Analysis of Endocrine and Inflammatory Markers in Preserved Ratio Impaired Spirometry
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Clinical Parameters
2.3. Hormones and Cytokine Quantification
2.4. Statistical Analyses
3. Results
3.1. COPD Patients Exhibit More Malnourished and Less FEV1
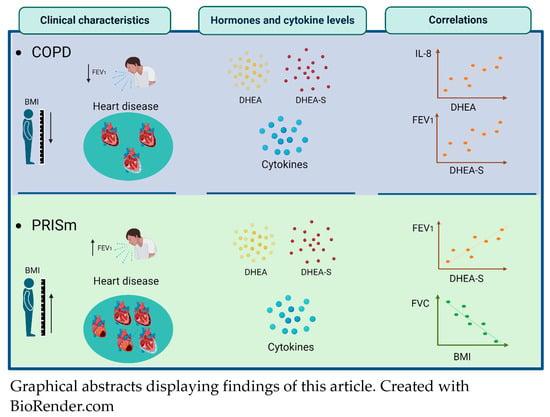
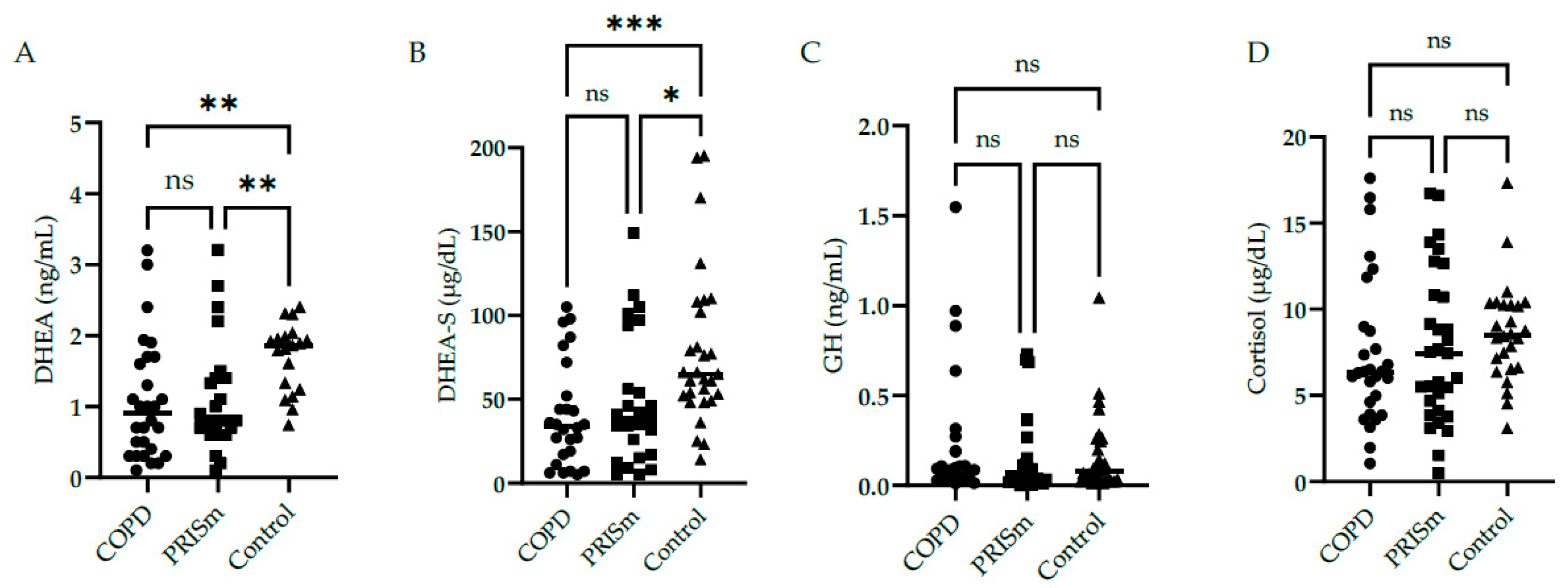
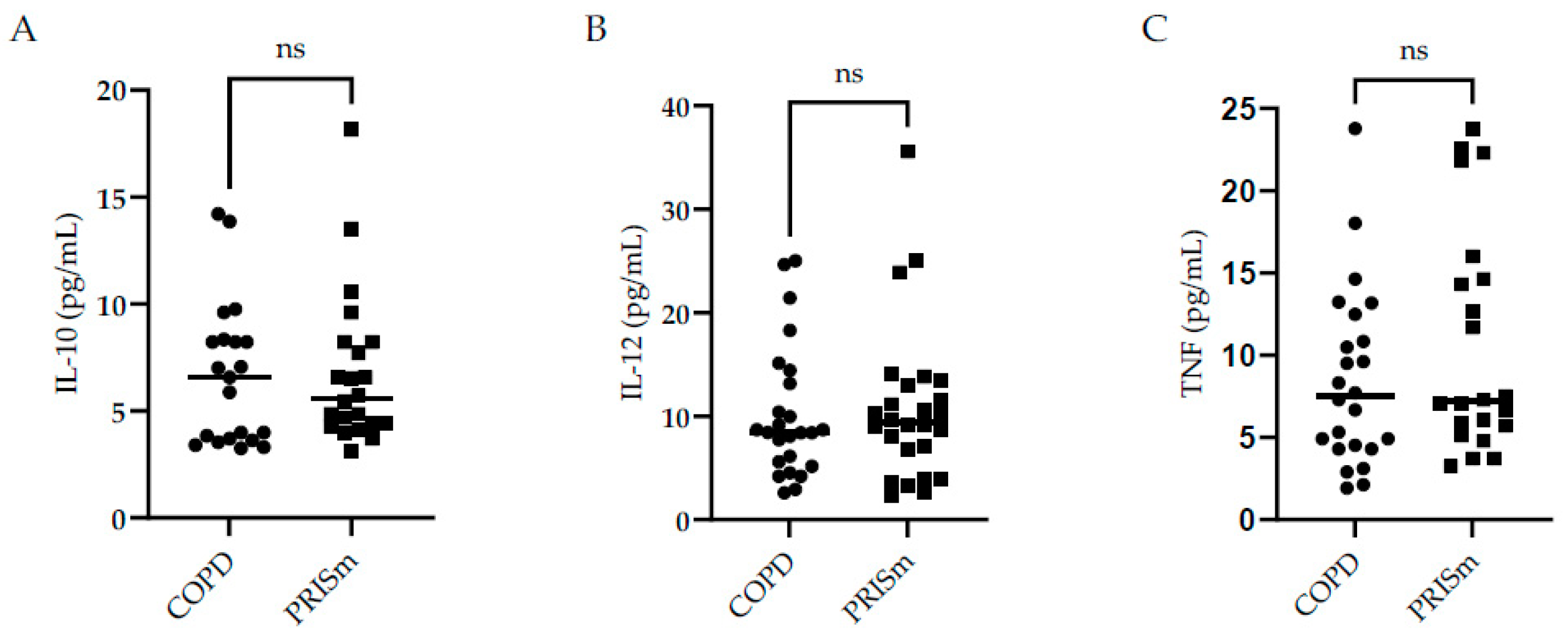
3.2. Evaluation of Hormones and Inflammatory Markers in PRISm and COPD Patients
3.3. DHEA-S and DHEA Correlates Positively with Lung Function Parameters and IL-8 Correlates Negatively with DHEA in COPD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Meek, P.M.; Petersen, H.; Washko, G.R.; Diaz, A.A.; Klm, V.; Sood, A.; Tesfaigzi, Y. Chronic Bronchitis Is Associated With Worse Symptoms and Quality of Life Than Chronic Airflow Obstruction. Chest 2015, 148, 408–416. [Google Scholar] [CrossRef]
- Salvi, S. Tobacco Smoking and Environmental Risk Factors for Chronic Obstructive Pulmonary Disease. Clin. Chest Med. 2014, 35, 17–27. [Google Scholar] [CrossRef]
- Agustí, A.; Celli, B.R.; Criner, G.J.; Halpin, D.; Anzueto, A.; Barnes, P.; Bourbeau, J.; Han, M.K.; Martinez, F.J.; Montes de Oca, M.; et al. Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD Executive Summary. Eur. Respir. J. 2023, 61, 2300239. [Google Scholar] [CrossRef]
- Larsson, K.; Janson, C.; Ställberg, B.; Lisspers, K.; Olsson, P.; Kostikas, K.; Gruenberger, J.-B.; Gutzwiller, F.S.; Uhde, M.; Jorgensen, L.; et al. Impact of COPD Diagnosis Timing on Clinical and Economic Outcomes: The ARCTIC Observational Cohort Study. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 995–1008. [Google Scholar] [CrossRef]
