Patient-Specific 3D-Printed Osteotomy Guides and Titanium Plates for Distal Femoral Deformities in Dogs with Lateral Patellar Luxation
Abstract
Simple Summary
Abstract
1. Introduction
2. Case Description
2.1. Animals and Study Design
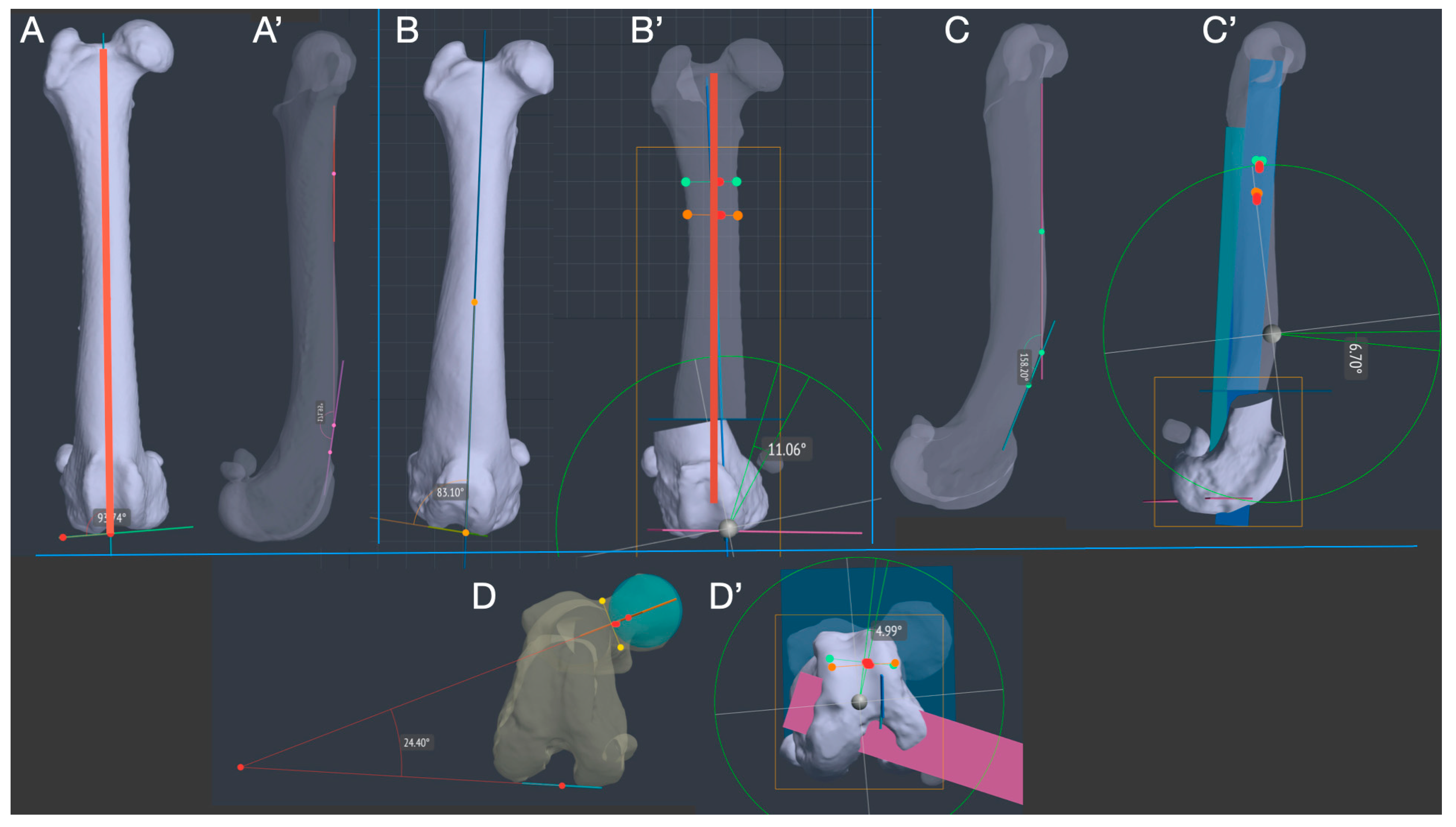
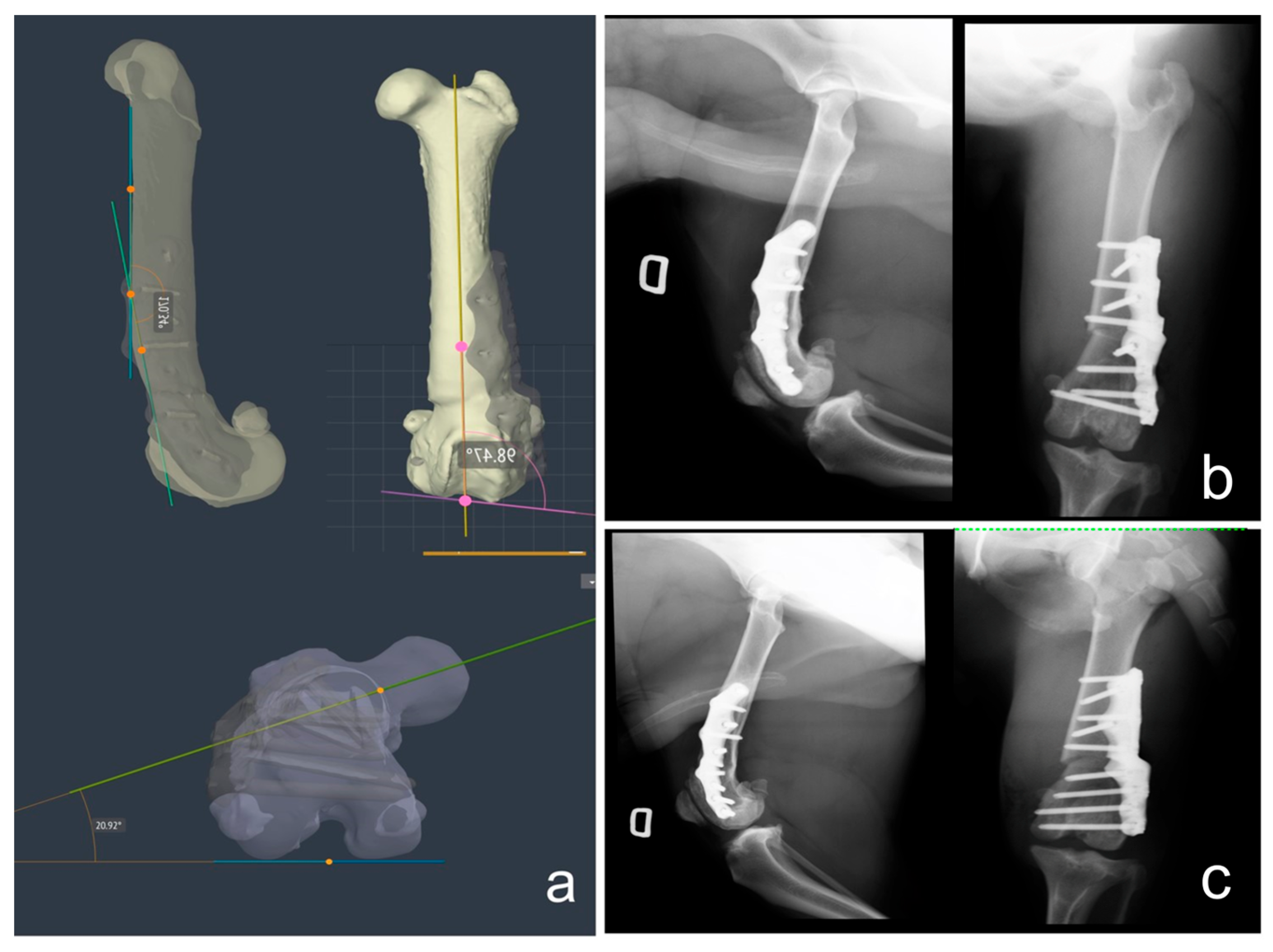
2.2. CT Scan Acquisition and Deformity 3D Measurements
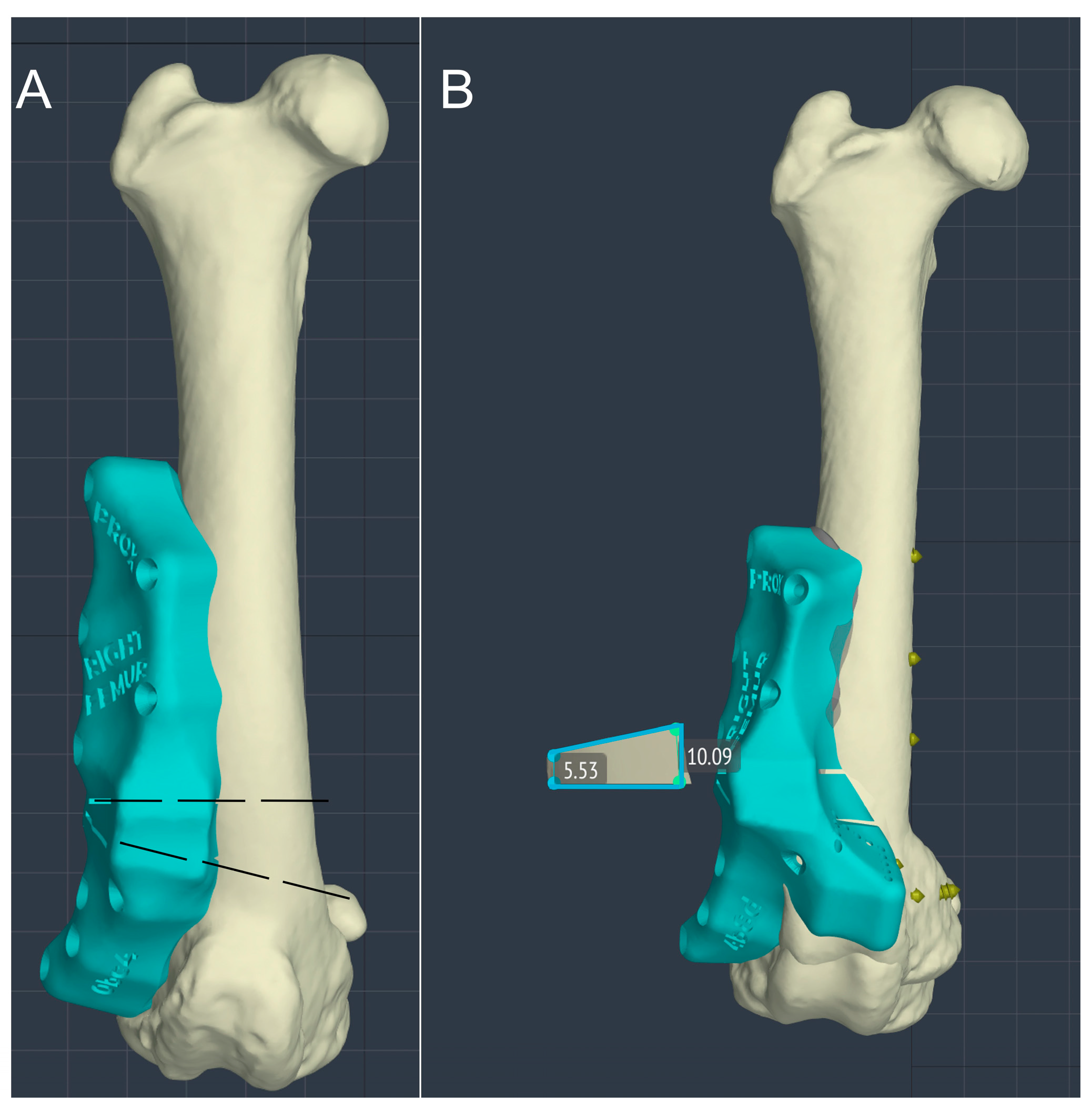
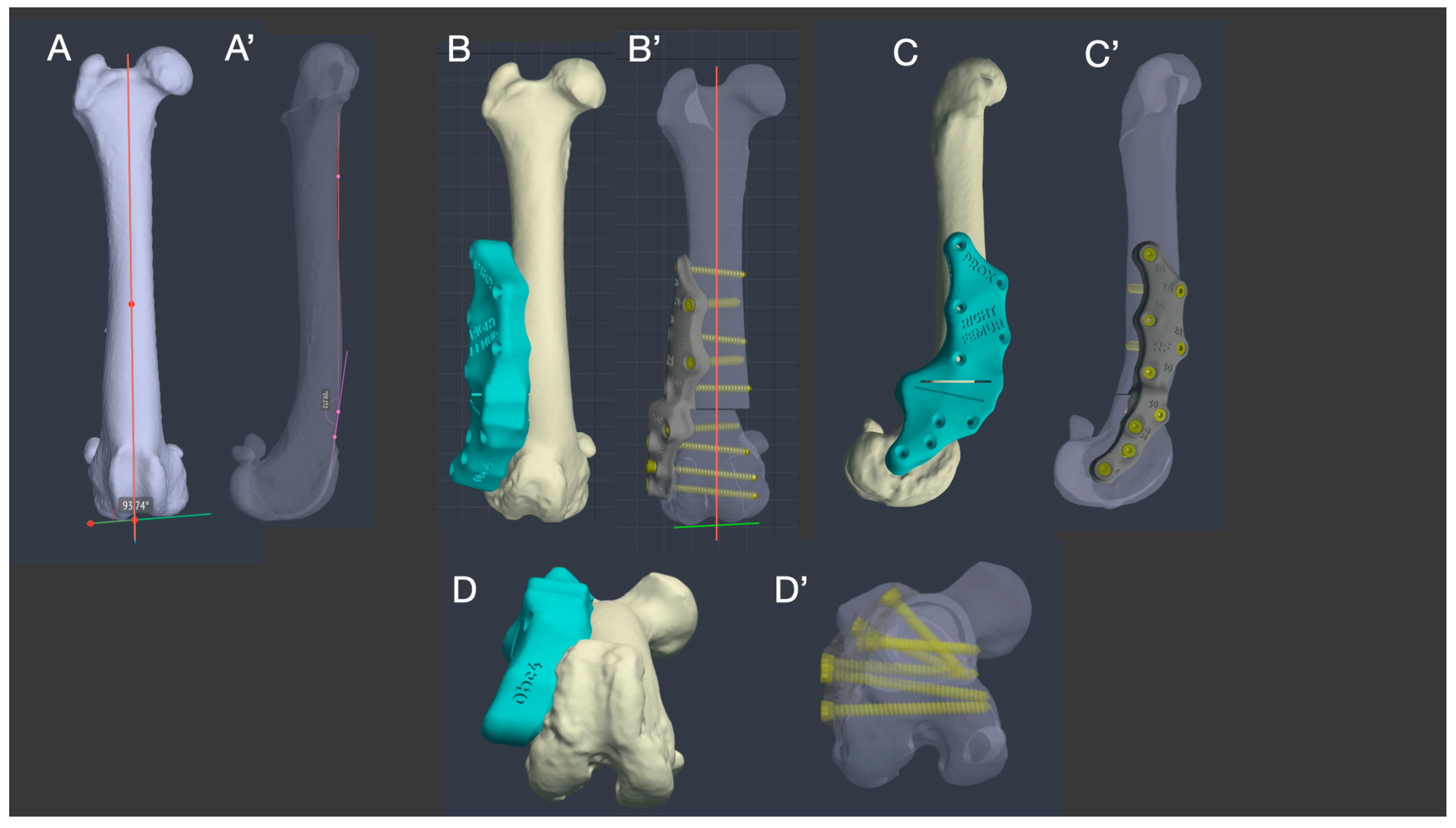
2.3. Virtual Surgery, Patient-Specific Osteotomy Guide and Titanium Plate Design
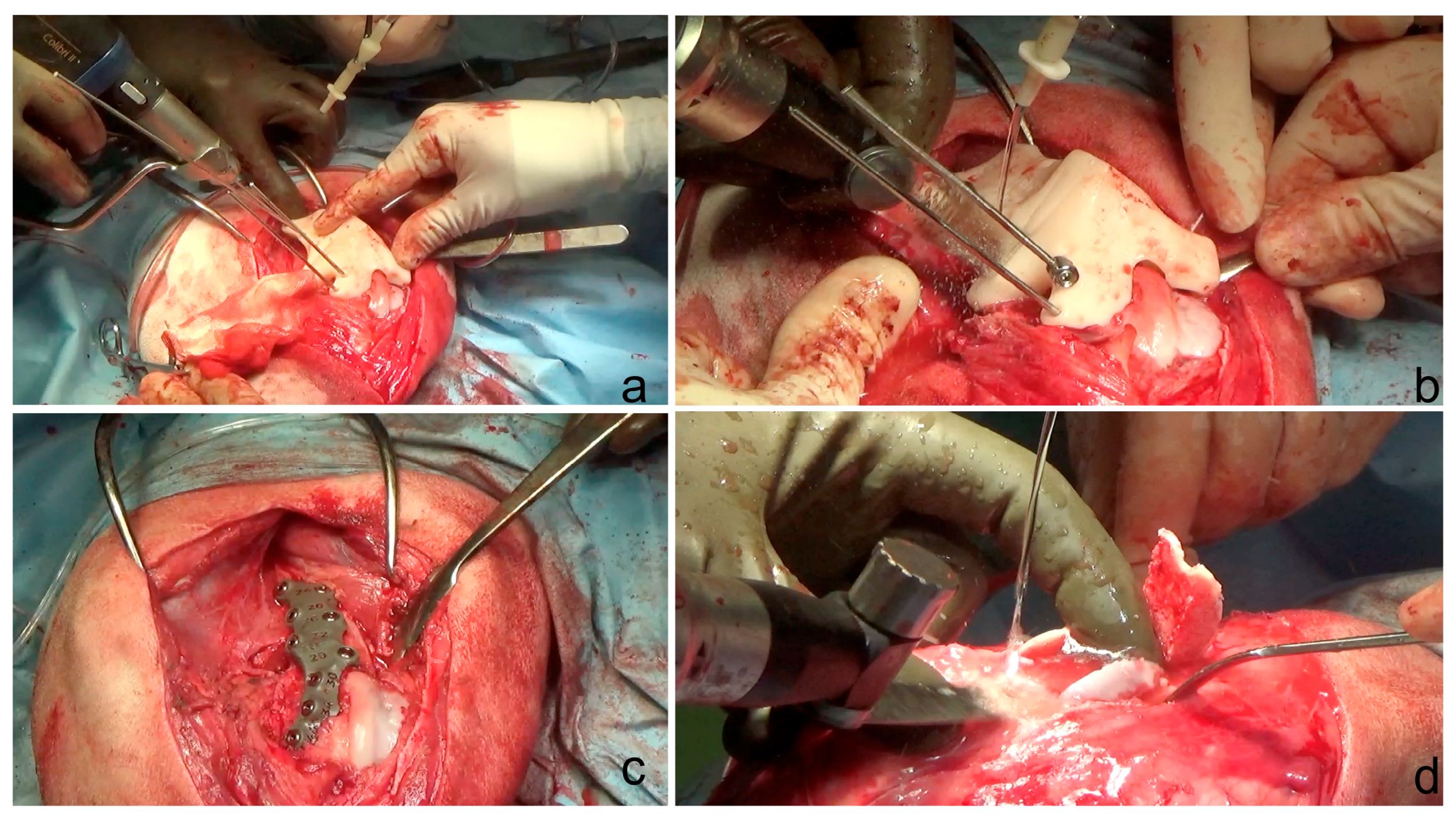
2.4. Surgical Technique
2.5. Postoperative Care
2.6. Postoperative CT Scan, X-rays and Joint Angle Measurements
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Di Dona, F.; Della Valle, G.; Fatone, G. Patellar luxation in dogs. Vet. Med. 2018, 9, 23–32. [Google Scholar] [CrossRef]
- Di Dona, F.; Della Valle, G.; Balestriere, C.; Lamagna, B.; Meomartino, L.; Napoleone, G.; Lamagna, F.; Fatone, G. Lateral patellar luxation in nine small breed dogs. Open Vet. J. 2016, 6, 255–258. [Google Scholar] [CrossRef]
- Kalff, S.; Butterworth, S.J.; Miller, A.; Keeley, B.; Baines, S.; McKee, W.M. Lateral patellar luxation in dogs: A retrospective study of 65 dogs. Vet. Comp. Orthop. Traumatol. 2014, 27, 130–134. [Google Scholar]
- Shaver, S.L.; Mayhew, K.N.; Sutton, J.S.; Mayhew, P.D.; Runge, J.J.; Brown, D.C.; Kass, P.H. Complications after corrective surgery for lateral patellar luxation in dogs: 36 cases (2000–2011). J. Am. Vet. Med. Assoc. 2014, 244, 444–448. [Google Scholar] [CrossRef]
- Gibbons, S.E.; Macias, C.; Tonzing, M.A.; Pinchbeck, G.L.; McKee, W.M. Patellar luxation in 70 large breed dogs. J. Small Anim. Pract. 2006, 47, 3–9. [Google Scholar] [CrossRef]
- Alam, M.R.; Lee, J.I.; Kang, H.S.; Kim, I.S.; Park, S.Y.; Lee, K.C.; Kim, N.S. Frequency and distribution of patellar luxation in dogs. 134 cases (2000 to 2005). Vet. Comp. Orthop. Traumatol. 2007, 20, 59–64. [Google Scholar] [CrossRef]
- LaFond, E.; Breur, G.J.; Austin, C.C. Breed susceptibility for developmental orthopedic diseases in dogs. J. Am. Anim. Hosp. Assoc. 2002, 38, 467–477. [Google Scholar] [CrossRef]
- L’Eplattenier, H.F.; Montavon, P. Patellar luxation in dogs and cats: Management and prevention. Comp. Cont. Edu. Pract. Vet. 2002, 24, 292–300. [Google Scholar]
