Liver Receptor homolog-1 Regulates Apoptosis of Bovine Ovarian Granulosa Cells by Progestogen Receptor Signaling Pathway
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
2.2. Primary Cell Cultures and Treatment
2.3. Steroid Assay
2.4. Measurement of Cell Viability
2.5. Apoptosis Measurements
2.6. Immunohistochemistry
2.7. Quantitative Real-Time PCR
2.8. Western Blotting
2.9. Immunofluorescence
2.10. Statistical Analysis
3. Results
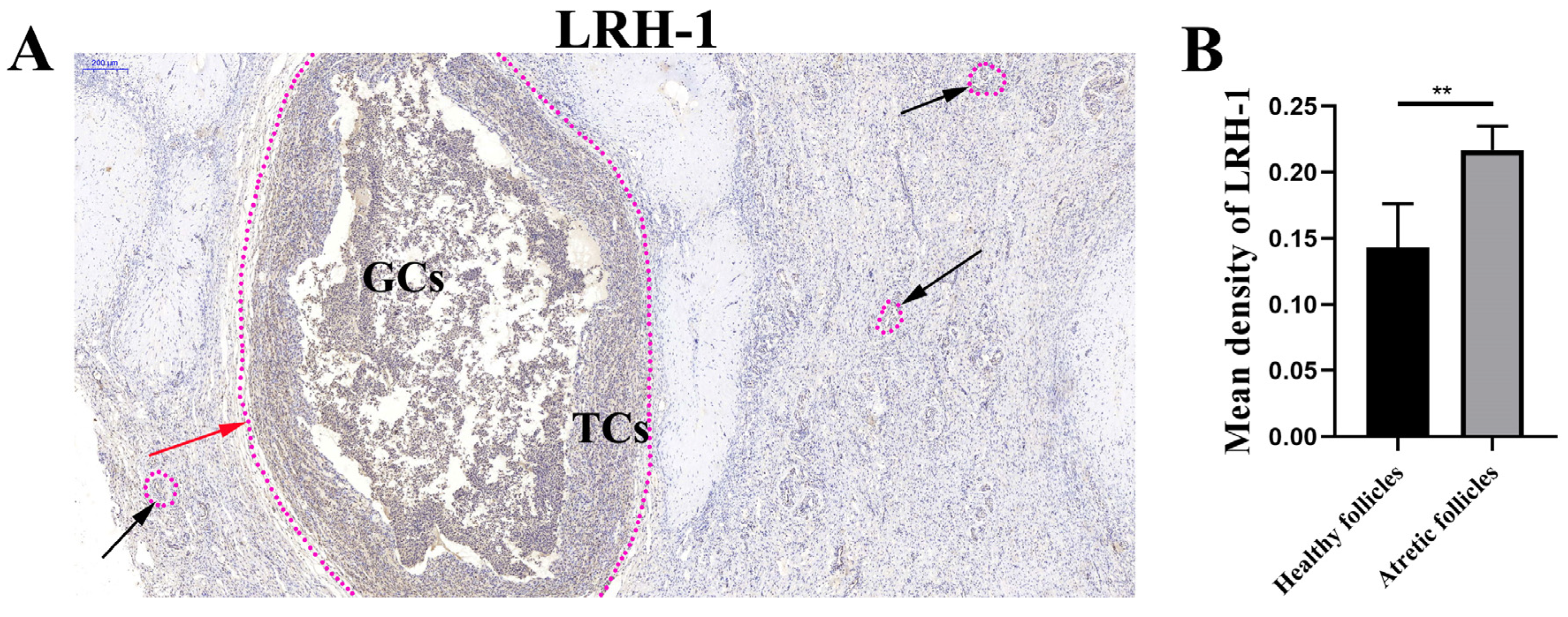
3.1. LRH-1 High Expression in the Atretic Follicles
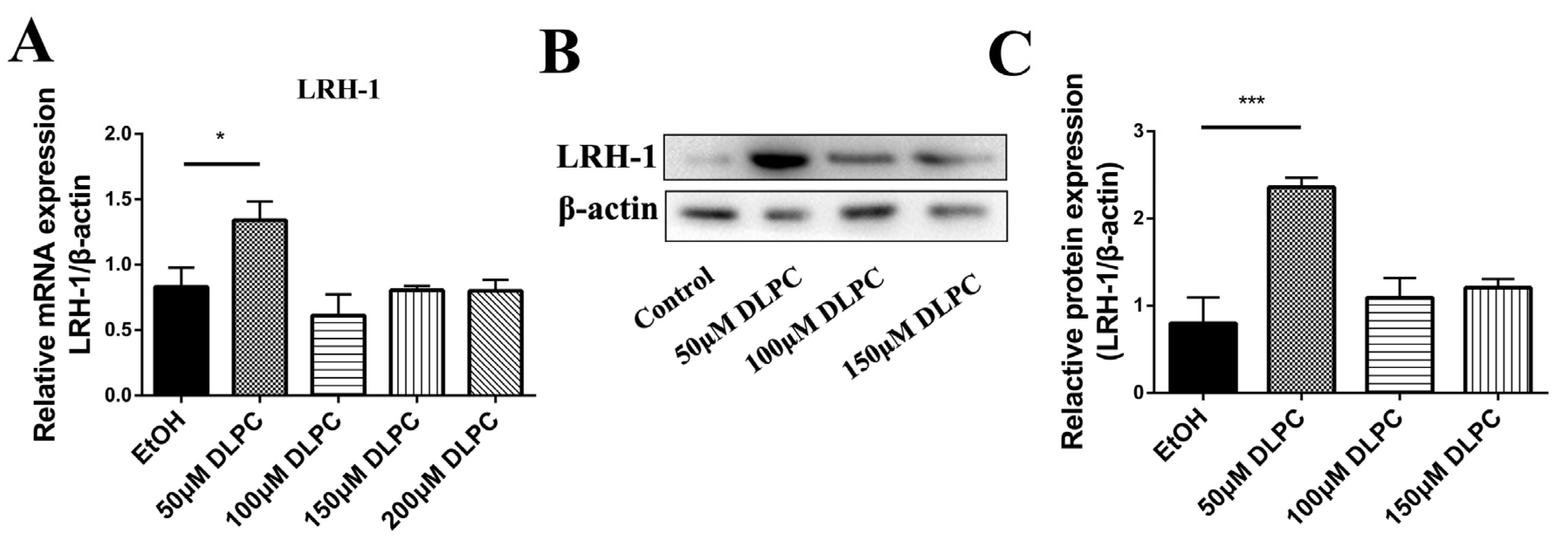
3.2. DLPC Induced LRH-1 Expression
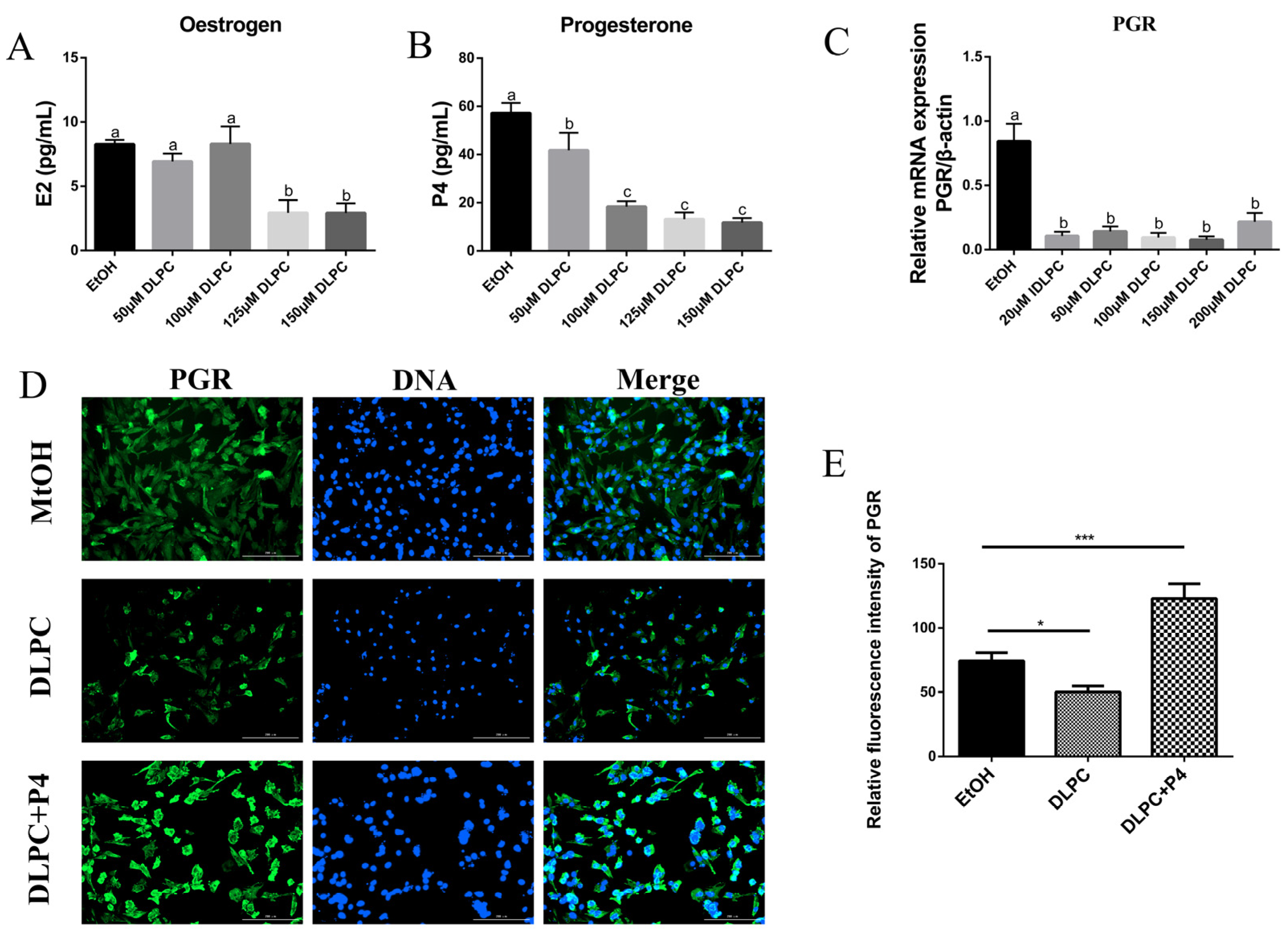
3.3. LRH-1 Activation Blocked Progestogen Receptor Signaling Pathway
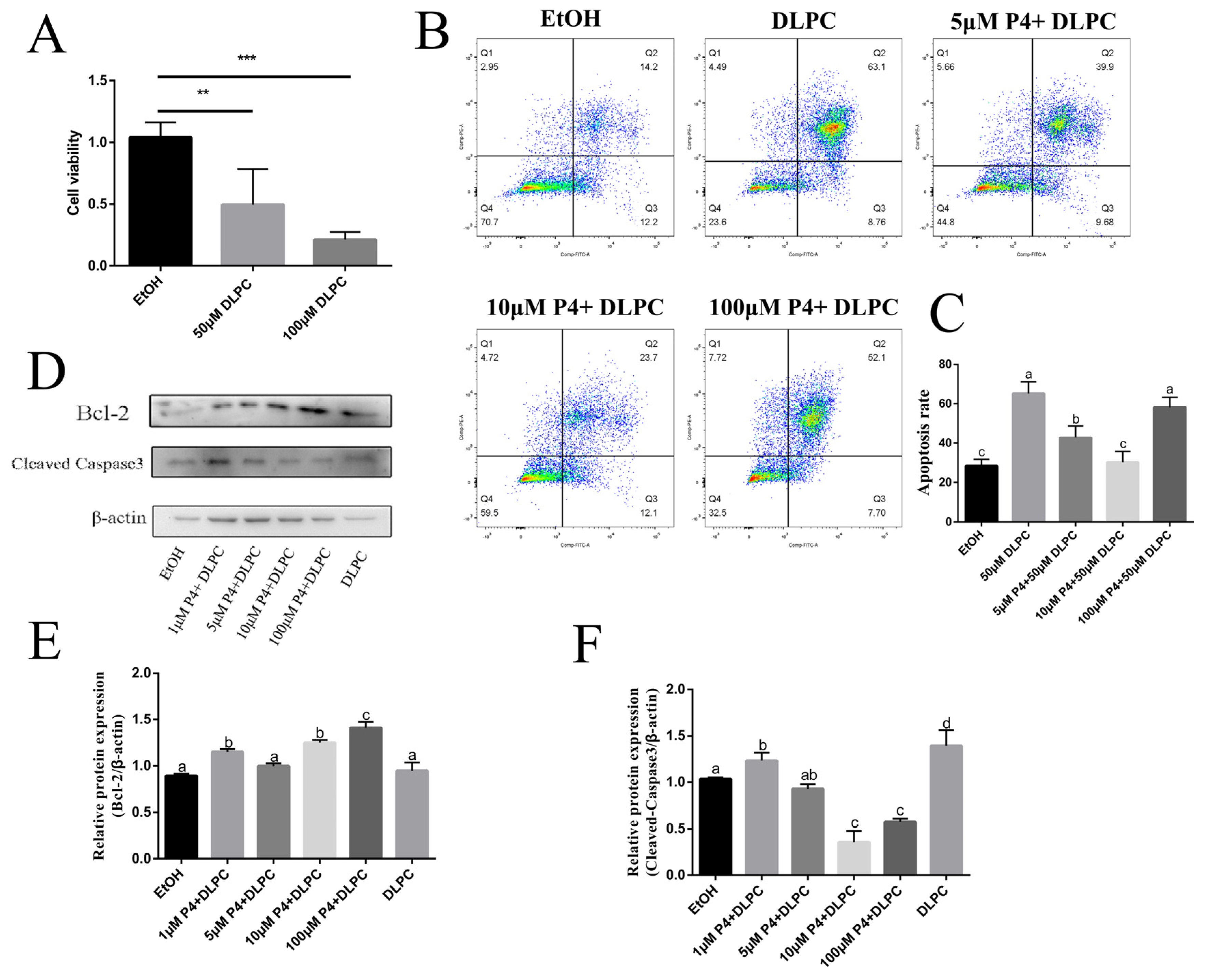
3.4. LRH-1 Mediated Apoptosis via Progestogen Signaling
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gougeon, A. Dynamics of follicular growth in the human: A model from preliminary results. Hum. Reprod. 1986, 1, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Hughes, F.M.; Gorospe, W.C. Biochemical identification of apoptosis (programmed cell death) in granulosa cells: Evidence for a potential mechanism underlying follicular atresia. Endocrinology 1991, 129, 2415–2422. [Google Scholar] [CrossRef] [PubMed]
- Manabe, N.; Goto, Y.; Matsuda-Minehata, F.; Inoue, N.; Maeda, A.; Sakamaki, K.; Miyano, T. Regulation mechanism of selective atresia in porcine follicles: Regulation of granulosa cell apoptosis during atresia. J. Reprod. Dev. 2004, 50, e493514. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, J.K.; Sharma, R.K. Scanning electron microscopic changes in granulosa cells during follicular atresia in caprine ovary. Scanning 2011, 33, 21–24. [Google Scholar] [CrossRef]