- Kanetake, R.; Takamatsu, K.; Park, K.; Yokoyama, A. Prevalence and Risk Factors for COPD in Subjects with Preserved Ratio Impaired Spirometry. BMJ Open Respir. Res. 2022, 9, e001298. [Google Scholar] [CrossRef]
- Lu, J.; Ge, H.; Qi, L.; Zhang, S.; Yang, Y.; Huang, X.; Li, M. Subtyping Preserved Ratio Impaired Spirometry (PRISm) by Using Quantitative HRCT Imaging Characteristics. Respir. Res. 2022, 23, 309. [Google Scholar] [CrossRef]
- Wan, E.S.; Castaldi, P.J.; Cho, M.H.; Hokanson, J.E.; Regan, E.A.; Make, B.J.; Beaty, T.H.; Han, M.K.; Curtis, J.L.; Curran-Everett, D.; et al. Epidemiology, Genetics, and Subtyping of Preserved Ratio Impaired Spirometry (PRISm) in COPDGene. Respir. Res. 2014, 15, 89. [Google Scholar] [CrossRef]
- Yoon, S.M.; Jin, K.N.; Lee, H.J.; Lee, H.W.; Park, T.Y.; Heo, E.Y.; Kim, D.K.; Lee, J.-K. Acute Exacerbation and Longitudinal Lung Function Change of Preserved Ratio Impaired Spirometry. Int. J. Chronic Obstr. Pulm. Dis. 2024, 19, 519–529. [Google Scholar] [CrossRef]
- Wei, X.; Ding, Q.; Yu, N.; Mi, J.; Ren, J.; Li, J.; Xu, S.; Gao, Y.; Guo, Y. Imaging Features of Chronic Bronchitis with Preserved Ratio and Impaired Spirometry (PRISm). Lung 2018, 196, 649–658. [Google Scholar] [CrossRef]
- Wan, E.S.; Fortis, S.; Regan, E.A.; Hokanson, J.; Han, M.K.; Casaburi, R.; Make, B.J.; Crapo, J.D.; DeMeo, D.L.; Silverman, E.K.; et al. Longitudinal Phenotypes and Mortality in Preserved Ratio Impaired Spirometry in the COPDGene Study. Am. J. Respir. Crit. Care Med. 2018, 198, 1397–1405. [Google Scholar] [CrossRef]
- Kotlyarov, S. Involvement of the Innate Immune System in the Pathogenesis of Chronic Obstructive Pulmonary Disease. Int. J. Mol. Sci. 2022, 23, 985. [Google Scholar] [CrossRef]
