A Systematic Literature Review of Complementary and Alternative Veterinary Medicine: Laser Therapy
Abstract
:Simple Summary
Abstract
1. Introduction
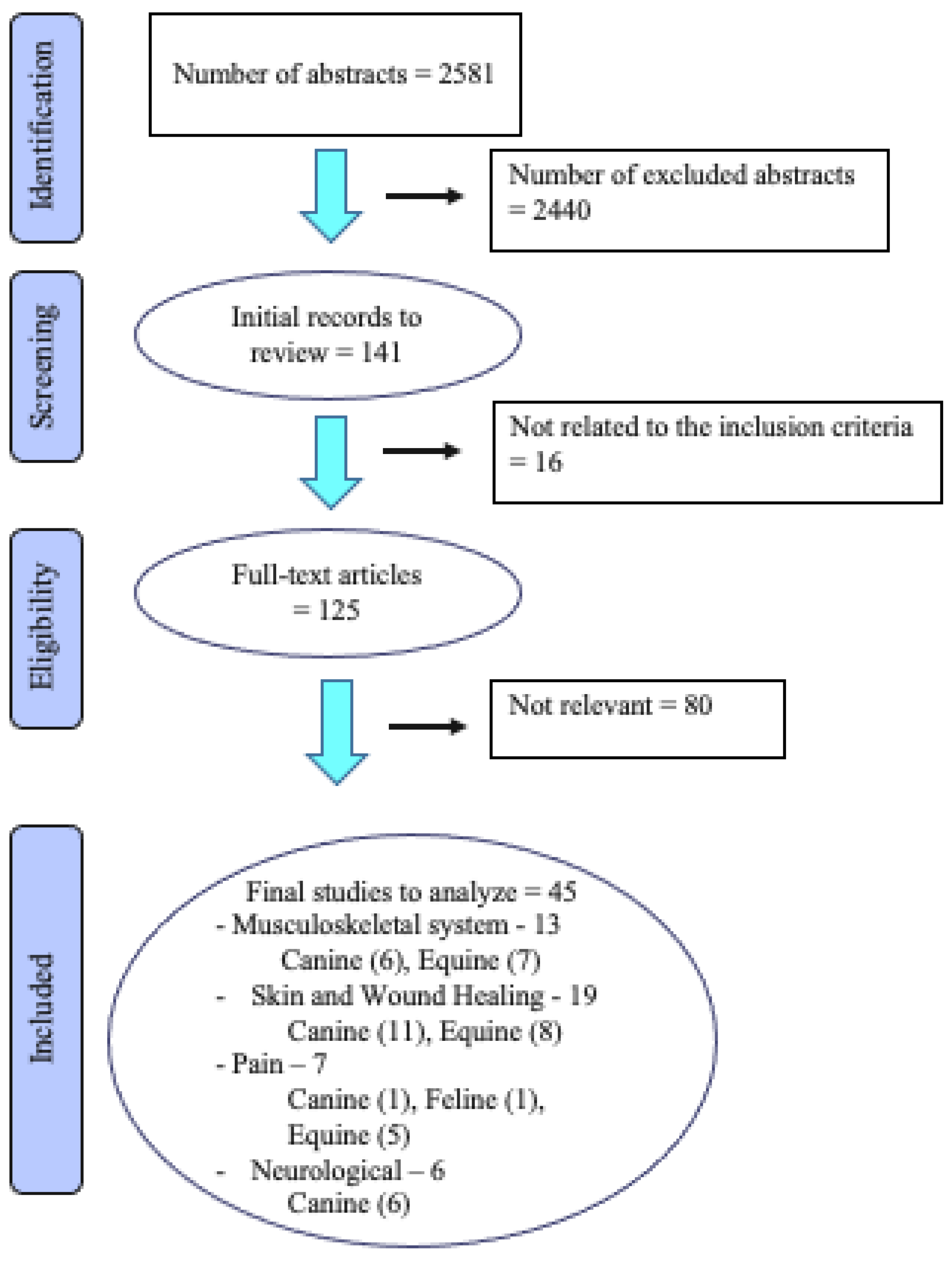
2. Materials and Methods
2.1. Review Topic/Research Question
2.2. Search Strategy
2.3. General Inclusion and Exclusion Criteria
2.4. Study Selection and Categorisation
3. Results
3.1. Study Quality
3.2. General Clinical Indications
3.3. Musculoskeletal Conditions
Intervention, Control and Clinical Effects
3.4. Skin and Wound Healing
Intervention, Control and Clinical Effects
3.5. Pain
Intervention, Control and Clinical Effects
3.6. Neurological Conditions
Intervention, Control and Clinical Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liebert, A.; Kiat, H. The history of light therapy in hospital physiotherapy and medicine with emphasis on Australia: Evolution into novel areas of practice. Physiother. Theory Pract. 2021, 37, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Pryor, B.; Millis, D.L. Therapeutic Laser in Veterinary Medicine. Vet. Clin. N. Am. Small Anim. Pract. 2015, 45, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Avci, P.; Gupta, A.; Sadasivam, M.; Vecchio, D.; Pam, Z.; Pam, N.; Hamblin, M.R. Low-level laser (light) therapy (LLLT) in skin: Stimulating, healing, restoring. Semin. Cutan. Med. Surg. 2013, 32, 41–52. [Google Scholar] [PubMed]
- Higgins, J.; Thomas, J. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.2; John Wiley & Sons: Hoboken, NJ, USA, 2021; Available online: https://training.cochrane.org/handbook/current2021 (accessed on 8 April 2022).