- Mataki, C.; Magnier, B.C.; Houten, S.M.; Annicotte, J.-S.; Argmann, C.; Thomas, C.; Overmars, H.; Kulik, W.; Metzger, D.; Auwerx, J.; et al. Compromised Intestinal Lipid Absorption in Mice with a Liver-Specific Deficiency of Liver Receptor Homolog 1. Mol. Cell. Biol. 2007, 27, 8330–8339. [Google Scholar] [CrossRef]
- Kramer, H.B.; Lai, C.F.; Patel, H.; Periyasamy, M.; Lin, M.L.; Feller, S.M.; Fuller-Pace, F.V.; Meek, D.W.; Ali, S.; Buluwela, L. LRH-1 drives colon cancer cell growth by repressing the expression of the CDKN1A gene in a p53-dependent manner. Nucleic Acids Res. 2016, 44, 582–594. [Google Scholar] [CrossRef]
- Baquié, M.; St-Onge, L.; Kerr-Conte, J.; Cobo-Vuilleumier, N.; Lorenzo, P.; Moreno, C.M.J.; Cederroth, C.R.; Nef, S.; Borot, S.; Bosco, D.; et al. The liver receptor homolog-1 (LRH-1) is expressed in human islets and protects β-cells against stress-induced apoptosis. Hum. Mol. Genet. 2017, 27, 406. [Google Scholar] [CrossRef]
- Saxena, D.; Escamilla-Hernandez, R.; Little-Ihrig, L.; Zeleznik, A.J. Liver receptor homolog-1 and steroidogenic factor-1 have similar actions on rat granulosa cell steroidogenesis. Endocrinology 2007, 148, 726–734. [Google Scholar] [CrossRef][Green Version]
- Zhang, C.; Large, M.J.; Duggavathi, R.; DeMayo, F.J.; Lydon, J.P.; Schoonjans, K.K.; Murphy, B.D. Liver receptor homolog-1 is essential for pregnancy. Nat. Med. 2013, 19, 1061–1066. [Google Scholar] [CrossRef]