- Nurwidya, F.; Damayanti, T.; Yunus, F. The Role of Innate and Adaptive Immune Cells in the Immunopathogenesis of Chronic Obstructive Pulmonary Disease. Tuberc. Respir. Dis. 2016, 79, 5. [Google Scholar] [CrossRef]
- Selvarajah, S.; Todd, I.; Tighe, P.J.; John, M.; Bolton, C.E.; Harrison, T.; Fairclough, L.C. Multiple Circulating Cytokines Are Coelevated in Chronic Obstructive Pulmonary Disease. Mediators Inflamm. 2016, 2016, 1–9. [Google Scholar] [CrossRef]
- MacNee, W. Is Chronic Obstructive Pulmonary Disease an Accelerated Aging Disease? Ann. Am. Thorac. Soc. 2016, 13, S429–S437. [Google Scholar] [CrossRef]
- Maté, I.; Martínez de Toda, I.; Arranz, L.; Álvarez-Sala, J.L.; De la Fuente, M. Accelerated Immunosenescence, Oxidation and Inflammation Lead to a Higher Biological Age in COPD Patients. Exp. Gerontol. 2021, 154, 111551. [Google Scholar] [CrossRef]
- Debigaré, R.; Marquis, K.; Côté, C.H.; Tremblay, R.R.; Michaud, A.; LeBlanc, P.; Maltais, F. Catabolic/Anabolic Balance and Muscle Wasting in Patients With COPD. Chest 2003, 124, 83–89. [Google Scholar] [CrossRef]
- Karadag, F.; Ozcan, H.; Karul, A.B.; CEYLAN, E.; CILDAG, O. Correlates of Erectile Dysfunction in Moderate-to-Severe Chronic Obstructive Pulmonary Disease Patients. Respirology 2007, 12, 248–253. [Google Scholar] [CrossRef]
- Karametos, I.; Tsiboli, P.; Togousidis, I.; Hatzoglou, C.; Giamouzis, G.; Gourgoulianis, K.I. Chronic Obstructive Pulmonary Disease as a Main Factor of Premature Aging. Int. J. Environ. Res. Public Health 2019, 16, 540. [Google Scholar] [CrossRef]
