Equine Rehabilitation: A Scoping Review of the Literature
Abstract
Simple Summary
Abstract
1. Introduction
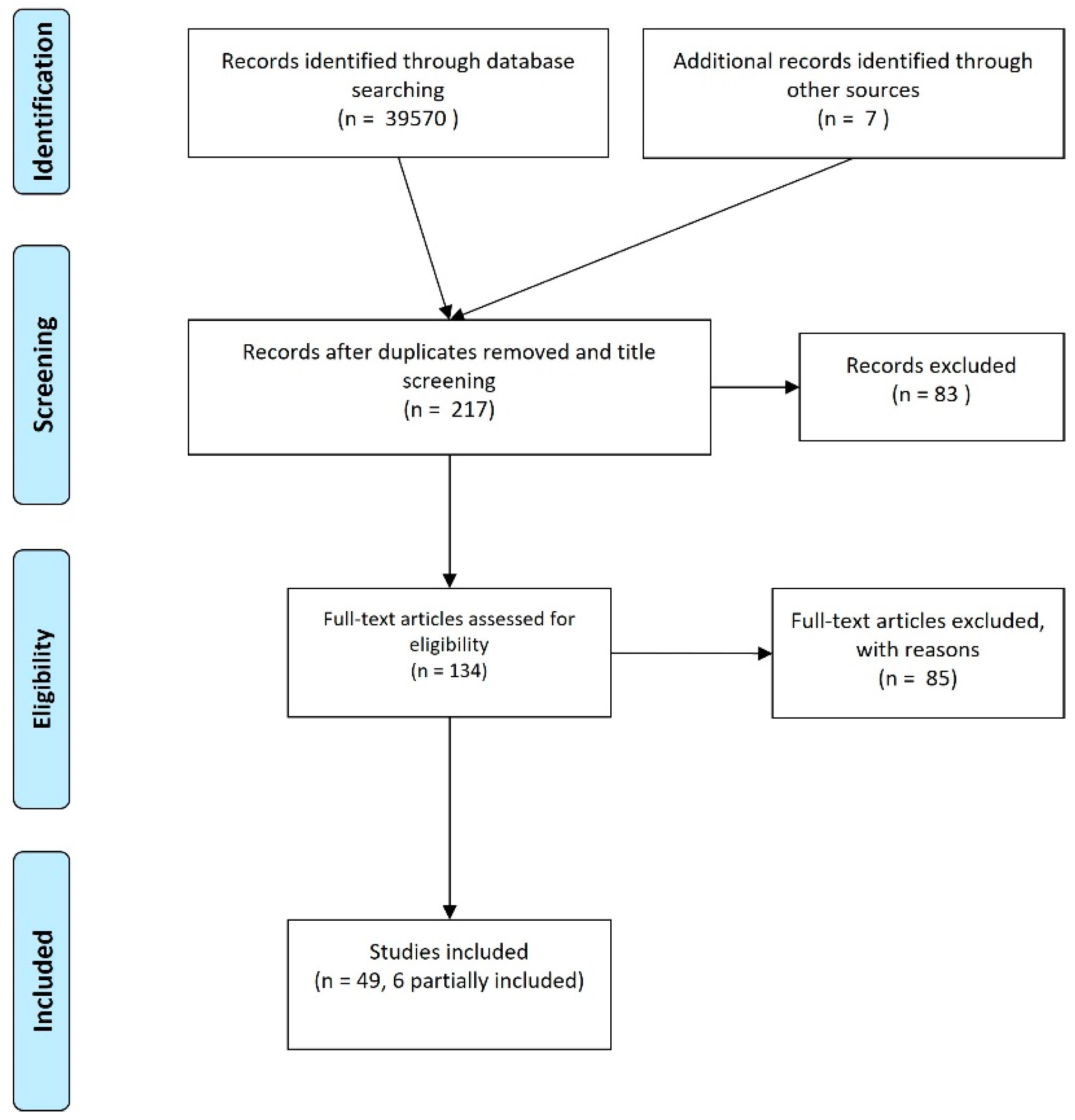
2. Materials and Methods
2.1. Identifying the Research Question
2.2. Identifying Relevant Studies
2.2.1. Electronic Databases
2.2.2. Reference Lists
2.2.3. Manual Search of Other Sources
2.3. Study Selection
2.3.1. Inclusion Criteria
2.3.2. Exclusion Criteria
2.4. Charting the Data
- Manuscript authors and date
- Type of intervention and comparator (if applicable)
- Populations
- Aims
- Methods
2.5. Collating, Summarizing, and Reporting Data
3. Results and Discussion
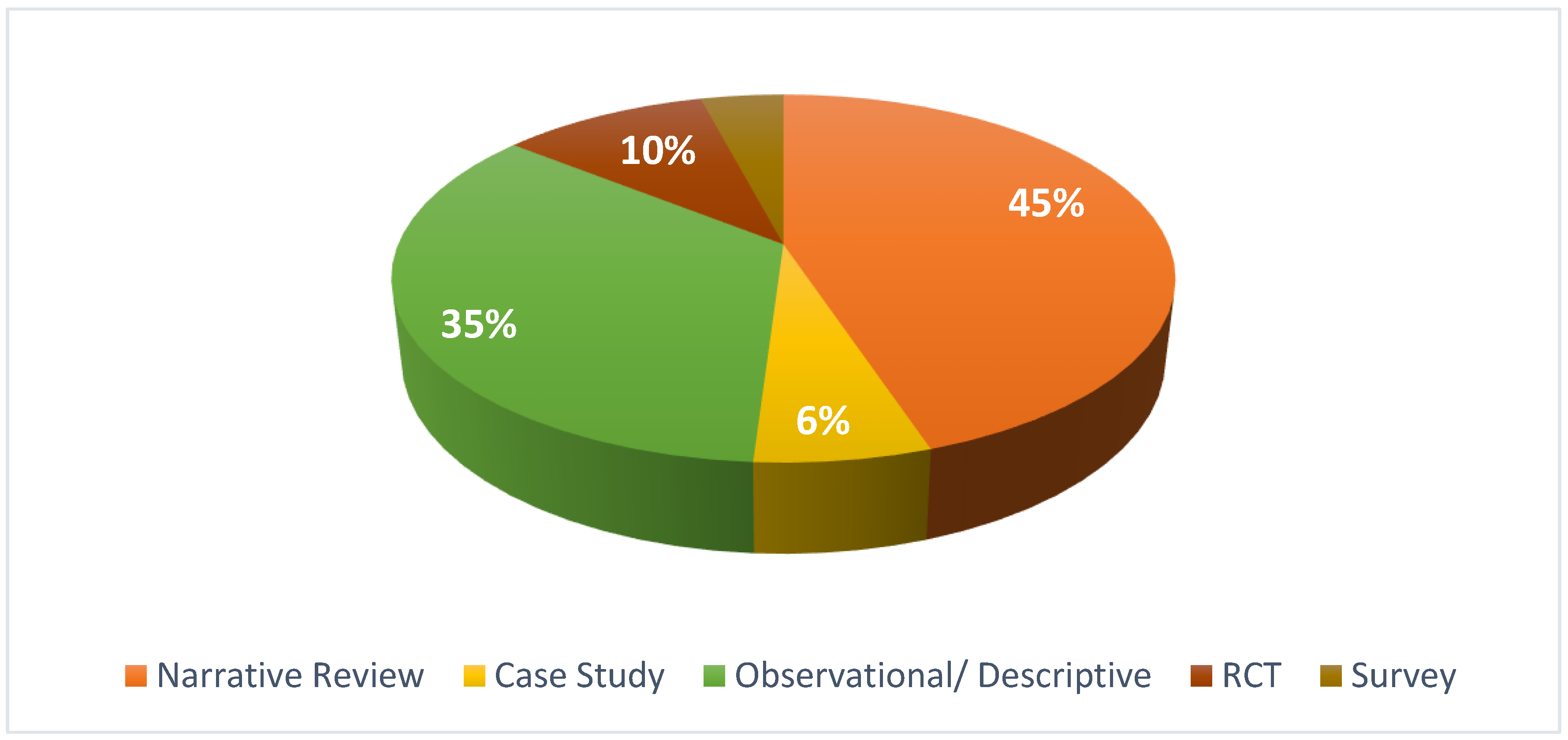
3.1. Type of Studies
3.2. Manual Therapy-Based Interventions
3.2.1. Passive Stretching
3.2.2. Tissue Mobilization
3.2.3. Joint Mobilization
3.3. Physical and Mechanical Agents
3.3.1. Kinesiological Taping and Bandages
3.3.2. Electrotherapy Interventions
Magnetic Field Therapy
Radial Pressure Wave Therapy
Extracorporeal Shock Wave Therapy (ESWT)
Therapeutic Ultrasound
Laser Therapy
Whole Body Vibration
3.3.3. Thermal Therapy
3.3.4. Hydrotherapy
3.4. Exercise Therapy
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Rehabilitation in Health Systems. In WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Evans, R. Merriam-Webster’s medical dictionary app. Nurs. Stand. 2014, 29, 33. [Google Scholar] [CrossRef] [PubMed]
- Kaneps, A.J. Practical Rehabilitation and Physical Therapy for the General Equine Practitioner. Vet. Clin. N. Am. Equine Pract. 2016, 32, 167–180. [Google Scholar] [CrossRef] [PubMed]
- McGowan, C.M.; Cottriall, S. Introduction to Equine Physical Therapy and Rehabilitation. Vet. Clin. N. Am. Equine Pract. 2016, 32, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Bromiley, M.W. Physical Therapy for the Equine Back. Vet. Clin. N. Am. Equine Pract. 1999, 15, 223–246. [Google Scholar] [CrossRef]
- Ridgway, K.; Harman, J. Equine Back Rehabilitation. Vet. Clin. N. Am. Equine Pract. 1999, 15, 263–280. [Google Scholar] [CrossRef]
- Blackford, J.; Doherty, T.J.; Ferslew, K.E.; Panus, P.C. Iontophoresis of dexamethasone-phosphate into the equine tibiotarsal joint. J. Vet. Pharmacol. Ther. 2000, 23, 229–236. [Google Scholar] [CrossRef]
- Arnold, C.E.; Schaer, T.P.; Baird, D.L.; Martin, B.B. Conservative management of 17 horses with nonarticular fractures of the tibial tuberosity. Equine Vet. J. 2003, 35, 202–206. [Google Scholar] [CrossRef]
- Crowe, O.M.; Dyson, S.J.; Wright, I.M.; Schramme, M.C.; Smith, R.K.W. Treatment of chronic or recurrent proximal suspensory desmitis using radial pressure wave therapy in the horse. Equine Vet. J. 2004, 36, 313–316. [Google Scholar] [CrossRef]
- Porter, M. Equine rehabilitation therapy for joint disease. Vet. Clin. N. Am. Equine Pract. 2005, 21, 599–607. [Google Scholar] [CrossRef]
- Buchner, H.H.F.; Schildboeck, U. Physiotherapy applied to the horse: A review. Equine Vet. J. 2006, 38, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Goff, L.M. Manual Therapy for the Horse—A Contemporary Perspective. J. Equine Vet. Sci. 2009, 29, 799–808. [Google Scholar] [CrossRef]
- Haussler, K.K. Review of Manual Therapy Techniques in Equine Practice. J. Equine Vet. Sci. 2009, 29, 849–869. [Google Scholar] [CrossRef]
- Paulekas, R.; Haussler, K.K. Principles and Practice of Therapeutic Exercise for Horses. J. Equine Vet. Sci. 2009, 29, 870–893. [Google Scholar] [CrossRef]
- Scott, M.; Swenson, L.A. Evaluating the Benefits of Equine Massage Therapy: A Review of the Evidence and Current Practices. J. Equine Vet. Sci. 2009, 29, 687–697. [Google Scholar] [CrossRef]
- Clayton, H.M.; Kaiser, L.J.; Lavagnino, M.; Stubbs, N.C. Dynamic mobilisations in cervical flexion: Effects on intervertebral angulations. Equine Vet. J. 2010, 42, 688–694. [Google Scholar] [CrossRef]
