Examining the Effects of Hyperbaric Oxygen Therapy on the Cardiovascular System and Oxidative Stress in Insulin-Treated and Non-Treated Diabetic Rats
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Animals and Experimental Design
- (1)
- DM group: diabetes induced by streptozotocin (STZ) injection;
- (2)
- DM+HBOT group: received both STZ injection and HBOT, exposed to 100% oxygen at 2.8 ATA (atmosphere absolute) for 1 h once daily, for 5 days (two weeks);
- (3)
- DM+INS group: NPH insulin 5 U/day;
- (4)
- DM+HBOT+INS group: received both NPH insulin and HBO exposure for 2 weeks.
2.3. Induction of Diabetes
2.4. Protocol of Human NPH Insulin Treatment
2.5. HBO Treatment
2.6. Biochemical Assays
2.6.1. TBARS Determination (Index of Lipid Peroxidation)
2.6.2. Nitrite Determination
2.6.3. Hydrogen Peroxide Determination
2.6.4. Superoxide Anion Radical Determination
2.7. Ex Vivo Monitoring of Cardiac Function
2.8. Statistical Analysis
3. Results
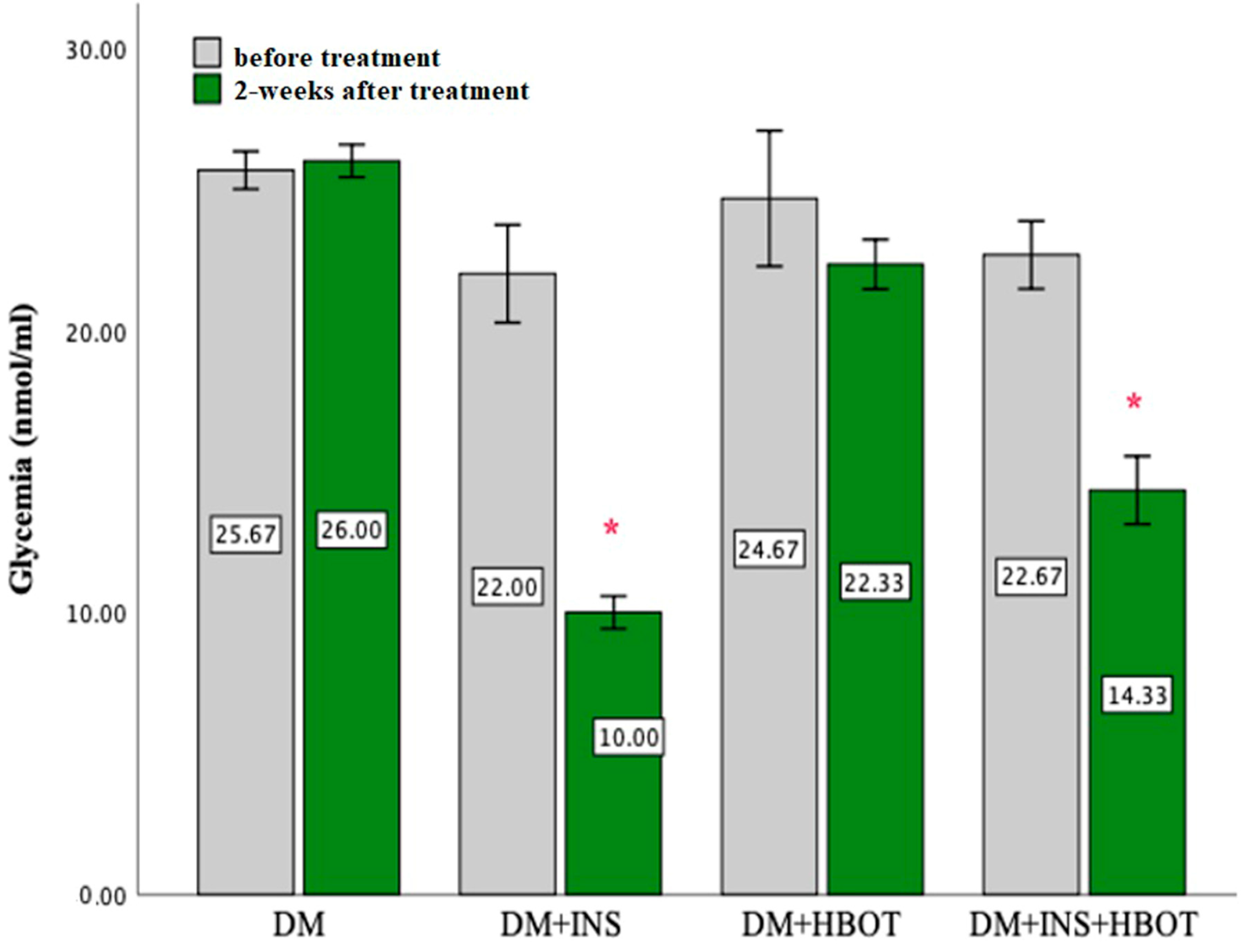
3.1. Glycemia
3.2. Biomarkers of Oxidative Stress
3.2.1. Superoxide Anion Radical (O2−)
3.2.2. Hydrogen Peroxide (H2O2)
3.2.3. Index of Lipid Peroxidation (Measured as TBARS)
3.2.4. Nitric Oxide (NO)
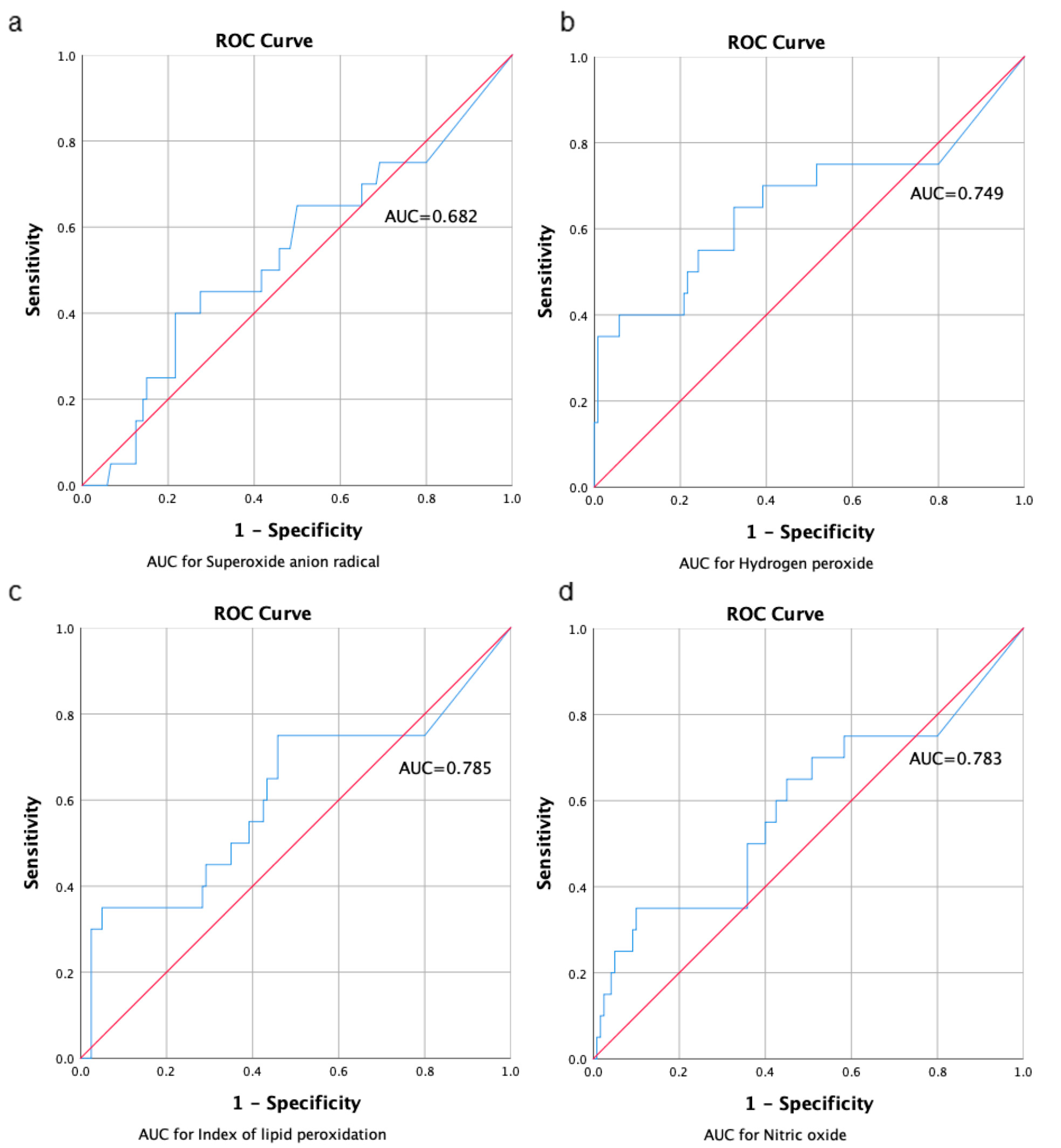
3.2.5. AUC for Markers of Oxidative Stress
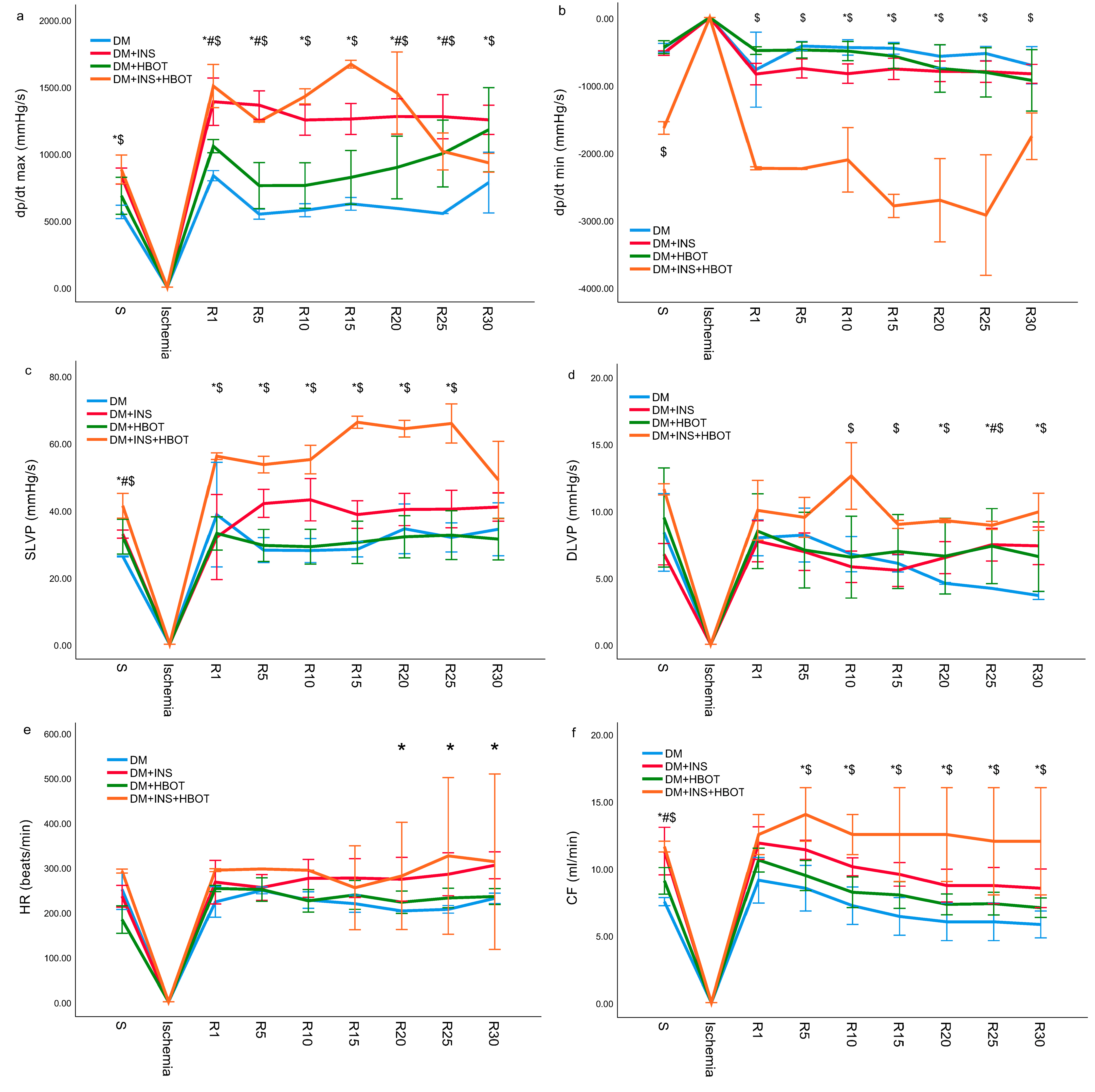
3.3. Estimation of Cardiac Function
3.3.1. Minimum Rate of Left Ventricular Pressure Development (dp/dt min)
3.3.2. Minimum Rate of Left Ventricular Pressure Development (dp/dt min)
3.3.3. Systolic Left Ventricular Pressure (SLVP)
3.3.4. Diastolic Left Ventricular Pressure (DLVP)
3.3.5. Heart Rate (HR)
3.3.6. Coronary Flow (CF)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Akinlade, O.M.; Owoyele, B.V.; Soladoye, A.O. Streptozotocin-induced type 1 and 2 diabetes in rodents: A model for studying diabetic cardiac autonomic neuropathy. Afr. Health Sci. 2021, 21, 719–727. [Google Scholar] [CrossRef] [PubMed]