- Statens Beredning för Medicinsk och Social Utvärdering [SBU]. SBU:s Metodbok 2022. Available online: https://www.sbu.se/sv/metod/sbus-metodbok/?pub=48286 (accessed on 8 April 2022).
- Looney, A.L.; Huntingford, J.L.; Blaeser, L.L.; Mann, S. A randomized blind placebo-controlled trial investigating the effects of photobiomodulation therapy (PBMT) on canine elbow osteoarthritis. Can. Vet. J. 2018, 59, 959–966. [Google Scholar] [PubMed]
- Rogatko, C.P.; Baltzer, W.I.; Tennant, R. Preoperative low level laser therapy in dogs undergoing tibial plateau levelling osteotomy: A blinded, prospective, randomized clinical trial. Vet. Comp. Orthop. Traumatol. 2017, 30, 46–53. [Google Scholar] [CrossRef]
- Renwick, A.I.; Brodbelt, D.C.; Ferguson, J.; Abreu, H. Influence of class IV laser therapy on the outcomes of tibial plateau leveling osteotomy in dogs. Vet. Surg. 2018, 47, 507–515. [Google Scholar] [CrossRef]
- Kennedy, K.C.; Martinez, S.A.; Martinez, S.E.; Tucker, R.L.; Davies, N.M. Effects of low-level laser therapy on bone healing and signs of pain in dogs following tibial plateau leveling osteotomy. Am. J. Vet. Res. 2018, 79, 893–904. [Google Scholar] [CrossRef]
- Santiago, V.; Piram, A.; Fuziy, A. Effect of soft laser in bone repair after expansion of the midpalatal suture in dogs. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 615–624. [Google Scholar] [CrossRef]
- Wozniak, P.; Brzeski, W.; Chyczewski, M.; Jalynski, M. The influence of limited strength laser radiation on the effective treatment of dogs with osteomyelitis. Med. Weter. 1997, 53, 665–668. [Google Scholar]
- Lindholm, A.C.; Swensson, U.; de Mitri, N.; Collinder, E. Clinical effects of betamethasone and hyaluronan, and of defocalized carbon dioxide laser treatment on traumatic arthritis in the fetlock joints of horses. J. Vet. Med. A Physiol. Pathol. Clin. Med. 2002, 49, 189–194. [Google Scholar] [CrossRef]
- Bergh, A.; Nyman, G.; Roepstorff, L.; Zhou, Q.; Hallberg, M.; Drevemo, S.; Roethlisberger-Holm, K. Defocused CO2 laser therapy in traumatic arthritis of the metacarpophalangeal joint: A randomized clinical study. Equine Comp. Exerc. Phys. 2006, 4, 169–177. [Google Scholar] [CrossRef]
- Zielinska, P.; Nicpon, J.; Kielbowicz, Z.; Soroko, M.; Dudek, K.; Zaborski, D. Effects of high intensity laser therapy in the treatment of tendon and ligament injuries in performance horses. Animals 2020, 8, 1327. [Google Scholar] [CrossRef]
- Marr, C.M.; Love, S.; Boyd, J.S.; McKellar, Q. Factors affecting the clinical outcome of injuries to the superficial digital flexor tendon in National Hunt and point-to-point racehorses. Vet. Rec. 1993, 132, 476–479. [Google Scholar] [CrossRef]
- Bergh, A.; Nyman, G.; Lundeberg, T.; Drevemo, S. Effect of defocused CO2 laser on equine tissue perfusion. Acta Vet. Scand. 2006, 47, 33–42. [Google Scholar] [CrossRef]
- Godlewska, M.; Soroko, M.; Zielinska, P.; Dudek, K. The use of thermography for assessment of high-intensity laser therapy in racehorses: Pilot study. Med. Weter.-Vet. Med.-Sci. Pract. 2020, 10, 593–596. [Google Scholar] [CrossRef]
- Monici, M.; Gnerucci, A.; Falconi, T.; Bani, D.; Cialdai, F.; Fusi, F.; Romano, G. Laser therapy penetration depth: A near-infrared study on a horse tendon model. Muscles Ligaments Tendons J. 2018, 8, 222–228. [Google Scholar] [CrossRef]
- Gammel, J.E.; Biskup, J.J.; Drum, M.G.; Newkirk Kim Lux, C.N. Effects of low-level laser therapy on the healing of surgically closed incisions and surgically created open wounds in dogs. Vet. Surg. 2018, 47, 499–506. [Google Scholar] [CrossRef]
- Kurach, L.M.; Stanley, B.J.; Gazzola, K.M.; Fritz, M.C.; Steficek, B.A.; Hauptman, J.G.; Seymour, K.J. The Effect of Low-Level Laser Therapy on the Healing of Open Wounds in Dogs. Vet. Surg. 2015, 44, 988–996. [Google Scholar] [CrossRef]
- Debraekt, M.M.H.I.; Vanalphen, F.A.M.; Kuijpersjagtman, A.M.; Maltha, J.C. Effect of low-level laser therapy on wound-healing after palatal surgery in beagle dogs. Lasers Surg. Med. 1991, 11, 462–470. [Google Scholar] [CrossRef]
- Wardlaw, J.L.; Gazzola, K.M.; Wagoner, A.; Brinkman, E.; Burt, J.; Butler, R.; Gunter, J.M.; Senter, L.H. Laser Therapy for Incision Healing in 9 Dogs. Front. Vet. Sci. 2019, 5, 349. [Google Scholar] [CrossRef]
- Bharti, B.; Pandey, S.S.; Garg, U.K.; Shukla, B.P. Low level laser therapy for the healing of contaminated wounds in dogs: Histopathological changes. Indian J. Vet. Surg. 2013, 34, 57–58. [Google Scholar]
