A Bilateral Acetabular Physeal Fracture Treated with External Fixation in an Immature Cat
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
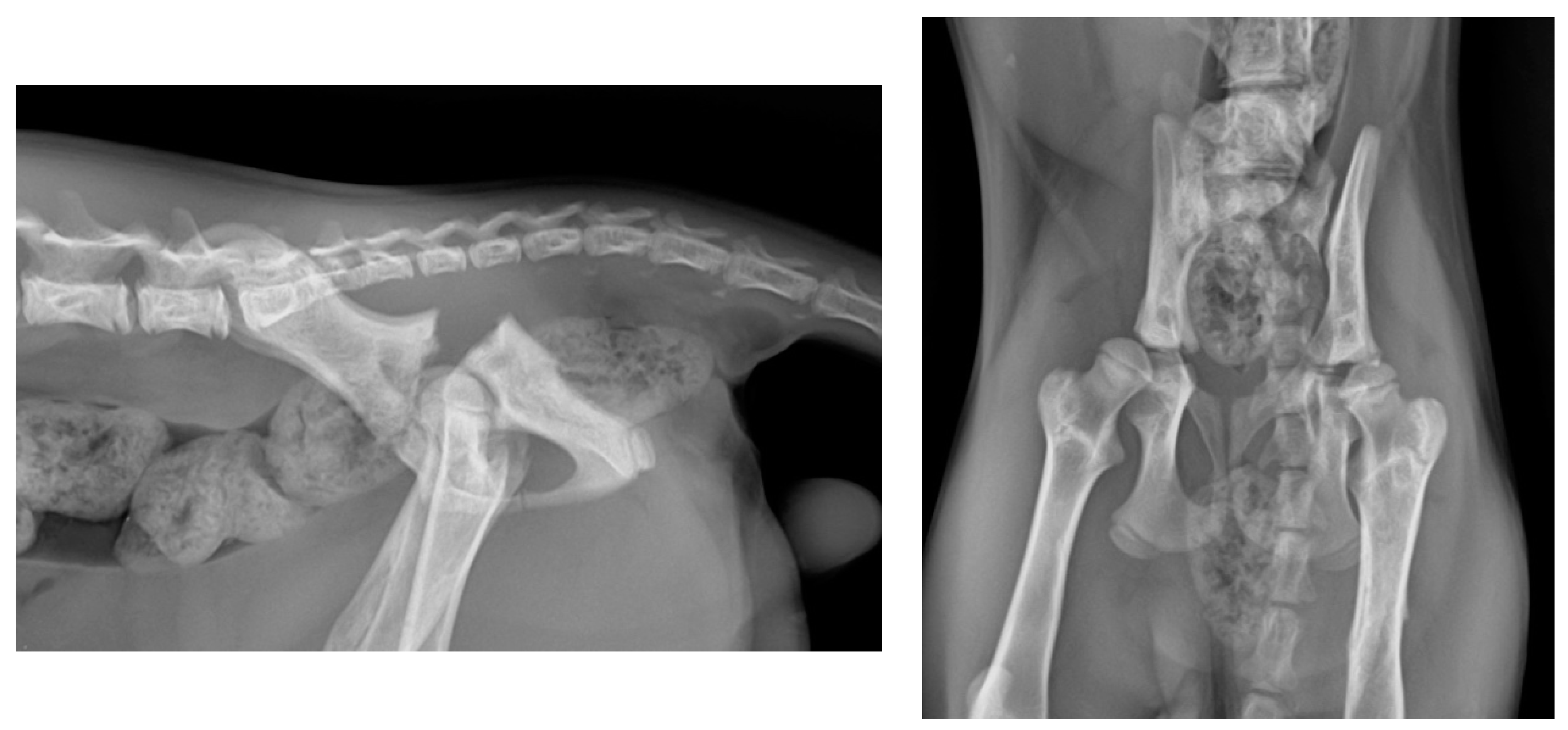
2.1. Preoperative Management
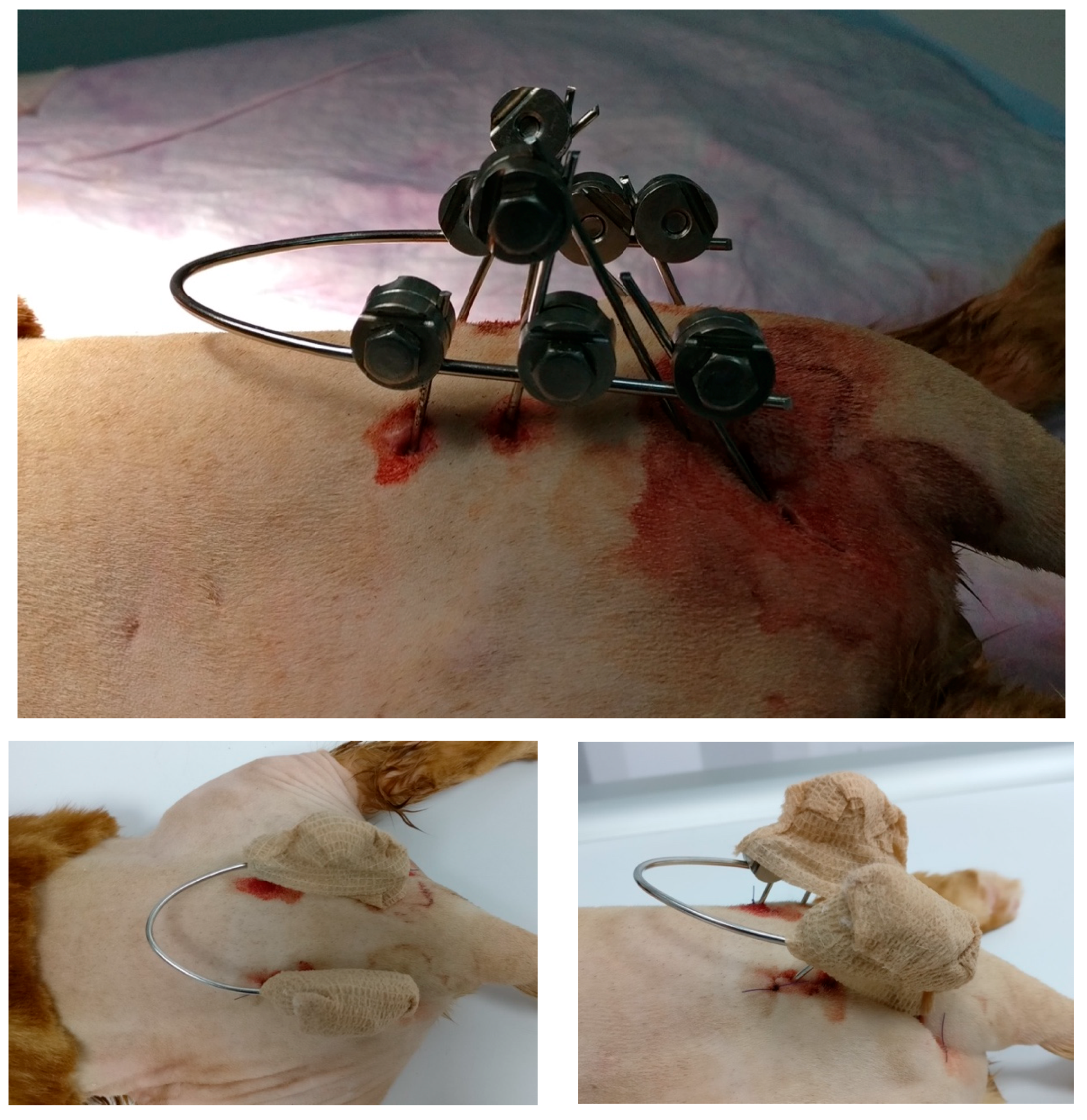