- Straub, R.H.; Konecna, L.; Hrach, S.; Rothe, G.; Kreutz, M.; Schölmerich, J.; Falk, W.; Lang, B. Serum Dehydroepiandrosterone (DHEA) and DHEA Sulfate Are Negatively Correlated with Serum Interleukin-6 (IL-6), and DHEA Inhibits IL-6 Secretion from Mononuclear Cells in Man in Vitro: Possible Link between Endocrinosenescence and Immunosenescence. J. Clin. Endocrinol. Metab. 1998, 83, 2012–2017. [Google Scholar] [CrossRef]
- Pesce, G.; Triebner, K.; van der Plaat, D.A.; Courbon, D.; Hustad, S.; Sigsgaard, T.; Nowak, D.; Heinrich, J.; Anto, J.M.; Dorado-Arenas, S.; et al. Low Serum DHEA-S Is Associated with Impaired Lung Function in Women. EClinicalMedicine 2020, 23, 100389. [Google Scholar] [CrossRef]
- Guler, S.A.; Machahua, C.; Geiser, T.K.; Kocher, G.; Marti, T.M.; Tan, B.; Trappetti, V.; Ryerson, C.J.; Funke-Chambour, M. Dehydroepiandrosterone in Fibrotic Interstitial Lung Disease: A Translational Study. Respir. Res. 2022, 23, 149. [Google Scholar] [CrossRef]
- Culver, B.H.; Graham, B.L.; Coates, A.L.; Wanger, J.; Berry, C.E.; Clarke, P.K.; Hallstrand, T.S.; Hankinson, J.L.; Kaminsky, D.A.; MacIntyre, N.R.; et al. Recommendations for a Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement. Am. J. Respir. Crit. Care Med. 2017, 196, 1463–1472. [Google Scholar] [CrossRef]
- Pereira, C.A.d.C.; Sato, T.; Rodrigues, S.C. Novos Valores de Referência Para Espirometria Forçada Em Brasileiros Adultos de Raça Branca. J. Bras. Pneumol. 2007, 33, 397–406. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Iwama, A.M.; Andrade, G.N.; Shima, P.; Tanni, S.E.; Godoy, I.; Dourado, V.Z. The Six-Minute Walk Test and Body Weight-Walk Distance Product in Healthy Brazilian Subjects. Braz. J. Med. Biol. Res. 2009, 42, 1080–1085. [Google Scholar] [CrossRef]
- Surveillance for Respiratory Hazards in the Occupational Setting [American Thoracic Society]. Am. Rev. Respir. Dis. 1982, 126, 952–956.
