Predictive Factors of Therapy-Related Cardiovascular Events in Patients with Lymphoma Receiving Anthracyclines
Abstract
1. Background
2. Material and Methods
2.1. Participants and Study Metods
2.2. Inclusion, Exclusion Criteria, and Study Period
2.3. Exposure and Covariates
2.4. Outcomes
2.5. Data Collection, Storage, and Ethics
2.6. Stastical Analysis
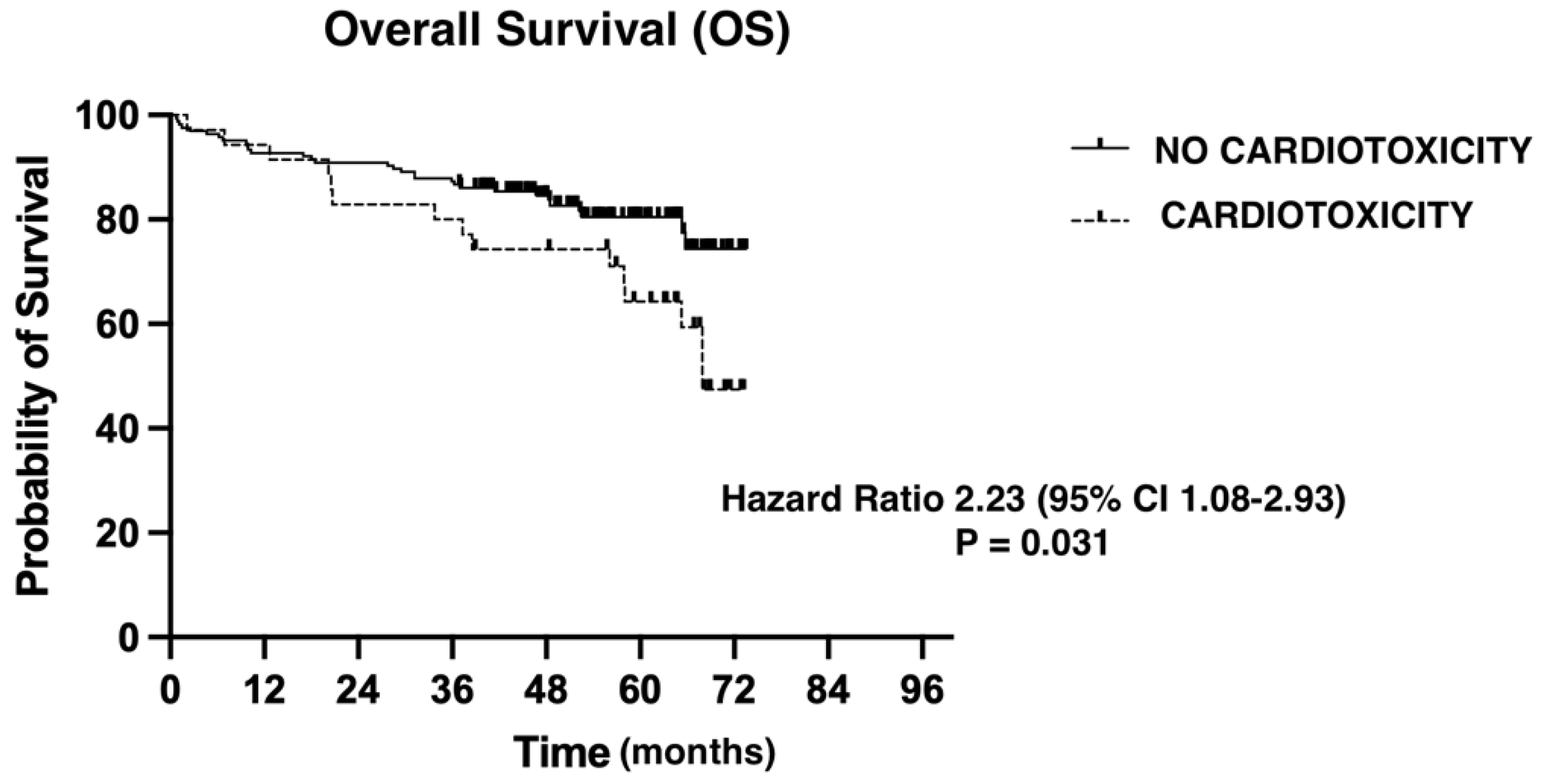
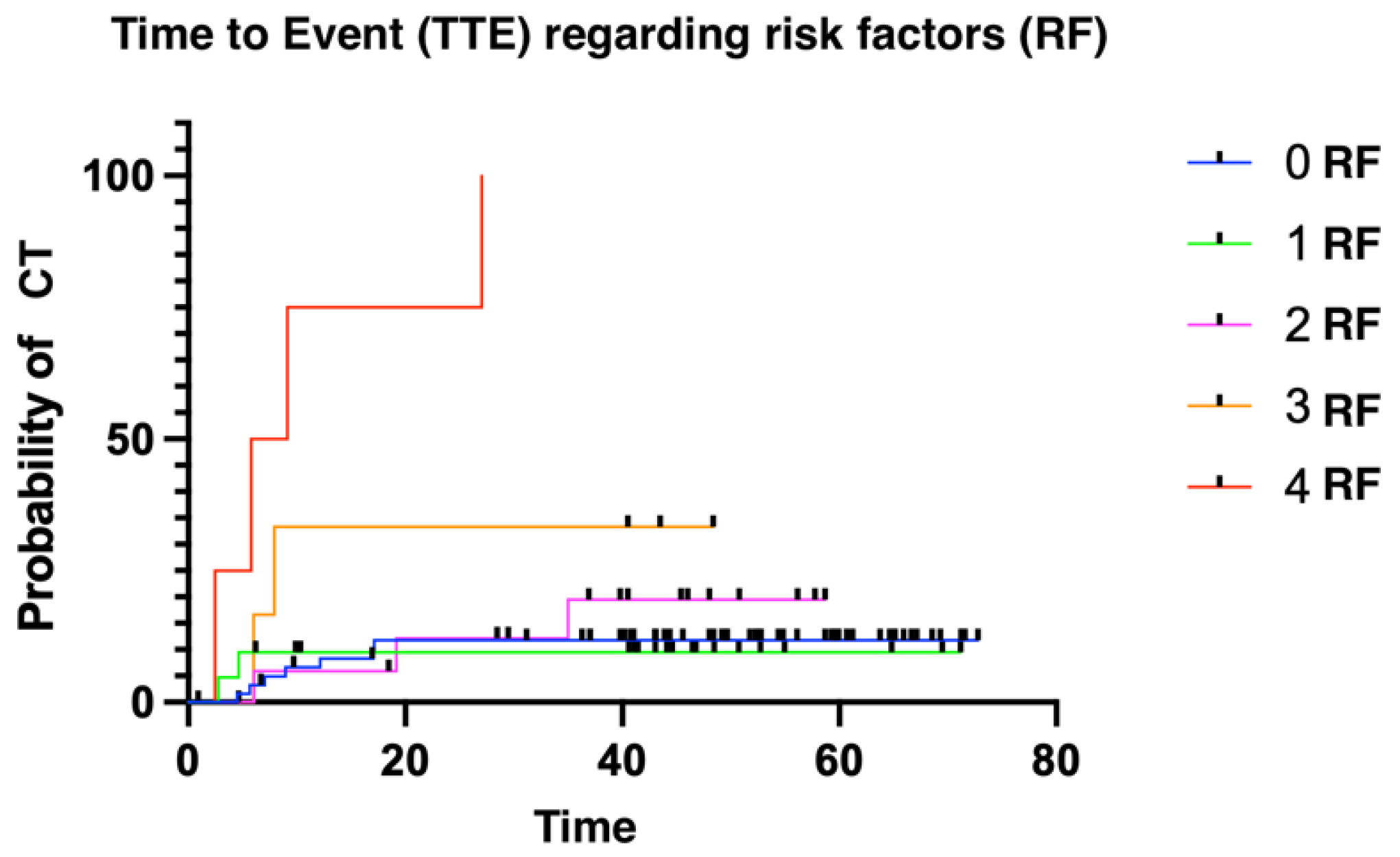
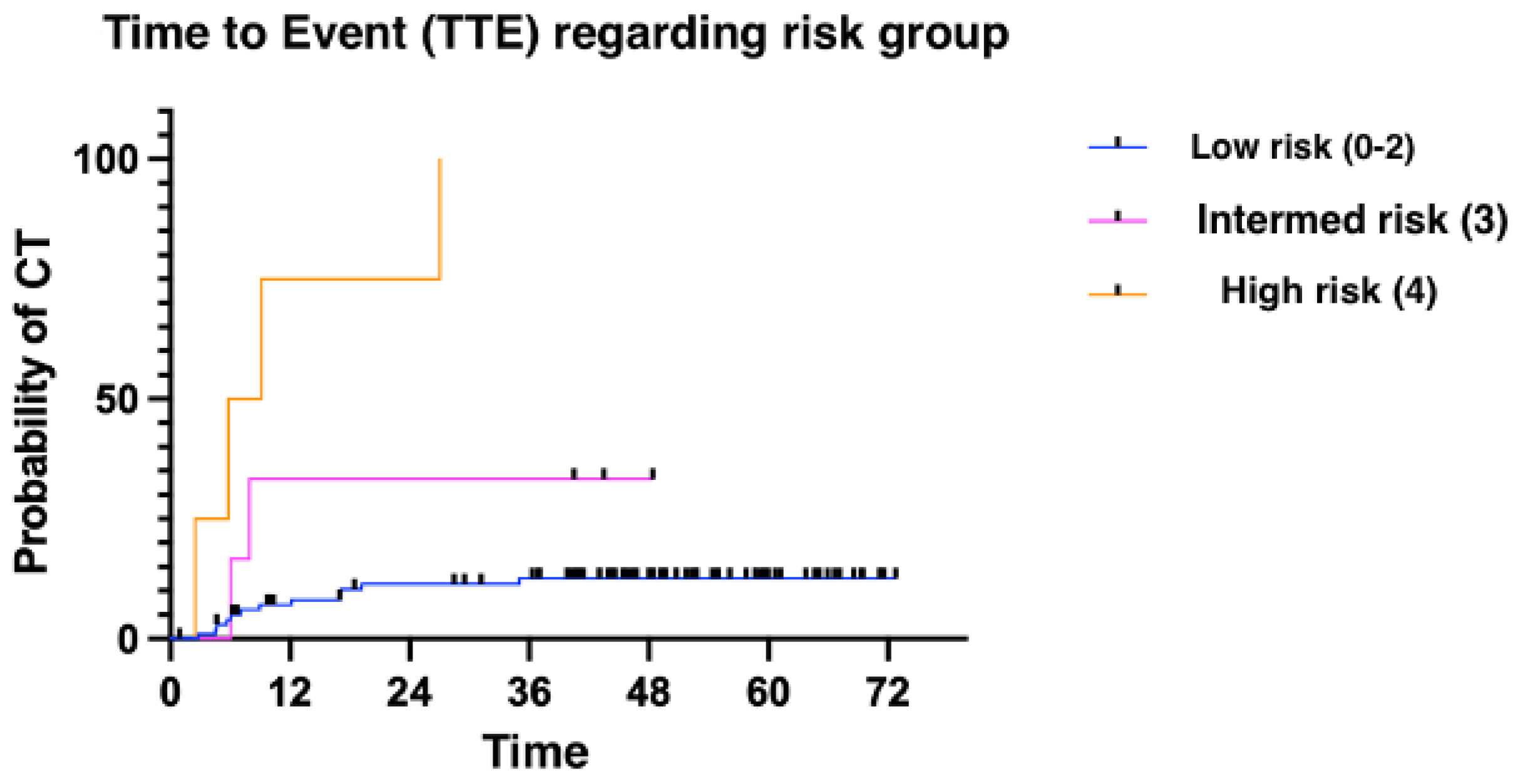
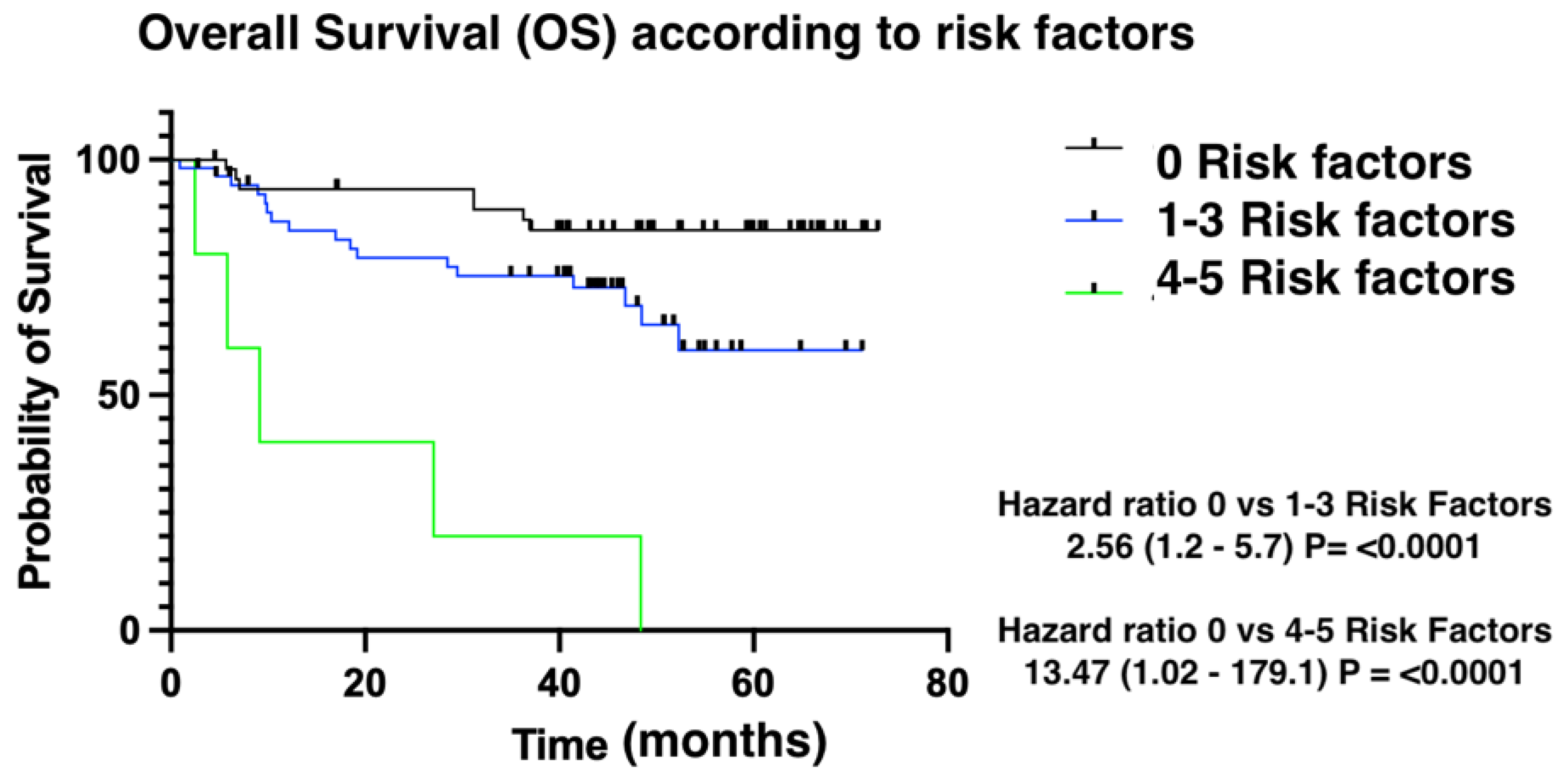
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| ABVD: doxorubicin, bleomycin, vinblastine, and dacarbazine |
| ACE: angiotensin-converting enzyme |
| ARBs: angiotensin II receptor blockers |
| ASE: American Society of Echocardiography |
| BEACOPP: bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazina, and prednisolone |
| CHOEP: cyclophosphamide, doxorubicin, vincristine, ethopoxide, and prednisone |
