Milk Lactose as a Biomarker of Subclinical Mastitis in Dairy Cows
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Location, Animals and Experimental Design
2.2. Measurements
2.3. Data Analysis and Statistics
3. Results
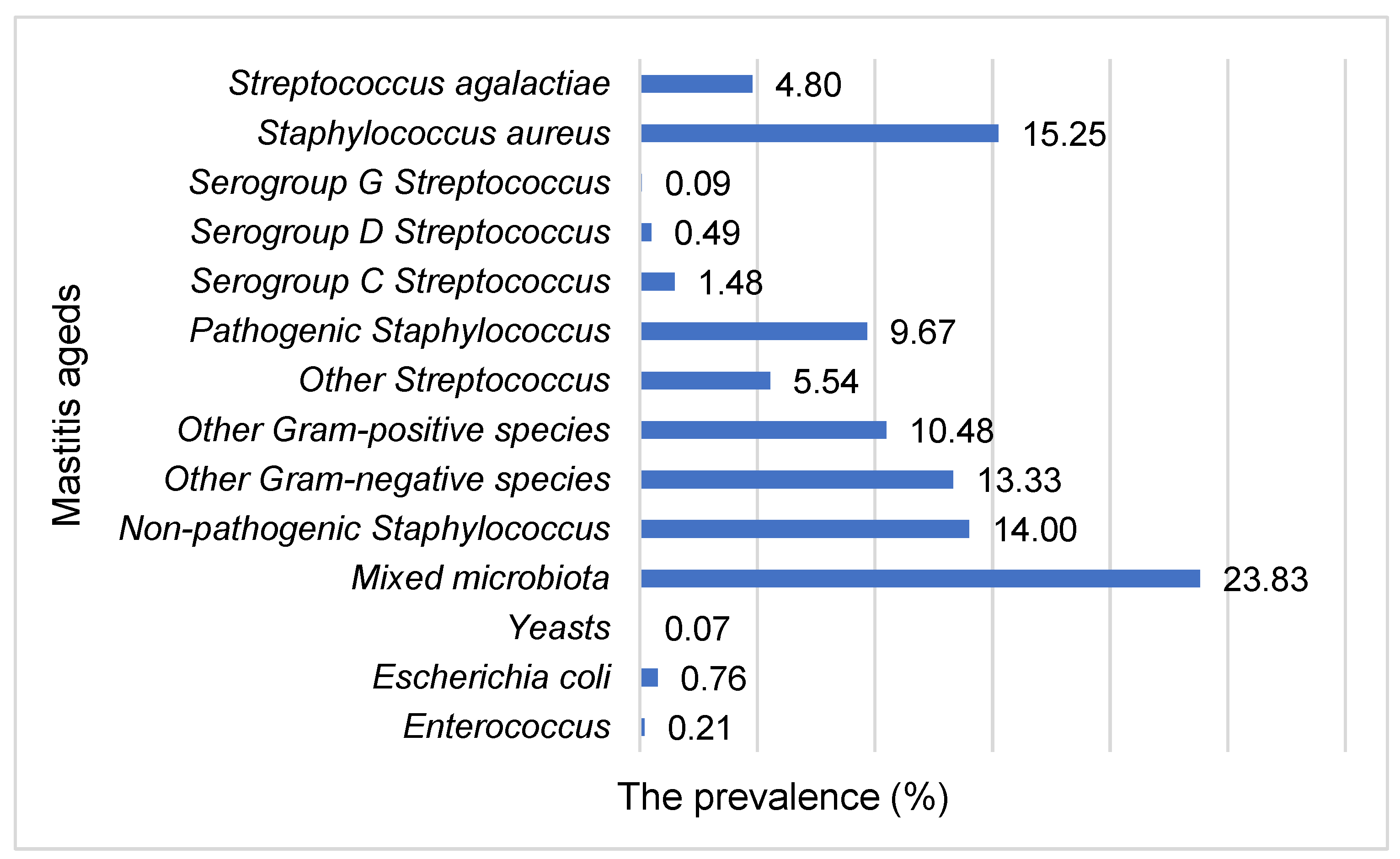
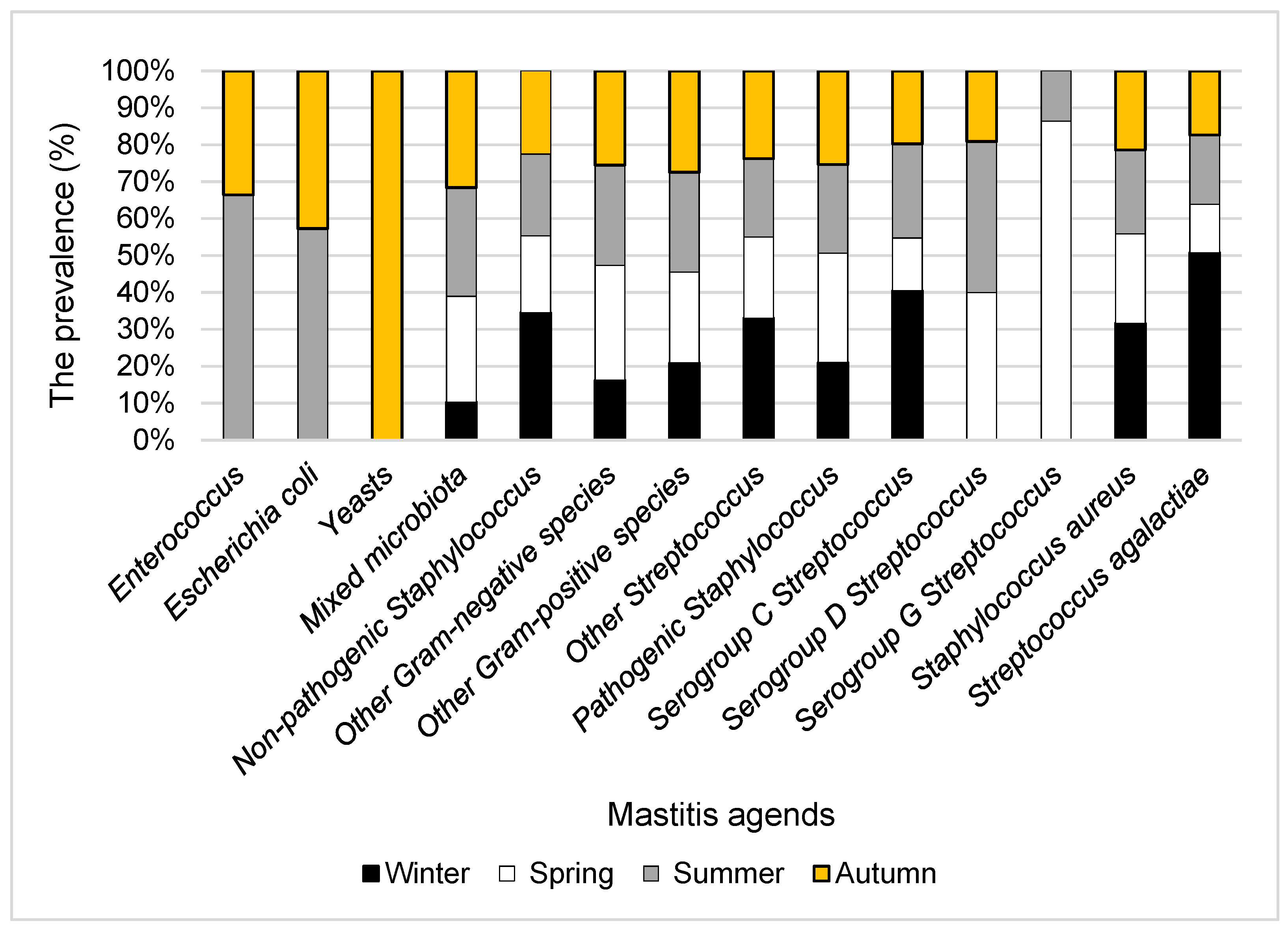
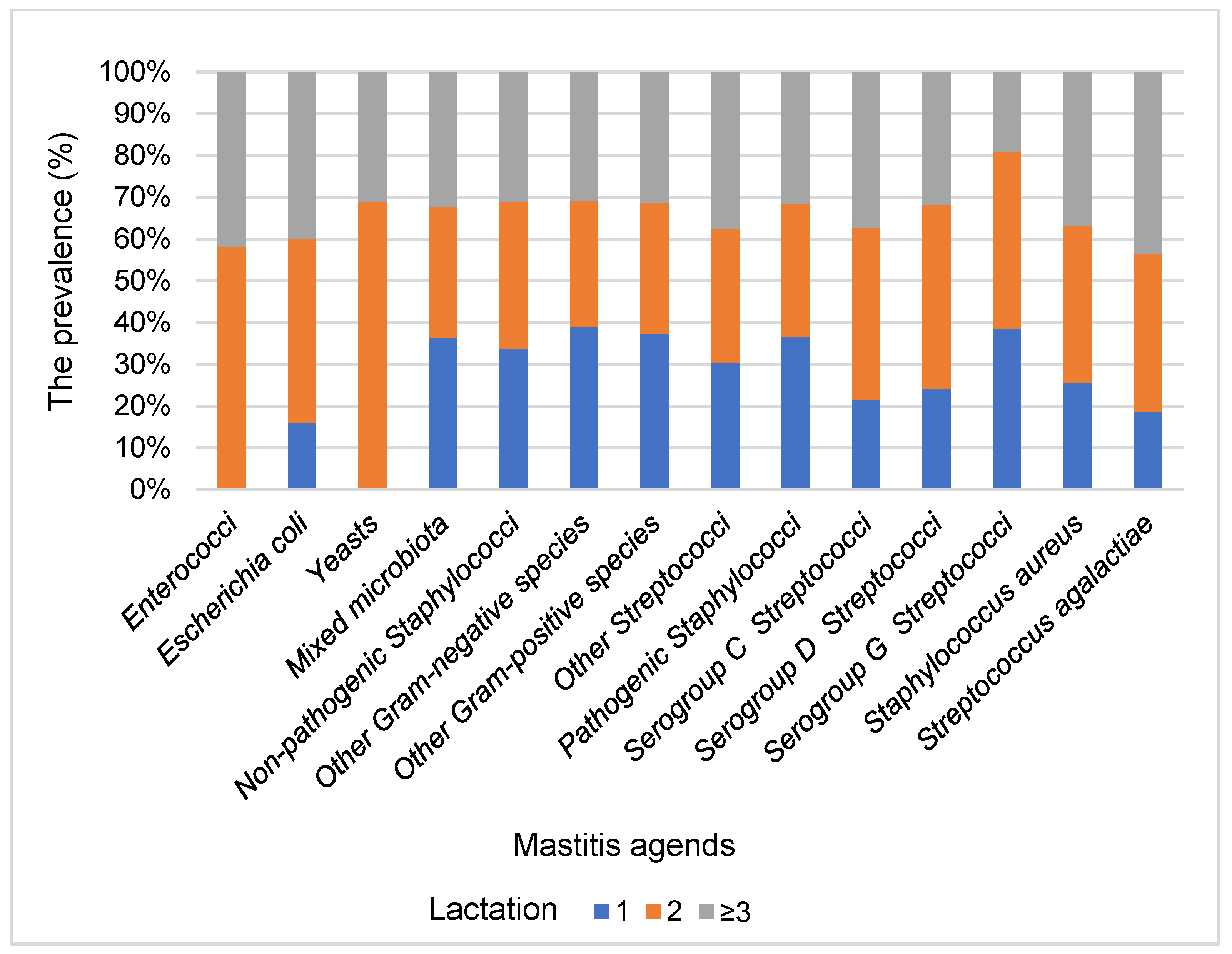
3.1. The Prevalence of Subclinical Mastitis Pathogens Isolated from the Mammary Glands of Cows
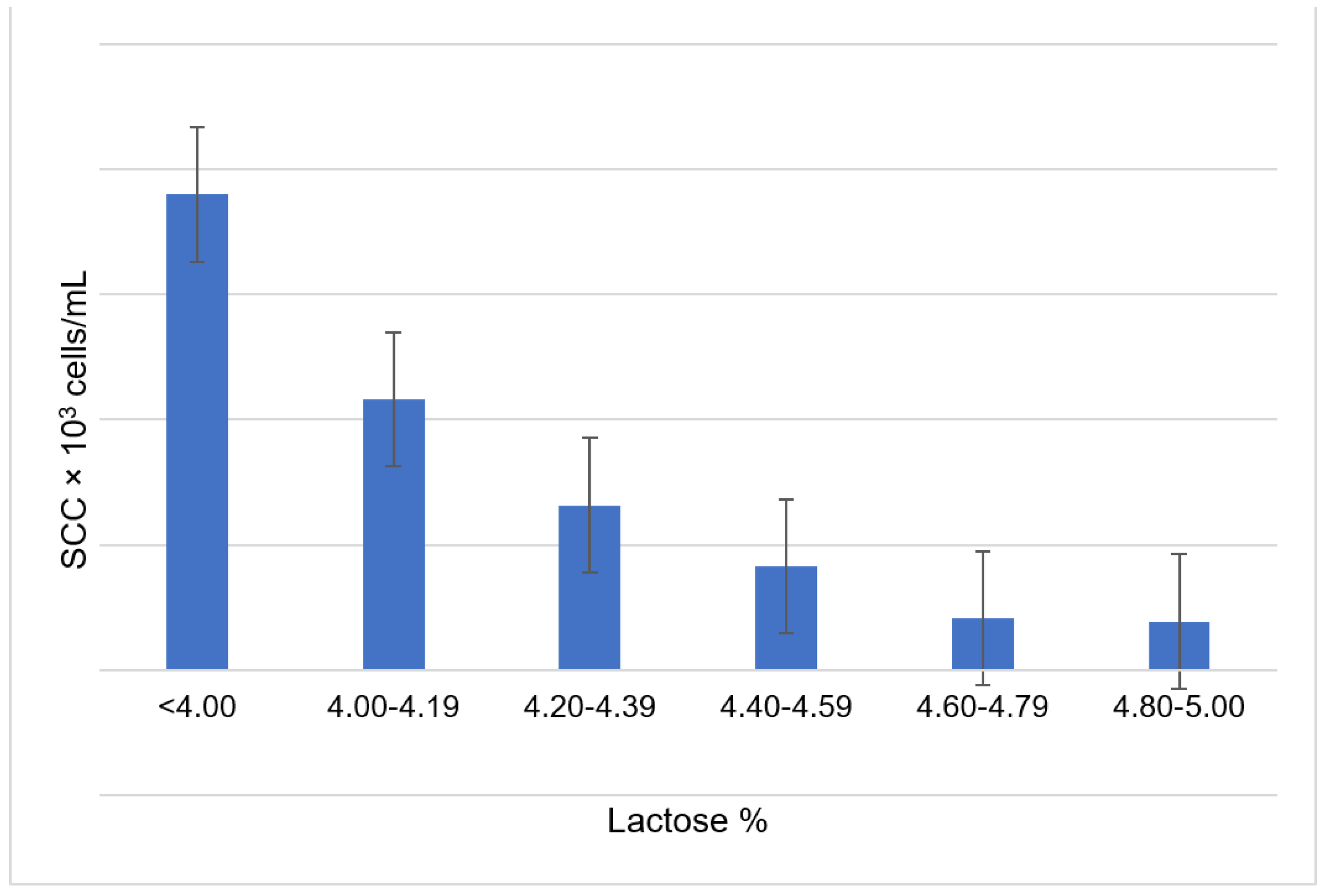
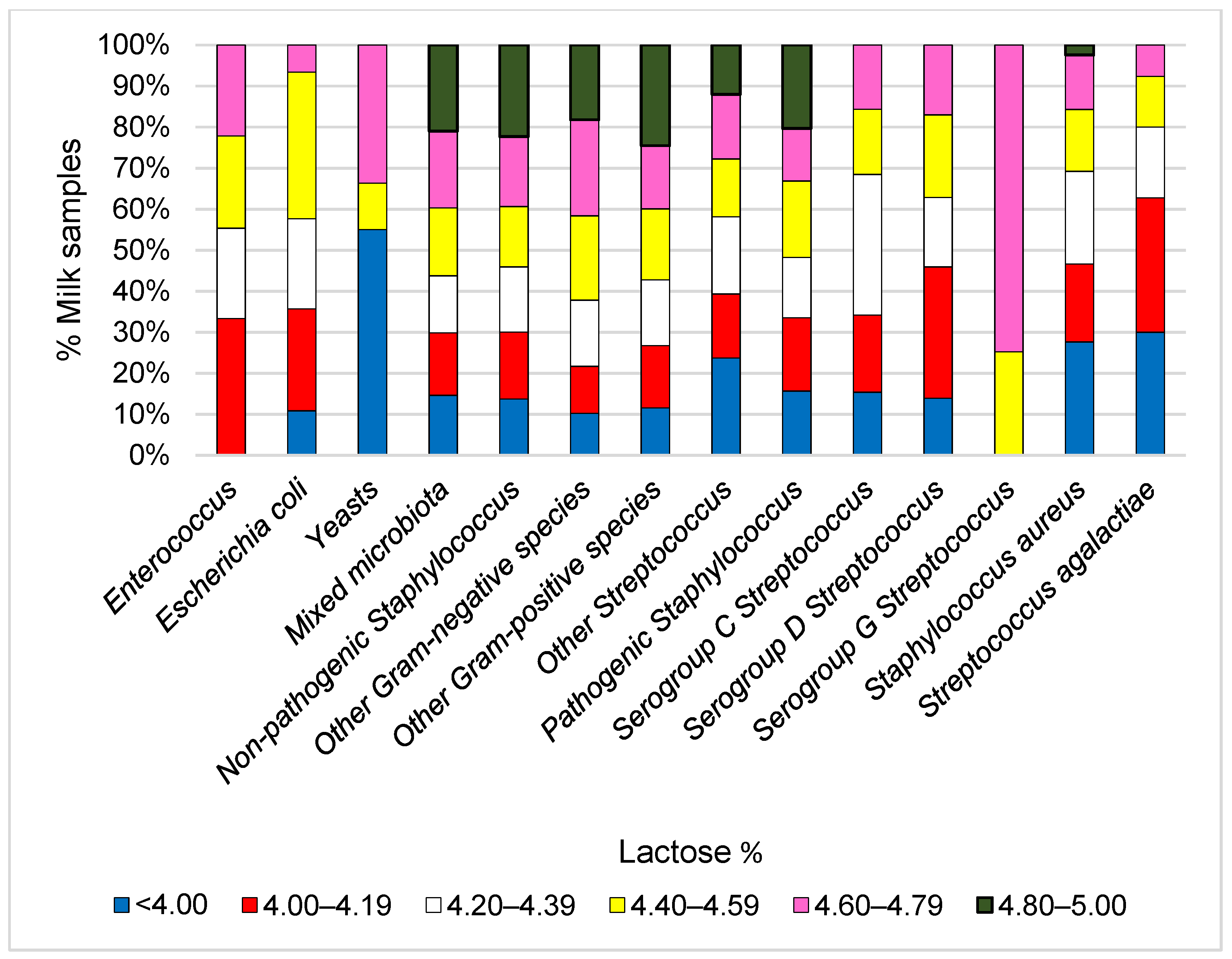
3.2. Relationship between Milk Lactose and the Prevalence of Subclinical Mastitis Pathogens and Somatic Cell Count in Cow’s Milk
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gomes, F.; Saavedra, M.J.; Henriques, M. Bovine mastitis disease/pathogenicity: Evidence of the potential role of microbial biofilms. Pathog. Dis. 2016, 74. [Google Scholar] [CrossRef]
- Lundberg, Å. Mastitis in Dairy Cows; Uppsala University: Uppsala, Sweden, 2015. [Google Scholar]
- Hogan, J.S.; Martin, M. Current Concepts of Bovine Mastitis; The National Mastitis Council: New Prague, MN, USA, 2016. [Google Scholar]
- Halasa, T.; Huijps, K.; Østerås, O.; Hogeveen, H. Economic effects of bovine mastitis and mastitis management: A review. Vet. Q. 2007, 29, 18–31. [Google Scholar] [CrossRef]
- Zadoks, R.N.; Middleton, J.R.; McDougall, S.; Katholm, J.; Schukken, Y.H. Molecular epidemiology of mastitis pathogens of dairy cattle and comparative relevance to humans. J. Mammary Gland Biol. Neoplasia 2011, 16, 357–372. [Google Scholar] [CrossRef]