- Bound, N.; Zakai, D.; Butterworth, S.J.; Pead, M. The prevalence of canine patellar luxation in three centres. Clinical features and radiographic evidence of limb deviation. Vet. Comp. Orthop. Traumatol. 2009, 22, 32–37. [Google Scholar] [PubMed]
- Harasen, G. Patellar luxation: Pathogenesis and surgical correction. Can. Vet. J. 2006, 47, 1037–1039. [Google Scholar] [PubMed]
- DeTora, M.D.; Boudrieau, R.J. Complex angular and torsional deformities (distal femoral malunions). Preoperative planning using stereolithography and surgical correction with locking plate fixation in four dogs. Vet. Comp. Orthop. Traumatol. 2016, 29, 416–425. [Google Scholar] [CrossRef]
- Arthurs, G.I.; Langley-Hobbs, S.J. Complications associated with corrective surgery for patellar luxation in 109 dogs. Vet. Surg. 2006, 35, 559–566. [Google Scholar] [CrossRef]
- Roch, S.P.; Gemmill, T.J. Treatment of medial patellar luxation by femoral closing wedge ostectomy using a distal femoral plate in four dogs. J. Small Anim. Pract. 2008, 49, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Bosio, F.; Bufalari, A.; Peirone, B.; Petazzoni, M.; Vezzoni, A. Prevalence, treatment and outcome of patellar luxation in dogs in Italy. A retrospective multicentric study (2009–2014). Vet. Comp. Orthop. Traumatol. 2017, 30, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Brower, B.E.; Kowaleski, M.P.; Peruski, A.M.; Pozzi, A.; Dyce, J.; Johnson, K.A.; Boudrieau, R.J. Distal femoral lateral closing wedge osteotomy as a component of comprehensive treatment of medial patellar luxation and distal femoral varus in dogs. Vet. Comp. Orthop. Traumatol. 2017, 30, 20–27. [Google Scholar] [CrossRef]
- Panichi, E.; Cappellari, F.; Olimpo, M.; Piras, L.A.; Radasch, R.; Ferretti, A.; Peirone, B. Distal femoral osteotomy using a novel deformity reduction device. Vet. Comp. Orthop. Traumatol. 2016, 29, 426–432. [Google Scholar]
- Swiderski, J.K.; Palmer, R.H. Long-term outcome of distal femoral osteotomy for treatment of combined distal femoral varus and medial patellar luxation: 12 cases (1999–2004). J. Am. Vet. Med. Assoc. 2007, 231, 1070–1075. [Google Scholar] [CrossRef]