| CT: cardiotoxicity CTRCD: cancer-therapy-related cardiac dysfunction CI: confidence interval |
| DL: dyslipidemia |
| EACVI: European Association of Cardiovascular Imaging |
| HF: heart failure HT: hypertension |
| HL: Hodgkin lymphoma |
| LV: left ventricular |
| LVEF: left ventricular ejection fraction |
| MALT: mucosa-associated lymphoid tissue |
| NHL: non-Hodgkin lymphoma |
| NT PROBNP: N-terminal B-type natriuretic peptide OR: odds ratio OS: overall survival PCVD: previous cardiovascular disease |
| R-CHOP: rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone |
| R-DAEPOCH: etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab |
| RNS: reactive nitrogen species |
| ROS: reactive oxygen Species |
| TOP2A: topoisomerases 2A |
| TOP2B: topoisomerases 2B TTE: time to event |
| VR-CAP: bortezomib, rituximab, cyclophosphamide, doxorrubicin, and prednisone |
References
- Pulte, D.; Jansen, L.; Castro, F.A.; Brenner, H. Changes in the survival of older patients with hematologic malignancies in the early 21st century. Cancer 2016, 122, 2031–2040. [Google Scholar] [CrossRef] [PubMed]
- Totzeck, M.; Schuler, M.; Stuschke, M.; Heusch, G.; Rassaf, T. Cardio-oncology—Strategies for management of cancer-therapy related cardiovascular disease. Int. J. Cardiol. 2019, 280, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Von Hoff, D.D. Risk Factors for Doxorubicin-lnduced Congestive Heart Failure. Ann. Intern. Med. 1979, 91, 710. [Google Scholar] [CrossRef] [PubMed]
- Townsend, W.; Linch, D. Hodgkin’s lymphoma in adults. Lancet 2012, 380, 836–847. [Google Scholar] [CrossRef] [PubMed]
- Bansal, N.; Adams, M.J.; Ganatra, S.; Colan, S.D.; Aggarwal, S.; Steiner, R.; Amdani, S.; Lipshultz, E.R.; Lipshultz, S.E. Strategies to prevent anthracycline-induced cardiotoxicity in cancer survivors. Cardio-Oncol. 2019, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, D.; Hawkes, E.A.; Jack, A.; Qian, W.; Smith, P.; Mouncey, P.; Pocock, C.; Ardeshna, K.M.; Radford, J.A.; McMillan, A.; et al. Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B-cell non-Hodgkin lymphoma: A phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet 2013, 381, 1817–1826. [Google Scholar] [CrossRef] [PubMed]
- Carrasco, R.; Castillo, R.L.; Gormaz, J.G.; Carrillo, M.; Thavendiranathan, P. Role of Oxidative Stress in the Mechanisms of Anthracycline-Induced Cardiotoxicity: Effects of Preventive Strategies. Oxid. Med. Cell Longev. 2021, 2021, 8863789. [Google Scholar] [CrossRef]
- Mercurio, V.; Cuomo, A.; Della Pepa, R.; Ciervo, D.; Cella, L.; Pirozzi, F.; Parrella, P.; Campi, G.; Franco, R.; Varricchi, G.; et al. What Is the Cardiac Impact of Chemotherapy and Subsequent Radiotherapy in Lymphoma Patients? Antioxid Redox Signal. 2019, 31, 1166–1174. [Google Scholar] [CrossRef]
- Felker, G.M.; Thompson, R.E.; Hare, J.M.; Hruban, R.H.; Clemetson, D.E.; Howard, D.L.; Baughman, K.L.; Kasper, E.K. Underlying causes and long-term survival in patients with initially unexplained cardiomyopathy. N. Engl. J. Med. 2000, 342, 1077–1084. [Google Scholar] [CrossRef]
- Perez, I.E.; Taveras Alam, S.; Hernandez, G.A.; Sancassani, R. Cancer Therapy-Related Cardiac Dysfunction: An Overview for the Clinician. Clin. Med. Insights Cardiol. 2019, 13, 117954681986644. [Google Scholar] [CrossRef]
- Cardinale, D.; Iacopo, F.; Cipolla, C.M. Cardiotoxicity of Anthracyclines. Front. Cardiovasc. Med. 2020, 7, 26. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, K.; Zhang, J.; Honbo, N.; Karliner, J.S. Doxorubicin cardiomyopathy. Cardiology 2010, 115, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.C. Cellular roles of DNA topoisomerases: A molecular perspective. Nat. Rev. Mol. Cell Biol. 2002, 3, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Our World in Data. Available online: https://ourworldindata.org (accessed on 1 April 2023).