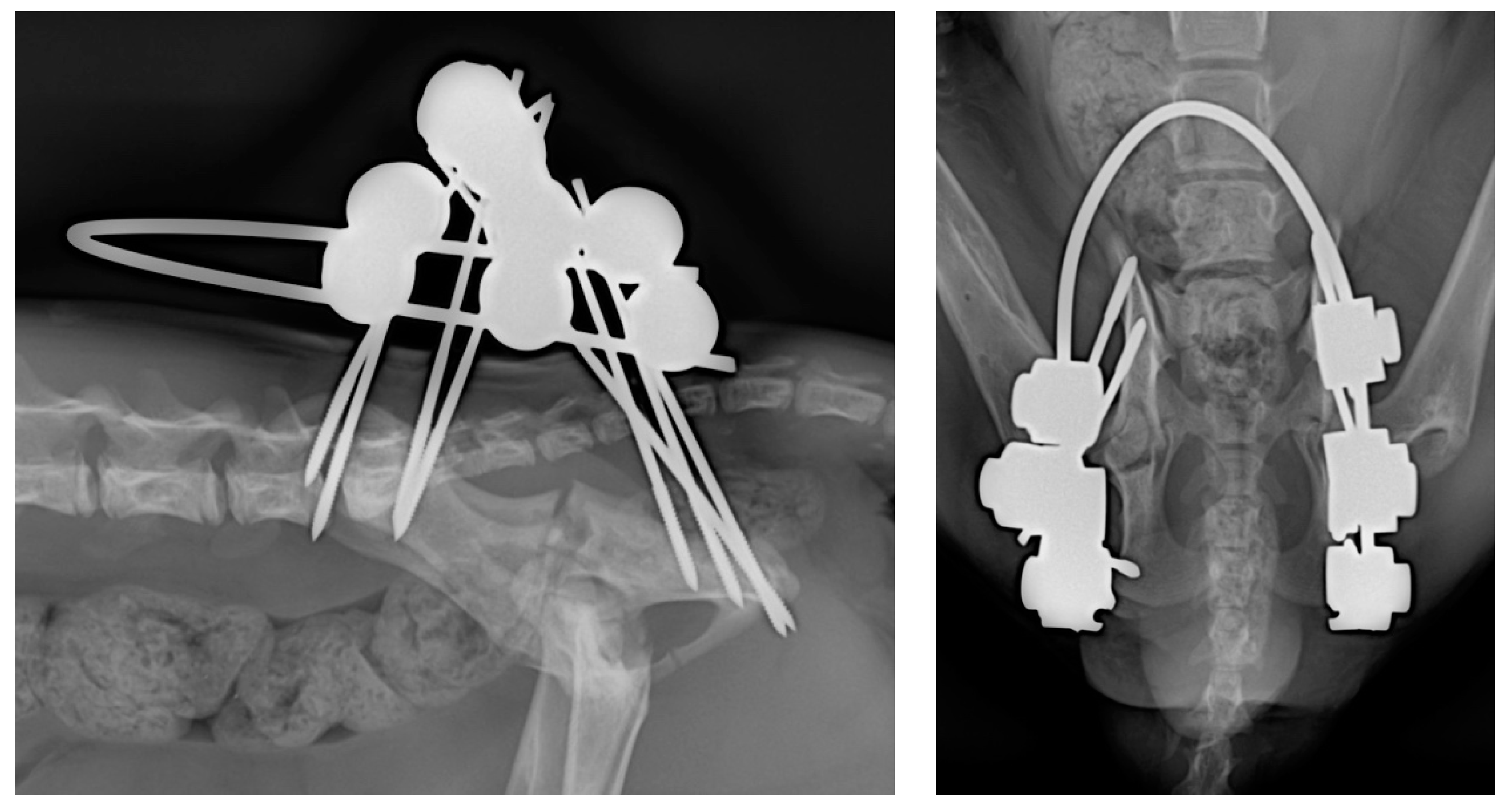
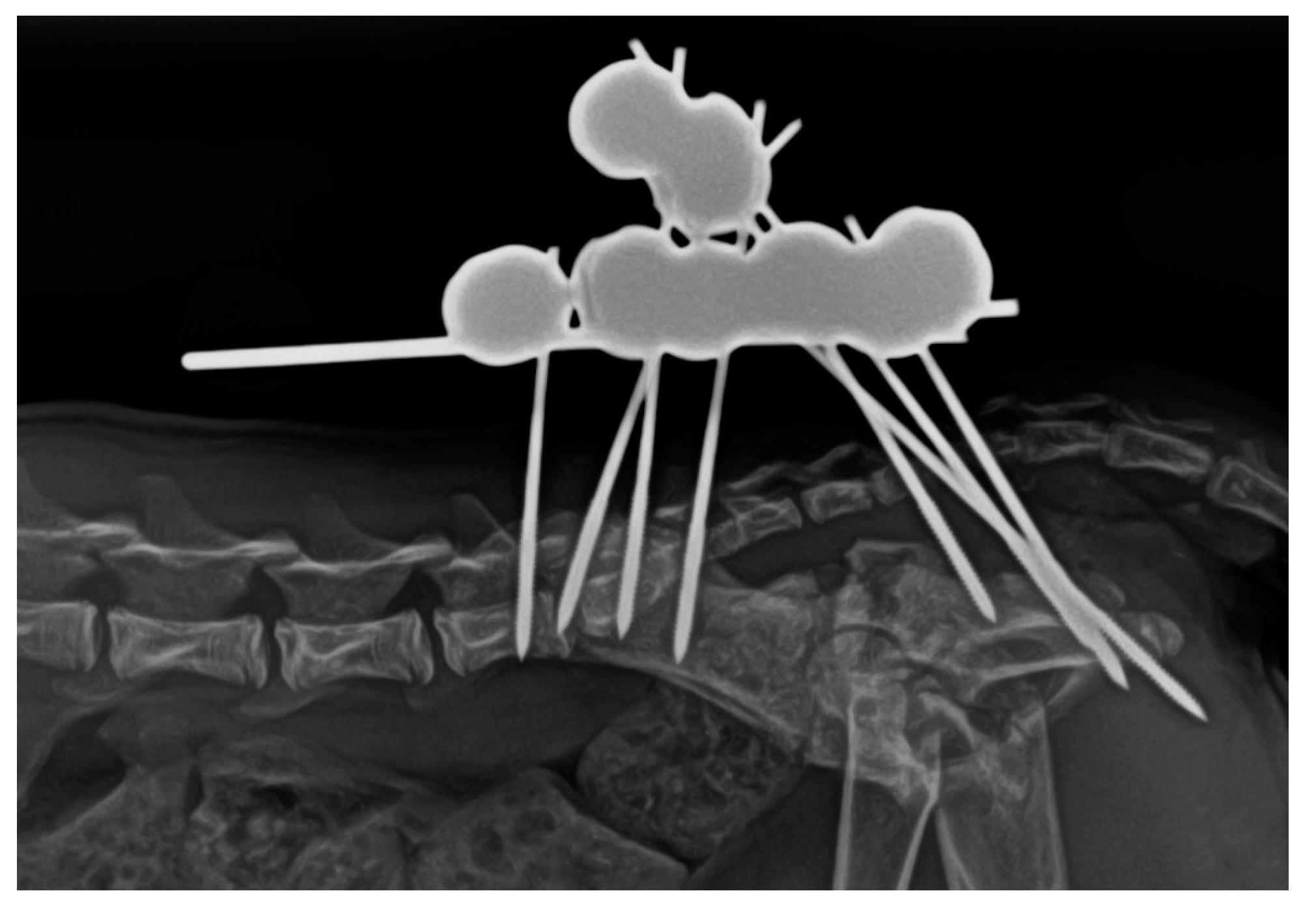
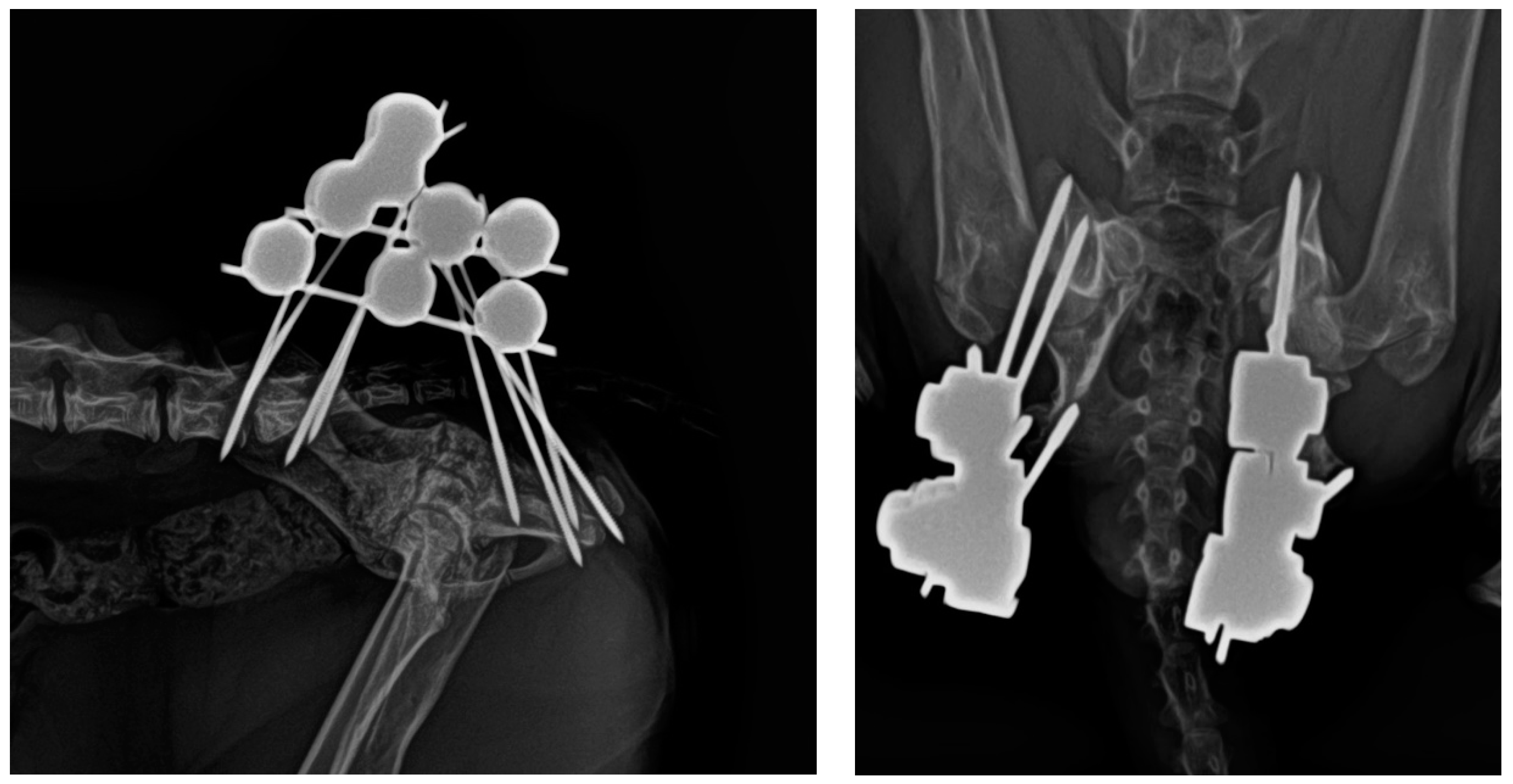
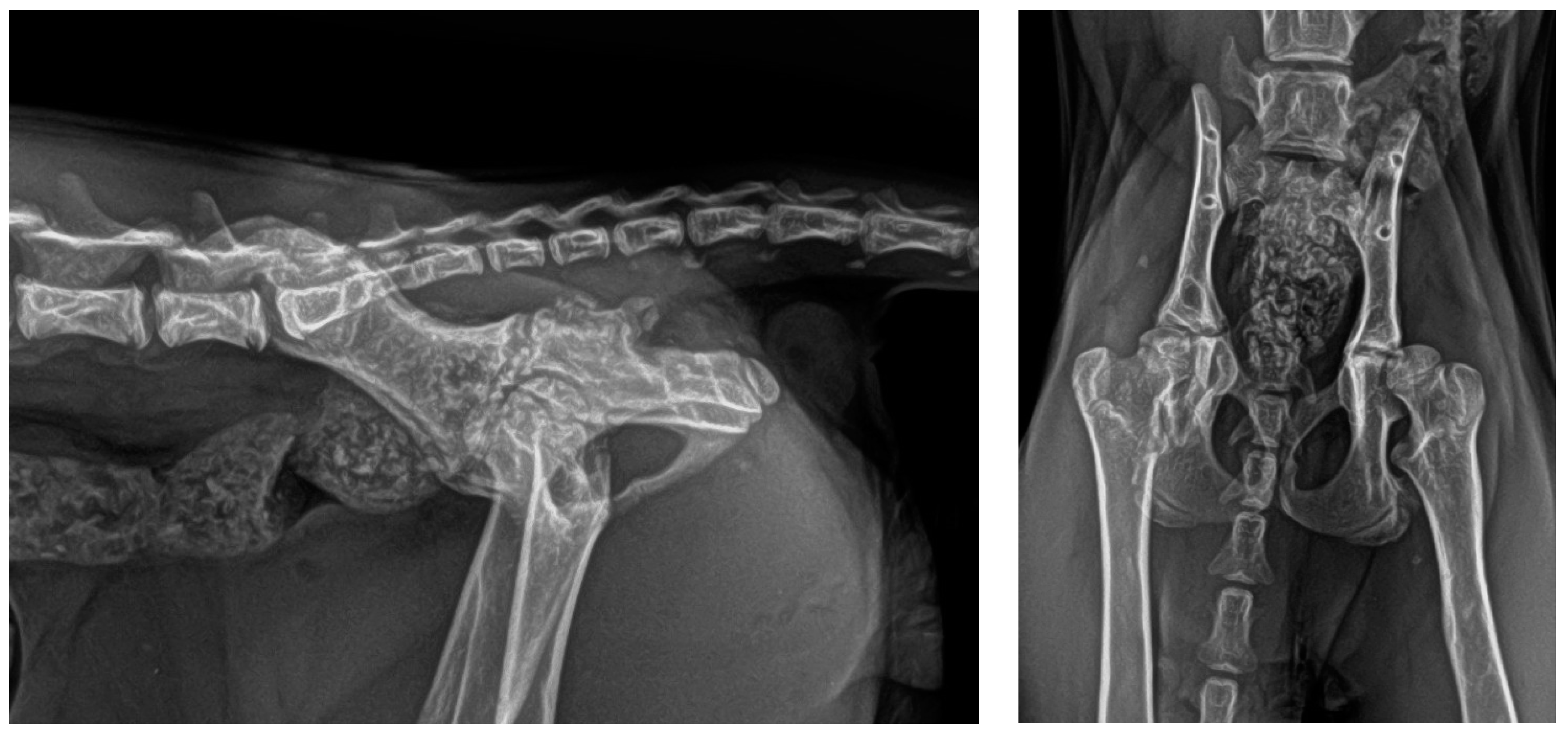
2.2. Surgical Technique
- Sacral tuberosity corridor of the ilium, near the origin of the gluteus medius muscle. The pins were inserted at an angle of 10–15° from proximo-medial to disto-lateral to the vertical.
- Corridor of the body of the ilium, in the caudal aspect, along the origin of the gluteus profundus muscle, with pins inserted at an angle of 10–15° to the vertical of the iliac crest.
- Ischial tuberosity corridor, with pins inserted at an entry angle of 10–15° to the vertical.
2.3. Postoperative Care
2.4. Follow-Up
- Level 0: no functional or locomotor alterations. The patient walks normally.
- Level 1: mild locomotor alterations, with occasional mild lameness.
- Level 2: mild-to-moderate locomotor alterations, with mild and consistent lameness.
- Level 3: moderate locomotor alterations, with moderate and partially constant lameness.