- Jansen, J.; Wessels, R.J.; Lam, T.J.G.M. January. Understanding the mastitis mindset: Applying social psychology in practice. In Proceedings of the National Mastitis Council 55th Annual Meeting, Glendale, AZ, USA, 31 January–2 February 2016; pp. 5–15. [Google Scholar]
- Carrillo-Casas, E.M.; Miranda-Morales, R.E. Bovine mastitis pathogens: Prevalence and effects on somatic cell count. In Milk Production—An up-to-Date Overview of Animal Nutrition, Management and Health; Intech Open: London, UK, 2012. [Google Scholar]
- Hameed, K.G.A.; Sender, G.; Korwin-Kossakowska, A. Public health hazard due to mastitis in dairy cows. Anim. Sci. Pap. Rep. 2007, 25, 73–85. [Google Scholar]
- Ashraf, A.; Imran, M. Causes, types, etiological agents, prevalence, diagnosis, treatment, prevention, effects on human health and future aspects of bovine mastitis. Anim. Health Res. Rev. 2020, 21, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Miglior, F.; Sewalem, A.; Jamprozik, J.; Bohmanova, J.; Lefebvre, D.M.; Moore, R.K. Genetic analysis of milk urea nitrogen and lactose and their relationships with other production traits in Canadian Holstein cattle. J. Dairy Sci. 2007, 90, 2468–2479. [Google Scholar] [CrossRef]
- Moussaoui, F.; Vangroenweghe, F.; Haddadi, K.; Le Roux, Y.; Laurent, F.; Duchateau, L.; Burvenich, C. Proteolysis in milk during experimental Escherichia coli mastitis. J. Dairy Sci. 2004, 87, 2923–2931. [Google Scholar] [CrossRef]