- Matsunami, T.; Sato, Y.; Morishima, T.; Mano, Y.; Yukawa, M. Enhancement of glucose toxicity by hyperbaric oxygen exposure in diabetic rats. Tohoku J. Exp. Med. 2008, 216, 127–132. [Google Scholar] [CrossRef] [PubMed]
- De Wolde, S.D.; Hulskes, R.H.; Weenink, R.P.; Hollmann, M.W.; van Hulst, R.A. The Effects of Hyperbaric Oxygenation on Oxidative Stress, Inflammation and Angiogenesis. Biomolecules 2021, 11, 1210. [Google Scholar] [CrossRef] [PubMed]
- Fosen, K.M.; Thom, S.R. Hyperbaric oxygen, vasculogenic stem cells, and wound healing. Antioxid. Redox Signal. 2014, 21, 1634–1647. [Google Scholar] [CrossRef] [PubMed]
- Francis, A.; Baynosa, R. Ischaemia-reperfusion injury and hyperbaric oxygen pathways: A review of cellular mechanisms. Diving Hyperb. Med. 2017, 47, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Zamboni, W.A.; Roth, A.C.; Russell, R.C.; Nemiroff, P.M.; Casas, L.; Smoot, E.C. The effect of acute hyperbaric oxygen therapy on axial pattern skin flap survival when administered during and after total ischemia. J. Reconstr. Microsurg. 1989, 5, 343–350. [Google Scholar] [CrossRef]
- Zamboni, W.A.; Roth, A.C.; Russell, R.C.; Smoot, E.C. The effect of hyperbaric oxygen on reperfusion of ischemic axial skin flaps: A laser Doppler analysis. Ann. Plast. Surg. 1992, 28, 339–341. [Google Scholar] [CrossRef]
- Kaelin, C.M.; Im, M.J.; Myers, R.A.; Manson, P.N.; Hoopes, J.E. The effects of hyperbaric oxygen on free flaps in rats. Arch. Surg. 1990, 125, 607–609. [Google Scholar] [CrossRef]
- Godman, C.A.; Chheda, K.P.; Hightower, L.E.; Perdrizet, G.; Shin, D.G.; Giardina, C. Hyperbaric oxygen induces a cytoprotective and angiogenic response in human microvascular endothelial cells. Cell Stress Chaperones 2010, 15, 431–442. [Google Scholar] [CrossRef]