- Gigi, R.; Gortzak, Y.; Barriga Moreno, J.; Golden, E.; Gabay, R.; Rumack, N.; Yaniv, M.; Dadia, S.; Segev, E. 3D-printed Cutting Guides for Lower Limb Deformity Correction in the Young Population. J. Pediatr. Orthop. 2022, 42, e427–e434. [Google Scholar] [CrossRef] [PubMed]
- Oraa, J.; Beitia, M.; Fiz, N.; González, S.; Sánchez, X.; Delgado, D.; Sánchez, M. Custom 3D-Printed Cutting Guides for Femoral Osteotomy in Rotational Malalignment Due to Diaphyseal Fractures: Surgical Technique and Case Series. J. Clin. Med. 2021, 10, 3366. [Google Scholar] [CrossRef]
- Fiz, N.; Delgado, D.; Sánchez, X.; Sánchez, P.; Bilbao, A.M.; Oraa, J.; Sánchez, M. Application of 3D Technology and Printing for Femoral Derotation Osteotomy: Case and Technical Report. Ann. Transl. Med. 2017, 5, 400. [Google Scholar] [CrossRef]
- Wong, K.C. 3D-Printed Patient-Specific Applications in Orthopedics. Orthop. Res. Rev. 2016, 8, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Chai, W.; Xu, M.; Zhang, G.; Zhang, L.; Gou, W.; Ni, M.; Chen, J. Computer-Aided Design and Custom-Made Guide in Corrective Osteotomy for Complex Femoral Deformity. J. Huazhong Univ. Sci. Technol. Med. Sci. 2013, 33, 398–405. [Google Scholar] [CrossRef]
- Memarian, P.; Pishavar, E.; Zanotti, F.; Trentini, M.; Camponogara, F.; Soliani, E.; Gargiulo, P.; Isola, M.; Zavan, B. Active Materials for 3D Printing in Small Animals: Current Modalities and Future Directions for Orthopedic Applications. Int. J. Mol. Sci. 2022, 23, 1045. [Google Scholar] [CrossRef]
- Mendaza-DeCal, R.; Peso-Fernandez, S.; Rodriguez-Quiros, J. Orthotics and prosthetics by 3D-printing: Accelerating its fabrication flow. Res. Vet. Sci. 2023, 162, 104960. [Google Scholar] [CrossRef]
- De Armond, C.C.; Lewis, D.D.; Kim, S.E.; Biedrzycki, A.H. Accuracy of virtual surgical planning and custom three-dimensionally printed osteotomy and reduction guides for acute uni- and biapical correction of antebrachial deformities in dogs. J. Am. Vet. Med. Assoc. 2022, 260, 1–9. [Google Scholar] [CrossRef]
- Carvajal, J.L.; Kim, S.E. Proximal femoral deformity correction and total hip arthroplasty in a dog using 3D printed custom guides. Vet. Surg. 2023, 52, 168–175. [Google Scholar] [CrossRef]