- Clayton, H.M.; White, A.D.; Kaiser, L.J.; Nauwelaerts, S.; Lavagnino, M.; Stubbs, N.C. Hindlimb response to tactile stimulation of the pastern and coronet. Equine Vet. J. 2010, 42, 227–233. [Google Scholar] [CrossRef]
- Frick, A. Stretching Exercises for Horses: Are They Effective? J. Equine Vet. Sci. 2010, 30, 50–59. [Google Scholar] [CrossRef]
- Haussler, K.K. The role of manual therapies in equine pain management. Vet. Clin. N. Am. Equine Pract. 2010, 26, 579–601. [Google Scholar] [CrossRef]
- Haussler, K.K.; Martin, C.E.; Hill, A.E. Efficacy of spinal manipulation and mobilisation on trunk flexibility and stiffness in horses: A randomised clinical trial. Equine Vet. J. 2010, 42, 695–702. [Google Scholar] [CrossRef]
- Hill, C.; Crook, T. The relationship between massage to the equine caudal hindlimb muscles and hindlimb protraction. Equine Vet. J. 2010, 42, 683–687. [Google Scholar] [CrossRef] [PubMed]
- Clayton, H.M.; Lavagnino, M.; Kaiser, L.J.; Stubbs, N.C. Evaluation of biomechanical effects of four stimulation devices placed on the hind feet of trotting horses. Am. J. Vet. Res. 2011, 72, 1489–1495. [Google Scholar] [CrossRef]
- Mykkänen, A.K.; Hyytiäinen, H.K.; McGowan, C.M. Generalised tetanus in a 2-week-old foal: Use of physiotherapy to aid recovery. Aust. Vet. J. 2011, 89, 447–451. [Google Scholar] [CrossRef]
- Stubbs, N.C.; Kaiser, L.J.; Hauptman, J.; Clayton, H.M. Dynamic mobilisation exercises increase cross sectional area of musculus multifidus. Equine Vet. J. 2011, 43, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Spencer, N.D.; Beadle, R.E.; Gaschen, L.; Buchert, M.R.; Lopez, M.J. Effects of athletic conditioning on horses with degenerative suspensory ligament desmitis: A preliminary report. Vet. J. 2011, 189, 49–57. [Google Scholar] [CrossRef]
- Clayton, H.M.; Kaiser, L.J.; Lavagnino, M.; Stubbs, N.C. Evaluation of intersegmental vertebral motion during performance of dynamic mobilization exercises in cervical lateral bending in horses. Am. J. Vet. Res. 2012, 73, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Carstanjen, B.; Trela, J.; Zukiewicz, K.; Gajewski, Z.; Rattenhuber, S. Repair and rehabilitation concept of a five-day-old radius fracture in a foal. Schweiz. Arch. Tierheilkd. 2012, 154, 153–154. [Google Scholar] [CrossRef]
- King, M.R.; Haussler, K.K.; Kawcak, C.E.; McIlwraith, C.W.; Reiser Ii, R.F. Effect of underwater treadmill exercise on postural sway in horses with experimentally induced carpal joint osteoarthritis. Am. J. Vet. Res. 2013, 74, 971–982. [Google Scholar] [CrossRef]
- Biermann, N.M.; Rindler, N.; Buchner, H.H.F. The Effect of Pulsed Electromagnetic Fields on Back Pain in Polo Ponies Evaluated by Pressure Algometry and Flexion Testing—A Randomized, Double-blind, Placebo-controlled Trial. J. Equine Vet. Sci. 2014, 34, 500–507. [Google Scholar] [CrossRef]
- De Oliveira, K.; Soutello, R.V.; Da Fonseca, R.; Costa, C.; Meirelles, P.R.d.L.; Fachiolli, D.F.; Clayton, H.M. Gymnastic Training and Dynamic Mobilization Exercises Improve Stride Quality and Increase Epaxial Muscle Size in Therapy Horses. J. Equine Vet. Sci. 2015, 35, 888–893. [Google Scholar] [CrossRef]
- Clayton, H.M. Core Training and Rehabilitation in Horses. Vet. Clin. N. Am. Equine Pract. 2016, 32, 49–71. [Google Scholar] [CrossRef] [PubMed]
- Daglish, J.; Mama, K.R. Pain: Its Diagnosis and Management in the Rehabilitation of Horses. Vet. Clin. N. Am. Equine Pract. 2016, 32, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Davidson, E.J. Controlled Exercise in Equine Rehabilitation. Vet. Clin. N. Am. Equine Pract. 2016, 32, 159–165. [Google Scholar] [CrossRef]
- Haussler, K.K. Joint Mobilization and Manipulation for the Equine Athlete. Vet. Clin. N. Am. Equine Pract. 2016, 32, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Schlachter, C.; Lewis, C. Electrophysical therapies for the equine athlete. Vet Clin N Amer: Equine Pract 2016, 32, 127–147. [Google Scholar] [CrossRef] [PubMed]
