A Prospective, Blinded, Open-Label Clinical Trial to Assess the Ability of Fluorescent Light Energy to Enhance Wound Healing after Mastectomy in Female Dogs
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Study Animals
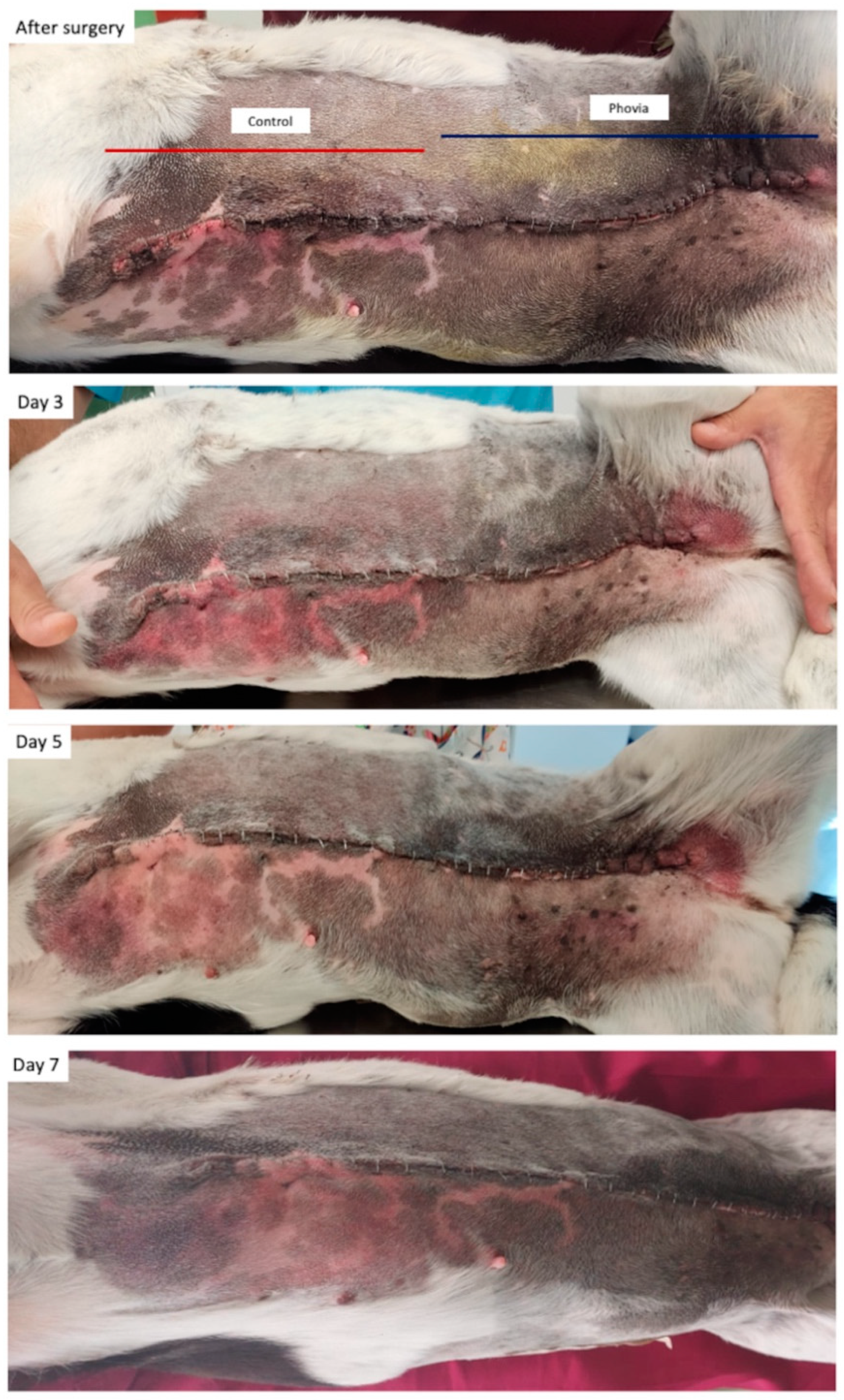
2.3. Study Protocol and Parameters Assessed
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Salas, Y.; Márquez, A.; Diaz, D.; Romero, L. Epidemiological Study of Mammary Tumors in Female Dogs Diagnosed during the Period 2002–2012: A Growing Animal Health Problem. PLoS ONE 2015, 10, 127381. [Google Scholar] [CrossRef] [PubMed]
- Papazoglou, L. Current Surgical Options for Mammary Tumor Removal in Dogs. J. Vet. Sci. Med. 2012, 1, 2–7. [Google Scholar] [CrossRef]
- Stratmann, N.; Failing, K.; Richter, A.; Wehrend, A. Mammary Tumor Recurrence in Bitches after Regional Mastectomy. Vet. Surg. 2008, 37, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Stetter, J.; Boge, G.S.; Grönlund, U.; Bergström, A. Risk Factors for Surgical Site Infection Associated with Clean Surgical Procedures in Dogs. Res. Vet. Sci. 2021, 136, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Spåre, P.; Ljungvall, I.; Ljungvall, K.; Bergström, A. Evaluation of Post-Operative Complications after Mastectomy Performed without Perioperative Antimicrobial Prophylaxis in Dogs. Acta Vet. Scand. 2021, 63, 35. [Google Scholar] [CrossRef] [PubMed]
- Field, E.J.; Kelly, G.; Pleuvry, D.; Demetriou, J.; Baines, S.J. Indications, Outcome and Complications with Axial Pattern Skin Flaps in Dogs and Cats: 73 Cases. J. Small Anim. Pract. 2015, 56, 698–706. [Google Scholar] [CrossRef]
- Montinaro, V.; Massari, F.; Vezzoni, L.; Liptak, J.M.; Straw, R.C.; Allen, L.; Cavanaugh, R.P.; Berg, J.; Doyle, R.S.; Buracco, P.; et al. Lateral Caudal Axial Pattern Flap in 13 Dogs. Vet. Surg. 2015, 44, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Burgess, B.A. Prevention and Surveillance of Surgical Infections: A Review. Vet. Surg. 2019, 48, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Eliashar, E. Monitoring Surgical Incisions. Vet. Nurs. J. 2008, 23, 30–31. [Google Scholar] [CrossRef]
- Garcia Stickney, D.N.; Thieman Mankin, K.M. The Impact of Postdischarge Surveillance on Surgical Site Infection Diagnosis. Vet. Surg. 2018, 47, 66–73. [Google Scholar] [CrossRef]
- Devriendt, N.; de Rooster, H. Initial Management of Traumatic Wounds. Vet. Clin. N. Am. Small Anim. Pract. 2017, 47, 1123–1134. [Google Scholar] [CrossRef] [PubMed]
