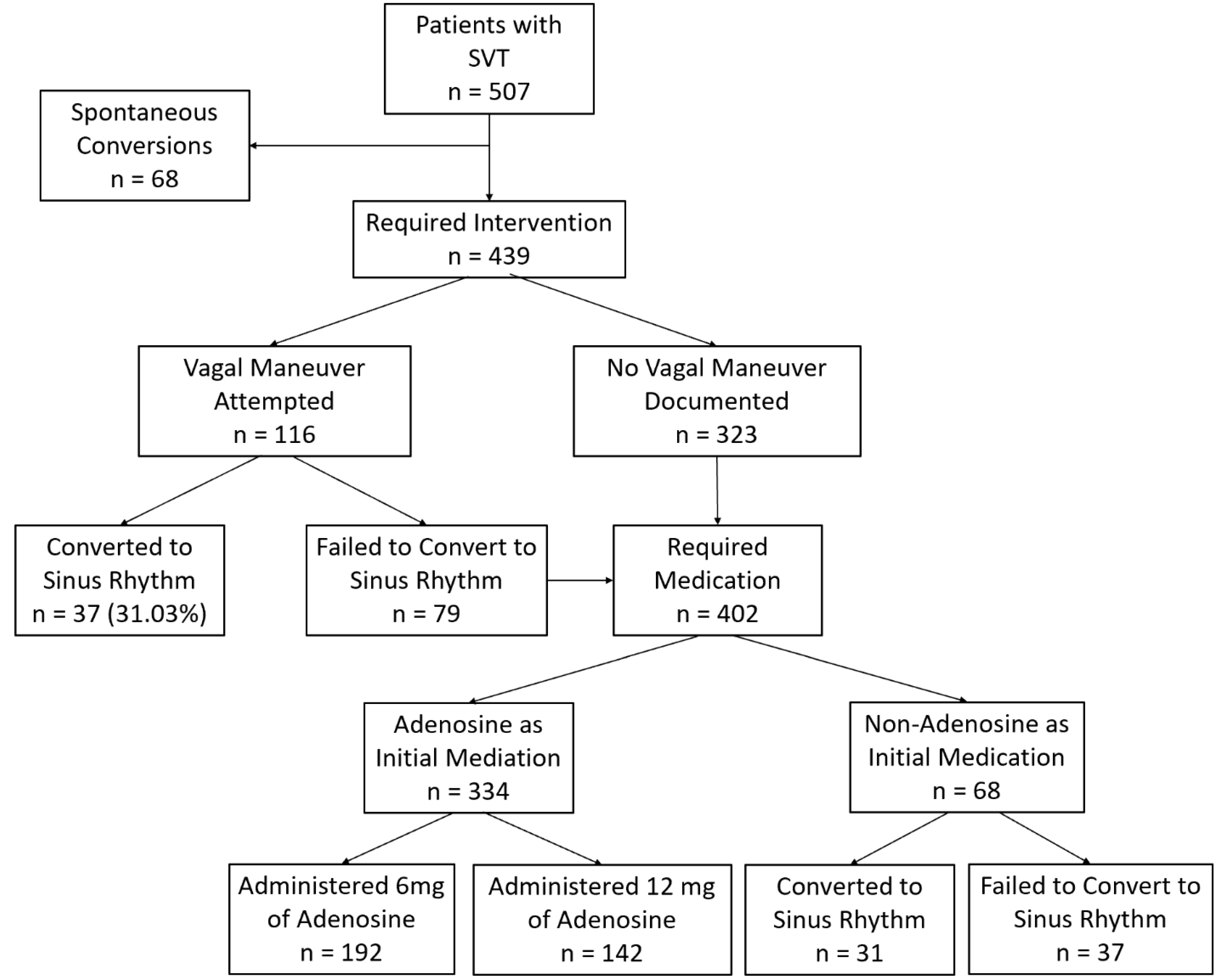
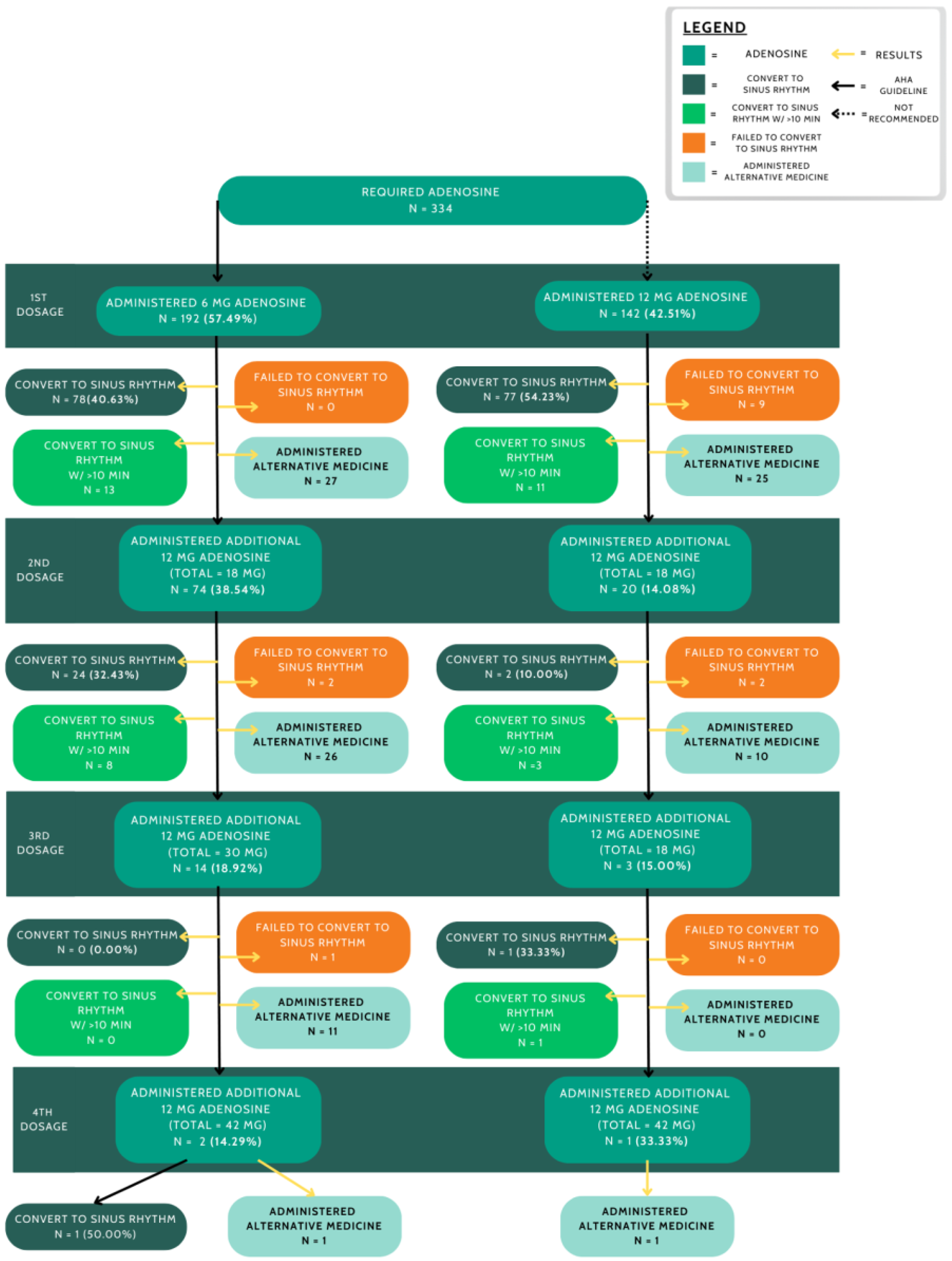
3. Results
Logistic Regression Analysis
4. Discussion
4.1. Vagal Maneuvers and Documentation
4.2. Adenosine Dosage and Treatment Efficacy
4.3. Non-Adenosine Pharmacological Treatments
4.4. Key Predictors and Clinical Implications
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Katritsis, D.G.; Josephson, M.E. Differential diagnosis of regular, narrow-QRS tachycardias. Heart Rhythm 2015, 12, 1667–1676. [Google Scholar] [CrossRef]
- Colucci, R.A.; Silver, M.J.; Shubrook, J. Common types of supraventricular tachycardia: Diagnosis and management. Am. Fam. Physician 2010, 82, 942–952. [Google Scholar] [PubMed]
- Erdinler, I.; Okmen, E.; Oguz, E.; Akyol, A.; Gurkan, K.; Ulufer, T. Differentiation of narrow QRS complex tachycardia types using the 12-lead electrocardiogram. Ann. Noninvasive Electrocardiol. 2002, 7, 120–126. [Google Scholar] [CrossRef]
- Ray, L.; Geier, C.; DeWitt, K.M. Pathophysiology and treatment of adults with arrhythmias in the emergency department, part 1: Atrial arrhythmias. Am. J. Health Syst. Pharm. 2023, 80, 1039–1055. [Google Scholar] [CrossRef]