- Chedly, H.B.; Lacasse, P.; Marnet, P.G.; Wiart-Letort, S.; Finot, L.; Boutinaud, M. Cell junction disruption after 36h milk accumulation was associated with changes in mammary secretory tissue activity and dynamics in lactating dairy goats. J. Physiol. Pharmacol. 2009, 60 (Suppl. S3), 105–111. [Google Scholar] [PubMed]
- Pessora, R.B.; Blagitz, M.G.; Batista, C.F.; Santos, B.P.; Parra, A.C.; Souza, F.N.; Della Libera, A.M.M.P. Avaliação da apoptose de leucócitos polimorfonucleares CH138+ em leite bovino de alta e baixa contagem de células somáticas dados preliminares. Arq. Bras. Med. Vet. Zootec. 2012, 64, 533–539. [Google Scholar] [CrossRef]
- Berglund, I.; Pettersson, G.; Östensson, K.; Svennersten-Sjaunja, K. Quarter milking for improved detection of increased SCC. Reprod. Domest. Anim. 2007, 42, 427–432. [Google Scholar] [CrossRef]
- Pollott, G.E. Deconstructing milk yield and composition during lactation using biologically based lactation models. J. Dairy Sci. 2004, 87, 2375–2387. [Google Scholar] [CrossRef]
- Lemosquet, S.; Delamaire, E.; Lapierre, H.; Blum, J.W.; Peyraud, J.L. Effects of glucose, propionic acid, and nonessential amino acids on glucose metabolism and milk yield in Holstein dairy cows. J. Dairy Sci. 2009, 92, 3244–3257. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.; Lopez-Villalobos, N.; Sneddon, N.W.; Shalloo, L.; Franzoi, M.; De Marchi, M.; Penasa, M. Invited review: Milk lactose—Current status and future challenges in dairy cattle. J. Dairy Sci. 2019, 102, 5883–5898. [Google Scholar] [CrossRef] [PubMed]