- Guedes, A. Pain Management in Horses. Vet. Clin. N. Am. Equine Pract. 2017, 33, 181–211. [Google Scholar] [CrossRef] [PubMed]
- Halsberghe, B.T. Long-Term and Immediate Effects of Whole Body Vibration on Chronic Lameness in the Horse: A Pilot Study. J. Equine Vet. Sci. 2017, 48, 121–128.e2. [Google Scholar] [CrossRef]
- King, M.R.; Haussler, K.K.; Kawcak, C.E.; McIlwraith, C.W.; Reiser, R.F.; Frisbie, D.D.; Werpy, N.M. Biomechanical and histologic evaluation of the effects of underwater treadmill exercise on horses with experimentally induced osteoarthritis of the middle carpal joint. Am. J. Vet. Res. 2017, 78, 558–569. [Google Scholar] [CrossRef]
- Mattos, L.H.L.; Yamada, A.L.M.; dos Santos, V.H.; Hussni, C.A.; Rodrigues, C.A.; Watanabe, M.J.; Alves, A.L.G. Treatment With Therapeutic Bandages to Control Equine Postarthroscopic Tibio-Patellofemoral Swelling. J. Equine Vet. Sci. 2017, 54, 87–92. [Google Scholar] [CrossRef]
- Nankervis, K.J.; Launder, E.J.; Murray, R.C. The Use of Treadmills Within the Rehabilitation of Horses. J. Equine Vet. Sci. 2017, 53, 108–115. [Google Scholar] [CrossRef]
- Contino, E.K. Management and Rehabilitation of Joint Disease in Sport Horses. Vet. Clin. N. Am. Equine Pract. 2018, 34, 345–358. [Google Scholar] [CrossRef]
- Gutierrez-Nibeyro, S.D.; McCoy, A.M.; Selberg, K.T. Recent advances in conservative and surgical treatment options of common equine foot problems. Vet. J. 2018, 237, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Jensen, A.-M.; Ahmed, W.; Elbrønd, V.S.; Harrison, A.P. The Efficacy of Intermittent Long-term Bell Boot Application for the Correction of Muscle Asymmetry in Equine Subjects. J. Equine Vet. Sci. 2018, 68, 73–80. [Google Scholar] [CrossRef]
- Nowlin, C.; Nielsen, B.; Mills, J.; Robison, C.; Schott, H.; Peters, D. Acute and Prolonged Effects of Vibrating Platform Treatment on Horses: A Pilot Study. J. Equine Vet. Sci. 2018, 62, 116–122. [Google Scholar] [CrossRef]
- Pluim, M.; Martens, A.; Vanderperren, K.; Sarrazin, S.; Koene, M.; Luciani, A.; van Weeren, P.R.; Delesalle, C. Short- and long term follow-up of 150 sports horses diagnosed with tendinopathy or desmopathy by ultrasonographic examination and treated with high-power laser therapy. Res. Vet. Sci. 2018, 119, 232–238. [Google Scholar] [CrossRef]
- Proctor-Brown, L.; Hicks, R.; Colmer, S.; Guilfoyle, D.; Dallap-Schaer, B.; Johnson, A.L.; Tomlinson, J. Distal limb pathologic conditions in horses treated with sleeve-style digital cryotherapy (285 cases). Res. Vet. Sci. 2018, 121, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Tranquille, C.A.; Tacey, J.B.; Walker, V.A.; Nankervis, K.J.; Murray, R.C. International Survey of Equine Water Treadmills—Why, When, and How? J. Equine Vet. Sci. 2018, 69, 34–42. [Google Scholar] [CrossRef]
- Wilson, J.M.; McKenzie, E.; Duesterdieck-Zellmer, K. International Survey Regarding the Use of Rehabilitation Modalities in Horses. Front. Vet. Sci. 2018, 5, 120. [Google Scholar] [CrossRef]
- Carrozzo, U.; Toniato, M.; Harrison, A. Assessment of Noninvasive Low-Frequency Ultrasound as a Means of Treating Injuries to Suspensory Ligaments in Horses: A Research Paper. J. Equine Vet. Sci. 2019, 80, 80–89. [Google Scholar] [CrossRef]
- Holcombe, S.J.; Shearer, T.R.; Valberg, S.J. The Effect of Core Abdominal Muscle Rehabilitation Exercises on Return to Training and Performance in Horses After Colic Surgery. J. Equine Vet. Sci. 2019, 75, 14–18. [Google Scholar] [CrossRef]