- Organización Panamericana de la Salud Encuesta Multicéntrica Salud Bienestar y Envejecimiento (SABE) En América Latina: Informe Preliminar. 2001. Available online: http://envejecimiento.csic.es/documentos/documentos/paho-salud-01.pdf (accessed on 21 March 2021).
- Frisancho, A. Anthropometric Standards for the Assessment of Growth and Nutritional Status; University of Michigan Press: Ann Arbor, MI, USA, 1990; ISBN 9780472101467. [Google Scholar]
- Mete, B.; Pehlivan, E.; Gülbaş, G.; Günen, H. Prevalence of Malnutrition in COPD and Its Relationship with the Parameters Related to Disease Severity. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 3307–3312. [Google Scholar] [CrossRef]
- Miura, S.; Iwamoto, H.; Omori, K.; Yamaguchi, K.; Sakamoto, S.; Horimasu, Y.; Masuda, T.; Miyamoto, S.; Nakashima, T.; Fujitaka, K.; et al. Preserved Ratio Impaired Spirometry with or without Restrictive Spirometric Abnormality. Sci. Rep. 2023, 13, 2988. [Google Scholar] [CrossRef]
- Melo, L.C.; Silva, M.A.M.d.; Calles, A.C. do N. Obesity and Lung Function: A Systematic Review. Einstein 2014, 12, 120–125. [Google Scholar] [CrossRef]
- Schachter, L.M.; Salome, C.M.; Peat, J.K.; Woolcock, A.J. Obesity Is a Risk for Asthma and Wheeze but Not Airway Hyperresponsiveness. Thorax 2001, 56, 4–8. [Google Scholar] [CrossRef]
- Park, J.-H.; Lee, J.-K.; Heo, E.Y.; Kim, D.K.; Chung, H.S. The Effect of Obesity on Patients with Mild Chronic Obstructive Pulmonary Disease: Results from KNHANES 2010 to 2012. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 757–763. [Google Scholar] [CrossRef][Green Version]
- Sun, Y.; Milne, S.; Jaw, J.E.; Yang, C.X.; Xu, F.; Li, X.; Obeidat, M.; Sin, D.D. BMI Is Associated with FEV1 Decline in Chronic Obstructive Pulmonary Disease: A Meta-Analysis of Clinical Trials. Respir. Res. 2019, 20, 236. [Google Scholar] [CrossRef]
- Tang, X.; Lei, J.; Li, W.; Peng, Y.; Wang, C.; Huang, K.; Yang, T. The Relationship Between BMI and Lung Function in Populations with Different Characteristics: A Cross-Sectional Study Based on the Enjoying Breathing Program in China. Int. J. Chronic Obstr. Pulm. Dis. 2022, 17, 2677–2692. [Google Scholar] [CrossRef]
- Wan, E.S.; Balte, P.; Schwartz, J.E.; Bhatt, S.P.; Cassano, P.A.; Couper, D.; Daviglus, M.L.; Dransfield, M.T.; Gharib, S.A.; Jacobs, D.R.; et al. Association Between Preserved Ratio Impaired Spirometry and Clinical Outcomes in US Adults. JAMA 2021, 326, 2287. [Google Scholar] [CrossRef]
- Sharma, G.; Hanania, N.A.; Shim, Y.M. The Aging Immune System and Its Relationship to the Development of Chronic Obstructive Pulmonary Disease. Proc. Am. Thorac. Soc. 2009, 6, 573–580. [Google Scholar] [CrossRef]
