Attachment to Pets Moderates Transitions in Latent Patterns of Mental Health Following the Onset of the COVID-19 Pandemic: Results of a Survey of U.S. Adults
Abstract
Simple Summary
Abstract
1. Introduction
1.1. Animal Companions and the COVID-19 Pandemic
1.2. Person-Centered Approaches to Examining Relations between Mental Health and HAI
1.3. Current Study
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Indicators of Mental Health
2.2.2. Attachment to Dogs and Cats
2.2.3. Covariates
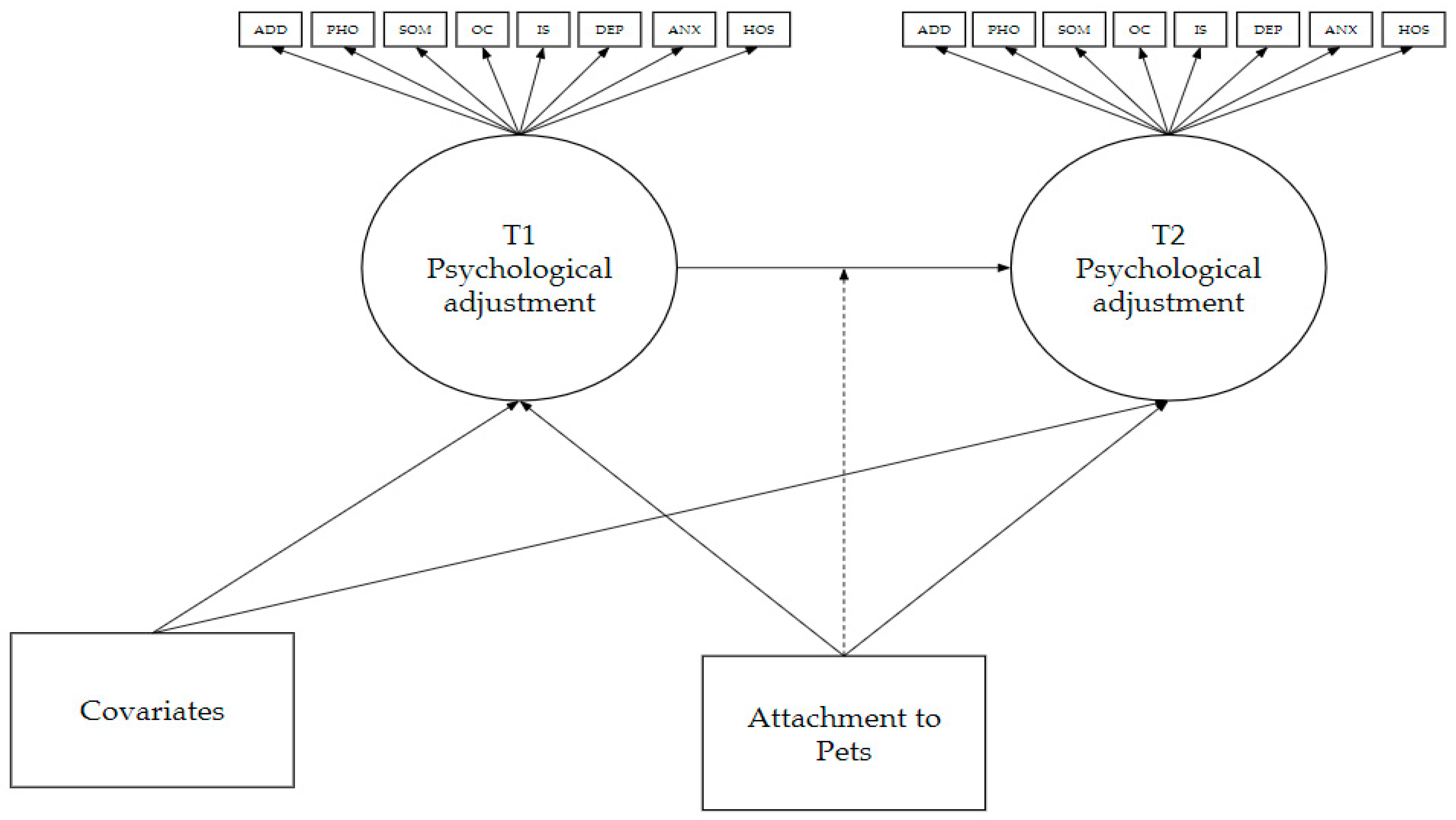
2.3. Analytic Plan
3. Results
3.1. Descriptive Statistics
3.2. Latent Profile Analyses
3.3. Latent Transition Analysis
4. Discussion
4.1. Limitations
4.2. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control. COVID Data Tracker; Centers for Disease Control, 2021. Available online: https://covid.cdc.gov/covid-data-tracker/ (accessed on 25 February 2021).
- John Hopkins University of Medicine Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/ (accessed on 25 February 2021).