- Muñoz, A.; Saitua, A.; Becero, M.; Riber, C.; Satué, K.; de Medina, A.S.; Argüelles, D.; Castejón-Riber, C. The Use of the Water Treadmill for the Rehabilitation of Musculoskeletal Injuries in the Sport Horse. J. Vet. Res. 2019, 63, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Trager, L.R.; Funk, R.A.; Clapp, K.S.; Dahlgren, L.A.; Werre, S.R.; Hodgson, D.R.; Pleasant, R.S. Extracorporeal shockwave therapy raises mechanical nociceptive threshold in horses with thoracolumbar pain. Equine Vet. J. 2020, 52, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Van Harreveld, P.D.; Lillich, J.D.; Kawcak, C.E.; Gaughan, E.M.; Mclaughlin, R.M.; Debowes, R.M. Clinical evaluation of the effects of immobilization followed by remobilization and exercise on the metacarpophalangeal joint in horses. Am. J. Vet. Res. 2002, 63, 282–288. [Google Scholar] [CrossRef] [PubMed]
| Authors and Date | Type of Study | Type of Intervention and Comparator | Aims | Methods |
|---|---|---|---|---|
| [6] Bromiley, 1999 | Narrative review | N/A | Generic description of equine physical therapy and associated interventions | Literature review and expert opinion |
| [7] Ridgway and Harman, 1999 | Narrative review | N/A | Review interventions commonly used to treat equine back problems | Literature review and expert opinion |
| [8] Blackford et al., 2000 | Pre-test post-test clinical trial | Iontophoretic drug delivery vs. intraarticular injection or passive delivery | Compare iontophoretic delivery of dexamethasone-phosphate with intraarticular injection or passive delivery | One group received a single intraarticular injection of 4 mL dexamethasone-phosphate (6 mg/mL). The second group received iontophoretic administration of dexamethasone-phosphate (6 mg/mL) at 4 mA for 40 min in the treated limb and at 0 mA for 40 min in the contralateral (control) limb. Blood and synovial fluid collected for drug screening. |
| [9] Arnold et al., 2003 | Retrospective descriptive study. Multiple cases | Conservative management | Assess the effects of conservative management in non-articular fractures of the tibial tuberosity | Medical records analysis indicated conservative management consisting of box rest for 2 or 3 months with hand-walking starting in the 2nd month and increasing gradually (no amount indicated). Small paddock turnout or walking under saddle (depending on temperament) separately or combined until sound at slow trot followed by gradual integration into training program. |
| [10] Crowe et al., 2004 | Descriptive study | Radial pressure wave therapy | Assess the use of radial pressure wave therapy in the treatment of chronic or recurrent proximal suspensory desmitis | Based on manufacturer’s recommendation, 3 treatments (starting on diagnosis, repeated at 2-week interval), 1000 impulses radial pressure waves on each side of limb, 10 Hz frequency. Treatments were followed by a controlled exercise program consisting of box rest with daily controlled walking exercise for 6 weeks gradually increasing from 3 to 60 min, followed by starting to trot at week 10–12 with a gradual increase in duration. |
| [11] Porter, 2005 | Narrative review | Rehabilitation therapy description | Describe rehabilitation therapies for joint disease | Literature review and expert opinion |
| [12] Buchner and Schildboeck, 2006 | Narrative review | Physical therapy | Describe physiotherapeutic methods applied to horses | Literature review and expert opinion |
| [13] Goff, 2009 | Narrative review | Manual therapy | Describe manual therapies used in horses | Literature review and expert opinion |
| [14] Haussler, 2009 | Narrative review | Manual therapy | Describe manual therapies used in horses | Literature review and expert opinion |
| [15] Paulekas and Haussler, 2009 | Narrative review | Therapeutic exercise | Describe therapeutic exercises used for equine rehabilitation | Literature review and expert opinion |