- Valde, J.P.; Hird, D.W.; Thurmond, M.C.; Østerås, O. Comparison of ketosis, clinical mastitis, somatic cell count, and reproductive performance between free stall and tie stall barns in Norwegian dairy herds with automatic feeding. Acta Vet. Scand. 1997, 38, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Washburn, S.P.; White, S.L.; Green, J.T., Jr.; Benson, G.A. Reproduction, mastitis, and body condition of seasonally calved Holstein and Jersey cows in confinement or pasture systems. J. Dairy Sci. 2002, 85, 105–111. [Google Scholar] [CrossRef]
- Ferrari, F.; Cocconi, D.; Bettini, R.; Giordano, F.; Santi, P.; Tobyn, M.; Price, R.; Young, P.; Caramella, C.; Colombo, P. The surface roughness of lactose particles can be modulated by wet-smoothing using a high-shear mixer. AAPS PharmSciTech 2004, 5, 69–74. [Google Scholar] [CrossRef]
- Televičius, M.; Juozaitiene, V.; Malašauskienė, D.; Antanaitis, R.; Rutkauskas, A.; Urbutis, M.; Baumgartner, W. Inline Milk Lactose Concentration as Biomarker of the Health Status and Reproductive Success in Dairy Cows. Agriculture 2021, 11, 38. [Google Scholar] [CrossRef]
- National Mastitis Council. The Guide to Bovine Mastitis Issues in the Laboratory and in Field; The National Mastitis Council: New Prague, MN, USA, 1987. [Google Scholar]
- Ali, A.K.A.; Shook, G.E. An optimum transformation for somatic cell concentration in milk. J. Dairy Sci. 1980, 63, 487–490. [Google Scholar] [CrossRef]
- Argaw, A. Review on epidemiology of clinical and subclinical mastitis on dairy cows. Food Sci. Qual. Manag. 2016, 52, 56–65. [Google Scholar]