- Boddicker, N.J.; Larson, M.C.; Castellino, A.; Herrmann, J.; Inwards, D.J.; Thanarajasingam, G.; Maurer, M.J.; Allmer, C.; Witzig, T.E.; Nowakowski, G.S.; et al. Anthracycline treatment, cardiovascular risk factors and the cumulative incidence of cardiovascular disease in a cohort of newly diagnosed lymphoma patients from the modern treatment era. Am. J. Hematol. 2021, 96, 979–988. [Google Scholar] [CrossRef] [PubMed]
- Curigliano, G.; Cardinale, D.; Dent, S.; Criscitiello, C.; Aseyev, O.; Lenihan, D.; Cipolla, C.M. Cardiotoxicity of anticancer treatments: Epidemiology, detection, and management. CA Cancer J. Clin. 2016, 66, 309–325. [Google Scholar] [CrossRef] [PubMed]
- Antoniak, S.; Phungphong, S.; Cheng, Z.; Jensen, B.C. Novel Mechanisms of Anthracycline-Induced Cardiovascular Toxicity: A Focus on Thrombosis, Cardiac Atrophy, and Programmed Cell Death. Front. Cardiovasc. Med. 2021, 8, 817977. [Google Scholar] [CrossRef] [PubMed]
- Plana, J.C.; Galderisi, M.; Barac, A.; Ewer, M.S.; Ky, B.; Scherrer-Crosbie, M.; Ganame, J.; Sebag, I.A.; Agler, D.A.; Badano, L.P.; et al. Expert Consensus for Multimodality Imaging Evaluation of Adult Patients during and after Cancer Therapy: A Report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2014, 27, 911–939. [Google Scholar] [CrossRef]
- Klotzka, A.; Iwańczyk, S.; Ropacka-Lesiak, M.; Misan, N.; Lesiak, M. Anthracycline-induced microcirculation disorders: AIM PILOT Study. Kardiol. Pol. 2023, 81, 766–768. [Google Scholar] [CrossRef] [PubMed]
- Triposkiadis, F.; Xanthopoulos, A.; Butler, J. Cardiovascular Aging and Heart Failure. J. Am. Coll. Cardiol. 2019, 74, 804–813. [Google Scholar] [CrossRef]
- Cardinale, D.; Colombo, A.; Sandri, M.T.; Lamantia, G.; Colombo, N.; Civelli, M.; Martinelli, G.; Veglia, F.; Fiorentini, C.; Cipolla, C.M.; et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation 2006, 114, 2474–2481. [Google Scholar] [CrossRef]
- Henriksen, P.A. Anthracycline cardiotoxicity: An update on mechanisms, monitoring and prevention. Heart Br. Card. Soc. 2018, 104, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C.; McDonald, K.; de Boer, R.A.; Maisel, A.; Cleland, J.G.; Kozhuharov, N.; Coats, A.J.; Metra, M.; Mebazaa, A.; Ruschitzka, F.; et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur. J. Heart Fail. 2019, 21, 715–731. [Google Scholar] [CrossRef] [PubMed]
- Bracun, V.; Aboumsallem, J.P.; van der Meer, P.; de Boer, R.A. Cardiac Biomarkers in Patients with Cancer: Considerations, Clinical Implications, and Future Avenues. Curr. Oncol. Rep. 2020, 22, 67. [Google Scholar] [CrossRef] [PubMed]