| [16] Scott and Swenson, 2009 | Narrative review | Massage therapy | Describe evidence for the benefits of massage therapy in equine rehabilitation | Literature review and expert opinion |
| [17] Clayton et al., 2010 | Descriptive cross-sectional study | Dynamic mobilization in cervical flexion | Assess the influence on intravertebral angulation of 3 dynamic mobilization exercises proposed to be part of a rehabilitation protocol for neck and back pain | Three exercises in different positions of neck flexion: chin to chest, chin between carpi, chin between fore fetlocks |
| [18] Clayton et al., 2010 | Descriptive cross-sectional study | Lightweight tactile limb stimulator | Measure swing phase kinematic and kinetic effects of tactile stimulation of the hind pastern and coronet | Lightweight (55 g) tactile stimulators attached to hind pasterns during trotting |
| [19] Frick, 2010 | Narrative review | Stretching exercises | Review the use of stretching exercises to improve range of motion, prevent injury, decrease pain and offer indications/protocols for stretching exercises | Literature review and expert opinion |
| [20] Haussler, 2010 | Narrative review | Manual therapies | Review manual therapies used in equine pain management | Literature review and expert opinion |
| [21] Haussler et al., 2010 | Randomized clinical trial | Spinal manipulation and spinal mobilization | Determine whether a combination of spinal manipulative therapy and spinal mobilization is more effective in decreasing vertebral stiffness compared to spinal mobilization alone | Both groups received spinal mobilization applied rhythmically in the standing horse at 5 intervertebral sites (T14–T15, T17–T18, L1–L2, L3–L4, L6–S1). The spinal manipulation treatment group also received high-velocity, low-amplitude thrusts directed at the same 5 intervertebral sites. Weekly measurements pre- and post-intervention of spinal mobility, displacement amplitudes of the trunk, spinal stiffness, and trunk oscillation frequency. |
| [22] Hill and Crook, 2010 | Descriptive, comparative crossover design | Massage therapy | Determine the effect of massage on equine hind limb protraction in terms of increment of passive and active hind limb protraction | The same physical therapist massaged (effleurage interspersed with 3 × 30 s bursts of circular kneading) the superficial gluteal, semitendinosus, biceps femoris, and semimembranosus muscles for 30 min in the treatment group. The control group received a sham massage procedure. After a “washout” period of 7 days, the treatment groups were reversed. |
| [23] Clayton et al., 2011 | Cross-sectional study | Hind limb stimulation devices | Compare effects of different tactile stimulators on range of joint motion, re-education of movement patterns, and hind limb muscle strength | Optometric motion analysis of limb kinematics at trot using 4 types of stimulators: lightweight strap (10 g), tactile stimulator (55 g), flexible human wrist weights (700 g), and tactile stimulators added to limb weights (700 g). |
| [24] Mykkänen et al., 2011 | Case study | Physical therapy-based intervention | Describe effects of a physical therapy program in a case of severe generalized tetanus | Physical therapy techniques adapted from those used for upper motor neuron syndromes, including passive range of motion exercises, assisted active range of motion exercises, stretching, massage and modified proprioceptive neuromuscular facilitation performed for 6-weeks. After 2 weeks, a walking frame was introduced to assist the foal to stand and walk, and to allow longer periods of weight-bearing. Two weeks later exercises introduced to overcome residual problems, in particular the foal’s inability to raise and lower itself independently and mild foot deformities treated with corrective shoeing for one month. |