- Amalsadvala, T.; Swaim, S.F. Management of Hard-to-Heal Wounds. Vet. Clin. N. Am. Small Anim. Pract. 2006, 36, 693–711. [Google Scholar] [CrossRef] [PubMed]
- Fahie, M.A.; Shettko, D. Evidence-Based Wound Management: A Systematic Review of Therapeutic Agents to Enhance Granulation and Epithelialization. Vet. Clin. N. Am. Small Anim. Pract. 2007, 37, 559–577. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.G. Dressings, Bandages, and Splints for Wound Management in Dogs and Cats. Vet. Clin. N. Am. Small Anim. Pract. 2006, 36, 759–791. [Google Scholar] [CrossRef] [PubMed]
- Gouveia, D.; Bimbarra, S.; Carvalho, C.; Cardoso, A.; Gamboa, Ó.; Teixeira, R.; Ferreira, A.; Martins, Â. Effects of Hyperbaric Oxygen Therapy on Wound Healing in Veterinary Medicine: A Pilot Study. Open Vet. J. 2021, 11, 544. [Google Scholar] [CrossRef] [PubMed]
- Thom, S.R. Hyperbaric Oxygen: Its Mechanisms and Efficacy. Plast. Reconstr. Surg. 2011, 127 (Suppl. S1), 131S–141S. [Google Scholar] [CrossRef] [PubMed]
- Langella, L.G.; Casalechi, H.L.; Tomazoni, S.S.; Johnson, D.S.; Albertini, R.; Pallotta, R.C.; Marcos, R.L.; de Carvalho, P.d.T.C.; Leal-Junior, E.C.P. Photobiomodulation Therapy (PBMT) on Acute Pain and Inflammation in Patients Who Underwent Total Hip Arthroplasty—A Randomized, Triple-Blind, Placebo-Controlled Clinical Trial. Lasers Med. Sci. 2018, 33, 1933–1940. [Google Scholar] [CrossRef]
- Ramos, R.M.; Burland, M.; Silva, J.B.; Burman, L.M.; Gelain, M.S.; Debom, L.M.; Bec, J.M.; Alirezai, M.; Uebel, C.O.; Valmier, J. Photobiomodulation Improved the First Stages of Wound Healing Process After Abdominoplasty: An Experimental, Double-Blinded, Non-Randomized Clinical Trial. Aesthetic Plast. Surg. 2019, 43, 147–154. [Google Scholar] [CrossRef]
- de Freitas, L.F.; Hamblin, M.R. Proposed Mechanisms of Photobiomodulation or Low-Level Light Therapy. IEEE J. Sel. Top. Quantum Electron. 2016, 22, 348–364. [Google Scholar] [CrossRef]
- Godine, R.L. Low Level Laser Therapy (LLLT) in Veterinary Medicine. Photomed. Laser Surg. 2014, 32, 1–2. [Google Scholar] [CrossRef]
- Avci, P.; Gupta, A.; Sadasivam, M.; Vecchio, D.; Pam, Z.; Pam, N.; Hamblin, M.R. Low-Level Laser (Light) Therapy (LLLT) in Skin: Stimulating, Healing, Restoring. Semin. Cutan. Med. Surg. 2013, 32, 41–52. [Google Scholar] [PubMed]
- Chung, H.; Dai, T.; Sharma, S.K.; Huang, Y.Y.; Carroll, J.D.; Hamblin, M.R. The Nuts and Bolts of Low-Level Laser (Light) Therapy. Ann. Biomed. Eng. 2012, 40, 516–533. [Google Scholar] [CrossRef] [PubMed]