- Kira, I.A.; Shuwiekh, H.A.M.; Rice, K.G.; Ashby, J.S.; Elwakeel, S.A.; Sous, M.S.F.; Alhuwailah, A.; Baali, S.B.A.; Azdaou, C.; Oliemat, E.M.; et al. Measuring COVID-19 as Traumatic Stress: Initial Psychometrics and Validation. J. Loss Trauma 2020, 1–18. [Google Scholar] [CrossRef]
- Czeisler, M.É.; Lane, R.I.; Petrosky, E.; Wiley, J.F.; Christensen, A.; Njai, R.; Weaver, M.D.; Robbins, R.; Facer-Childs, E.R.; Barger, L.K.; et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic—United States, June 24–30, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1049–1057. [Google Scholar] [CrossRef] [PubMed]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef] [PubMed]
- Holman, E.A.; Thompson, R.R.; Garfin, D.R.; Silver, R.C. The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Sci. Adv. 2020, 6, eabd5390. [Google Scholar] [CrossRef]
- Shanahan, L.; Steinhoff, A.; Bechtiger, L.; Murray, A.L.; Nivette, A.; Hepp, U.; Ribeaud, D.; Eisner, M. Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020, 1–10. [Google Scholar] [CrossRef]
- McGinty, E.E.; Presskreischer, R.; Anderson, K.E.; Han, H.; Barry, C.L. Psychological Distress and COVID-19–Related Stressors Reported in a Longitudinal Cohort of US Adults in April and July 2020. JAMA 2020, 324, 2555. [Google Scholar] [CrossRef]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Carr, J. Covid: “Pets Listen to Your Troubles without Judgement”. Available online: https://www.bbc.com/news/uk-england-cornwall-55797428 (accessed on 12 February 2021).
- Herzog, H. Why Do People Risk Their Own Health for Their Pets? Available online: https://www.psychologytoday.com/blog/animals-and-us/202010/why-do-people-risk-their-own-health-their-pets (accessed on 12 February 2021).
- Herzog, H. Do Pets Improve Mental Health during COVID Lockdowns? Available online: https://www.psychologytoday.com/blog/animals-and-us/202010/do-pets-improve-mental-health-during-covid-lockdowns (accessed on 12 February 2021).
- Applebaum, J.W.; Peek, C.W.; Zsembik, B.A. Examining U.S. pet ownership using the General Social Survey. Soc. Sci. J. 2020, 1–10. [Google Scholar] [CrossRef]
- Morgan, L.; Protopopova, A.; Birkler, R.I.D.; Itin-Shwartz, B.; Sutton, G.A.; Gamliel, A.; Yakobson, B.; Raz, T. Human–dog relationships during the COVID-19 pandemic: Booming dog adoption during social isolation. Humanit. Soc. Sci. Commun. 2020, 7, 1–11. [Google Scholar] [CrossRef]
- Packaged Facts. U.S. Pet Market Outlook, 2020–2021: Responding to the COVID-19 Impact; Packaged Facts: USA, 2020; p. 344. Available online: https://www.packagedfacts.com/prod-toc/Pet-Outlook-12153371/ (accessed on 25 February 2021).
- Bowen, J.; García, E.; Darder, P.; Argüelles, J.; Fatjó, J. The effects of the Spanish COVID-19 lockdown on people, their pets, and the human-animal bond. J. Veter Behav. 2020, 40, 75–91. [Google Scholar] [CrossRef] [PubMed]
- Shoesmith, E.; Shahab, L.; Kale, D.; Mills, D.; Reeve, C.; Toner, P.; de Assis, L.S.; Ratschen, E. The Influence of Human–Animal Interactions on Mental and Physical Health during the First COVID-19 Lockdown Phase in the U.K.: A Qualitative Exploration. Int. J. Environ. Res. Public Health 2021, 18, 976. [Google Scholar] [CrossRef]
- Young, J.; Pritchard, R.; Nottle, C.; Banwell, H. Pets, Touch, and COVID-19: Health Benefits from Non-Human Touch through Times of Stress. J. Behav. Econ. Pol. 2020, 4, 25–33. [Google Scholar]