- Esmaie, E.M.; Abo-Youssef, A.M.; Tohamy, M.A. Antidiabetic and antioxidant effects of tannic acid and melatonin on streptozotocin induced diabetes in rats. Pak. J. Pharm. Sci. 2019, 32, 1453–1459. [Google Scholar]
- Pinheiro, L.; de Melo, A.; Andreazzi, A.; de Caires, L.C., Jr.; Costa, M.; Garcia, R. Protocol of Insulin Therapy for Streptozotocin-Diabetic Rats Based on a Study of Food Ingestion and Glycemic Variation. Scand. J. Lab. Anim. Sci. 2011, 38, 117–127. [Google Scholar]
- Koo, S.T.; Lee, C.H.; Choi, H.; Shin, Y.I.; Ha, K.T.; Ye, H.; Shim, H.B. The Effects of Pressure on Arthritic Knees in a Rat Model of CFA-Induced Arthritis. Pain Physician 2013, 16, E95–E102. [Google Scholar] [PubMed]
- Ohkawa, H.; Ohishi, N.; Yagi, K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 1979, 95, 351–358. [Google Scholar] [CrossRef]
- Green, L.C.; Wagner, D.A.; Glogowski, J.; Skipper, P.L.; Wishnok, J.S.; Tannenbaum, S.R. Analysis of nitrate, nitrite and [15N]nitrate in biological fluids. Anal. Biochem. 1982, 126, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Pick, E.; Keisari, Y. A simple colorimetric method for the measurement of hydrogen peroxide produced by cells in culture. J. Immunol. Methods 1980, 38, 161–170. [Google Scholar] [CrossRef]
- Auclair, C.; Voisin, E. Nitroblue tetrazolium reduction. In Handbook of Methods for Oxygen Radical Research; Greenvvald, R.A., Ed.; CRC Press: Boka Raton, FL, USA, 1985; pp. 123–132. [Google Scholar]
- Jeremic, J.N.; Jakovljevic, V.L.; Zivkovic, V.I.; Srejovic, I.M.; Bradic, J.V.; Milosavljevic, I.M.; Mitrovic, S.L.; Jovicic, N.U.; Bolevich, S.B.; Svistunov, A.A.; et al. Garlic derived diallyl trisulfde in experimental metabolic syndrome: Metabolic efects and cardioprotective role. Int. J. Mol. Sci. 2020, 30, 9100. [Google Scholar] [CrossRef]