| [25] Stubbs et al., 2011 | Observational study | Dynamic mobilization exercises | Evaluate multifidus cross-sectional area before and after performing dynamic mobilization exercises for 12 weeks | Horses performed 3 cervical flexion exercises, one cervical extension exercise, and 3 cervical lateral bending exercises to both sides, 5 repetitions/exercise, 5 days/week for 12 weeks. Cross-sectional area of multifidus measured ultrasonographically on left and right sides at 5 thoracolumbar levels. |
| [26] Xie et al., 2011 | Observational study | Exercise (athletic conditioning) | Describe the effect of athletic conditioning on degenerative suspensory ligament desmitis | Horses exercised on a treadmill for 30 min every other day for 8 weeks. Treadmill speed adjusted to maintain average heart rate around 170 beats/min (80% of maximum heart rate and close to anaerobic threshold) for 20 min. After 8 weeks of exercise, horses turned out on pasture for 4 months. Effects evaluated using gait analysis, radiology, ultrasonography, and measurements of serum insulin and glucose at start of study, after 8 weeks exercise, and after 4 months rest. |
| [27] Clayton et al., 2012 | Observational study | Back problems, core training | Identify differences in cervical, thoracic, and lumbar intersegmental bending angles during 3 dynamic mobilization exercises in cervical lateral bending | Optometric motion analysis of skin-fixed markers on the head, cervical transverse processes (C1–C6), and dorsal spinous processes (T6, T8, T10, T16, L6, S2, and S4). Measures at rest and performing 3 dynamic cervical lateral bending exercises (chin-to-girth, chin-to-hip, and chin-to-tarsus) to the left and right sides. |
| [28] Carstanjen et al., 2012 | Case study | Rehabilitation concept | Describe intervention for repair and rehabilitation of a radial fracture | Manual passive physiological mobilization started 8 weeks post-surgery. At 16 weeks after surgery, swim training (100 to 500 m), hand-walking, and lunging-exercise on a firm surface were included for 5 to 20 min. |
| [29] King et al., 2013 | Narrative review | Aquatic therapy | Describe mechanisms of action of aquatic therapy in people, dogs, and horses and the potential value for treating equine osteoarthritis | Literature review and expert opinion |
| [30] Bierman et al., 2014 | Randomized double-blinded, placebo-controlled, clinical trial | Pulsed electromagnetic field therapy | Describe the effect of pulsed electromagnetic field therapy on back pain | Pulsed magnetic field therapy applied using blankets for 40 min/day, intensity approx. 50 microtesla, rectangular impulse and variable frequency of 1–30 Hz. Placebo blanket for control. |
| [31] Oliveira et al., 2015 | Randomized clinical trial | Gymnastic training and dynamic mobilization exercises | Assess effects of dynamic mobilization exercises and gymnastic training on quality of the walk stride and epaxial muscle size | Horses divided into 3 groups of 3 horses. All 3 groups performed hippotherapy sessions 3 days/week. Groups 2 and 3 performed dynamic mobilization exercises (3 cervical flexion exercises, one cervical extension exercise, and 3 cervical lateral bending exercises to left and right sides), 5 repetitions/session, 3 days/week. Group 3 also performed gymnastic exercises to strengthen abdominal and pelvic stabilization muscles: pelvic tilting (5 trials of 5 s duration), 10 steps rein back, walking around tight turns (3 circles to left and right), and walking over a 40 cm pole for 10 min. Evaluated using gait analysis and ultrasonographic measurements of size of multifidus and longissimus. |
| [32] Clayton, 2016 | Narrative review | Core training | Describe techniques associated with core training and rehabilitation of horses with back pain | Literature review and expert opinion |