- Ratschen, E.; Shoesmith, E.; Shahab, L.; Silva, K.; Kale, D.; Toner, P.; Reeve, C.; Mills, D.S. Human-animal relationships and interactions during the Covid-19 lockdown phase in the UK: Investigating links with mental health and loneliness. PLoS ONE 2020, 15, e0239397. [Google Scholar] [CrossRef] [PubMed]
- Applebaum, J.W. The Concerns, Difficulties, and Stressors of Caring for Pets during COVID-19: Results from a Large Survey of U.S. Pet Owners. Animials 2020, 10, 1882. [Google Scholar] [CrossRef] [PubMed]
- Applebaum, J.W. How pets factor into healthcare decisions for COVID-19: A One Health perspective. One Health 2020, 11, 100176. [Google Scholar] [CrossRef] [PubMed]
- Parry, N.M. COVID-19 and pets: When pandemic meets panic. Forensic Sci. Int. Rep. 2020, 2, 100090. [Google Scholar] [CrossRef]
- Matijczak, A.; McDonald, S.E.; Tomlinson, C.A.; Murphy, J.L.; O’Connor, K. The Moderating Effect of Comfort from Companion Animals and Social Support on the Relationship between Microaggressions and Mental Health in LGBTQ+ Emerging Adults. Behav. Sci. 2020, 11, 1. [Google Scholar] [CrossRef]
- McDonald, S.E.; O’Connor, K.; Matijczak, A.; Murphy, J.L.; Applebaum, J.W.; Tomlinson, C.A.; Wike, T.; Kattari, S. Victimization and Psychological Wellbeing among Sexual and Gender Minority Emerging Adults: Testing the Moderating Role of Emotional Comfort from Companion Animals. J. Soc. Soc. Work Res. 2021, 11, 1. [Google Scholar] [CrossRef]
- Pendry, P.; Vandagriff, J.L. Salivary Studies of the Social Neuroscience of Human-Animal Interaction. In Salivary Bioscience; Granger, D.A., Taylor, M.K., Eds.; Springer: Cham, Switzerland, 2020; pp. 555–581. [Google Scholar]
- Purewal, R.; Christley, R.; Kordas, K.; Joinson, C.; Meints, K.; Gee, N.; Westgarth, C. Companion Animals and Child/Adolescent Development: A Systematic Review of the Evidence. Int. J. Environ. Res. Public Health 2017, 14, 234. [Google Scholar] [CrossRef]
- Knowles, K.A.; Sripada, R.K.; Defever, M.; Rauch, S.A.M. Comorbid mood and anxiety disorders and severity of posttraumatic stress disorder symptoms in treatment-seeking veterans. Psychol. Trauma: Theory Res. Pract. Policy 2019, 11, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Spinhoven, P.; Penninx, B.W.; van Hemert, A.M.; de Rooij, M.; Elzinga, B.M. Comorbidity of PTSD in anxiety and depressive disorders: Prevalence and shared risk factors. Child Abus. Negl. 2014, 38, 1320–1330. [Google Scholar] [CrossRef]
- Watson, H.J.; Swan, A.; Nathan, P.R. Psychiatric diagnosis and quality of life: The additional burden of psychiatric comorbidity. Compr. Psychiatry 2011, 52, 265–272. [Google Scholar] [CrossRef]
- McMillan, K.A.; Asmundson, G.J.; Sareen, J. Comorbid PTSD and Social Anxiety Disorder. J. Nerv. Ment. Dis. 2017, 205, 732–737. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Koretz, D.; Merikangas, K.R.; Rush, A.J.; Walters, E.E.; Wang, P.S. The Epidemiology of Major Depressive Disorder. JAMA 2003, 289, 3095–3105. [Google Scholar] [CrossRef]
- Lanza, S.T.; Cooper, B.R. Latent Class Analysis for Developmental Research. Child Dev. Perspect. 2016, 10, 59–64. [Google Scholar] [CrossRef]
- Petersen, K.J.; Qualter, P.; Humphrey, N. The Application of Latent Class Analysis for Investigating Population Child Mental Health: A Systematic Review. Front. Psychol. 2019, 10, 1214. [Google Scholar] [CrossRef] [PubMed]
- Lanza, S.T.; Bray, B.C.; Collins, L.M. An introduction to latent class and latent transition analysis. In Handbook of Psychology; Schinka, J.A., Velicer, W.F., Weiner, I.B., Eds.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2013; Volume 2, pp. 691–716. [Google Scholar]