- Duggavathi, R.; Volle, D.H.; Mataki, C.; Antal, M.C.; Messaddeq, N.; Auwerx, J.; Murphy, B.D.; Schoonjans, K. Liver receptor homolog 1 is essential for ovulation. Genes Dev. 2008, 22, 1871–1876. [Google Scholar] [CrossRef]
- Lin, Q.; Aihara, A.; Chung, W.; Li, Y.; Huang, Z.; Chen, X.; Weng, S.; Carlson, R.I.; Wands, J.R.; Dong, X. LRH1 as a driving factor in pancreatic cancer growth. Cancer Lett. 2014, 345, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zou, Z.; Luo, X.; Mi, Y.; Chang, H.; Xing, D. LRH1 enhances cell resistance to chemotherapy by transcriptionally activating MDC1 expression and attenuating DNA damage in human breast cancer. Oncogene 2018, 37, 3243–3259. [Google Scholar] [CrossRef] [PubMed]
- Saxena, D.; Safi, R.; Little-Ihrig, L.; Zeleznik, A.J. Liver receptor homolog-1 stimulates the progesterone biosynthetic pathway during follicle-stimulating hormone-induced granulosa cell differentiation. Endocrinology 2004, 145, 3821–3829. [Google Scholar] [CrossRef] [PubMed]
- Labelle-Dumais, C.; Pare, J.F.; Belanger, L.; Farookhi, R.; Dufort, D. Impaired progesterone production in Nr5a2 mice leads to a reduction in female reproductive function. Biol. Reprod. 2007, 77, 217–225. [Google Scholar] [CrossRef]
- Mishra, B.; Park, J.Y.; Wilson, K.; Jo, M. X-linked lymphocyte regulated gene 5c-like (Xlr 5c-like) is a novel target of progesterone action in granulosa cells of periovulatory rat ovaries. Mol. Cell. Endocrinol. 2015, 412, 226–238. [Google Scholar] [CrossRef]
- Pompei, L.M.; Cunha, E.P.; Steiner, M.L.; Theodoro, T.R.; Mader, A.M.; Petri, G.; Pinhal, M.A.; Fernandes, C.E. Effects of estradiol, progestogens, and of tibolone on breast proliferation and apoptosis. Climacteric 2015, 18, 518–522. [Google Scholar] [CrossRef]