- Cobirka, M.; Tancin, V.; Slama, P. Epidemiology and Classification of Mastitis. Animals 2020, 10, 2212. [Google Scholar] [CrossRef]
- Klimienė, I.; Mockeliūnas, R.; Butrimaitė-Ambrozevičienė, Č.; Sakalauskienė, R. The distribution of dairy cow mastitis in Lithuania. Vet. Zootech. 2005, 31, 67–76. [Google Scholar]
- Čereškienė, E.; Juozaitienė, V.; Juozaitis, A.; Černauskienė, J.; Žymantienė, J.; Kantautaitė, J. Influence of mastitis agents on milk traits of cows. Vet. Zootech. 2016, 73, 24–27. [Google Scholar]
- Haltia, L.; Honkanen-Buzalski, T.; Spiridonova, I.; Olkonen, A.; Myllys, V. A study of bovine mastitis, milking procedures and management practices on 25 Estonian dairy herds. Acta Vet. Scand. 2006, 48, 22. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jemeljanovs, A.; Konosonoka, I.H.; Bluzmanis, J.; Ikauniece, D. Changes of mastitis pathogen spectrum in dairy herds of Latvia. In Mastitis Control–From Science to Practice; Wageningen Academic Publishers: Hague, The Netherlands, 2008; p. 83. [Google Scholar]
- Vitali, A.; Bernabucci, U.; Nardone, A.; Lacetera, N. Effect of season, month and temperature humidity index on the occurrence of clinical mastitis in dairy heifers. Adv. Anim. Vet. Sci. 2016, 7, 250. [Google Scholar] [CrossRef]
- Tarazona-Manrique, L.E.; Villate-Hernández, J.R.; Andrade-Becerra, R.J. Bacterial and fungal infectious etiology causing mastitis in dairy cows in the highlands of Boyacá (Colombia). Rev. Med. Vet. 2019, 66, 208–218. [Google Scholar] [CrossRef]