- Lanza, S.T.; Rhoades, B.L. Latent Class Analysis: An Alternative Perspective on Subgroup Analysis in Prevention and Treatment. Prev. Sci. 2013, 14, 157–168. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, S.L.; Moore, E.W.G.; Hull, D.M. Finding latent groups in observed data: A primer on latent profile analysis in Mplus for applied researchers. Int. J. Behav. Dev. 2019, 44, 458–468. [Google Scholar] [CrossRef]
- Kim, H.; Eaton, N.R. A Hierarchical Integration of Person-Centered Comorbidity Models: Structure, Stability, and Transition Over Time. Clin. Psychol. Sci. 2017, 5, 595–612. [Google Scholar] [CrossRef]
- El-Gabalawy, R.; Tsai, J.; Harpaz-Rotem, I.; Hoff, R.; Sareen, J.; Pietrzak, R.H. Predominant typologies of psychopathology in the United States: A latent class analysis. J. Psychiatr. Res. 2013, 47, 1649–1657. [Google Scholar] [CrossRef] [PubMed]
- Olino, T.M.; Klein, D.N.; Farmer, R.F.; Seeley, J.R.; Lewinsohn, P.M. Examination of the structure of psychopathology using latent class analysis. Compr. Psychiatry 2012, 53, 323–332. [Google Scholar] [CrossRef]
- Vaidyanathan, U.; Patrick, C.J.; Iacono, W.G. Patterns of comorbidity among mental disorders: A person-centered approach. Compr. Psychiatry 2011, 52, 527–535. [Google Scholar] [CrossRef]
- Kamphaus, R.W.; Huberty, C.J.; Distefano, C.; Petoskey, M.D. A Typology of Teacher-Rated Child Behavior for a National U.S. Sample. J. Abnorm. Child Psychol. 1997, 25, 453–463. [Google Scholar] [CrossRef]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, Severity, and Comorbidity of 12-Month DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef]
- Kamphaus, R.W.; Petoskey, M.D.; Cody, A.H.; Rowe, E.W.; Huberty, C.J.; Reynolds, C.R. A Typology of Parent Rated Child Behavior for a National U.S. Sample. J. Child Psychol. Psychiatry 1999, 40, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Fernández, R.S.; Crivelli, L.; Guimet, N.M.; Allegri, R.F.; Pedreira, M.E. Psychological distress associated with COVID-19 quarantine: Latent profile analysis, outcome prediction and mediation analysis. J. Affect. Disord. 2020, 277, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Derogatis, L.R.; Melisaratos, N. The Brief Symptom Inventory: An introductory report. Psychol. Med. 1983, 13, 595–605. [Google Scholar] [CrossRef]
- Masyn, K.E. Measurement Invariance and Differential Item Functioning in Latent Class Analysis With Stepwise Multiple Indicator Multiple Cause Modeling. Struct. Equ. Model. A Multidiscip. J. 2016, 24, 180–197. [Google Scholar] [CrossRef]
- Hawkins, R.D.; Williams, J.M. Childhood Attachment to Pets: Associations between Pet Attachment, Attitudes to Animals, Compassion, and Humane Behaviour. Int. J. Environ. Res. Public Health 2017, 14, 490. [Google Scholar] [CrossRef] [PubMed]
- Stallones, L.; Johnson, T.P.; Garrity, T.F.; Marx, M.B. Quality of Attachment to Companion Animals among U.S. Adults 21 to 64 Years of Age. Anthrozoös 1990, 3, 171–176. [Google Scholar] [CrossRef]
- Westgarth, C.; Boddy, L.M.; Stratton, G.; German, A.J.; Gaskell, R.M.; Coyne, K.P.; Bundred, P.; McCune, S.; Dawson, S. Pet ownership, dog types and attachment to pets in 9–10 year old children in Liverpool, UK. BMC Veter Res. 2013, 9, 102. [Google Scholar] [CrossRef]
- Moore, S.E.; Wierenga, K.L.; Prince, D.M.; Gillani, B.; Mintz, L.J. Disproportionate Impact of the COVID-19 Pandemic on Perceived Social Support, Mental Health and Somatic Symptoms in Sexual and Gender Minority Populations. J. Homosex. 2021, 68, 577–591. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Savitz, K.L. The SCL–90–R and Brief Symptom Inventory (BSI) in primary care. In Handbook of Psychological Assessment in Primary Care Settings; Maruish, M.E., Ed.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2000; pp. 297–334. ISBN 978-0-8058-2999-0. [Google Scholar]