- Carwardine, D.R.; Gosling, M.J.; Burton, N.J.; O’Malley, F.L.; Parsons, K.J. Three-dimensional-printed patient-specific osteotomy guides, repositioning guides and titanium plates for acute correction of antebrachial limb deformities in dogs. Vet. Comp. Orthop. Traumatol. 2021, 34, 43–52. [Google Scholar] [CrossRef]
- Hall, E.L.; Baines, S.; Bilmont, A.; Oxley, B. Accuracy of patientspecific three-dimensional-printed osteotomy and reduction guides for distal femoral osteotomy in dogs with medial patella luxation. Vet. Surg. 2019, 48, 584–591. [Google Scholar] [CrossRef]
- Oxley, B. Bilateral shoulder arthrodesis in a Pekinese using three-dimensional printed patient-specific osteotomy and reduction guides. Vet. Comp. Orthop. Traumatol. 2017, 30, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Fracka, A.B.; Oxley, B.; Allen, M.J. 3D-printed, patient-specific cutting guides improve femoral and tibial cut alignment in canine total knee replacement. Vet. Surg. 2023, 52, 674–685. [Google Scholar] [CrossRef]
- Longo, F.; Penelas, A.; Gutbrod, A.; Pozzi, A. Three-dimensional computer-assisted corrective osteotomy with a patient-specific surgical guide for an antebrachial limb deformity in two dogs. Schweiz. Arch. Tierheilkd. 2019, 161, 473–479. [Google Scholar] [CrossRef] [PubMed]
- Longo, F.; Nicetto, T.; Knell, S.C.; Evans, R.B.; Isola, M.; Pozzi, A. Three-dimensional volume rendering planning, surgical treatment, and clinical outcomes for femoral and tibial detorsional osteotomies in dogs. Vet. Surg. 2022, 51, 1126–1141. [Google Scholar] [CrossRef]
- Shi, J.; Lv, W.; Wang, Y.; Ma, B.; Cui, W.; Liu, Z.; Han, K. Three dimensional patient-specific printed cutting guides for closing-wedge distal femoral osteotomy. Int. Orthop. 2019, 43, 619–624. [Google Scholar] [CrossRef]
- Worth, A.J.; Crosse, K.R.; Kersley, A. Computer-Assisted Surgery Using 3D Printed Saw Guides for Acute Correction of Antebrachial Angular Limb Deformities in Dogs. Vet. Comp. Orthop. Traumatol. 2019, 32, 241–249. [Google Scholar] [CrossRef]
- Popov, V.V.; Muller-Kamskii, G.; Katz-Demyanetz, A.; Kovalevsky, A.; Usov, S.; Trofimcow, D.; Dzhenzhera, G.; Koptyug, A. Additive manufacturing to veterinary practice: Recovery of bony defects after the osteosarcoma resection in canines. Biomed. Eng. Lett. 2019, 9, 97–108. [Google Scholar] [CrossRef]