- Farivar, S.; Malekshahabi, T.; Shiari, R. Biological Effects of Low Level Laser Therapy. J. Lasers Med. Sci. 2014, 5, 58–62. [Google Scholar] [PubMed]
- Dompe, C.; Moncrieff, L.; Matys, J.; Grzech-Leśniak, K.; Kocherova, I.; Bryja, A.; Bruska, M.; Dominiak, M.; Mozdziak, P.; Skiba, T.H.I.; et al. Photobiomodulation—Underlying Mechanism and Clinical Applications. J. Clin. Med. 2020, 9, 1724. [Google Scholar] [CrossRef] [PubMed]
- Prada, J.; Perego, R.; Mazzeo, M.; Spada, E.; Proverbio, D. Critically Appraised Topic on Low-Level Laser Therapy (LLLT) in Dogs: An Advisable Treatment for Skin Diseases? Vet. Sci. 2022, 9, 505. [Google Scholar] [CrossRef] [PubMed]
- Marchegiani, A.; Spaterna, A.; Cerquetella, M. Current Applications and Future Perspectives of Fluorescence Light Energy Biomodulation in Veterinary Medicine. Vet. Sci. 2021, 8, 20. [Google Scholar] [CrossRef] [PubMed]
- Salvaggio, A.; Magi, G.E.; Rossi, G.; Tambella, A.M.; Vullo, C.; Marchegiani, A.; Botto, R.; Palumbo Piccionello, A. Effect of the Topical Klox Fluorescence Biomodulation System on the Healing of Canine Surgical Wounds. Vet. Surg. 2020, 49, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Fogacci, T.; Cattin, F.; Semprini, G.; Frisoni, G.; Fabiocchi, L.; Samorani, D. The Use of Chromophore Gel-Assisted Blue Light Phototherapy (Lumiheal) for the Treatment of Surgical Site Infections in Breast Surgery. Breast J. 2018, 24, 1135. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Singer, A.J.; Valentine, S.; Henry, M.C. Wound Registry: Development and Validation. Ann. Emerg. Med. 1995, 25, 675–684. [Google Scholar] [CrossRef]
- Draize, J.H.; Woodard, G.; Calvery, H.O. Methods for the study of irritation and toxicity of substances applied topically to the skin and mucous membranes. J. Pharmacol. Exp. Ther. 1944, 82, 377–390. [Google Scholar]
- Feßler, A.T.; Wang, Y.; Burbick, C.R.; Diaz-Campos, D.; Fajt, V.R.; Lawhon, S.D.; Li, X.-Z.; Lubbers, B.V.; Maddock, K.; Miller, R.A.; et al. Antimicrobial Susceptibility Testing in Veterinary Medicine: Performance, Interpretation of Results, Best Practices and Pitfalls. One Health Adv. 2023, 1, 26. [Google Scholar] [CrossRef]
- Marchegiani, A.; Fruganti, A.; Spaterna, A.; Cerquetella, M.; Tambella, A.M.; Paterson, S. The Effectiveness of Fluorescent Light Energy as Adjunct Therapy in Canine Deep Pyoderma: A Randomized Clinical Trial. Vet. Med. Int. 2021, 2021, 6643416. [Google Scholar] [CrossRef] [PubMed]