- Level 4: severe locomotor alterations, with pronounced lameness involving intermittent non-use of the limb.
- Level 5: very severe functional alterations with complete limb disuse.
- Level A: No apparent signs of pain. The animal exhibits no complaints upon manipulation. Considered normal behaviour.
- Level B: Mild -to-moderate signs of pain. The animal shows some discomfort with occasional spontaneous moans. There may be moderate difficulties in urination and defecation. No other significant behavioural alterations.
- Level C: Severe signs of pain. Inability to handle the patient without accompanying vocalisations. Severe difficulties in urination and defecation. Apathy and depression.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Langley-Hobbs, S.J.; Sissener, T.R.; Shales, C.J. Tension band stabilisation of acetabular physeal fractures in four kittens. J. Feline Med. Surg. 2007, 9, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Krebs, R.C.; Roe, S.C.; Lascelles, B.D.X.; Marcellin-Little, D.J.; Trumpatori, B.J.; Spodnick, G. Biomechanical evaluation of the influence of an intramedullary pin on the stability of a feline ilial fracture model stabilized with a bone plate. Vet. Surg. 2014, 43, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Boswell, K.A.; Boone, E.G.; Boudrieau, R.J. Reduction and temporary stabilization of acetabular fractures using ASIF mandibular reduction forceps: Technique and results using plate fixation in 25 dogs. Vet. Surg. 2001, 30, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Haine, D.L.; Parsons, K.; Barthelemy, N.; Burton, N.; Langley-Hobbs, S.L. Outcome of surgical stabilisation of acetabular fractures in 16 cats. J. Feline Med. Surg. 2019, 21, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Lafuente, P. Young, male neutered, obese, lame? Non-traumatic fractures of the femoral head and neck. J. Feline Med. Surg. 2011, 13, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Borak, D.; Wunderlin, N.; Brückner, M.; Schwarz, G.; Klang, A. Slipped capital femoral epiphysis in 17 Maine Coon cats. J. Feline Med. Surg. 2017, 19, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, G. Spontaneous capital femoral physeal fracture in a cat. Can. Vet. J. 2013, 54, 698–700. [Google Scholar]
- McNicholas, W.T.; Wilkens, B.E.; Blevins, W.E.; Snyder, P.W.; McCabe, G.P.; Applewhite, A.A.; Laverty, P.H.; Breur, G.J. Spontaneous femoral capital physeal fractures in adult cats: 26 cases (1996–2001). J. Am. Vet. Med. Assoc. 2002, 221, 1731–1736. [Google Scholar] [CrossRef]
- Diehm, M.; Dening, R.; Dziallas, P.; Wohlsein, P.; Schmicke, M.; Mischke, R. Bilateral femoral capital physeal fractures in an adult cat with suspected congenital primary hypothyroidism. Tierarztl. Prax. Ausg. K Kleintiere Heimtiere 2019, 47, 48–54. [Google Scholar] [CrossRef]
- Meeson, R.L.; Geddes, A.T. Management and long-term outcome of pelvic fractures: A retrospective study of 43 cats. J. Feline Med. Surg. 2017, 19, 36–41. [Google Scholar] [CrossRef]
- Orrenius, E. Long Term Outcome and Quality of Life in Cats and Dogs Suffering from Pelvic Fractures. Ph.D. Thesis, Swedish University of Agricultural Sciences, Uppsala, Sweden, 2019. [Google Scholar]
- Piana, F.; Solano, M.; Kalff, S.; Yeadon, R. Locking Plate Fixation for Canine Acetabular Fractures. Vet. Comp. Orthop. Traumatol. 2020, 33, 294–300. [Google Scholar] [CrossRef]
- Roberts, V.J.; Parsons, K.; Sajik, K.; Meeson, R.L. Management and Long-Term Outcome of Acetabular Fractures in Dogs: A Retrospective Study of 49 Dogs. Vet. Comp. Orthop. Traumatol. 2021, 34, 352–358. [Google Scholar] [CrossRef]
- Murugarren, M.; Piana, F.; Kalff, S.; Solano, M. Locking Compression Plate Fixation of Feline Acetabular Fractures: Application, Complications and Perioperative Outcome. Vet. Comp. Orthop. Traumatol. 2023, 36, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Amato, N.S.; Richards, A.; Knight, T.A.; Spector, D.; Boudrieau, R.J.; Belkoff, S. Ex vivo biomechanical comparison of the 2.4 mm uniLOCK reconstruction plate using 2.4 mm locking versus standard screws for fixation of acetabular osteotomy in dogs. Vet. Surg. 2008, 37, 741–748. [Google Scholar] [CrossRef]