- Easter, T.G.; Bilmont, A.; Pink, J.; Oxley, B. Accuracy of threedimensional printed patient-specific drill guides for treatment of canine humeral intracondylar fissure. Vet. Surg. 2020, 49, 363–372. [Google Scholar] [CrossRef]
- Lam, G.; Kim, S.Y. Three-dimensional computer-assisted surgical planning and use of three-dimensional printing in the repair of a complex articular femoral fracture in a dog. Vet. Comp. Orthop. Traumatol. 2018, 1, e12–e18. [Google Scholar] [CrossRef]
- Oxley, B. A 3-dimensional-printed patient-specific guide system for minimally invasive plate osteosynthesis of a comminuted mid-diaphyseal humeral fracture in a cat. Vet. Surg. 2018, 47, 445–453. [Google Scholar] [CrossRef]
- Toni, C.; Oxley, B.; Behr, S. Atlanto-axial ventral stabilisation using 3D-printed patient-specific drill guides for placement of bicortical screws in dogs. J. Small Anim. Pract. 2020, 61, 609–616. [Google Scholar] [CrossRef]
- Kamishina, H.; Sugawara, T.; Nakata, K.; Nishida, H.; Yada, N.; Fujioka, T.; Nagata, Y.; Doi, A.; Konno, N.; Uchida, F.; et al. Clinical application of 3D printing technology to the surgical treatment of atlantoaxial subluxation in small breed dogs. PLoS ONE 2019, 14, e0216445. [Google Scholar] [CrossRef] [PubMed]
- Toni, C.; Oxley, B.; Clarke, S.; Behr, S. Accuracy of placement of pedicle screws in the lumbosacral region of dogs using 3Dprinted patient-specific drill guides. Vet. Comp. Orthop. Traumatol. 2021, 34, 53–58. [Google Scholar]
- Hamilton-Bennett, S.E.; Oxley, B.; Behr, S. Accuracy of a patient-specific 3D printed drill guide for placement of cervical transpedicular screws. Vet. Surg. 2018, 47, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Dudley, R.M.; Kowaleski, M.P.; Drost, W.T.; Dyce, J. Radiographic and computed tomographic determination of femoral varus and torsion in the dog. Vet. Radiol. Ultrasound 2006, 47, 546–552. [Google Scholar] [CrossRef]
- Paley, D. Principles of Deformity Correction; Paley, D., Herzenberg, J.E., Eds.; Springer: Berlin/Heidelberg, Germany, 2002; pp. 99–154. [Google Scholar]
- Kieves, N.R.; Bergh, M.S.; Zellner, E.; Wang, C. Pilot study measuring the effects of bandaging and cold compression therapy following tibial plateau levelling osteotomy. J. Small Anim. Pract. 2016, 57, 543–547. [Google Scholar] [CrossRef] [PubMed]