- Marchegiani, A.; Spaterna, A.; Cerquetella, M.; Tambella, A.M.; Fruganti, A.; Paterson, A. Fluorescence biomodulation in the management of canine interdigital pyoderma cases: A prospective, single-blinded, randomized and controlled clinical study. Vet. Dermatol. 2019, 30, 371. [Google Scholar] [CrossRef] [PubMed]
- Stich, A.N.; Rosenkrantz, W.S.; Griffin, C.E. Clinical efficacy of low-level laser therapy on localized canine atopic dermatitis severity score and localized pruritic visual analog score in pedal pruritus due to canine atopic dermatitis. Vet. Dermatol. 2014, 25, 464. [Google Scholar] [CrossRef] [PubMed]
- Kampa, N.; Jitpean, S.; Seesupa, S.; Hoisang, S. Penetration depth study of 830 nm low-intensity laser therapy on living dog tissue. Vet. World 2020, 7, 1417–1422. [Google Scholar] [CrossRef]
- Hochman-Elam, L.N.; Heidel, R.E.; Shmalberg, J.W. Effects of laser power, wavelength, coat length, and coat color on tissue penetration using photobiomodulation in healthy dogs. Can. J. Vet. Res. 2020, 84, 131–137. [Google Scholar]
- Keerti, N.; Bhargava, M.K.; Madhu, S.; Dharmendra, K.; Bhowmick, D. Low level laser therapy for healing of aural haematoma in dogs. Intas Polivet 2016, 2, 262–269. [Google Scholar]
- Olivieri, L.; Cavina, D.; Radicchi, G.; Miragliotta, V.; Abramo, F. Efficacy of low-level laser therapy on hair regrowth in dogs with noninflammatory alopecia: A pilot study. Vet. Dermatol. 2015, 26, 35–39.e11. [Google Scholar] [CrossRef]
- Kaneps, A.J.; Hultgren, B.D.; Riebold, T.W.; Shires, G.M. Laser therapy in the horse: Histopathologic response. Am. J. Vet. Res. 1984, 45, 581–582. [Google Scholar]
- Petersen, S.L.; Botes, C.; Olivier, A.; Guthrie, A.J. The effect of low level laser therapy (LLLT) on wound healing in horses. Equine Vet. J. 1999, 31, 228–231. [Google Scholar] [CrossRef]
- Gomez-Villamandos, R.J.; Santisteban Valenzuela, J.M.; Ruiz Calatrava, I.; Gomez-Villamandos, J.C.; Avila Jurado, I. He-Ne laser therapy by fibroendoscopy in the mucosa of the equine upper airway. Lasers Surg. Med. 1995, 16, 184–188. [Google Scholar] [CrossRef]
- Bader, O.A.; Eesa, M.J. Treatment of hyper-granulated limb wounds in horses. Iraqi J. Vet. Sci. 2011, 2, 71–80. [Google Scholar]
- Bergh, A.; Ridderstråle, Y.; Ekman, S. Defocused CO2 laser on equine skin: A histological examination. Equine Vet. J. 2007, 39, 114–119. [Google Scholar] [CrossRef]
- Duesterdieck-Zellmer, K.F.; Larson, M.K.; Plant, T.K.; Sundholm-Tepper, A.; Payton, M.E. Ex vivo penetration of low-level laser light through equine skin and flexor tendons. Am. J. Vet. Res. 2016, 77, 991–999. [Google Scholar] [CrossRef]
- Ryan, T.; Smith, R.K.W. An investigation into the depth of penetration of low level laser therapy through the equine tendon in vivo. Ir. Vet. J. 2007, 60, 295–299. [Google Scholar] [CrossRef]
- Luna, S.P.L.; Schoen, A.; Trindade, P.H.E.; Rocha, P.B. Penetration profiles of a class iv therapeutic laser and a photobiomodulation therapy device in equine skin. J. Equine Vet. Sci. 2020, 85, 102846. [Google Scholar] [CrossRef]
- Tomacheuski, R.M.; Taffarel, M.O.; Cardoso, G.S.; Derussi, A.A.P.; Ferrante, M.; Volpato, R.; Luna, S.P.L. Postoperative analgesic effects of laserpuncture and meloxicam in bitches submitted to ovariohysterectomy. Vet. Sci. 2020, 21, 94. [Google Scholar] [CrossRef]
- Nascimento, F.F.; Marques, V.I.; Crociolli, G.C.; Nicácio, G.M.; Nicácio, I.P.A.G.; Cassu, R.N. Analgesic efficacy of laser acupuncture and electroacupuncture in cats undergoing ovariohysterectomy. J. Vet. Med. Sci. 2019, 81, 764–770. [Google Scholar] [CrossRef]
- Martin, B.B., Jr.; Klide, A.M. Treatment of chronic back pain in horses. Stimulation of acupuncture points with a low powered infrared laser. Vet. Surg. 1987, 16, 106–110. [Google Scholar] [CrossRef]
- Haussler, K.K.; Manchon, P.T.; Donnell, J.R.; Frisbie, D.D. Effects of low-level laser therapy and chiropractic care on back pain in quarter horses. J. Equine Vet. Sci. 2020, 86, 102891. [Google Scholar] [CrossRef]
- Brevault, S.; Dallongeville, E.; Geffroy, O. Etude de l’efficacite de la therapie laser dans la gestion des dorsalgies du cheval de sport [Study of the effectiveness of laser therapy in the management of dorsalgia in horses]. Prat. Vet. Equine 2016, 191, 24–33. [Google Scholar]