- Annie, L.; Gurusubramanian, G.; Roy, V.K. Estrogen and progesterone dependent expression of visfatin/NAMPT regulates proliferation and apoptosis in mice uterus during estrous cycle. J. Steroid. Biochem. Mol. Biol. 2019, 185, 225–236. [Google Scholar] [CrossRef]
- Chang, W.T.; Hsieh, B.S.; Cheng, H.L.; Lee, K.T.; Chang, K.L. Progesterone augments epirubicin-induced apoptosis in HA22T/VGH cells by increasing oxidative stress and upregulating Fas/FasL. J. Surg. Res. 2014, 188, 432–441. [Google Scholar] [CrossRef]
- Wu, N.Y.; Huang, H.S.; Chao, T.H.; Chou, H.M.; Fang, C.; Qin, C.Z.; Lin, C.Y.; Chu, T.Y.; Zhou, H.H. Progesterone Prevents High-Grade Serous Ovarian Cancer by Inducing Necroptosis of p53-Defective Fallopian Tube Epithelial Cells. Cell Rep. 2017, 18, 2557–2565. [Google Scholar] [CrossRef]
- Feng, Z.; Marti, A.; Jehn, B.; Altermatt, H.J.; Chicaiza, G.; Jaggi, R. Glucocorticoid and progesterone inhibit involution and programmed cell death in the mouse mammary gland. J. Cell Biol. 1995, 131, 1095–1103. [Google Scholar] [CrossRef]
- Wang, Y.; Abrahams, V.M.; Luo, G.; Norwitz, N.G.; Snegovskikh, V.V.; Ng, S.W.; Norwitz, E.R. Progesterone Inhibits Apoptosis in Fetal Membranes by Altering Expression of Both Pro- and Antiapoptotic Proteins. Reprod. Sci. 2018, 25, 1161–1167. [Google Scholar] [CrossRef] [PubMed]
- Rueda, B.R.; Hendry, I.R.; Hendry, I.W.; Stormshak, F.; Slayden, O.D.; Davis, J.S. Decreased progesterone levels and progesterone receptor antagonists promote apoptotic cell death in bovine luteal cells. Biol. Reprod. 2000, 62, 269–276. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Makrigiannakis, A.; Coukos, G.; Christofidou-Solomidou, M.; Montas, S.; Coutifaris, C. Progesterone is an autocrine/paracrine regulator of human granulosa cell survival in vitro. Ann. N. Y. Acad. Sci. 2000, 900, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Friberg, P.A.; Larsson, D.G.; Billig, H. Dominant role of nuclear progesterone receptor in the control of rat periovulatory granulosa cell apoptosis. Biol. Reprod. 2009, 80, 1160–1167. [Google Scholar] [CrossRef] [PubMed]
- Glister, C.; Tannetta, D.S.; Groome, N.P.; Knight, P.G. Interactions between follicle-stimulating hormone and growth factors in modulating secretion of steroids and inhibin-related peptides by nonluteinized bovine granulosa cells. Biol. Reprod. 2001, 65, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Otala, M.; Mäkinen, S.; Tuuri, T.; Sjöberg, J.; Pentikäinen, V.; Matikainen, T.; Dunkel, L. Effects of testosterone, dihydrotestosterone, and 17beta-estradiol on human ovarian tissue survival in culture. Fertil. Steril. 2004, 82, 1077–1085. [Google Scholar] [CrossRef]
- Chou, C.H.; Chen, M.J. The Effect of Steroid Hormones on Ovarian Follicle Development. Vitam. Horm. 2018, 107, 155–175. [Google Scholar] [PubMed]
- Kim, J.W.; Havelock, J.C.; Carr, B.R.; Attia, G.R. The orphan nuclear receptor, liver receptor homolog-1, regulates cholesterol side-chain cleavage cytochrome p450 enzyme in human granulosa cells. J. Clin. Endocrinol. Metab. 2005, 90, 1678–1685. [Google Scholar] [CrossRef] [PubMed]