- Drygas, K.A.; Mcclure, S.R.; Goring, R.L.; Pozzi, A.; Robertson, S.A.; Wang, C. Effect of cold compression therapy on postoperative pain, swelling, range of motion, and lameness after tibial plateau leveling osteotomy in dogs. J. Am. Vet. Med. Assoc. 2011, 238, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Szabo, S.D.; Levine, D.; Marcellin-Little, D.J.; Sidaway, B.K.; Hofmeister, E.; Urtuzuastegui, E. Cryotherapy Improves Limb Use but Delays Normothermia Early After Stifle Joint Surgery in Dogs. Front. Vet. Sci. 2020, 7, 381. [Google Scholar] [CrossRef]
- Fox, D.B.; Tomlinson, J.L.; Cook, J.L.; Breshears, L.M. Principles of uniapical and biapical radial deformity correction using dome osteotomies and the center of rotation of angulation methodology in dogs. Vet. Surg. 2006, 35, 67–77. [Google Scholar] [CrossRef]
- Knapp, J.L.; Tomlinson, J.L.; Fox, D.B. Classification of angular limb deformities affecting the canine radius and ulna using the center of rotation of angulation method. Vet. Surg. 2016, 45, 295–302. [Google Scholar] [CrossRef]
- Meola, S.D.; Wheeler, J.L.; Rist, C.L. Validation of a technique to assess radial torsion in the presence of procurvatum and valgus deformity using computed tomography: A cadaveric study. Vet. Surg. 2008, 37, 525–529. [Google Scholar] [CrossRef]
- Piras, L.A.; Peirone, B.; Fox, D. Effects of antebrachial torsion on the measurement of angulation in the frontal plane: A cadaveric radiographic analysis. Vet. Comp. Orthop. Traumatol. 2012, 25, 89–94. [Google Scholar] [CrossRef]
- Eby, A.; Bleedorn, J. A computed tomographic graphical approach to guide correction of femoral torsion. Vet. Surg. 2020, 49, 1015–1023. [Google Scholar] [CrossRef] [PubMed]
- Oxley, B.; Gemmill, T.J.; Pink, J.; Clarke, S.; Parry, A.; Baines, S.; Malcolm McKee, W. Precision of a novel computed tomographic method for quantification of femoral varus in dogs and an assessment of the effect of femoral malpositioning. Vet. Surg. 2013, 42, 751–758. [Google Scholar] [CrossRef] [PubMed]