- Johnson, T.P.; Garrity, T.F.; Stallones, L. Psychometric Evaluation of the Lexington Attachment to Pets Scale (Laps). Anthrozoös 1992, 5, 160–175. [Google Scholar] [CrossRef]
- Masyn, K. Latent Class Analysis and Finite Mixture Modeling. In The Oxford Handbook of Quantitative Methods; Little, T.D., Ed.; Oxford University Press: Oxford, UK, 2013; Volume 2, pp. 551–611. [Google Scholar]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Asner-Self, K.K.; Schreiber, J.B.; Marotta, S.A. A cross-cultural analysis of the Brief Symptom Inventory-18. Cult. Divers. Ethn. Minor. Psychol. 2006, 12, 367–375. [Google Scholar] [CrossRef]
- Pereda, N.; Forns, M.; Peró, M. Dimensional structure of the Brief Symptom Inventory with Spanish college students. Psicothema 2007, 19, 634–639. [Google Scholar] [PubMed]
- Prelow, H.M.; Weaver, S.R.; Swenson, R.R.; Bowman, M.A. A preliminary investigation of the validity and reliability of the Brief-Symptom Inventory-18 in economically disadvantaged Latina American mothers. J. Community Psychol. 2005, 33, 139–155. [Google Scholar] [CrossRef]
- Torres, L.C.; Miller, M.J.; Moore, K.M. Factorial invariance of the Brief Symptom Inventory-18 (BSI-18) for adults of Mexican descent across nativity status, language format, and gender. Psychol. Assess. 2013, 25, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Casullo, M.M.; Fernández, M. Malestares Psicológicos en Estudiantes Adolescentes Argentinos. Psykhe 2001, 10, 155–162. [Google Scholar]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H. “Chris” Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef]
- Ni, M.Y.; Yang, L.; Leung, C.M.C.; Li, N.; Yao, X.; Wang, Y.; Leung, G.M.; Cowling, B.J.; Liao, Q. Mental Health, Risk Factors, and Social Media Use During the COVID-19 Epidemic and Cordon Sanitaire Among the Community and Health Professionals in Wuhan, China: Cross-Sectional Survey. JMIR Ment. Health 2020, 7, e19009. [Google Scholar] [CrossRef] [PubMed]
- Arigo, D.; Pagoto, S.; Carter-Harris, L.; Lillie, S.; Nebeker, C. Using social media for health research: Methodological and ethical considerations for recruitment and intervention delivery. Digit. Health 2018, 4, 2055207618771757. [Google Scholar] [CrossRef]
- Reuben, A.; Moffitt, T.E.; Caspi, A.; Belsky, D.W.; Harrington, H.; Schroeder, F.; Hogan, S.; Ramrakha, S.; Poulton, R.; Danese, A. Lest we forget: Comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J. Child Psychol. Psychiatry 2016, 57, 1103–1112. [Google Scholar] [CrossRef]
- Bauer, D.J.; Curran, P.J. Distributional Assumptions of Growth Mixture Models: Implications for Overextraction of Latent Trajectory Classes. Psychol. Methods 2003, 8, 338–363. [Google Scholar] [CrossRef] [PubMed]
- Morin, A.J.; Meyer, J.P.; Creusier, J.; Biétry, F. Multiple-Group Analysis of Similarity in Latent Profile Solutions. Organ. Res. Methods 2015, 19, 231–254. [Google Scholar] [CrossRef]
- Kolacz, J.; Dale, L.P.; Nix, E.J.; Roath, O.K.; Lewis, G.F.; Porges, S.W. Adversity History Predicts Self-Reported Autonomic Reactivity and Mental Health in US Residents During the COVID-19 Pandemic. Front. Psychiatry 2020, 11, 577728. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.D.; McDonald, S.E.; O’Connor, K.; Matijczak, A.; Ascione, F.R.; Williams, J.H. Exposure to intimate partner violence and internalizing symptoms: The moderating effects of positive relationships with pets and animal cruelty exposure. Child Abus. Negl. 2019, 98, 104166. [Google Scholar] [CrossRef]