- Doyle, C.J.; Gleeson, D.; O’Toole, P.W.; Cotter, P.D. Impacts of seasonal housing and teat preparation on raw milk microbiota: A high-throughput sequencing study. Appl. Environ. Microbiol. 2017, 83, e02694-16. [Google Scholar] [CrossRef]
- Senda, A.; Nakamura, T.; Urashima, T.; Arai, I. Seasonal incidences and populations of yeast in a high-quality raw milk. Anim. Sci. J. 2003, 74, 517–523. [Google Scholar]
- Ranjan, R.; Gupta, M.K.; Singh, K.K. Study of bovine mastitis in different climatic conditions in Jharkhand, India. Vet. World 2011, 4, 205–208. [Google Scholar] [CrossRef]
- Da Costa, G.M.; de Pádua Pereira, U.; Souza-Dias, M.A.G.; da Silva, N. Yeast mastitis outbreak in a Brazilian dairy herd. Braz. J. Vet. Res. Anim. Sci. 2012, 49, 239–243. [Google Scholar]
- Krukowski, H.; Lisowski, A. Occurrence of yeast mastitis in cows in relation to the type of dairy farm, system of milking and maintenance system of cows. Med. Weter. 2010, 66, 339–342. [Google Scholar]
- Keller, B.; Scheibl, P.; Bleckmann, E.; Hoedemaker, M. Differentiation of yeasts in mastitis milk. Mycoses 2000, 43, 17–19. [Google Scholar]
- Dworecka-Kaszak, B.; Krutkiewicz, A.; Szopa, D.; Kleczkowski, M.; Biegańska, M. High prevalence of Candida yeast in milk samples from cows suffering from mastitis in Poland. Sci. World J. 2012, 2012, 196347. [Google Scholar] [CrossRef] [PubMed]
- Masteikienė, R. Maisto produktų mikrobiologija; Technologija: Kaunas, Lithuania, 2006; p. 342. [Google Scholar]