- Petermann, U. Comparison of pre- and post-treatment pain scores of twenty one horses with laminitis treated with acupoint and topical low level impulse laser therapy. Am. J. Tradit. Chin. Vet. Med. 2011, 1, 13–25. [Google Scholar]
- Ghazaleh, N.; Sharifi, D.; Ghamsari, S.; Mokmeli, S.; Rasooli, A. Evaluation of low level laser effects on epidural anaesthesia in horse. Iran. J. Vet. Surg. 2018, 1, 47–53. [Google Scholar]
- Bruno, E.; Canal, S.; Antonucci, M.; Bernardini, M.; Balducci, F.; Musella, V.; Mussoni, M.; Spinella, G. Perilesional photobiomodulation therapy and physical rehabilitation in post-operative recovery of dogs surgically treated for thoracolumbar disk extrusion. BMC Vet. Res. 2020, 16, 120. [Google Scholar] [CrossRef] [PubMed]
- Bennaim, M.; Porato, M.; Jarleton, A.; Hamon, M.; Carroll, J.D.; Gommeren, K.; Balligand, M. Preliminary evaluation of the effects of photobiomodulation therapy and physical rehabilitation on early postoperative recovery of dogs undergoing hemilaminectomy for treatment of thoracolumbar intervertebral disk disease. Am. J. Vet. Res. 2017, 78, 195–206. [Google Scholar] [CrossRef]
- Williams, C.C.; Barone, G. Is low level laser therapy an effective adjunctive treatment to hemilaminectomy in dogs with acute onset parapleglia secondary to intervertebral disc disease? J. Vet. Int. Med. 2011, 25, 730–731. [Google Scholar]
- Draper, W.E.; Schubert, T.A.; Clemmons, R.M.; Miles, S.A. Low-level laser therapy reduces time to ambulation in dogs after hemilaminectomy: A preliminary study. J. Small Anim. Pract. 2012, 53, 465–469. [Google Scholar] [CrossRef]
- Sharifi, D.; Hadjibekloo, A.R.; Ghamsari, S.M.; Taghvi, H.R. Evaluation of low level laser effects on muscular ability in dog: An animal model. J. Fac. Vet. Med. Univ. Tehran 2005, 4, 327–331. [Google Scholar]
- Miller, L.A.; Torraca, D.G.; De Taboada, L. Retrospective observational study and analysis of two different photobiomodulation therapy protocols combined with rehabilitation therapy as therapeutic interventions for canine degenerative myelopathy. Photobiomodul. Photomed. Laser Surg. 2020, 38, 195–205. [Google Scholar] [CrossRef]
- Song, F.; Parekh, S.; Hooper, L.; Loke, Y.K.; Ryder, J.; Sutton, A.J.; Hing, C.; Kwok, C.S.; Pang, C.; Harvey, I. Dissemination and publication of research findings: An updated review of related biases. Health Technol. Assess. 2010, 14, 1–193. [Google Scholar] [CrossRef]
- Rücker, G.; Carpenter, J.R.; Schwarzer, G. Detecting and adjusting for small-study effects in meta-analysis. Biom. J. 2011, 53, 351–368. [Google Scholar] [CrossRef]
- Saito, S.; Shimizu, N. Stimulatory effects of low-power laser irradiation on bone regeneration in midpalatal suture during expansion in the rat. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 525–532. [Google Scholar] [CrossRef]
| Musculoskeletal Conditions | |||||||
|---|---|---|---|---|---|---|---|
| Study | Study Design | Control Group | Study Sample | Intervention and Dosage | Outcome Variables | Main Results | Study Risk of Bias |
| Looney AL et al., 2018 [6] | RCT | Yes | 20 dogs | 10 to 20 J/cm2 (12 Watts, 980 nm, continuous) based on size of dog vs. 0 J/cm2 for 6 weeks | Lameness score, Helsinki Chronic Pain Index pain score, NSAID dose | Reduction in NSAID dose, lameness score, pain score in PBMT vs. sham group in dogs with elbow osteoarthritis | Low |
| Rogatko CP et al., 2016 [7] | RCT | Yes | 27 dogs | Single preoperative treatment 3 J/cm2 (6 watts, 800–970 nm dual wavelength, continuous and pulsed) vs. sham treatment | Lameness score, response to manipulation, force plate evaluation, radiographic healing | Increased weight bearing of treated dogs on force plate at 8 weeks after TPLO surgery, no other differences | Low |
| Renwick SM et al., 2018 [8] | RCT | Yes | 95 dogs | Three treatments in a 4 day post-operative period, optional fourth treatment 10–14 days post-op, total joules of 252 to 2280 J (up to 15 watt continuous, 20 watt peak power, 660 nm red [100 mW], 800, 905, and 970 nm infrared, with 10 phases of different pulse frequency vs. placebo of red light (660 nm [4 mW]). | Liverpool Osteoarthritis in Dogs, adjusted Canine Orthopedic Index, radiographic healing index of osteotomy, time to cessation of NSAID administration, wound healing | Gait section of adjusted Canine Orthopedic Index improved in laser group compared to control group 8 weeks after TPLO surgery. No other differences. | Low |