- Hardie, R.J.; Bertram, J.E.; Todhunter, R.J.; Trotter, E.J. Biomechanical comparison of two plating techniques for fixation of acetabular osteotomies in dogs. Vet. Surg. 1999, 28, 148–153. [Google Scholar] [CrossRef]
- Rodriguez, N.A.R.; Bailey, S.J.; Langley-Hobbs, S.J. Treatment of Pelvic Fractures in Cats with Patellar Fracture and Dental Anomaly Syndrome. J. Feline Med. Surg. 2021, 23, 375–388. [Google Scholar] [CrossRef] [PubMed]
- Blakely, J.A.; Butler, J.R.; Priddy, L.B.; McCabe, E.M.; Avendaño, J.N.; Elder, S.H.; Wills, R. Ex vivo biomechanical comparison of 2.7 mm string-of-pearl plate versus screw/wire/Polymethylmethacrylate composite fixation and 2.7 mm veterinary acetabular plate for repair of simulated canine acetabular fractures. BMC Vet. Res. 2019, 15, 287. [Google Scholar] [CrossRef]
- Beaver, D.P.; Lewis, D.D.; Lanz, O.I.; Madison, J.B.; Kubilis, P.S. Evaluation of four interfragmentary Kirschner wire configurations as a component of screw/wire/polymethylmethacrylate fixation for acetabular fractures in dogs. J. Am. Anim. Hosp. Assoc. 2000, 36, 456–462. [Google Scholar] [CrossRef]
- Voss, K.; Langley-Hobbs, S.J.; Borer, L.; Montavon, P.M. Pelvis. In Feline Orthopedic Surgery and Musculoskeletal Diseases, 1st ed.; Elsevier Limited: Beijing, China, 2009; pp. 423–441. [Google Scholar]
- Scott, H.W.; McLaughling, R. Feline Orthopedics; Manson Publishing Ltd.: London, UK, 2007; 400p. [Google Scholar]
- Graville, T.C.; Gambino, J.M.; Syrcle, J.A. Physeal Acetabular Fracture in a Dog Treated with External Fixation. J. Am. Anim. Hosp. Assoc. 2018, 54, e54605. [Google Scholar] [CrossRef] [PubMed]
- Guillaume, J.M.; Pesenti, S.; Jouve, J.L.; Launay, F. Pelvic fractures in children (pelvic ring and acetabulum). Orthop. Traumatol. Surg. Res. 2020, 106, 125–133. [Google Scholar] [CrossRef]
- Amorosa, L.F.; Kloen, P.; Helfet, D.L. High-energy pediatric pelvic and acetabular fractures. Orthop. Clin. N. Am. 2014, 45, 483–500. [Google Scholar] [CrossRef]
- Johnson, A.L.; DeCamp, C.E. External skeletal fixation. Linear fixators. Vet. Clin. N. Am. Small Anim. Pract. 1999, 29, 1135–1152. [Google Scholar] [CrossRef]
- Palmer, R.H. External fixators and minimally invasive osteosynthesis in small animal veterinary medicine. Vet. Clin. N. Am. Small Anim. Pract. 2012, 42, 913–934. [Google Scholar] [CrossRef]
- Hudson, C.C.; Kim, S.E.; Pozzi, A. Percutaneous Pinning for Fracture Repair in Dogs and Cats. Vet. Clin. N. Am. Small Anim. Pract. 2020, 50, 101–121. [Google Scholar] [CrossRef] [PubMed]
- Flores, J.A.; Rovesti, G.L.; Rodriguez-Quiros, J. External Fixation for Fracture Stabilization of the Sacrum in 15 Dogs. Front. Vet. Sci. 2023, 10, 1222504. [Google Scholar] [CrossRef] [PubMed]
- Egger, E.L. Complications of external fixation. A problem-oriented approach. Vet. Clin. N. Am. Small Anim. Pract. 1991, 21, 705–733. [Google Scholar] [CrossRef]
- Howes, C.; Longley, M.; Reyes, N.; Major, A.C.; Gracis, M.; Fulton Scanlan, A.; Bailey, S.; Langley-Hobbs, S.J. Skull Pathology in 10 Cats with Patellar Fracture and Dental Anomaly Syndrome. J. Feline Med. Surg. 2019, 21, 793–800. [Google Scholar] [CrossRef]
- Flores, J.A.; Rovesti, G.L.; Gimenez-Ortiz, L.; Rodriguez-Quiros, J. Retrospective Assessment of Thirty-Two Cases of Pelvic Fractures Stabilized by External Fixation in Dogs and Classification Proposal. Vet. Sci. 2023, 10, 656. [Google Scholar] [CrossRef] [PubMed]
- Mears, D.C.; Fu, F. External Fixation in Pelvic Fractures. Orthop. Clin. N. Am. 1980, 11, 465–479. [Google Scholar] [CrossRef]
- Hu, S.B.; Xu, H.; Guo, H.B.; Sun, T.; Wang, C.J. External Fixation in Early Treatment of Unstable Pelvic Fractures. Chin. Med. J. 2012, 125, 1420–1424. [Google Scholar]