- Jakovljevic, V.; Vorobyev, S.; Bolevich, S.; Morozova, E.; Bolevich, S.; Saltykov, A.; Litvickiy, P.; Fisenko, V.; Tsymbal, A.; Orlova, A.; et al. Dose-dependent effects of perfluorocarbon-based blood substitute on cardiac function in myocardial ischemia-reperfusion injury. Mol. Cell Biochem. 2022, 477, 2773–2786. [Google Scholar] [CrossRef] [PubMed]
- Stratton, I.M.; Adler, A.I.; Neil, H.A.; Matthews, D.R.; Manley, S.E.; Cull, C.A.; Hadden, D.; Turner, R.C.; Holman, R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ 2000, 321, 405–412. [Google Scholar] [CrossRef]
- Gaede, P.; Vedel, P.; Larsen, N.; Jensen, G.V.; Parving, H.H.; Pedersen, O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N. Engl. J. Med. 2003, 348, 383–393. [Google Scholar] [CrossRef]
- Klein, R. Hyperglycemia and microvascular and macrovascular disease in diabetes. Diabetes Care 1995, 18, 258–268. [Google Scholar] [CrossRef]
- Brownlee, M. Biochemistry and molecular cell biology of diabetic complications. Nature 2001, 414, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Newsholme, P.; Cruzat, V.F.; Keane, K.N.; Carlessi, R.; de Bittencourt, P.I., Jr. Molecular mechanisms of ROS production and oxidative stress in diabetes. Biochem. J. 2016, 473, 4527–4550. [Google Scholar] [CrossRef] [PubMed]
- Hanna, M.K. The contribution of preconditioning hyperbaric oxygen for complex re-operative surgery of bladder exstrophy and epispadias. A case study of 11 patients. J. Pediatr. Urol. 2021, 17, 656.e1–656.e8. [Google Scholar] [CrossRef] [PubMed]