- Barnes, D.M.; Anderson, A.A.; Frost, C.; Barnes, J. Repeatability and reproducibility of measurements of femoral and tibial alignment using computed tomography multiplanar reconstructions. Vet. Surg. 2015, 44, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, J.; Fox, D.; Cook, J.L.; Keller, G.G. Measurement of femoral angles in four dog breeds. Vet. Surg. 2007, 36, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Marcellin-Little, D.J.; Levine, D. Principles and application of range of motion and stretching in companion animals. Vet. Clin. N. Am. Small Anim. Pract. 2015, 45, 57–72. [Google Scholar] [CrossRef]
- Baltzer, W.I. Rehabilitation of companion animals following orthopaedic surgery. N. Z. Vet. J. 2020, 68, 157–167. [Google Scholar] [CrossRef]
- Drum, M.G.; Marcellin-Little, D.J.; Davis, M.S. Principles and applications of therapeutic exercises for small animals. Vet. Clin. N. Am. Small Anim. Pract. 2015, 45, 73–90. [Google Scholar] [CrossRef]
- Townsend, A.; Guevar, J.; Oxley, B.; Hetzel, S.; Bleedorn, J. Comparison of three-dimensional printed patient-specific guides versus freehand approach for radial osteotomies in normal dogs: Ex vivo model. Vet. Surg. 2024, 53, 234–242. [Google Scholar] [CrossRef]
- Lee, H.R.; Adam, G.O.; Yang, D.K.; Tungalag, T.; Lee, S.J.; Kim, J.S.; Kang, H.S.; Kim, S.J.; Kim, N.S. An Easy and Economical Way to Produce a Three-Dimensional Bone Phantom in a Dog with Antebrachial Deformities. Animals 2020, 10, 1445. [Google Scholar] [CrossRef] [PubMed]
- Olimpo, M.; Piras, L.A.; Peirone, B.; Fox, D.B. Comparison of osteotomy technique and jig type in completion of distal femoral osteotomies for correction of medial patellar luxation: An in vitro study. Vet. Comp. Orthop. Traumatol. 2017, 30, 28–36. [Google Scholar] [PubMed]
- Hespel, A.M.; Wilhite, R.; Hudson, J. Invited review—Applications for 3D printers in veterinary medicine. Vet. Radiol. Ultrasound 2014, 55, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Mulford, J.S.; Babazadeh, S.; Mackay, N. Three-dimensional printing in orthopaedic surgery: Review of current and future applications. ANZ J. Surg. 2016, 86, 648–653. [Google Scholar] [CrossRef] [PubMed]

| Dog | Side | aLDFA(°) | Proc. | FTA | Imaging Modality | Concurrent Deformity | Other Procedures | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre Op | Virtual Op | Post Op | Pre Op | Virtual Op | Post Op | Pre Op | Virtual Op | Post Op | |||||