| Kennedy KC, et al. 2018 [9] | RCT | Yes | 12 dogs | 2.25 J/cm2 during hospital treatment and 1.5 J/cm2 during at-home treatments (class 2 laser 635 nm) vs. control group treated with the same laser units, with the 5-mW diodes replaced with red LED light-bulbs. | Accelerometers, Canine Brief Pain Inventory, force plate evaluation, radiographs, synovial fluid inflammatory markers | Improved ground reaction forces and pain scores in control group compared to laser group | Low |
| Santiago V et al. 2014 [10] | Case control experimental | Yes | 11 dogs | Group 1: of 90 to 120 J/cm2, 790 to 904 nm. Group 2: no laser | Histologic specimens of palatal suture after maxilla expansion | Significant difference in the quality of palatal sutures visually observed. No difference in number of osteoblasts. | Moderate |
| Wozniak P et al., 1997 [11] | Case Study | No | 16 dogs | Details lacking other than continuous 810 nm wavelength | Clinical, radiographic and hematologic clinical assessments | Authors state that most dogs had a positive result of photobiomodulation in dogs with clinical signs of osteomyelitis | High |
| Lindholm AC et al., 2002 [12] | RCT | Comparison group | 179 horses | 60 J/cm2 (25 watts, 10,600 nm) treatments on days 1, 3 and 5 vs. 12 mg betamethasone and 20 mg HA in affected fetlock joints | Lameness score, flexion test, radiographic and ultrasonographic evaluations | Carbon dioxide laser treatment had 80% response rate vs. 68% for betamethasone/hyaluronic acid treatment for arthritis of the fetlock joint | Moderate |
| Bergh A, et al. 2006 [13] | RCT | Yes | 16 horses | 91 J/cm2 (16 watts), 5 treatments over 1 week | Lameness score, accerelrometer, synovial fluid inflammatory markers | No significant differences in lameness scores or synovial fluid inflammatory markers | Low |
| Zielinska P, et al. 2020 [14] | RCT | Yes | 25 horses | 16 J/cm2 (808 nm, 5 watts, 700 Hz) and 16 J/cm2 (980 nm, 4 watts, 1000 Hz) vs. control group | Pain, swelling, lameness, ultrasound evaluation | Laser therapy improved pain, edema, lameness, and lesion percentage, but not tendon lesion echogenicity | Low |
| Marr CM et al., 1993 [15] | Retrospective Study | No | 73 horses | Laser compared with polysulfated glycosaminoglyans or conservative therapy | Return to work, time out of training | No significant differences among groups regarding return to work or time out of training | High |
| Bergh A et al., 2006 [16] | Controlled prospective study | Yes | 10 horses | 91 J/cm2 (10,600 nm, 16 watts, continuous) | Skin and muscle temperature, blood perfusion | Laser treatment increased perfusion and skin temperature in both clipped and unclipped skin, with greater increases in clipped skin. No changes in muscle perfusion or temperature. | Low |
| Godlewska M et al., 2020 [17] | Prospective study | No | 16 horses | 20 J/cm2 (600 J total, 808 nm, 4 watts, 700 Hz) and 15 J/cm2 (980 nm, 450 J total, 2000 Hz) | Surface temperature measurements obtained by thermography camera | Surface temperature of fetlock joints increased by a mean of 3.0 degrees C after laser treatment | Low |
| Monici M et al., 2018 [18] | Ex-vivo experimental study | No | Cadaveric specimens from 1 horse | Two laser diodes, 905 nm (25 watt peak power with 100 ns pulse width, 10 Hz) and 808 nm (1.1 watt continuous mode) | Laser penetration measured in up to 50 μm thickness sections of tendon and ligament with pyroelectric detector | Penetration depth values for superficial digital flexor tendons and suspensory ligaments were 0.5 mm and 0.16 mm, respectively, corresponding to a respective power attenuation factor of 10−3/mm and 10−4/mm, respectively | Moderate |
| Skin and Wound Healing | |||||||
|---|---|---|---|---|---|---|---|
| Study | Study Design | Control Group | Study Sample | Intervention and Dosage | Outcome Variables | Main Results | Study Risk of Bias |
| Gammel JE et al., 2018 [19] | RCT | Yes | 10 dogs | 5 J/cm2 (980 nm, 2 to 3.5 watts, daily treatment for 5 days) vs. sham treatment | Visual assessment, wound measurements, photographs, and biopsies of surgical incisions and punch biopsy wounds | No differences between groups regarding subjective assessment of healing time and wound measurements. Control group had more necrosis and perivascular lymphocytes and macrophages at day 7, and treated group had more perivascular lymphocytes and macrophages on day 14 | Low |