| [33] Daglish and Mama, 2016 | Narrative review | General rehabilitation procedures | Describe pain assessment methods and interventions | Literature review and expert opinion |
| [34] Davidson, 2016 | Narrative review | Controlled exercise | Describe the usage of controlled exercise and commonly used protocols | Literature review and expert opinion with general recommendations for injuries of specific tissues. |
| [35] Haussler, 2016 | Narrative review | Joint mobilization and manipulation | Review joint mobilization and manipulation in the musculoskeletal management of the equine athlete | Literature review and expert opinion |
| [3] Kaneps, 2016 | Narrative review | General rehabilitation procedures | Review common rehabilitation approaches to surgical or medical equine conditions | Literature review and expert opinion |
| [36] Schlachter and Lewis, 2016 | Narrative review | Electrophysical modalities | Describe common electrophysical therapies used for equine athletes | Literature review and expert opinion |
| [37] Guedes, 2017 | Narrative review | Pain management | Review the pain mechanism and describe pain management in equine rehabilitation | Literature review and expert opinion |
| [38] Halsberghe, 2017 | Observational, pilot study | Whole body vibration | Verify long-term and immediate effects of whole-body vibration on chronic lameness | Lameness diagnosed by clinical assessment (AAEP lameness scale). All horses stood on a vibration platform during 30 min sessions at 40 Hz, amplitude 0.8 mm, acceleration 4.9 m/s2, 5 days/week for 60 days. Normal exercise routine maintained. Kinematic data acquired by inertial sensors. |
| [39] King et al., 2017 | Randomized clinical trial | Underwater treadmill | 16, 2- to 5-year-old horses with surgically induced osteoarthritis in one carpal joint | One week after surgery, horses randomly assigned to treatment or control groups. Both groups exercised at walk on the treadmill, but water added only for the treatment group. Effects evaluated by lameness examinations, and kinematic, kinetic, and electromyographic analyses during overground locomotion, diagnostic imaging, goniometry, and diagnostic imaging. |
| [40] Mattos et al., 2017 | Randomized clinical trial | Therapeutic bandages | Verify the contribution of kinesiology taping to control post-operative swelling following arthroscopy of the tibio-patellofemoral joint | Kinesiology taping of the stifle using a FAN technique with 10% tension (original tension from factory). Tape applied 12–72 h post-surgery. |
| [41] Nankervis et al., 2017 | Narrative review | Overground and water treadmills | Present evidence to inform the use of overground and water treadmills for rehabilitation of injury | Literature review and expert opinion |
| [42] Contino, 2018 | Narrative review | General rehabilitation procedures | Describe the common management and rehabilitation of joint injury in sports horses | Literature review and expert opinion |
| [43] Gutierrrez-Nibeyro et al., 2018 | Narrative review | Conservative management | Describe conservative and surgical treatment options for common equine foot problems | Literature review and expert opinion |
| [44] Jensen et al., 2018 | Clinical study | Proprioceptive stimulation | Describes the effects of using a bell boot on a hind limb with imbalanced function of the superficial gluteal muscle | Eight trained horses that were shown by acoustic myography to have an imbalance of superficial gluteal muscle function when circling to the left. Horses were trained for 6 weeks with a single bell boot applied to the “weaker” hind limb. Evaluation based on improved acoustic myography scores. |
| [45] Nowlin et al., 2018 | Pair-matched control study | Vibration therapy | Verify the effects of vibration therapy on performance improvement and healing in competitive horses | Treatment group: vibration platform at 50 Hz for 30 min. Control group: 30 min on the platform while turned off. |