- Marchegiani, A.; Spaterna, A.; Cerquetella, M.; Tambella, A.M.; Fruganti, A.; Paterson, S. Fluorescence Biomodulation in the Management of Canine Interdigital Pyoderma Cases: A Prospective, Single-blinded, Randomized and Controlled Clinical Study. Vet. Dermatol. 2019, 30, 371. [Google Scholar] [CrossRef] [PubMed]
- Gammel, J.E.; Biskup, J.J.; Drum, M.G.; Newkirk, K.; Lux, C.N. Effects of Low-Level Laser Therapy on the Healing of Surgically Closed Incisions and Surgically Created Open Wounds in Dogs. Vet. Surg. 2018, 47, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Hörnfeldt, M.B.; Mortensen, J.K. Surgical Dose and the Clinical Outcome in the Treatment of Mammary Gland Tumours in Female Dogs: A Literature Review. Acta Vet. Scand. 2023, 65, 12. [Google Scholar] [CrossRef]
- Turk, R.; Singh, A.; Weese, J.S. Prospective Surgical Site Infection Surveillance in Dogs. Vet. Surg. 2015, 44, 2–8. [Google Scholar] [CrossRef]

| Score | Step-Off Borders | Contour Irregularity | Margin Separation | Excessive Distortion |
|---|---|---|---|---|
| 0 | No step-off borders | No contour irregularities | No edges of wound are apparent, looks like normal skin | No edema or appearance of infection |
| 1 | Very slight borders (barely perceptible) | Very slight wrinkling (barely perceptible) | Very slight distance between wound edges (barely perceptible) | Very slight amount of edema and indication of infection |
| 2 | Well-defined step-off borders | Slight wrinkling around wound | Slight but apparent distance between wound edges | Slight but apparent amount of edema and indication of infection |
| 3 | Moderate-to-severe step-off borders | Moderate wrinkling around wound | Moderate distance between wound edges, but less than original wound size | Moderate amount of edema and indication of infection |
| 4 | Severe step-off borders (wound edges are on very different planes from one another) | Severe wrinkling around wound | Maximum observable distance between wound edges as upon creation of wound | Severe amount of edema and indication of infection |
| Score | Erythema | Edema | Serous Discharge | Purulent Exudate |
|---|---|---|---|---|
| 0 | No erythema | No edema | Wound is dry | No purulent exudate |
| 1 | Very slight (barely perceptible) | Very slight (barely perceptible) | Very slight (barely perceptible) | Small amount of purulent exudate—no color |