- Lyon, A.R.; Lyon, A.R.; López-Fernández, T.; López-Fernández, T.; Couch, L.S.; Couch, L.S.; Asteggiano, R.; Asteggiano, R.; Aznar, M.C.; Aznar, M.C.; et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. 2022, 43, 4229–4361. [Google Scholar] [CrossRef]
- Martin-Garcia, A.; Diaz-Pelaez, E.; Lopez-Corral, L.; Sanchez-Pablo, C.; de Plasencia, G.M.; Galan-Arriola, C.; Sanchez-Gonzalez, J.; Cruz, J.J.; Ibanez, B.; Sanchez, P.L. T2 Mapping Identifies Early Anthracycline-Induced Cardiotoxicity in Elderly Patients with Cancer. JACC Cardiovasc. Imaging 2020, 13, 1630–1632. [Google Scholar] [CrossRef]
| Median Age (Range) | 59 (18–89) |
| Sex (male) | 101 (50.2%) |
| LYMPHOMA SUBTYPE | |
| Diffuse large B lymphoma | 86 (42.9%) |
| Hodgkin lymphoma | 54 (27%) |
| Follicular lymphoma | 38 (19%) |
| Primary mediastinal B cell lymphoma | 10 (5.1%) |
| Non-Hodgkin lymphoma T | 7 (3.6%) |
| Mantle cell lymphoma | 5 (2.6%) |
| REGIMEN USED | |
| R-CHOP | 103 (51.7%) |
| ABVD | 51 (25.4%) |
| RminiCHOP | 21 (10.4%) |
| R-DAEPOCH | 15 (7.5%) |
| BEACOPP | 4 (2%) |
| CHOEP | 3 (1.5%) |
| VR-CAP | 3 (1.5%) |
| CARDIOVASCULAR RISK FACTORS | |
| Hypertension (HT) | 50 (25%) |
| Diabetes (DM) | 13 (6.5%) |
| Dyslipidemia (DL) | 51 (25.5%) |
| Previous cardiovascular disease | 35 (17.5%) |
| Obesity | 65 (32.8%) |
| Alcohol intake | 24 (12%) |
| Smoker or former smoker | 60 (30.5%) |
| Heart Failure | 12 (34.4%) |
| Myocardiopathy | 9 (25.7%) |
| Thromboembolism | 7 (20%) |
| Myocardial Infarction | 3 (8.5%) |
| Conduction disorders | 3 (8.5%) |
| Valve disease | 1 (2.9%) |
| Event (CT) | No Event (NO CT) | p-Value | |
|---|---|---|---|
| Median age (CI 95%) | 70.85 y/o (65.3–76.39) | 54.62 y/o (51.23–58.01) | p < 0.0001 |
| Hypertension (HT) | 30.30% | 16.67% | p 0.09 |
| Dyslipidemia (DL) | 36.84% | 13.19% | p 0.037 |
| Diabetes | 20% | 20.17% | p 0.98 |
| Smoker or former smoker | 21.43% | 19.54% | p 0.8 |
| Alcohol intake | 13% | 18.8% | p 0.67 |
| Obesity | 21.15% | 19.84% | p 0.81 |
| Sex | 21.54% | 18.75% | p 0.83 |
| Previous cardiovascular disease | 61.05% | 14.02% | p < 0.0001 |
| Baseline LVEF | |||
|---|---|---|---|
| Event | No Event | ||
| AVERAGE | 61.15% | 60.59% | |
| CI 95% | 58.85–63.46% | 59.35–61.83% | p 0.92 |
| Troponin I (N < 0.08 µg/L) | |||
|---|---|---|---|
| Event | No Event | ||
| BASELINE TROPONIN | |||
| AVERAGE | 0.022 µg/L | 0.018 µg/L | |
| IC 95% | 0.013–0.031 µg/L | 0.014–0.022 µg/L | p 0.23 |
| INTERMEDIATE TROPONIN | |||
| AVERAGE | 0.031 µg/L | 0.025 µg/L | |