- Kakkar, R.; Kalra, J.; Mantha, S.V.; Prasad, K. Lipid peroxidation and activity of antioxidant enzymes in diabetic rats. Mol. Cell Biochem. 1995, 151, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Ilhan, H.; Eroglu, M.; Inal, V.; Eyi, Y.E.; Arziman, I.; Yildirim, A.O.; Tansel, A.; Uzun, G.; Yamanel, L. Hyperbaric oxygen therapy alleviates oxidative stress and tissue injury in renal ischemia/reperfusion injury in rats. Ren. Fail. 2012, 34, 1305–1308. [Google Scholar] [CrossRef]
- Açiksari, K.; Eğin, S.; Hepgül, G.; Mirasoğlu, B.; Tanriverdi, G.; Kanber, D.S.; Demirci, S.; Doğan, H.; Özüçelik, D.N.; Toklu, A.S.; et al. Protective effect of hyperbaric oxygen treatment on rat intestinal mucosa after mesenteric ischaemia and reperfusion. Diving Hyperb. Med. 2019, 49, 253–258. [Google Scholar] [CrossRef]
- Ishibashi, M.; Hayashi, A.; Akiyoshi, H.; Ohashi, F. The influences of hyperbaric oxygen therapy with a lower pressure and oxygen concentration than previous methods on physiological mechanisms in dogs. J. Vet. Med. Sci. 2015, 77, 297–304. [Google Scholar] [CrossRef]
- Sadi, G.; Güray, T. Gene expressions of Mn-SOD and GPx-1 in streptozotocin-induced diabetes: Effect of antioxidants. Mol. Cell Biochem. 2009, 327, 127–134. [Google Scholar] [CrossRef]
- Tepic, S.; Petkovic, A.; Srejovic, I.; Jeremic, N.; Zivkovic, V.; Loncarevic, S.; Bradic, J.; Jakovljevic, V.; Zivkovic, M. Impact of hyperbaric oxygenation on oxidative stress in diabetic patients. Undersea Hyperb. Med. 2018, 45, 9–17. [Google Scholar] [CrossRef]
- Dedov, I.I.; Abusuev, S.A.; Muslimova, Z.Z.; Dreval’, A.V. Efficacy of repeated courses of hyperbaric oxygenation in treatment of insulin-dependent diabetes mellitus. Probl. Endokrinol. 1994, 40, 25–28. [Google Scholar]