- Silva, B.S.A.; Lira, F.S.; Ramos, D.; Uzeloto, J.S.; Rossi, F.E.; Freire, A.P.C.F.; Silva, R.N.; Trevisan, I.B.; Gobbo, L.A.; Ramos, E.M.C. Severity of COPD and Its Relationship with IL-10. Cytokine 2018, 106, 95–100. [Google Scholar] [CrossRef]
- Baidya, A.; Sangle, S.; Marbaniang, I.; Kulkarni, V.; Deshpande, P.; Nimkar, S.; Chavan, A.; Salvi, S.; Lokhande, R.; Kadam, D.; et al. Clinical and Immunological Markers of Pulmonary Impairment Among People With HIV in India. Open Forum Infect. Dis. 2022, 9, ofac233. [Google Scholar] [CrossRef]
- Karadag, F.; Ozcan, H.; Karul, A.B.; Yilmaz, M.; Cildag, O. Sex Hormone Alterations and Systemic Inflammation in Chronic Obstructive Pulmonary Disease. Int. J. Clin. Pract. 2009, 63, 275–281. [Google Scholar] [CrossRef]
- Espinoza, J.; Montaño, L.M.; Perusquía, M. Nongenomic Bronchodilating Action Elicited by Dehydroepiandrosterone (DHEA) in a Guinea Pig Asthma Model. J. Steroid Biochem. Mol. Biol. 2013, 138, 174–182. [Google Scholar] [CrossRef]
- Mkacher, W.; Tabka, Z.; Chaieb, F.; Gueddes, M.; Zaouali, M.; Aouichaoui, C.; Zbidi, A.; Trabelsi, Y. Effect of Rehabilitation Program on Endocrinological Parameters in Patients with COPD and in Healthy Subjects. COPD J. Chronic Obstr. Pulm. Dis. 2014, 11, 681–688. [Google Scholar] [CrossRef]
- Roelfsema, F.; Veldhuis, J.D. Growth Hormone Dynamics in Healthy Adults Are Related to Age and Sex and Strongly Dependent on Body Mass Index. Neuroendocrinology 2016, 103, 335–344. [Google Scholar] [CrossRef]
- Yang, I.A.; Clarke, M.S.; Sim, E.H.; Fong, K.M. Inhaled Corticosteroids for Stable Chronic Obstructive Pulmonary Disease. Cochrane Database Syst. Rev. 2012, 2016, CD002991. [Google Scholar] [CrossRef]
- Moffat, S.D.; An, Y.; Resnick, S.M.; Diamond, M.P.; Ferrucci, L. Longitudinal Change in Cortisol Levels Across the Adult Life Span. J.Gerontol. Ser. A 2020, 75, 394–400. [Google Scholar] [CrossRef]
- Brauer, V.S.; Zambuzi, F.A.; Espíndola, M.S.; Cavalcanti Neto, M.P.; Prado, M.K.B.; Cardoso, P.M.; Soares, L.S.; Galvao-Lima, L.J.; Leopoldino, A.M.; Cardoso, C.R.d.B.; et al. The Influence of Dehydroepiandrosterone on Effector Functions of Neutrophils. Braz. J. Pharm. Sci. 2021, 57, e19139. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Shaper, A.G.; Lennon, L.; Whincup, P.H. Decreased Muscle Mass and Increased Central Adiposity Are Independently Related to Mortality in Older Men. Am. J. Clin. Nutr. 2007, 86, 1339–1346. [Google Scholar] [CrossRef]
- Voláková, E.; Zatloukal, J.; Plutinsky, M.; Popelkova, P.; Dvorak, T.; Safranek, P.; Sobotik, O.; Vlachova, A.; Vanik, P.; Liptakova, Z. Assessment of Nutrition and Muscle Mass Loss in Patients with Severe COPD. In Proceedings of the Monitoring Airway Disease, Milan, Italy, 6 September 2017; European Respiratory Society: Lausanne, Brussels, 2017; p. PA1087. [Google Scholar]