- Yetkin, E.; Ozturk, S.; Cuglan, B.; Turhan, H. Clinical presentation of paroxysmal supraventricular tachycardia: Evaluation of usual and unusual symptoms. Cardiovasc. Endocrinol. Metab. 2020, 9, 153–158. [Google Scholar] [CrossRef]
- Nasir, M.; Sturts, A.; Sturts, A. Common Types of Supraventricular Tachycardia: Diagnosis and Management. Am. Fam. Physician 2023, 107, 631–641. [Google Scholar] [PubMed]
- Rehorn, M.; Sacks, N.C.; Emden, M.R.; Healey, B.; Preib, M.T.; Cyr, P.L.; Pokorney, S.D. Prevalence and incidence of patients with paroxysmal supraventricular tachycardia in the United States. J. Cardiovasc. Electrophysiol. 2021, 32, 2199–2206. [Google Scholar] [CrossRef]
- Page, R.L.; Joglar, J.A.; Caldwell, M.A.; Calkins, H.; Conti, J.B.; Deal, B.J.; Estes, N.A.M.; Field, M.E.; Goldberger, Z.D.; Hammill, S.C.; et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients with Supraventricular Tachycardia. Circulation 2016, 133, e471–e505. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.S.; Scheinman, M.M.; Chien, W.W.; Cohen, T.J.; Lesh, M.D.; Griffin, J.C. Patients with supraventricular tachycardia presenting with aborted sudden death: Incidence, mechanism and long-term follow-up. J. Am. Coll. Cardiol. 1991, 18, 1711–1719. [Google Scholar] [CrossRef]