- Zhang, D.; Zhang, Z.; Huang, C.; Gao, X.; Wang, Z.; Liu, Y.; Tian, C.; Hong, W.; Niu, S.; Liu, M. The phylogenetic group, antimicrobial susceptibility, and virulence genes of Escherichia coli from clinical bovine mastitis. J. Dairy Sci. 2017, 101, 572–580. [Google Scholar] [CrossRef]
- Petersson-Wolfe, C.S.; Wolf, S.L.; Hogan, J.S. Experimental challenge of bovine mammary glands with Enterococcus faecium during early and late lactation. J. Dairy Sci. 2009, 92, 3158–3164. [Google Scholar] [CrossRef]
- Reist, M.; Erdin, D.; Von Euw, D.; Tschuemperlin, K.; Leuenberger, H.; Chilliard, Y.; Hammon, H.M.; Morel, C.; Philipona, C.; Zbinden, Y.; et al. Estimation of energy balance at the individual and herd level using blood and milk traits in high-yielding dairy cows. J. Dairy Sci. 2002, 85, 3314–3327. [Google Scholar] [CrossRef]
- Pyörälä, S. Indicators of inflammation in the diagnosis of mastitis. Vet. Res. 2003, 34, 565–578. [Google Scholar] [CrossRef] [PubMed]
- Forsbäck, L.; Lindmark-Månsson, H.; Andrén, A.; Åkerstedt, M.; Andrée, L.; Svennersten-Sjaunja, K. Day-to-day variation in milk yield and milk composition at the udder-quarter level. J. Dairy Sci. 2010, 93, 3569–3577. [Google Scholar] [CrossRef]
- Gillon, A.; Bastin, C.; Soyeurt, H.; Gengler, N. Genetic parameters of mastitis-correlated milk components in first parity dairy cows. In Proceedings of the 9th World Congress on Genetics Applied to Livestock Production; German Society for Animal Science: Bonn, Germany, 2010; Available online: https://orbi.uliege.be/bitstream/2268/69462/1/GILLON_full_paper.pdf (accessed on 12 April 2021).