- Peng, N.; Kim, J.W.; Rainey, W.E.; Carr, B.R.; Attia, G.R. The role of the orphan nuclear receptor, liver receptor homologue-1, in the regulation of human corpus luteum 3beta-hydroxysteroid dehydrogenase type II. J. Clin. Endocrinol. Metab. 2003, 88, 6020–6028. [Google Scholar] [CrossRef]
- Yazawa, T.; Inanoka, Y.; Mizutani, T.; Kuribayashi, M.; Umezawa, A.; Miyamoto, K. Liver receptor homolog-1 regulates the transcription of steroidogenic enzymes and induces the differentiation of mesenchymal stem cells into steroidogenic cells. Endocrinology 2009, 150, 3885–3893. [Google Scholar] [CrossRef]
- Lee, Y.K.; Moore, D.D. Liver receptor homolog-1, an emerging metabolic modulator. Front. Biosci. 2008, 13, 5950–5958. [Google Scholar] [CrossRef]
- Hinshelwood, M.M.; Repa, J.J.; Shelton, J.M.; Richardson, J.A.; Mangelsdorf, D.J.; Mendelson, C.R. Expression of LRH-1 and SF-1 in the mouse ovary: Localization in different cell types correlates with differing function. Mol. Cell Endocrinol. 2003, 207, 39–45. [Google Scholar] [CrossRef]
- Hammes, S.R.; Levin, E.R. Extranuclear steroid receptors: Nature and actions. Endocr. Rev. 2007, 28, 726–741. [Google Scholar] [CrossRef] [PubMed]
- Svensson, E.C.; Markström, E.; Andersson, M.; Billig, H. Progesterone receptor-mediated inhibition of apoptosis in granulosa cells isolated from rats treated with human chorionic gonadotropin. Biol. Reprod. 2000, 63, 1457–1464. [Google Scholar] [CrossRef] [PubMed]
- Quirk, S.M.; Cowan, R.G.; Harman, R.M. Progesterone receptor and the cell cycle modulate apoptosis in granulosa cells. Endocrinology 2004, 145, 5033–5043. [Google Scholar] [CrossRef] [PubMed]
- Falender, A.E.; Lanz, R.; Malenfant, D.; Belanger, L.; Richards, J.S. Differential expression of steroidogenic factor-1 and FTF/LRH-1 in the rodent ovary. Endocrinology 2003, 144, 3598–3610. [Google Scholar] [CrossRef]