- Kotadia, I.D.; Williams, S.E.; O’Neill, M. Supraventricular tachycardia: An overview of diagnosis and management. Clin. Med. 2020, 20, 43–47. [Google Scholar] [CrossRef]
- Ebrille, E.; Contreras-Valdes, F.M.; Zimetbaum, P.J. Hemodynamic response to supraventricular tachycardia in a patient with hypertrophic cardiomyopathy. Heart Rhythm Case Rep. 2019, 5, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Al-Khatib, S.M.; Page, R.L. Acute Treatment of Patients with Supraventricular Tachycardia. JAMA Cardiol. 2016, 1, 483–485. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Jung, J.Y.; Lee, S.U.; Park, J.W.; Choi, J.Y. Delayed adenosine therapy is associated with the refractory supraventricular tachycardia in children. Am. J. Emerg. Med. 2020, 38, 2291–2296. [Google Scholar] [CrossRef] [PubMed]
- Brugada, J.; Katritsis, D.G.; Arbelo, E.; Arribas, F.; Bax, J.J.; Blomström-Lundqvist, C.; Calkins, H.; Corrado, D.; Deftereos, S.G.; Diller, G.P.; et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC): Developed in collaboration with the Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 2020, 41, 655–720. [Google Scholar] [CrossRef]
- Patti, L.; Horenstein, M.S.; Ashurst, J.V. Supraventricular Tachycardia. Available online: https://www.ncbi.nlm.nih.gov/books/NBK441972/ (accessed on 13 March 2025).