- McDonald, S.E.; Murphy, J.L.; Tomlinson, C.A.; Matijczak, A.; Applebaum, J.W.; Wike, T.L.; Kattari, S.K. Relations Between Sexual and Gender Minority Stress, Personal Hardiness, and Psychological Stress in Emerging Adulthood: Examining Indirect Effects via Human-animal Interaction. Youth Soc. 2021. [Google Scholar] [CrossRef]
- Riggs, D.W.; Taylor, N.; Signal, T.; Fraser, H.; Donovan, C. People of Diverse Genders and/or Sexualities and Their Animal Companions: Experiences of Family Violence in a Binational Sample. J. Fam. Issues 2018, 39, 4226–4247. [Google Scholar] [CrossRef]
- Rauktis, M.E.; Lee, H.; Bickel, L.; Giovengo, H.; Nagel, M.; Cahalane, H. Food Security Challenges and Health Opportunities of Companion Animal Ownership for Low-Income Adults. J. Evidence-Based Soc. Work. 2020, 17, 662–676. [Google Scholar] [CrossRef] [PubMed]
- Power, E.R. Renting with pets: A pathway to housing insecurity? Hous. Stud. 2016, 32, 336–360. [Google Scholar] [CrossRef]

| Variable Name | Variable Categories | Frequency (%) |
|---|---|---|
| Race/Ethnicity | Arab/Arab American | 2 (0.1) |
| Asian/Asian American | 42 (2.2) | |
| Black/African American | 15 (0.8) | |
| First Nations/Indigenous | 3 (0.2) | |
| Latino/Latina/Latinx | 50 (2.6) | |
| South Asian/Pacific Islander | 7 (0.4) | |
| White | 1702 (87.6) | |
| Multiracial/Mixed Race | 111 (5.7) | |
| Prefer to self-describe | 10 (0.5) | |
| Gender Identity | Cisgender female/woman | 1743 (89.8) |
| Cisgender male/man | 137 (7.0) | |
| Genderqueer/gender non-conforming | 21 (1.1) | |
| Transgender female/woman | 2 (0.1) | |
| Transgender male/man | 9 (0.5) | |
| Multiple Identities | 27 (1.4) | |
| Missing | 5 (0.3) | |
| Sexual Orientation | Asexual | 25 (1.3) |
| Bisexual | 157 (8.1) | |
| Demisexual | 11 (0.6) | |
| Gay | 21 (1.1) | |
| Heterosexual/straight | 1510 (77.8) | |
| Lesbian | 50 (2.6) | |
| Pansexual | 27 (1.4) | |
| Queer | 29 (1.5) | |
| Two-Spirit | 1 (0.1) | |
| Prefer to self-describe | 6 (0.3) | |
| Multiple identities | 83 (4.3) | |
| Not sure/questioning | 22 (1.1) | |
| Employment Change | Begun new job | 13 (0.7) |
| Laid off or fired | 121 (6.2) | |
| No change | 680 (35.0) | |
| Working from home | 692 (35.6) | |
| Other change | 194 (10.0) | |
| Multiple options selected | 242 (12.5) | |
| Pet Type—Owned 1 | Bird(s) | 70 (3.6) |
| Cat(s) | 1029 (53.0) | |
| Dog(s) | 1442 (74.3) | |
| Fish | 155 (8) | |
| Horse(s) | 54 (2.8) | |
| Small mammal(s) (e.g., rat, hedgehog, rabbit) | 68 (3.5) | |
| Reptile(s) (e.g., snake, lizard, turtle) | 109 (5.6) | |
| Other pet(s) (e.g., cow, goat, spider, chicken) | 49 (2.5) | |
| Pet Type—Favorite | Cat | 667 (34.3) |
| Dog | 1275 (65.7) |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | -- | |||||||||||||||||
| 2. Attachment to Pet | −0.09 | -- | ||||||||||||||||
| 3. Anxiety (T1) | −0.26 | 0.09 | -- | |||||||||||||||
| 4. Depression (T1) | −0.24 | 0.09 | 0.62 | -- | ||||||||||||||
| 5. Hostility (T1) | −0.22 | 0.09 | 0.51 | 0.52 | -- | |||||||||||||
| 6. Interpersonal Sensitivity (T1) | −0.30 | 0.09 | 0.61 | 0.68 | 0.52 | -- | ||||||||||||
| 7. Obsessive-Compulsive (T1) | −0.26 | 0.08 | 0.62 | 0.64 | 0.52 | 0.62 | -- | |||||||||||
| 8. Phobic Anxiety (T1) | −0.21 | 0.12 | 0.50 | 0.48 | 0.37 | 0.50 | 0.47 | -- | ||||||||||
| 9. Somatization (T1) | −0.08 | 0.08 | 0.46 | 0.43 | 0.37 | 0.40 | 0.47 | 0.35 | -- | |||||||||