- Wu, C.; Feng, J.; Li, L.; Wu, Y.; Xie, H.; Yin, Y.; Ye, J.; Li, Z. Liver receptor homologue 1, a novel prognostic marker in colon cancer patients. Oncol. Lett. 2018, 16, 2833–2838. [Google Scholar] [CrossRef] [PubMed]
| Gene Name | Primer Sequences (5′–3′) | GenBank Accession No. |
|---|---|---|
| LRH-1 | F: TCTTTGAACACCACCCAATACCA | XM_015470800.1 |
| R: ATCTGCTGGTCGGAAAGGC | ||
| PGR | F: TCCCCCCACTGATCAACTTG | NM_001205356.1 |
| R: TCCGAAAACCTGGCAGTGA | ||
| β-actin | F: TCACCAACTGGGACGACA | NM_173979.3 |
| R: GCATACAGGGACAGCACA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, D.; Jiang, X.; Wang, Y.; Song, S. Liver Receptor homolog-1 Regulates Apoptosis of Bovine Ovarian Granulosa Cells by Progestogen Receptor Signaling Pathway. Animals 2022, 12, 1213. https://doi.org/10.3390/ani12091213
Xu D, Jiang X, Wang Y, Song S. Liver Receptor homolog-1 Regulates Apoptosis of Bovine Ovarian Granulosa Cells by Progestogen Receptor Signaling Pathway. Animals. 2022; 12(9):1213. https://doi.org/10.3390/ani12091213
Chicago/Turabian StyleXu, Dejun, Xiaohan Jiang, Yukun Wang, and Shuaifei Song. 2022. "Liver Receptor homolog-1 Regulates Apoptosis of Bovine Ovarian Granulosa Cells by Progestogen Receptor Signaling Pathway" Animals 12, no. 9: 1213. https://doi.org/10.3390/ani12091213
APA StyleXu, D., Jiang, X., Wang, Y., & Song, S. (2022). Liver Receptor homolog-1 Regulates Apoptosis of Bovine Ovarian Granulosa Cells by Progestogen Receptor Signaling Pathway. Animals, 12(9), 1213. https://doi.org/10.3390/ani12091213