| IC 95% | 0.021–0.041 µg/L | 0.01–0.04 µg/L | p 0.0009 |
| FINAL TROPONIN | |||
| AVERAGE | 0.07 µg/L | 0.033 µg/L | |
| IC 95% | 0.024–0.1 µg/L | 0.026–0.039 µg/L | p 0.0082 |
| NT-PROBNP | |||
|---|---|---|---|
| Event | No Event | p-Value | |
| BASELINE NT-proBNP | |||
| AVERAGE | 456.1 µg/L | 120.1 µg/L | |
| CI 95% | 156.2–755.9 µg/L | 87.4–152.9 µg/L | p 0.0052 |
| INTERMEDIATE NT-proBNP | |||
| AVERAGE | 563.5 µg/L | 125.9 µg/L | |
| CI 95% | 223.9–903.1 µg/L | 94.05–157.8 µg/L | p 0.03 |
| FINAL NT-proBNP | |||
| AVERAGE | 785.7 µg/L | 165.4 µg/L | |
| CI 95% | 208.9–1363 µg/L | 124.1–206.7 µg/L | p 0.022 |
| Event | No Event | ||
|---|---|---|---|
| BASAL HEMOGLOBIN | |||
| AVERAGE | 11.8 gr/dL | 12.6 gr/dL | |
| CI 95% | 10.87–12.47 gr/dL | 11.25–16.41 gr/dL | p 0.503 |
| INTERMEDIATE HEMOGLOBIN | |||
| AVERAGE | 11.28 gr/dL | 11.96 gr/dL | |
| CI 95% | 10.81–11.75 gr/dL | 11.66–12.27 gr/dL | p 0.3 |
| FINAL HEMOGLOBIN | |||
| AVERAGE | 11.52 gr/dL | 11.94 gr/dL | |
| CI 95% | 10.74–12.3 gr/dL | 11.6–12.27 gr/dL | p 0.24 |
| p-Value | Odds Ratio (OR) CI 95% | |
|---|---|---|
| Dyslipidemia | 0.05 | 3.18 (1.45–6.71) |
| ≥72 years | 0.047 | 3.79 (1.78–8.1) |
| PCVD | 0.018 | 4.57 (2.02–10.35) |
| Basal NT-proBNP | 0.02 | 17.5 (3.1–99.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopez-Garcia, A.; Macia, E.; Gomez-Talavera, S.; Castillo, E.; Morillo, D.; Tuñon, J.; Ibañez, B.; Cordoba, R. Predictive Factors of Therapy-Related Cardiovascular Events in Patients with Lymphoma Receiving Anthracyclines. Med. Sci. 2024, 12, 23. https://doi.org/10.3390/medsci12020023
Lopez-Garcia A, Macia E, Gomez-Talavera S, Castillo E, Morillo D, Tuñon J, Ibañez B, Cordoba R. Predictive Factors of Therapy-Related Cardiovascular Events in Patients with Lymphoma Receiving Anthracyclines. Medical Sciences. 2024; 12(2):23. https://doi.org/10.3390/medsci12020023
Chicago/Turabian StyleLopez-Garcia, Alberto, Ester Macia, Sandra Gomez-Talavera, Eva Castillo, Daniel Morillo, Jose Tuñon, Borja Ibañez, and Raul Cordoba. 2024. "Predictive Factors of Therapy-Related Cardiovascular Events in Patients with Lymphoma Receiving Anthracyclines" Medical Sciences 12, no. 2: 23. https://doi.org/10.3390/medsci12020023
APA StyleLopez-Garcia, A., Macia, E., Gomez-Talavera, S., Castillo, E., Morillo, D., Tuñon, J., Ibañez, B., & Cordoba, R. (2024). Predictive Factors of Therapy-Related Cardiovascular Events in Patients with Lymphoma Receiving Anthracyclines. Medical Sciences, 12(2), 23. https://doi.org/10.3390/medsci12020023