| [46] Pluim et al., 2018 | Retrospective, observational clinical study | High-power laser therapy | Verify the effectiveness of high-power laser therapy in treatment of 150 sports horses diagnosed ultrasonographically with tendinopathy or desmopathy | Horses treated once daily for 20 min using the manufacturer’s pre-established protocol to provide approximately 250 J/cm3 per treatment to injured area for 2 weeks. Additional pharmacological and physical treatments applied based on clinical judgement. Diagnostic ultrasonography used at start of study, at completion of laser treatment, and 4 weeks after treatment ceased. A progressive exercise rehabilitation protocol was used. |
| [47] Proctor-Brown et al., 2018 | Retrospective study | Cryotherapy | Verify the benefits of digital cryotherapy on distal limb conditions | Sleeve-style digital cryotherapy. Three administration protocols: continuous (211 cases), interrupted (57 cases), and intermittent (17 cases). |
| [48] Tranquille et al., 2018 | Survey | Water treadmill | To understand how and why the water treadmill is used in equine rehabilitation | n/a |
| [49] Wilson et al., 2018 | Survey | Rehabilitation modalities | Describe rehabilitation modalities used the horse | n/a |
| [50] Carrozzo et al., 2019 | Retrospective description | Non-invasive low frequency ultrasound | Describe the effect of the therapeutic ultrasound in the treatment of lameness | Low frequency therapeutic ultrasound started at 50% dosage for each protocol for 1 min for horse habituation to stimulus, then increased to desired dosage. Protocols defined by injury stage (acute, subacute, chronic), using different transducers for pulsed and continuous emission, and various shapes for different wave emission. |
| [51] Holcombe et al., 2019 | Retrospective cohort | Core training | Determine effects of 4-week core abdominal rehabilitation exercises (CARE) after colic surgery in terms of safety and return to training | The CARE exercise program is a 4-week protocol, based on increasing the type and number of core training exercises on a weekly basis. |
| [52] Muñoz et al., 2019 | Narrative review | Water treadmill | Review the principles of aquatic therapy, types of aquatic exercise, and rehabilitation parameters for specific injuries | Describes pros and cons of the use of a water treadmill exercise in a rehabilitation program for a variety of injuries. |
| [53] Trager et al., 2019 | Observational study | Extracorporeal shockwave therapy | Assess effects of extracorporeal shockwave therapy on mechanical nociceptive threshold and cross-sectional area of multifidus muscle | Shockwave therapy used in 3 treatment sessions, 2 weeks apart (days 0, 14 and 28), 80 mm probe, power E4 (penetration depth 113 mm, energy flux density 0.13 mJ/mm2), 45° angulation of probe. Continuous movement of probe between T12 and L5 for 1500 pulses (750 each side). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atalaia, T.; Prazeres, J.; Abrantes, J.; Clayton, H.M. Equine Rehabilitation: A Scoping Review of the Literature. Animals 2021, 11, 1508. https://doi.org/10.3390/ani11061508
Atalaia T, Prazeres J, Abrantes J, Clayton HM. Equine Rehabilitation: A Scoping Review of the Literature. Animals. 2021; 11(6):1508. https://doi.org/10.3390/ani11061508
Chicago/Turabian StyleAtalaia, Tiago, José Prazeres, João Abrantes, and Hilary M. Clayton. 2021. "Equine Rehabilitation: A Scoping Review of the Literature" Animals 11, no. 6: 1508. https://doi.org/10.3390/ani11061508
APA StyleAtalaia, T., Prazeres, J., Abrantes, J., & Clayton, H. M. (2021). Equine Rehabilitation: A Scoping Review of the Literature. Animals, 11(6), 1508. https://doi.org/10.3390/ani11061508