- Lundqvist, C.B.; Potpara, T.S.; Malmborg, H. Supraventricular Arrhythmias in Patients with Adult Congenital Heart Disease. Arrhythm Electrophysiol. Rev. 2017, 6, 42–49. [Google Scholar] [CrossRef]
- Shakespeare, C.F.; Anderson, M.; Camm, A.J. Pathophysiology of supraventricular tachycardia. Eur. Heart J. 1993, 14 (Suppl. E), 2–8. [Google Scholar] [CrossRef]
- Hafeez, Y.; Quintanilla Rodriguez, B.S.; Ahmed, I.; Grossman, S.A. Paroxysmal Supraventricular Tachycardia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Al-Salamah, T.; AlAgeel, M.; Alblaihed, L. Narrow Complex Tachycardias. Emerg. Med. Clin. N. Am. 2022, 40, 717–732. [Google Scholar] [CrossRef]
- Mustafa, S.J.; Morrison, R.R.; Teng, B.; Pelleg, A. Adenosine receptors and the heart: Role in regulation of coronary blood flow and cardiac electrophysiology. Handb. Exp. Pharmacol. 2009, 193, 161–188. [Google Scholar] [CrossRef]
- Layland, J.; Carrick, D.; Lee, M.; Oldroyd, K.; Berry, C. Adenosine: Physiology, pharmacology, and clinical applications. JACC Cardiovasc. Interv. 2014, 7, 581–591. [Google Scholar] [CrossRef]
- Pantely, G.A.; Bristow, J.D. Adenosine. Renewed interest in an old drug. Circulation 1990, 82, 1854–1856. [Google Scholar] [CrossRef]
- Riccardi, A.; Arboscello, E.; Ghinatti, M.; Minuto, P.; Lerza, R. Adenosine in the treatment of supraventricular tachycardia: 5 years of experience (2002–2006). Am. J. Emerg. Med. 2008, 26, 879–882. [Google Scholar] [CrossRef]
- Alabed, S.; Sabouni, A.; Providencia, R.; Atallah, E.; Qintar, M.; Chico, T.J. Adenosine versus intravenous calcium channel antagonists for supraventricular tachycardia. Cochrane Database Syst. Rev. 2017, 10, CD005154. [Google Scholar] [CrossRef]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef]
- Krug, N.; Baize, P.; Barre, S.; Barnes, R.; Weigartz, K. Comparison of initial adenosine dose conversion rate for supraventricular tachycardia in the emergency department. Am. J. Emerg. Med. 2024, 85, 117–122. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Hosmer, D.W.; Hosmer, T.; Le Cessie, S.; Lemeshow, S. A comparison of goodness-of-fit tests for the logistic regression model. Stat. Med. 1997, 16, 965–980. [Google Scholar] [CrossRef]
- DiMarco, J.P.; Miles, W.; Akhtar, M.; Milstein, S.; Sharma, A.D.; Platia, E.; McGovern, B.; Scheinman, M.M.; Govier, W.C. Adenosine for paroxysmal supraventricular tachycardia: Dose ranging and comparison with verapamil. Assessment in placebo-controlled, multicenter trials. The Adenosine for PSVT Study Group. Ann. Intern. Med. 1990, 113, 104–110. [Google Scholar] [CrossRef]
- Delaney, B.; Loy, J.; Kelly, A.M. The relative efficacy of adenosine versus verapamil for the treatment of stable paroxysmal supraventricular tachycardia in adults: A meta-analysis. Eur. J. Emerg. Med. 2011, 18, 148–152. [Google Scholar] [CrossRef]