| 2 | Well-defined erythema | Slight edema (edges of area well defined by definite raising) | Slight serous discharge | Moderate amount of purulent exudate—no color |
| 3 | Moderate-to-severe erythema | Moderate edema (raised approximately 1 mm) | Moderate serous discharge with blood-tinged fluid | Moderate amount of purulent exudate—red- or green-tinged color |
| 4 | Severe (beet redness)-to-slight eschar formation | Severe edema (raised more than 1 mm and extending beyond area of exposure) | Large volume of serous discharge with marked blood-tinged fluid | Purulent exudate including accumulation in subcutaneous tissues at wound margin—abscess formation |
| NES Score | Numbers of Neutrophils Engulfing Bacteria * |
|---|---|
| 0 | None seen |
| 1 | <1 |
| 2 | 1–4 |
| 3 | 5–10 |
| 4 | >10 |
| # | Breed | Age (Years) | Sexual Status at VTH Presentation | Neoplasia | Type of Mastectomy | Location of FLE Treatment * |
|---|---|---|---|---|---|---|
| 1 | Mixed breed | 12 | neutered | solid carcinoma | unilateral | cranial |
| 2 | White Swiss shepherd dog | 7 | intact | tubular adenocarcinoma | bilateral | caudal |
| 3 | Lagotto Romagnolo | 6 | intact | solid carcinoma | unilateral | cranial |
| 4 | Italian bloodhound | 9 | intact | tubular adenocarcinoma | unilateral | cranial |
| 5 | Springer spaniel | 6 | intact | tubular adenocarcinoma | bilateral | caudal |
| 6 | White Swiss shepherd dog | 8 | intact | tubular adenocarcinoma | bilateral | caudal |
| 7 | Mixed breed | 13 | intact | tubular adenocarcinoma | bilateral | caudal |
| 8 | English setter | 10 | intact | solid carcinoma | bilateral | caudal |
| 9 | German shepherd | 8 | intact | solid carcinoma | bilateral | cranial |
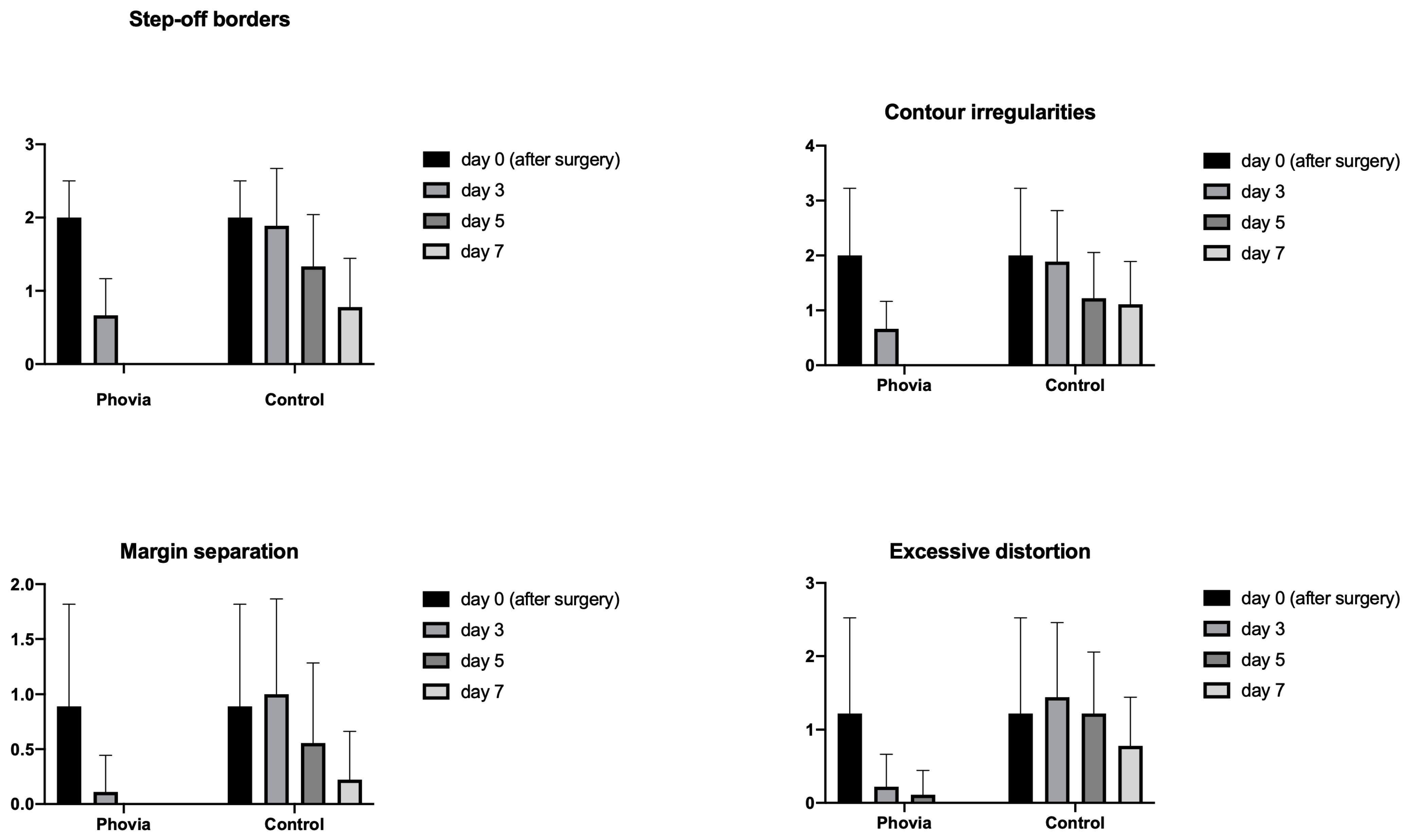
| Step-Off Borders | Contour Irregularities | Margin Separation | Excessive Distortion | |||||
|---|---|---|---|---|---|---|---|---|
| p Values | Summary | p Values | Summary | p Values | Summary | p Values | Summary | |
| FLE | ||||||||
| day 0 (after surgery) vs. day 3 | 0.0001 | *** | 0.0044 | ** | 0.0202 | * | 0.0419 | * |
| day 0 (after surgery) vs. day 5 | <0.0001 | **** | 0.0031 | ** | 0.0504 | ns | 0.0517 | ns |
| day 0 (after surgery) vs. day 7 | <0.0001 | **** | 0.0031 | ** | 0.0504 | ns | 0.0549 | ns |
| Control | ||||||||
| day 0 (after surgery) vs. day 3 | 0.9491 | ns | 0.9491 | ns | 0.9681 | ns | 0.7681 | ns |
| day 0 (after surgery) vs. day 5 | 0.1165 | ns | 0.0563 | ns | 0.6438 | ns | >0.9999 | ns |
| day 0 (after surgery) vs. day 7 | 0.0138 | * | 0.0504 | ns | 0.054 | ns | 0.5947 | ns |