| 10. Additional Items (T1) | −0.10 | 0.07 | 0.50 | 0.53 | 0.36 | 0.47 | 0.54 | 0.38 | 0.43 | -- | ||||||||
| 11. Anxiety (T2) | −0.24 | 0.09 | 0.62 | 0.46 | 0.34 | 0.45 | 0.43 | 0.39 | 0.34 | 0.37 | -- | |||||||
| 12. Depression (T2) | −0.30 | 0.09 | 0.50 | 0.68 | 0.38 | 0.54 | 0.47 | 0.38 | 0.34 | 0.41 | 0.66 | -- | ||||||
| 13. Hostility (T2) | −0.27 | 0.06 | 0.41 | 0.41 | 0.56 | 0.40 | 0.38 | 0.29 | 0.26 | 0.29 | 0.52 | 0.53 | -- | |||||
| 14. Interpersonal Sensitivity (T2) | −0.28 | 0.13 | 0.47 | 0.55 | 0.40 | 0.73 | 0.49 | 0.42 | 0.34 | 0.38 | 0.52 | 0.63 | 0.49 | -- | ||||
| 15. Obsessive-Compulsive (T2) | −0.31 | 0.07 | 0.53 | 0.53 | 0.40 | 0.50 | 0.69 | 0.39 | 0.36 | 0.45 | 0.60 | 0.65 | 0.51 | 0.55 | -- | |||
| 16. Phobic Anxiety (T2) | −0.12 | 0.07 | 0.34 | 0.28 | 0.23 | 0.31 | 0.28 | 0.42 | 0.20 | 0.26 | 0.55 | 0.46 | 0.30 | 0.36 | 0.41 | -- | ||
| 17. Somatization (T2) | −0.08 | 0.08 | 0.38 | 0.37 | 0.29 | 0.34 | 0.37 | 0.30 | 0.68 | 0.33 | 0.48 | 0.46 | 0.34 | 0.39 | 0.44 | 0.31 | -- | |
| 18. Additional Items (T2) | −0.18 | 0.06 | 0.44 | 0.45 | 0.30 | 0.41 | 0.44 | 0.34 | 0.33 | 0.64 | 0.57 | 0.60 | 0.43 | 0.46 | 0.57 | 0.41 | 0.42 | -- |
| Mean | 39.68 | 79.93 | 1.24 | 1.29 | 1.26 | 1.32 | 1.42 | 0.89 | 0.96 | 1.38 | 1.46 | 1.58 | 1.30 | 1.11 | 1.64 | 1.73 | 1.01 | 1.67 |
| Standard Deviation | 13.61 | 9.08 | 0.77 | 0.87 | 0.76 | 0.92 | 0.77 | 0.92 | 0.80 | 0.87 | 0.88 | 0.95 | 0.88 | 0.99 | 0.90 | 1.21 | 0.88 | 0.91 |
| Variance/Covariance Structure | k | Par | LL | AIC | BIC | aBIC | VLMR-LRT | LMR-LRT | BLRT | Entropy | Smallest Class | Condition # | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p-Value | p-Value | p-Value | n | % | |||||||||
| Non-Diagonal, Class Invariant | 1 | 44 | −16,322.3 | 32,732.5 | 32,979.4 | 32,839.7 | NA | NA | NA | NA | 2021 | 100% | 2.55 × 10−3 |
| 2 | 53 | −16,194.0 | 32,494.0 | 32,791.4 | 32,623.0 | 0.429 | 0.432 | 0.000 | 0.841 | 241 | 12% | 4.10 × 10−4 | |
| 3 | 62 | −15,886.7 | 31,897.4 | 32,245.3 | 32,048.3 | 0.006 | 0.007 | 0.000 | 0.970 | 269 | 13% | 1.74 × 10−10 | |
| 4 | 71 | −15,177.5 | 30,496.9 | 30,895.3 | 30,669.8 | 0.000 | 0.000 | 0.000 | 0.984 | 115 | 6% | 2.73 × 10−10 | |
| Diagonal, Class Invariant | 1 | 16 | −20,027.8 | 40,087.5 | 40,177.3 | 40,126.5 | NA | NA | NA | NA | 2021 | 100% | 3.63 × 10−2 |
| 2 | 25 | −17,758.9 | 35,567.8 | 35,708.0 | 35,628.6 | 0.000 | 0.000 | 0.000 | 0.888 | 482 | 24% | 1.92 × 10−2 | |
| 3 | 34 | −16,789.1 | 33,646.2 | 33,837.0 | 33,728.9 | 0.000 | 0.000 | 0.000 | 0.855 | 286 | 14% | 5.04 × 10−3 | |
| 4 | 43 | −16,438.3 | 32,962.7 | 33,204.0 | 33,067.3 | 0.021 | 0.022 | 0.000 | 0.846 | 150 | 7% | 1.33 × 10−3 | |
| 5 | 52 | −16,277.8 | 32,659.5 | 32,951.3 | 32,786.1 | 0.000 | 0.000 | 0.000 | 0.809 | 91 | 5% | 5.41 × 10−4 | |
| 6 | 61 | −16,221.7 | 325,65.3 | 32,907.6 | 32,713.8 | 0.318 | 0.325 | 0.000 | 0.826 | 95 | 5% | 2.77 × 10−6 | |
| Diagonal, Class Varying | 1 | 16 | −20,027.8 | 40,087.5 | 40,177.3 | 40,126.5 | NA | NA | NA | NA | 2021 | 100% | 3.63 × 10−2 |
| 2 | 33 | −17,582.1 | 35,230.3 | 35,415.5 | 35,310.6 | 0.000 | 0.000 | 0.000 | 0.848 | 640 | 32% | 1.21 × 10−2 | |
| 3 | 50 | −16,349.1 | 32,798.2 | 33,078.8 | 32,920.0 | 0.000 | 0.000 | 0.000 | 0.860 | 528 | 26% | 3.14 × 10−3 | |
| Non-Diagonal, Class Varying | 1 | 44 | −16,322.3 | 32,732.5 | 32,979.4 | 32,839.7 | NA | NA | NA | NA | 2021 | 100% | 2.55 × 10−3 |
| 2 | 89 | −15,748.0 | 31,674.0 | 32,173.4 | 31,890.6 | 0.000 | 0.000 | 0.000 | 0.567 | 872 | 43% | 3.82 × 10−4 | |