- Lim, S.H.; Anantharaman, V.; Teo, W.S.; Chan, Y.H. Slow infusion of calcium channel blockers compared with intravenous adenosine in the emergency treatment of supraventricular tachycardia. Resuscitation 2009, 80, 523–528. [Google Scholar] [CrossRef]
- Lim, S.H.; Anantharaman, V.; Teo, W.S. Slow-infusion of calcium channel blockers in the emergency management of supraventricular tachycardia. Resuscitation 2002, 52, 167–174. [Google Scholar] [CrossRef]
- Brady, W.J., Jr.; DeBehnke, D.J.; Wickman, L.L.; Lindbeck, G. Treatment of out-of-hospital supraventricular tachycardia: Adenosine vs verapamil. Acad. Emerg. Med. 1996, 3, 574–585. [Google Scholar] [CrossRef]
- Furlong, R.; Gerhardt, R.T.; Farber, P.; Schrank, K.; Willig, R.; Pittaluga, J. Intravenous adenosine as first-line prehospital management of narrow-complex tachycardias by EMS personnel without direct physician control. Am. J. Emerg. Med. 1995, 13, 383–388. [Google Scholar] [CrossRef] [PubMed]
- McCabe, J.L.; Adhar, G.C.; Menegazzi, J.J.; Paris, P.M. Intravenous adenosine in the prehospital treatment of paroxysmal supraventricular tachycardia. Ann. Emerg. Med. 1992, 21, 358–361. [Google Scholar] [CrossRef] [PubMed]
- Madsen, C.D.; Pointer, J.E.; Lynch, T.G. A comparison of adenosine and verapamil for the treatment of supraventricular tachycardia in the prehospital setting. Ann. Emerg. Med. 1995, 25, 649–655. [Google Scholar] [CrossRef]
- Parker, R.B.; McCollam, P.L. Adenosine in the episodic treatment of paroxysmal supraventricular tachycardia. Clin. Pharm. 1990, 9, 261–271. [Google Scholar]
- Rankin, A.C.; Brooks, R.; Ruskin, J.N.; McGovern, B.A. Adenosine and the treatment of supraventricular tachycardia. Am. J. Med. 1992, 92, 655–664. [Google Scholar] [CrossRef]
- Corbacioglu, S.K.; Uzunosmanoglu, H.; Karaarslan, F.N.; Dagar, S.; Emektar, E.; Cevik, Y. The effect of patient weight on the success of converting sinus rhythm in patients with PSVT treated with standard dose adenosine. Am. J. Emerg. Med. 2023, 69, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Cabalag, M.S.; Taylor, D.M.; Knott, J.C.; Buntine, P.; Smit, D.; Meyer, A. Recent Caffeine Ingestion Reduces Adenosine Efficacy in the Treatment of Paroxysmal Supraventricular Tachycardia. Acad. Emerg. Med. 2010, 17, 44–49. [Google Scholar] [CrossRef]
- Lim, S.H.; Anantharaman, V.; Teo, W.S.; Goh, P.P.; Tan, A. Comparison of Treatment of Supraventricular Tachycardia by Valsalva Maneuver and Carotid Sinus Massage. Ann. Emerg. Med. 1998, 31, 30–35. [Google Scholar] [CrossRef]
- Dougherty, A.H.; Jackman, W.M.; Naccarelli, G.V.; Friday, K.J.; Dias, V.C. Acute conversion of paroxysmal supraventricular tachycardia with intravenous diltiazem. IV Diltiazem Study Group. Am. J. Cardiol. 1992, 70, 587–592. [Google Scholar] [CrossRef]