| 1 | R | 83° | 94° | 98° | 158° | 170° | 170° | 25° | 20° | 20° | CT | Mild Metatarsal rotation | CWO; TBR; LD; MER. |
| 1 | L | 82° | 94° | 98° | 156° | 170° | 169° | 29° | 20° | 20° | CT | Mild Metatarsal rotation | CWO; TBR; LD; MER. |
| 2 | R | 82° | 94° | 95° | 163° | 170° | 172° | 29° | 20° | 20° | CT | Mild Metatarsal rotation | CWO; TBR; LD; MER. |
| PROM | TIE Circumference | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dog | Side | Pre Operative | FWUP 6 m | FWUP 18 m | FWUP 24 m | FWUP 36 m | Pre Operative | FWUP 6 m | FWUP 18 m | FWUP 24 m | FWUP 36 m |
| 1 | R | 1 = 130 2 = 35° | 1 = 140 2 = 90° | 1 = 150 2 = 80° | 1 = 138 2 = 80° | 1 = 138 2 = 80° | 28 cm | 38 cm | 42 cm | 42 cm | 42 cm |
| 1 | L | 1 = 125 2 = 35° | 1 = 140 2 = 80° | 1 = 138 2 = 80° | 1 = 138 2 = 80° | 1 = 140 2 = 80° | 28 cm | 39 cm | 32 cm | 39 cm | 40 cm |
| 2 | R | 1 = 130 2 = 35° | 1 = 155 2 = 70° | 1 = 155 2 = 60° | 1 = 155 2 = 60° | 1 = 155 2 = 60° | 30 cm | 37 cm | 42 cm | 42 cm | 42 cm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panichi, E.; Cappellari, F.; Burkhan, E.; Principato, G.; Currenti, M.; Tabbì, M.; Macrì, F. Patient-Specific 3D-Printed Osteotomy Guides and Titanium Plates for Distal Femoral Deformities in Dogs with Lateral Patellar Luxation. Animals 2024, 14, 951. https://doi.org/10.3390/ani14060951
Panichi E, Cappellari F, Burkhan E, Principato G, Currenti M, Tabbì M, Macrì F. Patient-Specific 3D-Printed Osteotomy Guides and Titanium Plates for Distal Femoral Deformities in Dogs with Lateral Patellar Luxation. Animals. 2024; 14(6):951. https://doi.org/10.3390/ani14060951
Chicago/Turabian StylePanichi, Enrico, Fulvio Cappellari, Ekaterina Burkhan, Gaetano Principato, Marco Currenti, Marco Tabbì, and Francesco Macrì. 2024. "Patient-Specific 3D-Printed Osteotomy Guides and Titanium Plates for Distal Femoral Deformities in Dogs with Lateral Patellar Luxation" Animals 14, no. 6: 951. https://doi.org/10.3390/ani14060951
APA StylePanichi, E., Cappellari, F., Burkhan, E., Principato, G., Currenti, M., Tabbì, M., & Macrì, F. (2024). Patient-Specific 3D-Printed Osteotomy Guides and Titanium Plates for Distal Femoral Deformities in Dogs with Lateral Patellar Luxation. Animals, 14(6), 951. https://doi.org/10.3390/ani14060951