| Kurach LM et al., 2015 [20] | RCT | Yes | 10 dogs | 1.125 J/cm2 (635 nm, 7.5 mW) 3 times weekly for 32 days vs. standard of care management | Wound planimetry, percent contractions and epithelialization, histologic evaluation | No differences between treated and control wounds for any parameter | Low |
| Debraekt MM et al., 1991 [21] | RCT | Yes | 30 dogs | 1 J/cm2 (830 nm, 30 mW) 3 times per week for 10 treatments vs. sham treatment | Wound areas and contraction from standard photographs of Von Langenbeck’s palatal repair | No significant differences in quality or rate of wound healing | Low |
| Wardlaw JL et al., 2019 [22] | RCT | Yes | 9 dogs | 8 J/cm2 (850 nm laser, pulsed 8 Hz with 90% on, 10% off emissions, and 670 nm LED) daily for 7 days vs. non-laser treated controls | Digital photographs and incision healing scores following intervertebral disc surgery | Laser treatment resulted in improved scar scale and cosmetic wound healing | Moderate |
| Bharti, B et al. 2013 [23] | RCT | Yes | 18 dogs | 3 J (10 Hz for 5 min) or 6 J (20 Hz for 10 min) daily for 5 days vs. dressing and antiseptic liquid | Biopsies on days 0 and 14 | No differences between treated and control groups in histopathological examinations | Moderate |
| Marchegiani, A. et al., 2019 [24] | RCT | Yes | 36 dogs | Blue LED device with peak wavelength between 440 and 460 nm, power density of between 55 and 129 mW/cm 2, for 2 min and antibiotic vs. antibiotic control treatment | Global lesion score, neutrophil engulfing bacterial score for evaluation of canine interdigital pyoderma | Significant improvement in both scoring systems compared to antibiotic control group, and decreased time to resolution of lesions | Moderate |
| Stich AN et al., 2014 [25] | RCT | Yes | 30 dogs | 4 J/cm2 (980 nm and 810 nm dual wavelength with 80%/20% output, 4 W, 3 times per week for 2 weeks, then 2 times per week for 2 weeks) vs. placebo laser | Localized atopic dermatitis severity score and owner localized pruritic visual analog score in dogs with atopic dermatitis | No significant differences between groups from weeks 0 and 5, but both groups had decreased scores from baseline | Low |
| Kampa N et al. 2020 [26] | Controlled trial | No | 24 dogs | 4 J/cm2 (830 nm, 200 mW) continuous and pulsed laser with contact and non-contact application | Power meter to determine penetration depth through abdominal skin | Continuous laser had higher mean output power than pulsed laser, mean output power greater for contact vs. non-contact technique, tissue penetration up to 14 mm of tissue depth | Low |
| Hochman-Elam LN et al., 2020 [27] | Prospective research study | N/A | 47 dogs | Two laser systems used, Class IV (980/810 nm, 0.5, 1,5, 3, and 5 W assessed) and Class IIIb (904 nm, 500 mW) | Thermophile laser sensor to detect light penetration through inguinal fold and calcaneal tendon in different coloured dogs with varying coat lengths | Laser transmission was greater in Class IV laser, higher powers, dogs with shaved skin, less skin pigment. Coat length was not a significant predictor of laser penetration. | Low |
| Keerti N et al., 2016 [28] | RCT | Yes | 12 dogs | 2.4 J (30 Hz, 2 or 4 min) for 7 days vs. antibiotic control | Visual score cards for evaluation of inflammation, exudation, embedding of sutures, and gross appearance of suture line in dogs with aural hematomas | Laser treated dogs had less inflammation, exudation, minimum embedding of sutures and faster healing | High |
| Olivieri L et al., 2014 [29] | Case study | No (untreated area of skin for comparison) | 7 dogs | 3 J/cm2 (3 diodes, 470 nm, 685 nm, 830 nm, 13 × 16 MW, 4 × 50 mW, and 4 × 200 mW, respectively, 5 Hz) twice weekly | Hair regrowth in dogs with canine non-inflammatory alopecia | Hair regrowth greatly improved in 6/7 dogs, improved in 1 | High |
| Kaneps AJ et al., 1984 [30] | RCT | Yes | 6 horses | 57 mJ, (904 nm, pulsed with 300 nsec pulse dura-tion), 15 min, for 5 days | Histologic evaluation of skin and superficial digital flexor tendons of horse with surgical incisions | No qualitative differences in healing between laser irradiated and nonirradiated tissues | Low |
| Petersen SL et al., 1999 [31] | RCT | Yes | 6 horses | 2 J/cm2 (830 nm, 30 mW) daily vs. nontreated controls | Photoplanimetry to evaluate wound contraction and epithelialization on surgically created open wounds | Laser had no clinically significant effect on wound healing | Low |
| Gomez-Villamandos RJ et al., 1995 [32] | RCT | Yes | 12 horses | He-Ne fibroendoscope, daily for 7 days | Histopathology of created pharyngeal mucosal ulcers | Laser treatment accelerated cicatrisation faster than controls | Moderate |
| Bader OA et al., 2011 [33] | RCT | Yes | 40 wounds | 9.72 J/cm2 laser treatment compare with bandage alone, copper sulfate ointment, silver nitrate ointment, red mercury ointment | Clinical and histopathology of created wounds with granulation tissue | Surgical removal of granulation tissue followed by laser treatment resulted in more rapid healing | Moderate |
| Bergh A, 2007 [34] | RCT | No | 13 horses | 91 J/cm2 to skin of hamstrings, 137 J/cm2 to fetlock, and 450 J/cm2 to loin areas (10,600 nm, 16–20 W) | Histology of skin in horses | Dose dependent changes occurred in skin histology after laser, with severe tissue damage in the 450 J/cm2 dose | Low |
| Duesterdieck-Zellmer KF et al., 2016 [35] | Research Study | No | 19 equine cadavers | 1 W, 800 and 970 nm | Percentage of energy penetration by photodetector measured in superficial digital and deep digital flexor tendons before and after clipping and after shaving in horses of different skin color | Clipping or shaving improved laser penetration, light-colored skin allowed the greatest penetration, 800 nm was best in light-colored skin, and 970 nm best in dark-colored skin. Only 1–20% and 0.1–4% of energy was absorbed by SDFT and DDFT, respectively | Low |
| Ryan T et al., 2007 [36] | Research Study | No | 9 equine cadavers | 500 mW, 810 nm | Photodetector for measuring penetration of laser in tendons | Coat colour did not affect penetration to superficial digital flexor tendons. Clipped hair and skin cleaned with alcohol increased light transmission | Low |
| Luna SPL et al., 2020 [37] | Experimental study | No | 12 horses | 2 lasers compared, 67.92 J/cm2 (980 nm, 9 W) and 0.34 J/cm2 (905 nm, superpulsed peak power 50 W, 1.25 W average output) | Cervical skin thickness measured with a cutometer and ultrasound, percentage of laser penetration measured with photodector | There was greater penetration in cervical skin with the superpulsed laser than the class IV laser. There was also greater penetration in light skin horses | Moderate |
| Pain | |||||||
|---|---|---|---|---|---|---|---|
| Study | Study Design | Control Group | Study Sample | Intervention and Dosage | Outcome Variables | Main Results | Study Risk of Bias |
| Tomacheuski RM et al., 2020 [38] | RCT | No | 16 dogs | 10 J over 5 acupuncture points (904 nm, 124 Hz) laser acupuncture vs. meloxicam | Glasgow Composite Measure Pain Scale and Dynamic Interactive Visual Analog Scale | Dogs with laser acupuncture had lower pain scores at several time points following routine ovariohysterectomy | Moderate |
| Nascimento FF et al., 2019 [39] | RCT | Yes | 30 cats | 3 J/cm2 (904 nm, 70 mW, 124 Hz) at acupuncuture points vs. electroacupuncture at same points vs. control | Interactive Visual Analogue Scale and UNESP-Botucatu Multidimensional Composite Pain Scale in cats undergoing routine ovariohysterectomy. | The pain scores did not significantly differ between the treatment groups at any time point. The prevalence of rescue analgesia was significantly higher in the control group than in the laser acupuncture and electroacupuncture groups | Moderate |
| Martin BB et al., 1987 [40] | Case study | No | 14 horses | 3 mW, 904 nm, 360 Hz, 2 min contact over each of five acupuncture points once weekly for 8–16 weeks | Clinical signs of back pain, ability to perform, owner evaluation of horses with back pain | Clinical signs alleviated in 10, 3 unchanged, 1 lost to follow-up | High |
| Haussler KK et al., 2020 [41] | RCT | No | 61 horses | 94 J/cm2 (4 810 nm diode lasers, 3 W total power) laser applied to 5–10 sites based on clinical findings compared with chiropractic or combined laser and chiropractic treatment | Visual analog scale of perceived back pain and dysfunction, detailed spinal examinations evaluating pain, muscle tone, and stiffness. | Laser therapy produced significant reductions in back pain, epaxial muscle hypertonicity, and trunk stiffness. Combined laser and chiropractic produced similar reductions. Chiropractic treatment by itself did not produce any significant changes in back pain, muscle hypertonicity, or trunk stiffness. | Moderate |