- Zhang, Y.; Wernly, B.; Cao, X.; Mustafa, S.J.; Tang, Y.; Zhou, Z. Adenosine and adenosine receptor-mediated action in coronary microcirculation. Basic. Res. Cardiol. 2021, 116, 22. [Google Scholar] [CrossRef]
- Ballesteros-Yáñez, I.; Castillo, C.A.; Merighi, S.; Gessi, S. The Role of Adenosine Receptors in Psychostimulant Addiction. Front. Pharmacol. 2018, 8, 320873. [Google Scholar] [CrossRef] [PubMed]
- Luscher, T.F.; Richard, V.; Tschudi, M.; Yang, Z.H.; Boulanger, C. Endothelial control of vascular tone in large and small coronary arteries. J. Am. Coll. Cardiol. 1990, 15, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Khayat, M.T.; Nayeem, M.A. The Role of Adenosine A(2A) Receptor, CYP450s, and PPARs in the Regulation of Vascular Tone. Biomed. Res. Int. 2017, 2017, 1720920. [Google Scholar] [CrossRef]
- Singh Patidar, B.; Meena, A.; Kumar, M.; Menon, B.; Rohil, V.; Kumar Bansal, S. Adenosine Metabolism in COPD: A Study on Adenosine Levels, 5’-Nucleotidase, Adenosine Deaminase and Its Isoenzymes Activity in Serum, Lymphocytes and Erythrocytes. J. Chronic Obstr. Pulm. Dis. 2018, 15, 559–571. [Google Scholar] [CrossRef] [PubMed]
- Robson, S.C.; Schuppan, D. Adenosine: Tipping the balance towards hepatic steatosis and fibrosis. J. Hepatol. 2010, 52, 941–943. [Google Scholar] [CrossRef]
- Oyarzun, C.; Garrido, W.; Alarcon, S.; Yanez, A.; Sobrevia, L.; Quezada, C.; San Martin, R. Adenosine contribution to normal renal physiology and chronic kidney disease. Mol. Asp. Med. 2017, 55, 75–89. [Google Scholar] [CrossRef]
- Cheng, L.; Eilbert, W. High-dose adenosine for treatment of refractory paroxysmal supraventricular tachycardia. Am. J. Emerg. Med. 2020, 38, 1541.e3–1541.e4. [Google Scholar] [CrossRef]
| Characteristic | Total Patients Requiring Medication (n = 402) | 6 mg Adenosine (n = 192) | 12 mg Adenosine (n = 142) | Alternative Treatment (n = 68) |
|---|---|---|---|---|
| Age, mean (SD) | 58.87 (15.97) | 58.28 (15.36) | 56.54 (16.20) | 65.6 (15.92) |
| Male gender, n (%) | 173 (43.03%) | 78 (40.21%) | 62 (43.66%) | 34 (50%) |
| Race, n (%) | ||||
| Asian | 9 (2.24%) | 4 (2.06%) | 0 (0%) | 5 (7.35%) |
| Black | 77 (19.15%) | 39 (20.10%) | 29 (20.42%) | 9 (13.24%) |
| White | 308 (76.62%) | 148 (76.29%) | 109 (76.76%) | 53 (77.94%) |
| Other | 8 (1.99%) | 3 (1.55%) | 4 (2.82%) | 1 (1.47%) |
| Hispanic ethnicity, n (%) | 50 (12.44%) | 25 (12.89%) | 20 (14.08%) | 6 (8.82%) |
| Comorbidities, n (%) | ||||
| Diabetes mellitus | 107 (26.62%) | 43 (22.16%) | 42 (29.58%) | 23 (33.82%) |
| Hypertension | 211 (52.49%) | 93 (47.94%) | 75 (52.82%) | 44 (64.71%) |
| Smoking history | 171 (42.54%) | 79 (40.72%) | 61 (42.96%) | 31 (45.59%) |
| Coronary artery disease | 56 (13.93%) | 21 (10.82%) | 25 (17.61%) | 11 (16.18%) |
| Cancer | 53 (13.18%) | 23 (11.86%) | 12 (8.45%) | 10 (14.71%) |
| Initial vital signs, mean (SD) | ||||