| Erythema | Edema | Serous Discharge | Purulent Discharge | |||||
|---|---|---|---|---|---|---|---|---|
| p Values | Summary | p Values | Summary | p Values | Summary | p Values | Summary | |
| FLE | ||||||||
| day 0 (after surgery) vs. day 3 | <0.0001 | **** | <0.0001 | **** | - | - | ||
| day 0 (after surgery) vs. day 5 | <0.0001 | **** | 0.0003 | *** | - | - | ||
| day 0 (after surgery) vs. day 7 | <0.0001 | **** | 0.0008 | *** | - | - | ||
| Control | ||||||||
| day 0 (after surgery) vs. day 3 | 0.3573 | ns | 0.9776 | ns | 0.0053 | ** | - | |
| day 0 (after surgery) vs. day 5 | 0.0177 | * | 0.5485 | ns | 0.0213 | * | - | |
| day 0 (after surgery) vs. day 7 | 0.0001 | *** | 0.0056 | ** | 0.1829 | ns | - | |
| Enrolment | Day 3 | Day 5 | Day 7 | |||||
|---|---|---|---|---|---|---|---|---|
| Isolated Bacteria | before Surgery | after Surgery | FLE | Control | FLE | Control | FLE | Control |
| Staphylococcus pseudintermedius | 9 | - | - | 3 | - | 2 | - | 1 |
| Staphylococcus aureus | 3 | - | - | 4 | - | 1 | - | - |
| Streptococcus spp. | 2 | - | - | 1 | - | 1 | - | - |
| Enterococcus spp. | 1 | - | - | - | - | 1 | - | 1 |
| Pseudomonas spp. | - | - | 1 | - | 1 | - | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marchegiani, A.; Troisi, A.; Bazzano, M.; Spaterna, A.; Fruganti, A. A Prospective, Blinded, Open-Label Clinical Trial to Assess the Ability of Fluorescent Light Energy to Enhance Wound Healing after Mastectomy in Female Dogs. Animals 2024, 14, 1250. https://doi.org/10.3390/ani14081250
Marchegiani A, Troisi A, Bazzano M, Spaterna A, Fruganti A. A Prospective, Blinded, Open-Label Clinical Trial to Assess the Ability of Fluorescent Light Energy to Enhance Wound Healing after Mastectomy in Female Dogs. Animals. 2024; 14(8):1250. https://doi.org/10.3390/ani14081250
Chicago/Turabian StyleMarchegiani, Andrea, Alessandro Troisi, Marilena Bazzano, Andrea Spaterna, and Alessandro Fruganti. 2024. "A Prospective, Blinded, Open-Label Clinical Trial to Assess the Ability of Fluorescent Light Energy to Enhance Wound Healing after Mastectomy in Female Dogs" Animals 14, no. 8: 1250. https://doi.org/10.3390/ani14081250
APA StyleMarchegiani, A., Troisi, A., Bazzano, M., Spaterna, A., & Fruganti, A. (2024). A Prospective, Blinded, Open-Label Clinical Trial to Assess the Ability of Fluorescent Light Energy to Enhance Wound Healing after Mastectomy in Female Dogs. Animals, 14(8), 1250. https://doi.org/10.3390/ani14081250