- Poulain, M.; Doucet, M.; Drapeau, V.; Fournier, G.; Tremblay, A.; Poirier, P.; Maltais, F. Metabolic and Inflammatory Profile in Obese Patients with Chronic Obstructive Pulmonary Disease. Chron. Respir. Dis. 2008, 5, 35–41. [Google Scholar] [CrossRef]
- Tkacova, R. Systemic Inflammation in Chronic Obstructive Pulmonary Disease: May Adipose Tissue Play a Role? Review of the Literature and Future Perspectives. Mediat. Inflamm. 2010, 2010, 585989. [Google Scholar] [CrossRef]
- Ling, P.-R.; Smith, R.J.; Kie, S.; Boyce, P.; Bistrian, B.R. Effects of Protein Malnutrition on IL-6-Mediated Signaling in the Liver and the Systemic Acute-Phase Response in Rats. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2004, 287, R801–R808. [Google Scholar] [CrossRef]
- de Oliveira, D.C.; Hastreiter, A.A.; Mello, A.S.; de Oliveira Beltran, J.S.; Oliveira Santos, E.W.C.; Borelli, P.; Fock, R.A. The Effects of Protein Malnutrition on the TNF-RI and NF-ΚB Expression via the TNF-α Signaling Pathway. Cytokine 2014, 69, 218–225. [Google Scholar] [CrossRef]
- Eagan, T.M.L.; Aukrust, P.; Ueland, T.; Hardie, J.A.; Johannessen, A.; Mollnes, T.E.; Damas, J.K.; Bakke, P.S.; Wagner, P.D. Body Composition and Plasma Levels of Inflammatory Biomarkers in COPD. Eur. Respir. J. 2010, 36, 1027–1033. [Google Scholar] [CrossRef]
- Eid, A.A.; Ionescu, A.A.; Nixon, L.S.; Lewis-Jenkins, V.; Matthews, S.B.; Griffiths, T.L.; Shale, D.J. Inflammatory Response and Body Composition in Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2001, 164, 1414–1418. [Google Scholar] [CrossRef]

| COPD | PRISm | Control | |
|---|---|---|---|
| Male/Female | 15/17 | 15/17 | 15/17 |
| Age, years; median (IQR) | 64 (60–70) | 64 (60–72) | 63 (59–68) |
| BMI kg/m2; median (IQR) | 23 (19–29) # | 27 (23–33) * | 27 (24–31) |
| <23 kg/m2, n (%) | 17 (53) ## | 6 (19) ** | 4 (13) |
| 23–28 kg/m2, n (%) | 7 (22) # | 12 (37) | 15 (47) |
| >28 kg/m2, n (%) | 8 (25) | 14 (44) | 13 (40) |
| FVC, L; median (IQR) | 1.96 (1.5–2.9) # | 1.96 (1.5–3.0) # | 2.64 (2.0–3.3) |
| FEV1, L; median (IQR) | 0.95 (0.82–1.36) ### | 1.44 (1.14–2.26) **# | 2.19 (1.86–3.1) |
| FEV1% pred, (%); median (IQR) | 62 (51–76) ### | 65 (54–72) ### | 94 (81–100) |
| FEV1/FVC, (%); median (IQR) | 50 (40–65) ### | 73 (71–77) ***## | 83 (83–94) |
| Current smoker | |||
| Yes, n (%) | 12 (38) # | 8 (25) | 5 (14) |
| No, n (%) | 18 (67) # | 24 (75) | 9 (33) |
| MAMC, cm; median (IQR) | 21 (19–26) | 26 (22–27) ** | ----- |
| mMRC scale; median (IQR) | 2 (1–3) | 2 (1–3) | ----- |
| Exacerbations in last year | 12 (37.5) | 7 (21.8) | ----- |
| 6MWTD, % predicted | 66 (54–76) | 73 (60–80) | ----- |