- Frydrýšek, K.; Jořenek, J.; UþeĖb, O.; Kubín, T.; Žilka, L.; Pleva, L. Design of External Fixators Used in Traumatology and Orthopaedics. Treatment of Fractures of Pelvis and its Acetabulum. Procedia Eng. 2012, 48, 164–173. [Google Scholar] [CrossRef][Green Version]
- Frydrýšek, K.; Pleva, L.; Jořenek, J.; Ječmínek, V.; Klučka, R.; Sivera, M. New External Fixators for Treatment of Pelvis and Acetabulum Fractures. Int. J. Biol. Biomed. Eng. 2013, 7, 36–46. [Google Scholar]
- Mcdonald, E.; Theologis, A.A.; Horst, P.; Kandemir, U.; Pekmezci, M. When do anterior external or internal fixators provide additional stability in an unstable (Tile C) pelvic fracture? A biomechanical study. Eur. J. Trauma Emerg. Surg. 2015, 41, 665–671. [Google Scholar] [CrossRef]
- Tiziani, S.; Osterhoff, G.; Ferguson, S.J.; Spreiter, G.; Scheyerer, M.J.; Spinas, G.L.; Wanner, G.A.; Simmen, H.P.; Werner, C.M.L. Biomechanical Comparison of Different External Fixation Configurations for Posttraumatic Pelvic Ring Instability. Adv. Orthop. Surg. 2014, 2014, 360165. [Google Scholar] [CrossRef]
- Vécsei, V.; Negrin, L.L.; Hajdu, S. Today’s Role of External Fixation in Unstable and Complex Pelvic Fractures. Eur. J. Trauma Emerg. Surg. 2010, 36, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Scaglione, M.; Parchi, P.; Digrandi, G.; Latessa, M.; Guido, G. External Fixation in Pelvic Fractures. Musculoskelet. Surg. 2010, 94, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Gardner, M.J.; Nork, S.N. Stabilization of Unstable Pelvic Fractures with Supraacetabular Compression External Fixation. J. Orthop. Trauma 2007, 21, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Harper, T.A.M. Femoral Head and Neck Excision. Vet. Clin. N. Am. Small Anim. Pract. 2017, 47, 885–897. [Google Scholar] [CrossRef] [PubMed]
- Tonks, C.A.; Tomlinson, J.L.; Cook, J.L. Evaluation of closed reduction and screw fixation in lag fashion of sacroiliac fracture-luxations. Vet. Surg. 2008, 37, 603–607. [Google Scholar] [CrossRef]
- Piermattei, D.L.; Johnson, K.A. An Atlas of Surgical Approaches to the Bones and Joints of the Dog and Cat, 4th ed.; Saunders: Philadelphia, PA, USA, 2004; pp. 306–308. [Google Scholar]
- Dudley, M.; Johnson, A.L.; Olmstead, M.; Smith, C.W.; Schaeffer, D.J.; Abbuehl, U. Open reduction and bone plate stabilization, compared with closed reduction and external fixation, for treatment of comminuted tibial fractures: 47 cases (1980–1995) in dogs. J. Am. Vet. Med. Assoc. 1997, 211, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Yeh, S.D.; Trout, N.J.; Keys, D.A. Description of and complications associated with reinforced, free-form external skeletal fixation for treatment of appendicular fractures in cats: 46 cases (2010–2019). J. Am. Vet. Med. Assoc. 2021, 259, 510–517. [Google Scholar] [CrossRef] [PubMed]
| PrO | PO | W1 | W2 | W3 | W4 | W5 | W6 | EXP | W16 | W24 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional Scale | 5 | 5 | 3 | 3 | 2 | 2 | 1 | 1 | 2 | 0 | 0 |
| Pain Scale | C | C | B | B | B | B | A | A | A | A | A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flores, J.A.; Rovesti, G.L.; Rodriguez-Quiros, J. A Bilateral Acetabular Physeal Fracture Treated with External Fixation in an Immature Cat. Animals 2024, 14, 379. https://doi.org/10.3390/ani14030379
Flores JA, Rovesti GL, Rodriguez-Quiros J. A Bilateral Acetabular Physeal Fracture Treated with External Fixation in an Immature Cat. Animals. 2024; 14(3):379. https://doi.org/10.3390/ani14030379
Chicago/Turabian StyleFlores, Jose Antonio, Gian Luca Rovesti, and Jesus Rodriguez-Quiros. 2024. "A Bilateral Acetabular Physeal Fracture Treated with External Fixation in an Immature Cat" Animals 14, no. 3: 379. https://doi.org/10.3390/ani14030379
APA StyleFlores, J. A., Rovesti, G. L., & Rodriguez-Quiros, J. (2024). A Bilateral Acetabular Physeal Fracture Treated with External Fixation in an Immature Cat. Animals, 14(3), 379. https://doi.org/10.3390/ani14030379