| Systolic blood pressure (mmHg) | 128.5 (27.6) | 126 (35.5) | 122 (35.5) | 129 (30) |
| Diastolic blood pressure (mmHg) | 83 (20) | 83 (26.25) | 79 (29) | 81 (23) |
| Heart rate (bpm) | 150.6 (46) | 165 (66) | 167 (77) | 131 (73.5) |
| Laboratory values, mean (SD) | ||||
| Serum sodium | 138 (5) | 139 (5) | 138 (4) | 138 (4.5) |
| Serum potassium | 3.9 (0.6) | 4 (0.6) | 3.9 (0.6) | 3.9 (0.6) |
| Serum creatinine | 1.07 (0.45) | 1.1(0.49) | 1.07 (0.46) | 1.09 (0.36) |
| Hemoglobin | 13.9 (2.8) | 14.2 (2.8) | 13.7 (2.7) | 13.8 (1.35) |
| White blood cell count | 9.4 (4.55) | 9.8 (4.2) | 9.25 (4.65) | 9.2 (4.93) |
| Variable | Odds Ratio (95% CI) | p-Value |
|---|---|---|
| ST EKG changes | 0.51 (0.2, 1.28) | 0.15 |
| Age | 1.04 (1.0, 1.07) | 0.05 |
| Smoking history | 3.37 (1.09, 10.41) | 0.04 |
| DM | 10.25 (0.66, 158.39) | 0.10 |
| HTN | 0.65 (0.21, 2.03) | 0.46 |
| CAD | 372.78 (0.54, 2.59 × 105) | 0.08 |
| CHF | 0.13 (0.02, 0.74) | 0.02 |
| COPD | 0.08 (0.01, 0.54) | <0.01 |
| CVA | 8.05 × 103 (10.13, 6.39 × 106) | <0.01 |
| Cirrhosis | 0.0 (0.0, 0.09) | <0.01 |
| CKD | 0.05 (0.0, 0.5) | 0.01 |
| Dementia | 0.0 (0.0, inf) | 0.99 |
| Cancer | 147.53 (2.09, 1.04 × 104) | 0.02 |
| Heart rate | 1.01 (1.0, 1.02) | 0.09 |
| Serum BUN | 0.87 (0.81, 0.93) | <0.001 |
| Serum K | 8.78 (2.76, 28.0) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ku, K.; Healy, J.; Lee, C.A.; Khan, M.; Chao, K.D.; Hassan, S.; Tzeng, C.-F.T.; Hsieh, Y.-L.; Shedd, A.; Bhakta, T.; et al. Exploring Treatment Protocol Adherence and Variations in Paroxysmal Supraventricular Tachycardia in the Emergency Department: A Multi-Center Cohort Study. Med. Sci. 2025, 13, 58. https://doi.org/10.3390/medsci13020058
Ku K, Healy J, Lee CA, Khan M, Chao KD, Hassan S, Tzeng C-FT, Hsieh Y-L, Shedd A, Bhakta T, et al. Exploring Treatment Protocol Adherence and Variations in Paroxysmal Supraventricular Tachycardia in the Emergency Department: A Multi-Center Cohort Study. Medical Sciences. 2025; 13(2):58. https://doi.org/10.3390/medsci13020058
Chicago/Turabian StyleKu, Kevin, Jack Healy, Christian A. Lee, Maha Khan, Kevin D. Chao, Saleh Hassan, Ching-Fang Tiffany Tzeng, Yu-Lin Hsieh, Andrew Shedd, Toral Bhakta, and et al. 2025. "Exploring Treatment Protocol Adherence and Variations in Paroxysmal Supraventricular Tachycardia in the Emergency Department: A Multi-Center Cohort Study" Medical Sciences 13, no. 2: 58. https://doi.org/10.3390/medsci13020058
APA StyleKu, K., Healy, J., Lee, C. A., Khan, M., Chao, K. D., Hassan, S., Tzeng, C.-F. T., Hsieh, Y.-L., Shedd, A., Bhakta, T., Hassani, D., & Chou, E. H. (2025). Exploring Treatment Protocol Adherence and Variations in Paroxysmal Supraventricular Tachycardia in the Emergency Department: A Multi-Center Cohort Study. Medical Sciences, 13(2), 58. https://doi.org/10.3390/medsci13020058