| 3 | 134 | −15,646.4 | 31,560.9 | 32,312.8 | 31,887.1 | 0.107 | 0.108 | 0.000 | 0.700 | 111 | 5% | 8.12 × 10−5 | |
| Variance/Covariance Structure | k | Par | LL | AIC | BIC | aBIC | VLMR-LRT | LMR-LRT | BLRT | Entropy | Smallest Class | Condition # | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p-Value | p-Value | p-Value | n | % | |||||||||
| Non-Diagonal, Class Invariant | 1 | 44 | −18,177.9 | 36,443.8 | 36,690.2 | 36,550.4 | NA | NA | NA | NA | 2000 | 100% | 1.88 × 10−3 |
| 2 | 53 | −18,064.4 | 36,234.8 | 36,531.6 | 36,363.3 | 0.000 | 0.000 | 0.000 | 0.779 | 317 | 16% | 1.56 × 10−3 | |
| 3 | 62 | −17,873.2 | 35,870.4 | 36,217.6 | 36,020.7 | 0.002 | 0.002 | 0.000 | 0.952 | 181 | 9% | 4.88 × 10−9 | |
| 4 | 71 | −17,449.5 | 35,040.9 | 35,438.6 | 35,213.0 | 0.000 | 0.000 | 0.000 | 0.971 | 169 | 8% | 9.40 × 10−12 | |
| 5 | 80 | −17,340.4 | 34,840.8 | 35,288.9 | 35,034.7 | 0.027 | 0.028 | 0.000 | 0.956 | 42 | 2% | 6.72 × 10−14 | |
| 6 | 89 | −17,101.6 | 34,381.3 | 34,879.8 | 34,597.0 | 0.210 | 0.214 | 0.000 | 0.977 | 12 | 1% | 7.31 × 10−16 | |
| Diagonal, Class Invariant | 1 | 16 | −21,822.8 | 43,677.6 | 43,767.2 | 43,716.4 | NA | NA | NA | NA | 2000 | 100% | 1.73 × 10−2 |
| 2 | 25 | −19,516.7 | 39,083.4 | 39,223.5 | 39,144.0 | 0.000 | 0.000 | 0.000 | 0.860 | 672 | 34% | 3.46 × 10−2 | |
| 3 | 34 | −18,651.1 | 37,370.3 | 37,560.7 | 37,452.7 | 0.000 | 0.000 | 0.000 | 0.844 | 267 | 13% | 9.08 × 10−3 | |
| 4 | 43 | −18,309.1 | 36,704.3 | 36,945.1 | 36,808.5 | 0.000 | 0.000 | 0.000 | 0.833 | 198 | 10% | 2.62 × 10−3 | |
| 5 | 52 | −18,203.7 | 36,511.5 | 36,802.7 | 36,637.5 | 0.036 | 0.037 | 0.000 | 0.823 | 80 | 4% | 6.78 × 10−4 | |
| 6 | 61 | −18,122.4 | 36,366.9 | 36,708.5 | 36,514.7 | 0.002 | 0.002 | 0.000 | 0.796 | 77 | 4% | 5.03 × 10−4 | |
| 7 | 70 | −18,034.2 | 36,208.5 | 36,600.5 | 36,378.1 | 0.412 | 0.418 | 0.000 | 0.861 | 92 | 4.6% | 2.77 × 10−6 | |
| Diagonal, Class Varying | 1 | 16 | −21,822.8 | 43,677.6 | 43,767.2 | 43,716.4 | NA | NA | NA | NA | 2000 | 100% | 1.73 × 10−2 |
| 2 | 33 | −19,350.8 | 38,767.6 | 38,952.4 | 38,847.6 | 0.000 | 0.000 | 0.000 | 0.846 | 820 | 41% | 2.14 × 10−2 | |
| 3 | 50 | −18,510.2 | 37,120.4 | 37,400.5 | 37,241.6 | 0.020 | 0.021 | 0.000 | 0.841 | 310 | 16% | 8.48 × 10−3 | |
| Non-Diagonal, Class Varying | 1 | 44 | −18,177.9 | 36,443.8 | 36,690.2 | 36,550.4 | NA | NA | NA | NA | 2000 | 100% | 1.88 × 10−3 |
| Post-COVID | ||||||
|---|---|---|---|---|---|---|
| Low Symptoms (12%) | Mild Symptoms (42%) | Moderate Symptoms (32%) | High Symptoms (11%) | Severe Symptoms (4%) | ||
| Pre-COVID | Transition probabilities | |||||
| Low symptoms (12%) | 0.67 | 0.23 | 0.08 | 0.03 | 0.00 | |
| Mild symptoms (39%) | 0.02 | 0.81 | 0.14 | 0.03 | 0.00 | |
| Moderate symptoms (33%) | 0.00 | 0.09 | 0.79 | 0.12 | 0.01 | |
| High symptoms (11%) | 0.00 | 0.04 | 0.23 | 0.70 | 0.03 | |
| Severe symptoms (5%) | 0.01 | 0.06 | 0.20 | 0.34 | 0.39 | |
| Transition proportions (%) | ||||||
| Low symptoms (12%) | 10.14% | 1.34% | 0.36% | 0.05% | 0.00% | |
| Mild symptoms (39%) | 1.85% | 33.52% | 3.50% | 0.77% | 0.26% | |
| Moderate symptoms (33%) | 0.26% | 3.50% | 25.49% | 3.30% | 0.36% | |
| High symptoms (11%) | 0.00% | 0.46% | 2.21% | 7.11% | 0.82% | |
| Severe symptoms (5%) | 0.05% | 0.21% | 0.57% | 0.88% | 2.99% | |
| Attachment to pets (X2) | ||||||
| Low symptoms (12%) | a | −0.87 | 0.35 | 16.06 b | 0.26 b | |
| Mild symptoms (39%) | a | −0.21 | −0.23 | 18.52 | 0.79 | |
| Moderate symptoms (33%) | a | −12.51 *** | −13.18 *** | −13.35 *** | −12.02 *** | |
| High symptoms (11%) | a | −5.34 b | −4.13 *** | −4.79 *** | −5.76 *** | |
| