Genomic Characterization of Staphylococcus aureus in Wildlife
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. Staphylococcus aureus Isolation and Characterization
2.3. Genome Sequencing and Assembly
2.4. Molecular Typing and Phylogenetic Analysis
2.5. Phenotypic Antimicrobial Susceptibility Testing
2.6. Statistical Analysis
3. Results
3.1. Animal Sampling and S. aureus Identification
3.2. Sampling Localization
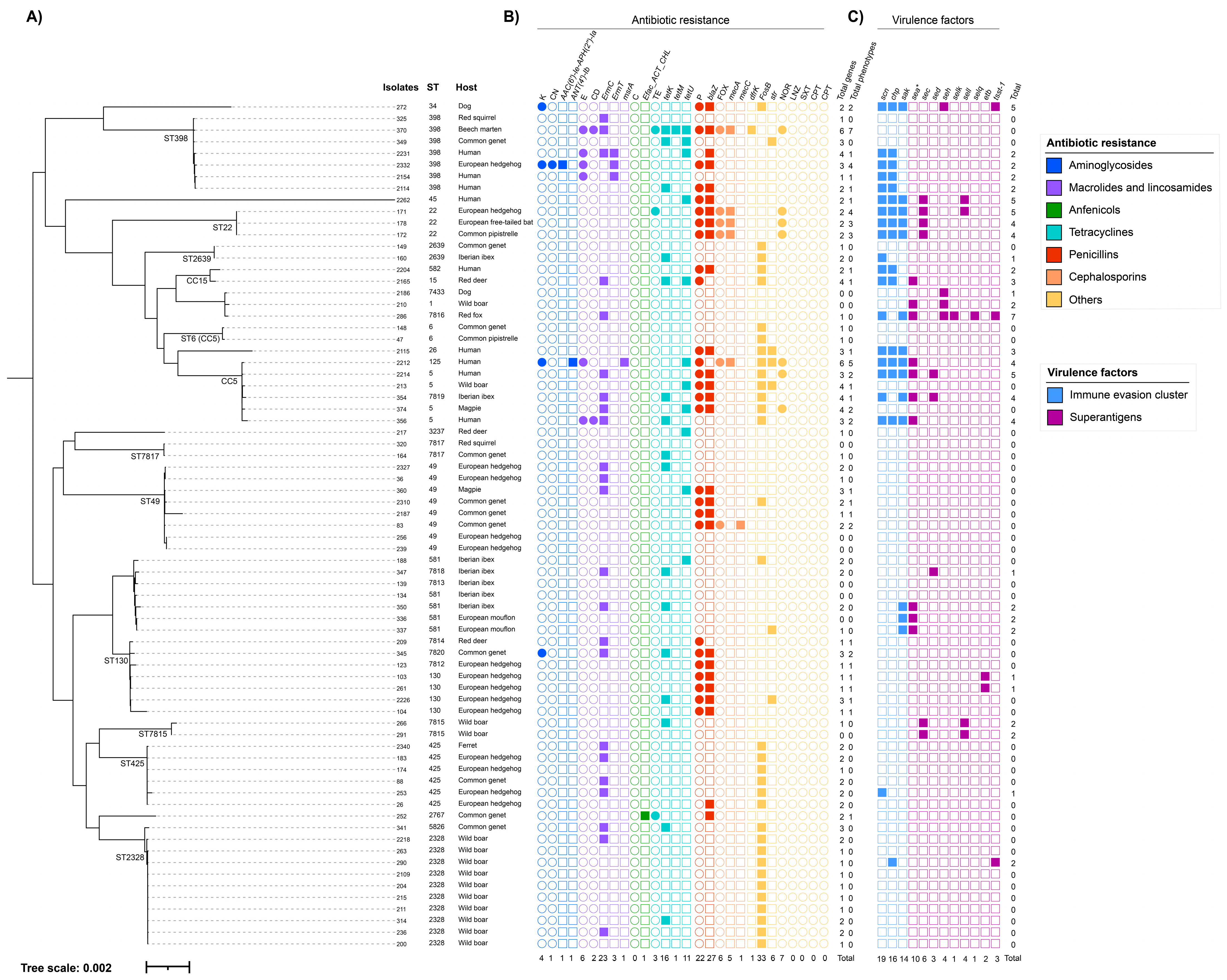
3.3. MLST Results
3.4. Antibiotic Resistance Analysis
3.5. Virulence Genes Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Haag, A.F.; Fitzgerald, J.R.; Penades, J.R. Staphylococcus aureus in Animals. Microbiol. Spectr. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Peton, V.; le Loir, Y. Staphylococcus aureus in Veterinary Medicine. Infect. Genet. Evol. 2014, 21, 602–615. [Google Scholar] [CrossRef]
- Mrochen, D.M.; Fernandes de Oliveira, L.M.; Raafat, D.; Holtfreter, S. Staphylococcus aureus Host Tropism and Its Implications for Murine Infection Models. Int. J. Mol. Sci 2020, 21, 7061. [Google Scholar] [CrossRef] [PubMed]
- Chambers, H.F.; DeLeo, F.R. Waves of Resistance: Staphylococcus aureus in the Antibiotic Era. Nat. Rev. Microbiol. 2009, 7, 629–641. [Google Scholar] [CrossRef]
- Dantes, R.; Mu, Y.; Belflower, R.; Aragon, D.; Dumyati, G.; Harrison, L.H.; Lessa, F.C.; Lynfield, R.; Nadle, J.; Petit, S.; et al. National Burden of Invasive Methicillin-Resistant Staphylococcus aureus Infections, United States, 2011. JAMA Intern. Med. 2013, 173, 1970–1979. [Google Scholar] [CrossRef]
- Turner, N.A.; Sharma-Kuinkel, B.K.; Maskarinec, S.A.; Eichenberger, E.M.; Shah, P.P.; Carugati, M.; Holland, T.L.; Fowler, V.G. Methicillin-Resistant Staphylococcus aureus: An Overview of Basic and Clinical Research. Nat. Rev. Microbiol. 2019, 17, 203–218. [Google Scholar] [CrossRef] [PubMed]
- Benito, D.; Gómez Villaescusa, P.; Aspiroz Sancho, C.; Zarazaga Chamorro, M.; Lozano Fernández, C.; Torres Manrique, C. Molecular Characterization of Staphylococcus aureus Isolated from Humans Related to a Livestock Farm in Spain, with Detection of MRSA-CC130 Carrying mecC Gene: A Zoonotic Case? Enferm. Infecc. Microbiol. Clín. 2016, 34, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Chuang, Y.Y.; Huang, Y.C. Livestock-Associated Meticillin-Resistant Staphylococcus aureus in Asia: An Emerging Issue? Int. J. Antimicrob. Agents 2015, 45, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Price, L.B.; Stegger, M.; Hasman, H.; Aziz, M.; Larsen, J.; Andersen, P.S.; Pearson, T.; Waters, A.E.; Foster, J.T.; Schupp, J.; et al. Staphylococcus aureus CC398: Host Adaptation and Emergence of Methicillin Resistance in Livestock. mBio 2012, 3, e00305-11. [Google Scholar] [CrossRef]
- Heaton, C.J.; Gerbig, G.R.; Sensius, L.D.; Patel, V.; Smith, T.C. Staphylococcus aureus Epidemiology in Wildlife: A Systematic Review. Antibiotics 2020, 9, 89. [Google Scholar] [CrossRef]
- Larsen, J.; Raisen, C.L.; Ba, X.; Sadgrove, N.J.; Kerschner, H.; Apfalter, P.; Hartl, R.; Deplano, A. Emergence of Methicillin Resistance Predates the Clinical Use of Antibiotics. Nature 2022, 602, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Porrero, M.C.; Mentaberre, G.; Sánchez, S.; Fernández-Llario, P.; Gómez-Barrero, S.; Navarro-Gonzalez, N.; Serrano, E.; Casas-Díaz, E.; Marco, I.; Fernández-Garayzabal, J.F.; et al. Methicillin Resistant Staphylococcus aureus (MRSA) Carriage in Different Free-Living Wild Animal Species in Spain. Vet. J. 2013, 198, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Ripa, L.; Alcalá, L.; Simón, C.; Gómez, P.; Mama, O.M.; Rezusta, A.; Zarazaga, M.; Torres, C. Diversity of Staphylococcus aureus Clones in Wild Mammals in Aragon, Spain, with Detection of MRSA ST130- mecC in Wild Rabbits. J. Appl. Microbiol. 2019, 127, 284–291. [Google Scholar] [CrossRef]
- Moreno-Grúa, E.; Pérez-Fuentes, S.; Viana, D.; Cardells, J.; Lizana, V.; Aguiló, J.; Selva, L.; Corpa, J.M. Marked Presence of Methicillin-Resistant Staphylococcus aureus in Wild Lagomorphs in Valencia, Spain. Animals 2020, 10, 1109. [Google Scholar] [CrossRef] [PubMed]
- Hookey, J.V.; Richardson, J.F.; Cookson, B.D. Molecular Typing of Staphylococcus aureus Based on PCR Restriction Fragment Length Polymorphism and DNA Sequence Analysis of the Coagulase Gene. J. Clin. Microbiol. 1998, 36, 1083–1089. [Google Scholar] [CrossRef]
- Frenay, H.M.E.; Theelen, J.P.G.; Schouls, L.M.; Vandenbroucke-Grauls, C.M.J.E.; Verhoef, J.; van Leeuwen, W.J.; Mooi, F.R. Discrimination of Epidemic and Nonepidemic Methicillin-Resistant Staphylococcus aureus Strains on the Basis of Protein A Gene Polymorphism. J. Clin. Microbiol. 1994, 32, 846–847. [Google Scholar] [CrossRef]
- Viana, D.; Selva, L.; Segura, P.; Penadés, J.R.; Corpa, J.M. Genotypic Characterization of Staphylococcus aureus Strains Isolated from Rabbit Lesions. Vet. Microbiol. 2007, 121, 288–298. [Google Scholar] [CrossRef]
- Chen, S.; Zhou, Y.; Chen, Y.; Gu, J. Fastp: An Ultra-Fast All-in-One FASTQ Preprocessor. Bioinformatics 2018, 34, i884–i890. [Google Scholar] [CrossRef]
- Andrews, S. FastQC A Quality Control Tool for High Throughput Sequence Data. Available online: https://github.com/s-andrews/FastQC (accessed on 24 July 2022).
- Gurevich, A.; Saveliev, V.; Vyahhi, N.; Tesler, G. QUAST: Quality Assessment Tool for Genome Assemblies. Bioinformatics 2013, 29, 1072–1075. [Google Scholar] [CrossRef]
- Blankenberg, D.; Coraor, N.; von Kuster, G.; Taylor, J.; Nekrutenko, A. Integrating Diverse Databases into an Unified Analysis Framework: A Galaxy Approach. Database (Oxf.) 2011, 2011, bar011. [Google Scholar] [CrossRef]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A New Genome Assembly Algorithm and Its Applications to Single-Cell Sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef] [PubMed]
- Torsten, S. MLST: Scan Contig Files against PubMLST Typing Schemes. 2016. Available online: https://github.com/tseemann/mlst (accessed on 2 August 2022).
- Jolley, K.A.; Bray, J.E.; Maiden, M.C.J. Open-Access Bacterial Population Genomics: BIGSdb Software, the PubMLST.Org Website and Their Applications. Wellcome Open Res. 2018, 3, 124. [Google Scholar] [CrossRef] [PubMed]
- Torsten, S. Prokka: Rapid Prokaryotic Genome Annotation. Bioinformatics 2014, 30, 2068–2069. [Google Scholar] [CrossRef]
- Page, A.J.; Cummins, C.A.; Hunt, M.; Wong, V.K.; Reuter, S.; Holden, M.T.G.; Fookes, M.; Falush, D.; Keane, J.A.; Parkhill, J. Roary: Rapid Large-Scale Prokaryote Pan Genome Analysis. Bioinformatics 2015, 31, 3691–3693. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, A. RaxML Version 8: A Tool for Phylogenetic Analysis and Post-Analysis of Large Phylogenies. Bioinformatics 2014, 30, 1312–1313. [Google Scholar] [CrossRef] [PubMed]
- Letunic, I.; Bork, P. Interactive Tree Of Life (ITOL) v5: An Online Tool for Phylogenetic Tree Display and Annotation. Nucleic Acids Res. 2021, 49, W293–W296. [Google Scholar] [CrossRef] [PubMed]
- Torsten, S. ABRicate: Mass Screening of Contigs for Antiobiotic Resistance Genes. 2016. Available online: https://github.com/tseemann/abricate (accessed on 12 August 2022).
- Bortolaia, V.; Kaas, R.S.; Ruppe, E.; Roberts, M.C.; Schwarz, S.; Cattoir, V.; Philippon, A.; Allesoe, R.L.; Rebelo, A.R.; Florensa, A.F.; et al. ResFinder 4.0 for Predictions of Phenotypes from Genotypes. J. Antimicrob. Chemother. 2020, 75, 3491–3500. [Google Scholar] [CrossRef] [PubMed]
- Jia, B.; Raphenya, A.R.; Alcock, B.; Waglechner, N.; Guo, P.; Tsang, K.K.; Lago, B.A.; Dave, B.M.; Pereira, S.; Sharma, A.N.; et al. CARD 2017: Expansion and Model-Centric Curation of the Comprehensive Antibiotic Resistance Database. Nucleic Acids Res. 2017, 45, D566–D573. [Google Scholar] [CrossRef]
- Liu, B.; Zheng, D.; Jin, Q.; Chen, L.; Yang, J. VFDB 2019: A Comparative Pathogenomic Platform with an Interactive Web Interface. Nucleic Acids Res. 2019, 47, D687–D692. [Google Scholar] [CrossRef]
- Chaguza, C.; Smith, J.T.; Bruce, S.A.; Gibson, R.; Martin, I.W.; Andam, C.P. Prophage-Encoded Immune Evasion Factors Are Critical for Staphylococcus aureus Host Infection, Switching, and Adaptation. Cell Genom. 2022, 2, 100194. [Google Scholar] [CrossRef]
- Tam, K.; Torres, V.J. Staphylococcus aureus Secreted Toxins and Extracellular Enzymes. Microbiol. Spectr. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Kaya, H.; Hasman, H.; Larsen, J.; Stegger, M.; Johannesen, T.B.; Allesøe, R.L.; Lemvigh, C.K.; Aarestrup, F.M.; Lund, O.; Larsen, A.R. SCC Mec Finder, a Web-Based Tool for Typing of Staphylococcal Cassette Chromosome Mec in Staphylococcus aureus Using Whole-Genome Sequence Data. mSphere 2018, 3, e00612-17. [Google Scholar] [CrossRef]
- Leclercq, R.; Cantón, R.; Brown, D.F.J.; Giske, C.G.; Heisig, P.; Macgowan, A.P.; Mouton, J.W.; Nordmann, P.; Rodloff, A.C.; Rossolini, G.M.; et al. EUCAST Expert Rules in Antimicrobial Susceptibility Testing. Clin. Microbiol. Infect. 2013, 19, 141–160. [Google Scholar] [CrossRef] [PubMed]
- Abdullahi, I.N.; Fernández-Fernández, R.; Juárez-Fernández, G.; Martínez-Álvarez, S.; Eguizábal, P.; Zarazaga, M.; Lozano, C.; Torres, C. Wild Animals Are Reservoirs and Sentinels of Staphylococcus aureus and MRSA Clones: A Problem with “One Health” Concern. Antibiotics 2021, 10, 1556. [Google Scholar] [CrossRef] [PubMed]
- Stallknecht, D.E. Impediments to Wildlife Disease Surveillance, Research, and Diagnostics. Curr. Top. Microbiol. Immunol. 2007, 315, 445–461. [Google Scholar] [CrossRef]
- Porrero, M.C.; Mentaberre, G.; Sánchez, S.; Fernández-Llario, P.; Casas-Díaz, E.; Mateos, A.; Vidal, D.; Lavín, S.; Fernández-Garayzábal, J.F.; Domínguez, L. Carriage of Staphylococcus aureus by Free-Living Wild Animals in Spain. Appl. Environ. Microbiol. 2014, 80, 4865–4870. [Google Scholar] [CrossRef] [PubMed]
- Gómez, P.; González-Barrio, D.; Benito, D.; Garciá, J.T.; Viñuela, J.; Zarazaga, M.; Ruiz-Fons, F.; Torres, C. Detection of Methicillin-Resistant Staphylococcus aureus (MRSA) Carrying the mecC Gene in Wild Small Mammals in Spain. J. Antimicrob. Chemother. 2014, 69, 2061–2064. [Google Scholar] [CrossRef]
- Monecke, S.; Gavier-Widén, D.; Hotzel, H.; Peters, M.; Guenther, S.; Lazaris, A.; Loncaric, I.; Müller, E.; Reissig, A.; Ruppelt-Lorz, A.; et al. Diversity of Staphylococcus aureus Isolates in European Wildlife. PLoS ONE 2016, 11, e0168433. [Google Scholar] [CrossRef]
- Mrochen, D.M.; Schulz, D.; Fischer, S.; Jeske, K.; el Gohary, H.; Reil, D.; Imholt, C.; Trübe, P.; Suchomel, J.; Tricaud, E.; et al. Wild Rodents and Shrews Are Natural Hosts of Staphylococcus aureus. Int. J. Med. Microbiol. 2018, 308, 590–597. [Google Scholar] [CrossRef]
- Paterson, G.K.; Larsen, A.R.; Robb, A.; Edwards, G.E.; Pennycott, T.W.; Foster, G.; Mot, D.; Hermans, K.; Baert, K.; Peacock, S.J.; et al. The Newly Described mecA Homologue, mecALGA251, Is Present in Methicillin-Resistant Staphylococcus aureus Isolates from a Diverse Range of Host Species. J. Antimicrob. Chemother. 2012, 67, 2809–2813. [Google Scholar] [CrossRef]
- Haenni, M.; Châtre, P.; Dupieux, C.; Métayer, V.; Maillard, K.; Bes, M.; Madec, J.Y.; Laurent, F. mecC -Positive MRSA in Horses. J. Antimicrob. Chemother. 2015, 70, 3401–3402. [Google Scholar] [CrossRef] [PubMed]
- Deplano, A.; Vandendriessche, S.; Nonhoff, C.; Denis, O. Genetic Diversity among Methicillin-Resistant Staphylococcus aureus Isolates Carrying the mecC Gene in Belgium. J. Antimicrob. Chemother. 2014, 69, 1457–1460. [Google Scholar] [CrossRef] [PubMed]
- PubMLST: Public Databases for Molecular Typing and Microbial Genome Diversity. Available online: https://pub-686mlst.org/bigsdb?db=pubmlst_saureus_isolates&page=query&genomes=1 (accessed on 10 November 2022).
- Zarazaga, M.; Gómez, P.; Ceballos, S.; Torres, C. Molecular Epidemiology of Staphylococcus aureus Lineages in the Animal–Human Interface. In Staphylococcus aureus; Fetsch, A., Ed.; Elsevier: Cambridge, MA, USA, 2018; pp. 189–214. ISBN 978-0-12-809671-0. [Google Scholar]
- Yebra, G.; Harling-Lee, J.D.; Lycett, S.; Aarestrup, F.M.; Larsen, G.; Cavaco, L.M.; Seo, K.S.; Abraham, S.; Norris, J.M.; Schmidt, T.; et al. Multiclonal Human Origin and Global Expansion of an Endemic Bacterial Pathogen of Livestock. Proc. Natl. Acad. Sci. USA 2022, 119, e2211217119. [Google Scholar] [CrossRef] [PubMed]
- Loncaric, I.; Kübber-Heiss, A.; Posautz, A.; Stalder, G.L.; Hoffmann, D.; Rosengarten, R.; Walzer, C. mecC- and mecA-Positive Meticillin-Resistant Staphylococcus aureus (MRSA) Isolated from Livestock Sharing Habitat with Wildlife Previously Tested Positive for mecC-Positive MRSA. Vet. Derm. 2014, 25, 147–148. [Google Scholar] [CrossRef]
- Mama, O.M.; Aspiroz, C.; Ruiz-Ripa, L.; Ceballos, S.; Iñiguez-Barrio, M.; Cercenado, E.; Azcona, J.M.; López-Cerero, L.; Seral, C.; López-Calleja, A.I.; et al. Prevalence and Genetic Characteristics of Staphylococcus aureus CC398 Isolates From Invasive Infections in Spanish Hospitals, Focusing on the Livestock-Independent CC398-MSSA Clade. Front. Microbiol. 2021, 12, 623108. [Google Scholar] [CrossRef]
- Gómez, P.; Lozano, C.; Camacho, M.C.; Lima-Barbero, J.F.; Hernández, J.M.; Zarazaga, M.; Höfle, Ú.; Torres, C. Detection of MRSA ST3061-T843-mecC and ST398-T011-mecA in White Stork Nestlings Exposed to Human Residues. J. Antimicrob. Chemother. 2016, 71, 53–57. [Google Scholar] [CrossRef]
- Monecke, S.; Coombs, G.; Shore, A.C.; Coleman, D.C.; Akpaka, P.; Borg, M.; Chow, H.; Ip, M.; Jatzwauk, L.; Jonas, D.; et al. A Field Guide to Pandemic, Epidemic and Sporadic Clones of Methicillin-Resistant Staphylococcus aureus. PLoS ONE 2016, 6, e17936. [Google Scholar] [CrossRef]
- Aires-de-Sousa, M. Methicillin-Resistant Staphylococcus aureus among Animals: Current Overview. Clin. Microbiol. Infect. 2017, 23, 373–380. [Google Scholar] [CrossRef]
- Hau, S.J.; Sun, J.; Davies, P.R.; Frana, T.S.; Nicholson, T.L. Comparative Prevalence of Immune Evasion Complex Genes Associated with β-Hemolysin Converting Bacteriophages in MRSA ST5 Isolates from Swine, Swine Facilities, Humans with Swine Contact, and Humans with No Swine Contact. PLoS ONE 2015, 10, e0142832. [Google Scholar] [CrossRef]
- Lowder, B.V.; Guinane, C.M.; Zakour, N.L.B.; Weinert, L.A.; Conway-Morris, A.; Cartwright, R.A.; Simpson, A.J.; Rambaut, A.; Nübel, U.; Fitzgerald, J.R. Recent Human-to-Poultry Host Jump, Adaptation, and Pandemic Spread of Staphylococcus aureus. Proc. Natl. Acad. Sci. USA 2009, 106, 19545–19550. [Google Scholar] [CrossRef]
- Schaumburg, F.; Pauly, M.; Anoh, E.; Mossoun, A.; Wiersma, L.; Schubert, G.; Flammen, A.; Alabi, A.S.; Muyembe-Tamfum, J.J.; Grobusch, M.P.; et al. Staphylococcus aureus Complex from Animals and Humans in Three Remote African Regions. Clin. Microbiol. Infect. 2015, 21, 345.e1–345.e8. [Google Scholar] [CrossRef] [PubMed]
- Silva, V.; Caniça, M.; Capelo, J.L.; Igrejas, G.; Poeta, P. Diversity and Genetic Lineages of Environmental Staphylococci: A Surface Water Overview. FEMS Microbiol. Ecol. 2020, 96, fiaa191. [Google Scholar] [CrossRef] [PubMed]
- Boopathy, R. Presence of Methicillin Resistant Staphylococcus aureus (MRSA) in Sewage Treatment Plant. Bioresour. Technol. 2017, 240, 144–148. [Google Scholar] [CrossRef]
- Gómez, P.; Lozano, C.; Benito, D.; Estepa, V.; Tenorio, C.; Zarazaga, M.; Torres, C. Characterization of Staphylococci in Urban Wastewater Treatment Plants in Spain, with Detection of Methicillin Resistant Staphylococcus aureus ST398. Environ. Pollut. 2016, 212, 71–76. [Google Scholar] [CrossRef]
- Porrero, M.C.; Harrison, E.M.; Fernández-Garayzábal, J.F.; Paterson, G.K.; Díez-Guerrier, A.; Holmes, M.A.; Domínguez, L. Detection of mecC-Methicillin-Resistant Staphylococcus aureus Isolates in River Water: A Potential Role for Water in the Environmental Dissemination. Environ. Microbiol. Rep. 2014, 6, 705–708. [Google Scholar] [CrossRef]
- Torres, C.; Esteve, C.; Nieto, M.P.; Burgui, J.M. Institutional technical report: Estadísticas cinegéticas de la Comunitat Valenciana. Memoria 2021. Temporada 2020/2021 [Hunting statistics of the Valencian Community. Annual Report 2021. 20120/2021 Season]. Hunting and Fishing Service; Valencia Region Government: Valencia, Spain, 2021. Available online: https://agroambient.gva.es/documents/20551003/367855780/Informe+Estado+Conservaci%C3%B3n+Especies+Cineg%C3%A9ticas+CV_junio2022.pdf/74730a51-2386-4fff-9a50-0c9aa45c03cc?t=1670239629983 (accessed on 24 July 2022).
- Carrasco-Garcia, R.; Barasona, J.A.; Gortazar, C.; Montoro, V.; Sanchez-Vizcaino, J.M.; Vicente, J. Wildlife and Livestock Use of Extensive Farm Resources in South Central Spain: Implications for Disease Transmission. Eur. J. Wildl. Res. 2016, 62, 65–78. [Google Scholar] [CrossRef]
- Ramos, B.; Rosalino, L.M.; Palmeira, J.D.; Torres, R.T.; Cunha, M.V. Antimicrobial Resistance in Commensal Staphylococcus aureus from Wild Ungulates Is Driven by Agricultural Land Cover and Livestock Farming. Environ. Pollut. 2022, 303, 119116. [Google Scholar] [CrossRef]
- Abdullahi, I.N.; Zarazaga, M.; Campaña-Burguet, A.; Eguizábal, P.; Lozano, C.; Torres, C. Nasal Staphylococcus aureus and S. pseudintermedius Carriage in Healthy Dogs and Cats: A Systematic Review of Their Antibiotic Resistance, Virulence and Genetic Lineages of Zoonotic Relevance. J. Appl. Microbiol. 2022, 133, 3368–3390. [Google Scholar] [CrossRef]
- Bruce, S.A.; Smith, J.T.; Mydosh, J.L.; Ball, J.; Needle, D.B.; Gibson, R.; Andam, C.P. Shared Antibiotic Resistance and Virulence Genes in Staphylococcus aureus from Diverse Animal Hosts. Sci. Rep. 2022, 12, 1–11. [Google Scholar] [CrossRef]
- Moon, B.Y.; Park, J.Y.; Robinson, D.A.; Thomas, J.C.; Ho Park, Y.; Thornton, J.A.; Seo, K.S. Mobilization of Genomic Islands of Staphylococcus aureus by Temperate Bacteriophage. PLoS ONE 2016, 11, e0151409. [Google Scholar] [CrossRef]
- Roberts, G.A.; Houston, P.J.; White, J.H.; Chen, K.; Stephanou, A.S.; Cooper, L.P.; Dryden, D.T.F.; Lindsay, J.A. Impact of Target Site Distribution for Type I Restriction Enzymes on the Evolution of Methicillin-Resistant Staphylococcus aureus (MRSA) Populations. Nucleic Acids Res. 2013, 41, 7472–7484. [Google Scholar] [CrossRef]
- Merda, D.; Felten, A.; Vingadassalon, N.; Denayer, S.; Titouche, Y.; Decastelli, L.; Hickey, B.; Kourtis, C.; Daskalov, H.; Mistou, M.Y.; et al. NAuRA: Genomic Tool to Identify Staphylococcal Enterotoxins in Staphylococcus aureus Strains Responsible for FoodBorne Outbreaks. Front. Microbiol. 2020, 11, 1483. [Google Scholar] [CrossRef] [PubMed]