- Haile-Mariam, M.; Pryce, J.E. Genetic parameters for lactose and its correlation with other milk production traits and fitness traits in pasture-based production systems. J. Dairy Sci. 2017, 100, 3754–3766. [Google Scholar] [CrossRef]
- Ptak, E.; Brzozowski, P.; Bieniek, J. Genetic parameters for lactose percentage in the milk of Polish Holstein-Friesians. J. Anim. Feed Sci. 2012, 21, 251–262. [Google Scholar] [CrossRef]
- Noro, G.; González, F.H.D.; Campos, R.; Dürr, J.W. Fatores ambientais que afetam a produção e a composição do leite emrebanhos assistidos por cooperativas no Rio Grande do Sul. Rev. Bras. Zootec. 2006, 5, 1129–1135. [Google Scholar] [CrossRef]
- Zanela, M.B.; Fischer, V.; Ribeiro, M.E.R.; Stumpf Junior, W.; Zanela, C.; Marques, L.T.; Martins, P.R.G. Qualidade do leite em sistemas de produção na região Sul do Rio Grande do Sul. Pesqui Agropecu Bras. 2006, 41, 153–159. [Google Scholar] [CrossRef][Green Version]
- Shimkiene, A.; Juozaitiene, V.; Juozaitis, A.; Shimkus, A.; Zilaitis, V.; Urbonavicius, A. Relationship between lactose content in cow’s milk with selection attributes and heritability. Vet. Med. Zoot. 2009, 45, 81–86. [Google Scholar]
- Bobbo, T.; Ruegg, P.L.; Stocco, G.; Fiore, E.; Gianesella, M.; Morgante, M.; Pasotto, D.; Bittante, G.; Cecchinato, A. Associations between pathogen-specific cases of subclinical mastitis and milk yield, quality, protein composition, and cheese-making traits in dairy cows. J. Dairy Sci. 2017, 100, 4868–4883. [Google Scholar] [CrossRef] [PubMed]
- Coulona, J.B.; Gasquib, P.; Barnouin, J.; Ollier, A.; Pradel, P.; Pomiès, D. Effect of mastitis and related-germ on milk yield and composition during naturally-occurring udder infections in dairy cows. Anim. Res. 2002, 51, 383–393. [Google Scholar] [CrossRef]
- Kayano, M.; Itoh, M.; Kusaba, N.; Hayashiguchi, O.; Kida, K.; Tanaka, Y.; Kawamoto, K.; Gröhn, Y.T. Associations of the first occurrence of pathogen-specific clinical mastitis with milk yield and milk composition in dairy cows. J. Dairy Res. 2018, 85, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Ianieva, O.D.; Voronina, G.O.; Pidgorskyi, V.S. Isolation and characteristics of the lactose-fermenting yeasts Candida kefyr. Cytol. Genet. 2013, 47, 359–365. [Google Scholar] [CrossRef]
| Item | Pathogens | Lactose % | 95% CI | ||
|---|---|---|---|---|---|
| M | SEM | Lower Bound | Upper Bound | ||
| 1 | Enterococcus spp. | 4.37 13 | 0.079 | 4.214 | 4.523 |
| 2 | Escherichia coli | 4.36 | 0.041 | 4.284 | 4.445 |
| 3 | Yeasts | 4.32 | 0.137 | 4.056 | 4.591 |
| 4 | Mixed microbiota | 4.36 6,8,13,14 | 0.007 | 4.349 | 4.378 |
| 5 | Non-pathogenic Staphylococcus | 4.35 6 | 0.01 | 4.33 | 4.368 |
| 6 | Other Gram-negative species | 4.40 4,5,10,13,14 | 0.01 | 4.379 | 4.417 |
| 7 | Other Gram-positive species | 4.36 13,14 | 0.011 | 4.337 | 4.381 |
| 8 | Other Streptococcus | 4.32 4,14 | 0.015 | 4.293 | 4.353 |
| 9 | Pathogenic Staphylococcus | 4.35 13,14 | 0.012 | 4.325 | 4.37 |
| 10 | Serogroup C Streptococcus | 4.31 6,14 | 0.03 | 4.255 | 4.371 |
| 11 | Serogroup D Streptococcus | 4.33 | 0.052 | 4.23 | 4.433 |
| 12 | Serogroup G Streptococcus | 4.55 13,14 | 0.118 | 4.313 | 4.777 |
| 13 | Staphylococcus aureus | 4.30 4,5,6,7,9,14 | 0.009 | 4.282 | 4.318 |
| 14 | Streptococcus agalactiae | 4.25 1,4,5,6,7,8,9,12,14 | 0.016 | 4.215 | 4.279 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antanaitis, R.; Juozaitienė, V.; Jonike, V.; Baumgartner, W.; Paulauskas, A. Milk Lactose as a Biomarker of Subclinical Mastitis in Dairy Cows. Animals 2021, 11, 1736. https://doi.org/10.3390/ani11061736
Antanaitis R, Juozaitienė V, Jonike V, Baumgartner W, Paulauskas A. Milk Lactose as a Biomarker of Subclinical Mastitis in Dairy Cows. Animals. 2021; 11(6):1736. https://doi.org/10.3390/ani11061736
Chicago/Turabian StyleAntanaitis, Ramūnas, Vida Juozaitienė, Vesta Jonike, Walter Baumgartner, and Algimantas Paulauskas. 2021. "Milk Lactose as a Biomarker of Subclinical Mastitis in Dairy Cows" Animals 11, no. 6: 1736. https://doi.org/10.3390/ani11061736
APA StyleAntanaitis, R., Juozaitienė, V., Jonike, V., Baumgartner, W., & Paulauskas, A. (2021). Milk Lactose as a Biomarker of Subclinical Mastitis in Dairy Cows. Animals, 11(6), 1736. https://doi.org/10.3390/ani11061736