| Brevault S et al., 2016 [42] | RCT | Yes | Details unavailable | Details unavailable | Muscle tone, back mobility, deep and superficial sensitivity, dynamic assessment and rider evaluation of back pain in horses | Muscle tone, back mobility, deep and superficial sensitivity improved with laser treatment, but no differences in dynamic assessment and rider evaluation | High |
| Petermann U, 2011 [43] | Case study | No | 21 horses | Details unavailable, laser therapy to acupuncture points | Pain score of horses with laminitis | Post treatment pain scores improved over pre-treatment scores | High |
| Ghazaleh N et al., 2018 [44] | Prospective experimental cross-over design | Yes | 5 horses | Laser treatment (3000 Hz for 10 min) compared with saline, lidocaine, and laser plus lidocaine caudal epidural injections | Motor and sensory blockade evaluations assess by transcutaneous electrical nerve stimulation, noxious stimulus with a pin, and pinch test in horses undergoing epidural analgesia | No difference in sensory or motor stimulation response between groups, but laser in combination with lidocaine had a longer duration of analgesia than laser or epidural alone | High |
| Neurologic Conditions | |||||||
|---|---|---|---|---|---|---|---|
| Study | Study Design | Control Group | Study Sample | Intervention and Dosage | Outcome Variables | Main Results | Study Risk of Bias |
| Bruno E et al., 2020 [45] | Retrospective study | Yes | 24 dogs | 4 J/cm2 (808 and 905 nm, 50% duty cycle, 18 Hz,1.2 W with peak power of 75 W, correction of dose with skin color) daily at the time of rehabilitation vs. rehabilitation and no laser. | Modified Frankel scoring system in dogs undergoing postoperative care following intervertebral disk herniation surgery | There was no statistical difference in time to regain ambulatory ability | Moderate |
| Bennaim M et al., 2017 [46] | RCT | Yes | 32 dogs | 12 J (810 nm, 1 W cluster probe with 5 clusters, 5.5 W/cm2, 2.5 Hz) daily for 5 days vs. laser and physical rehabilitation with sham laser or sham laser only | Duration of postoperative IV opioid administration and recovery grades in dogs following intervertebral disk herniation surgery | Time to reach recovery and duration of postoperative IV opioid administration did not differ among groups | Low |
| Williams CC et al., 2011 [47] | RCT | Yes | 17 dogs | 635 nm, 9–1151 Hz, other details not available vs. control | Recovery time following intervertebral disk herniation surgery | Laser did not shorten recovery times | Moderate |
| Draper WE, et al. 2012 [48] | RCT | Yes | 36 dogs | 12 J (810 nm, 1 W cluster probe with 5 clusters, 25 W/cm2) over 3 sites for 1 min/site daily for 5 days vs. no treatment | Modified Frankel scoring system in dogs following intervertebral disk herniation surgery | Time to achieve a modified Frankel score of 4 was significantly lower in the laser group compared to the control group | Moderate |
| Sharifi, D et al. 2005 [49] | Experimental controlled study | Yes | 10 dogs | Details not available regarding laser treatment except 10 min of laser treatment daily for 2 weeks vs. no laser | Electromyography (EMG) | EMG showed significant differences in muscle force of the semimembranosus and semitendinosus muscles in dogs undergoing experimental crush sciatic nerve injury | High |
| Miller LA et al., 2020 [50] | Retrospective | No | 20 dogs | Class III laser 8 J/cm2 (904 nm, 500 mW) vs. Class IV laser 14–21 J/cm2 (980 nm, 6–12 W) | Time from symptom onset and euthanasia, time between symptom onset and nonambulatory paresis or paralysis | Dogs receiving Class IV laser had slower disease progression and longer survival times | High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Millis, D.L.; Bergh, A. A Systematic Literature Review of Complementary and Alternative Veterinary Medicine: Laser Therapy. Animals 2023, 13, 667. https://doi.org/10.3390/ani13040667
Millis DL, Bergh A. A Systematic Literature Review of Complementary and Alternative Veterinary Medicine: Laser Therapy. Animals. 2023; 13(4):667. https://doi.org/10.3390/ani13040667
Chicago/Turabian StyleMillis, Darryl L., and Anna Bergh. 2023. "A Systematic Literature Review of Complementary and Alternative Veterinary Medicine: Laser Therapy" Animals 13, no. 4: 667. https://doi.org/10.3390/ani13040667
APA StyleMillis, D. L., & Bergh, A. (2023). A Systematic Literature Review of Complementary and Alternative Veterinary Medicine: Laser Therapy. Animals, 13(4), 667. https://doi.org/10.3390/ani13040667