- Schipke, J.D.; Muth, T.; Pepper, C.; Schneppendahl, J.; Hoffmanns, M.; Dreyer, S. Hyperoxia and the cardiovascular system: Experiences with hyperbaric oxygen therapy. Med. Gas Res. 2022, 12, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Takemura, A. Exposure to a mild hyperbaric oxygen environment elevates blood pressure. J. Phys. Ther. Sci. 2022, 34, 360–364. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ristic, P.; Savic, M.; Bolevich, S.; Bolevich, S.; Orlova, A.; Mikhaleva, A.; Kartashova, A.; Yavlieva, K.; Nikolic Turnic, T.; Pindovic, B.; et al. Examining the Effects of Hyperbaric Oxygen Therapy on the Cardiovascular System and Oxidative Stress in Insulin-Treated and Non-Treated Diabetic Rats. Animals 2023, 13, 2847. https://doi.org/10.3390/ani13182847
Ristic P, Savic M, Bolevich S, Bolevich S, Orlova A, Mikhaleva A, Kartashova A, Yavlieva K, Nikolic Turnic T, Pindovic B, et al. Examining the Effects of Hyperbaric Oxygen Therapy on the Cardiovascular System and Oxidative Stress in Insulin-Treated and Non-Treated Diabetic Rats. Animals. 2023; 13(18):2847. https://doi.org/10.3390/ani13182847
Chicago/Turabian StyleRistic, Petar, Maja Savic, Sergey Bolevich, Stefani Bolevich, Alexandra Orlova, Anastasiya Mikhaleva, Anna Kartashova, Koka Yavlieva, Tamara Nikolic Turnic, Bozidar Pindovic, and et al. 2023. "Examining the Effects of Hyperbaric Oxygen Therapy on the Cardiovascular System and Oxidative Stress in Insulin-Treated and Non-Treated Diabetic Rats" Animals 13, no. 18: 2847. https://doi.org/10.3390/ani13182847
APA StyleRistic, P., Savic, M., Bolevich, S., Bolevich, S., Orlova, A., Mikhaleva, A., Kartashova, A., Yavlieva, K., Nikolic Turnic, T., Pindovic, B., Djordjevic, K., Srejovic, I., Zivkovic, V., & Jakovljevic, V. (2023). Examining the Effects of Hyperbaric Oxygen Therapy on the Cardiovascular System and Oxidative Stress in Insulin-Treated and Non-Treated Diabetic Rats. Animals, 13(18), 2847. https://doi.org/10.3390/ani13182847