- Tuffs, S.W.; Herfst, C.A.; Baroja, M.L.; Podskalniy, V.A.; DeJong, E.N.; Coleman, C.E.M.; McCormick, J.K. Regulation of Toxic Shock Syndrome Toxin-1 by the Accessory Gene Regulator in Staphylococcus aureus Is Mediated by the Repressor of Toxins. Mol. Microbiol. 2019, 112, 1163–1177. [Google Scholar] [CrossRef] [PubMed]
- Harrison, E.M.; Paterson, G.K.; Holden, M.T.G.; Larsen, J.; Stegger, M.; Larsen, A.R.; Petersen, A.; Skov, R.L.; Christensen, J.M.; Bak Zeuthen, A.; et al. Whole Genome Sequencing Identifies Zoonotic Transmission of MRSA Isolates with the Novel mecA Homologue mecC. EMBO Mol. Med. 2013, 5, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Shi, C.; Song, M.; Xu, X.; Yang, P.; Paoli, G.; Shi, X. Phenotypic and Genotypic Antimicrobial Resistance Traits of Foodborne Staphylococcus aureus Isolates from Shanghai. J. Food Sci. 2014, 79, M635–M642. [Google Scholar] [CrossRef] [PubMed]
- Nurjadi, D.; Zizmann, E.; Chanthalangsy, Q.; Heeg, K.; Boutin, S. Integrative Analysis of Whole Genome Sequencing and Phenotypic Resistance Toward Prediction of Trimethoprim-Sulfamethoxazole Resistance in Staphylococcus aureus. Front. Microbiol. 2021, 11, 607842. [Google Scholar] [CrossRef]
- Macesic, N.; Polubriaginof, F.; Tatonetti, N.P. Machine Learning: Novel Bioinformatics Approaches for Combating Antimicrobial Resistance. Curr. Opin. Infect. Dis. 2017, 30, 511–517. [Google Scholar] [CrossRef]
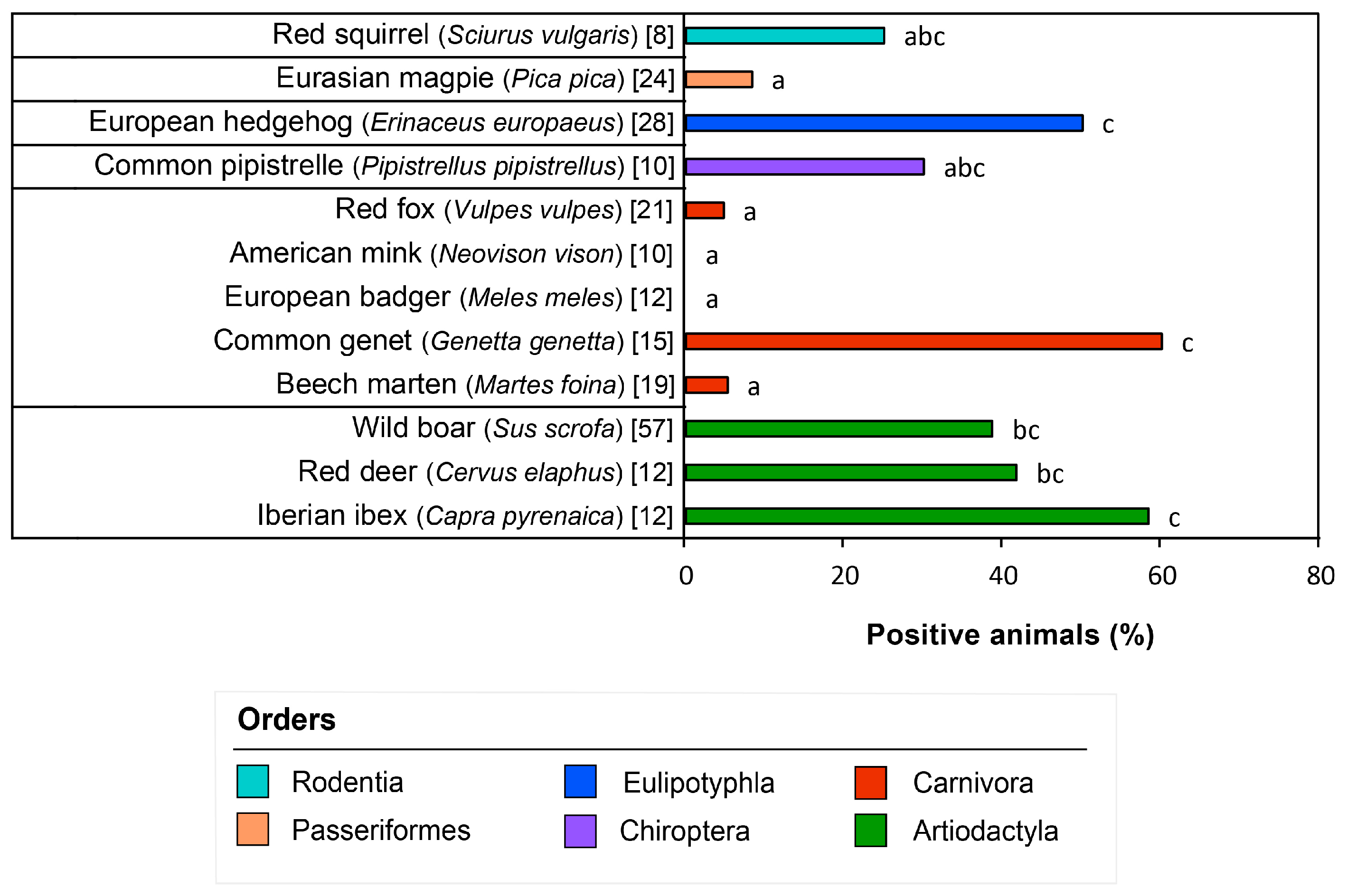
| Order/Species. | Animals (Total) | Nº and % of Positive Animals to S. aureus | Auricular Isolates | Nasal Isolates | Genital Isolates | Total Isolates |
|---|---|---|---|---|---|---|
| Artiodactyla | 83 | 35 (42.2%) | ||||
| Eurasian wild boar (Sus scrofa) | 57 | 22 (38.6%) | 0 | 20 | 4 | 24 |
| European mouflon (Ovis orientalis musimon) | 2 | 1 (50%) | 0 | 1 | 1 | 2 |
| Iberian ibex (Capra pyrenaica) | 12 | 7 (58.3%) | 2 | 4 | 3 | 9 |
| Red deer (Cervus elaphus) | 12 | 5 (41.7%) | 0 | 4 | 1 | 5 |
| Carnivora | 82 | 11 (13.4%) | ||||
| American mink (Neovison vison) | 10 | 0 (0%) | - | - | - | - |
| Beech marten (Martes foina) | 19 | 1 (5.3%) | 0 | 1 | 0 | 1 |
| Common genet (Genetta genetta) | 15 | 9 (60%) | 6 | 3 | 3 | 12 |
| Eurasian otter (Lutra lutra) | 3 | 0 (0%) | - | - | - | - |
| European badger (Meles meles) | 12 | 0 (0%) | - | - | - | - |