| Emphysema, n (%) | 23 (72) | 20 (62) | ----- |
| Airway wall thickening, n (%) | 13 (41) | 9 (31) | ---- |
| Chronic disease | ---- | ||
| Heart disease, n (%) | 6 (19) | 14 (44) * | ---- |
| Diabetes mellitus, n (%) | 9 (28) | 10 (31) | ---- |
| Osteoporosis, n (%) | 2 (6) | 5 (16) | ---- |
| SAH, n (%) | 16 (50) | 21 (65) | ---- |
| FEV1, L | FVC, L | FEV1 pred, (%) | FEV1/FVC, (%) | IL-6 | IL-8 | IL-10 | IL-12 | TNF | ||
|---|---|---|---|---|---|---|---|---|---|---|
| r | r | r | r | r | r | r | r | r | ||
| COPD | BMI | 0.20 | −0.01 | 0.06 | 0.31 | 0.32 | 0.21 | 0.05 | 0.30 | 0.11 |
| MAMC | 0.31 | 0.22 | −0.01 | 0.14 | 0.00 | -0.17 | 0.05 | 0.18 | 0.06 | |
| DHEA | 0.47 * | 0.37 * | 0.05 | −0.18 | −0.07 | −0.62 ** | 0.34 | 0.00 | 0.26 | |
| DHEA-S | 0.49 * | 0.38 | 0.05 | −0.12 | −0.14 | −0.52 ** | −0.00 | 0.11 | 0.01 | |
| PRISm | BMI | −0.33 | −0.35 * | 0.33 | −0.12 | 0.17 | 0.01 | 0.20 | 0.13 | 0.20 |
| MAMC | 0.37 * | 0.32 | 0.35 * | 0.01 | 0.04 | 0.07 | 0.26 | 0.25 | 0.02 | |
| DHEA | 0.24 | 0.23 | 0.05 | 0.13 | 0.03 | −0.13 | 0.08 | 0.04 | 0.05 | |
| DHEA-S | 0.53 ** | 0.52 ** | 0.29 | 0.09 | 0.13 | −0.01 | 0.16 | 0.14 | −0.11 | |
| COPD+ PRISm | BMI | 0.10 | −0.14 | 0.13 | 0.37 ** | 0.22 | 0.12 | 0.21 | 0.28 * | 0.12 |
| MAMC | 0.40 *** | 0.26 * | 0.23 | 0.35 ** | 0.09 | −0.00 | 0.16 | 0.32 * | 0.08 | |
| DHEA | 0.29 * | 0.36 ** | 0.06 | 0.04 | −0.01 | −0.39 ** | 0.24 | −0.03 | 0.22 | |
| DHEA-S | 0.42 ** | 0.52 **** | 0.28 * | 0.08 | 0.02 | −0.24 | −0.05 | 0.13 | −0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jesus, F.R.; Moraes, A.C.S.; da Silva, I.L.N.; Passos, F.C.; Salles, C.; Neves, M.C.L.C.; Baccan, G.C. Analysis of Endocrine and Inflammatory Markers in Preserved Ratio Impaired Spirometry. Med. Sci. 2024, 12, 18. https://doi.org/10.3390/medsci12020018
Jesus FR, Moraes ACS, da Silva ILN, Passos FC, Salles C, Neves MCLC, Baccan GC. Analysis of Endocrine and Inflammatory Markers in Preserved Ratio Impaired Spirometry. Medical Sciences. 2024; 12(2):18. https://doi.org/10.3390/medsci12020018
Chicago/Turabian StyleJesus, Fabíola Ramos, Anna Clara Santiago Moraes, Ingrid Lorena Neves da Silva, Fabine Correia Passos, Cristina Salles, Margarida Célia Lima Costa Neves, and Gyselle Chrystina Baccan. 2024. "Analysis of Endocrine and Inflammatory Markers in Preserved Ratio Impaired Spirometry" Medical Sciences 12, no. 2: 18. https://doi.org/10.3390/medsci12020018
APA StyleJesus, F. R., Moraes, A. C. S., da Silva, I. L. N., Passos, F. C., Salles, C., Neves, M. C. L. C., & Baccan, G. C. (2024). Analysis of Endocrine and Inflammatory Markers in Preserved Ratio Impaired Spirometry. Medical Sciences, 12(2), 18. https://doi.org/10.3390/medsci12020018