| European polecat (Mustela putorius) | 1 | 0 (0%) | - | - | - | - |
| European wildcat (Felis silvestris) | 1 | 0 (0%) | - | - | - | - |
| Red fox (Vulpes vulpes) | 21 | 1 (4.8%) | 0 | 1 | 0 | 1 |
| Chiroptera | 15 | 4 (26.7%) | ||||
| Common pipistrelle (Pipistrellus pipistrellus) | 10 | 3 (30%) | 0 | 0 | 3 | 3 |
| European free-tailed bat (Tadarida teniotis) | 3 | 1 (33.3%) | 0 | 0 | 1 | 1 |
| Soprano pipistrelle (Pipistrellus pygmaeus) | 2 | 0 (0%) | - | - | - | - |
| Eulipotyphla | 30 | 14 (46.7%) | ||||
| European hedgehog (Erinaceus europaeus) | 28 | 14 (50%) | 8 | 8 | 7 | 23 |
| Greater white-toothed shrew (Crocidura russula) | 1 | 0 (0%) | - | - | - | - |
| North African hedgehog (Atelerix algirus) | 1 | 0 (0%) | - | - | - | - |
| Passeriformes | 24 | 2 (8.3%) | ||||
| Eurasian magpie (Pica pica) | 24 | 2 (8.3%) | - | 1 * | 1 * | 2 |
| Rodentia | 8 | 2 (25%) | ||||
| Red squirrel (Sciurus vulgaris) | 8 | 2 (25%) | 1 | 2 | 1 | 4 |
| Total | 242 | 68 (28.1%) | 17 | 45 | 25 | 87 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Seijas, C.; Mascarós, P.; Lizana, V.; Martí-Marco, A.; Arnau-Bonachera, A.; Chillida-Martínez, E.; Cardells, J.; Selva, L.; Viana, D.; Corpa, J.M. Genomic Characterization of Staphylococcus aureus in Wildlife. Animals 2023, 13, 1064. https://doi.org/10.3390/ani13061064
Martínez-Seijas C, Mascarós P, Lizana V, Martí-Marco A, Arnau-Bonachera A, Chillida-Martínez E, Cardells J, Selva L, Viana D, Corpa JM. Genomic Characterization of Staphylococcus aureus in Wildlife. Animals. 2023; 13(6):1064. https://doi.org/10.3390/ani13061064
Chicago/Turabian StyleMartínez-Seijas, Carmen, Patricia Mascarós, Víctor Lizana, Alba Martí-Marco, Alberto Arnau-Bonachera, Eva Chillida-Martínez, Jesús Cardells, Laura Selva, David Viana, and Juan M. Corpa. 2023. "Genomic Characterization of Staphylococcus aureus in Wildlife" Animals 13, no. 6: 1064. https://doi.org/10.3390/ani13061064
APA StyleMartínez-Seijas, C., Mascarós, P., Lizana, V., Martí-Marco, A., Arnau-Bonachera, A., Chillida-Martínez, E., Cardells, J., Selva, L., Viana, D., & Corpa, J. M. (2023). Genomic Characterization of Staphylococcus aureus in Wildlife. Animals, 13(6), 1064. https://doi.org/10.3390/ani13061064







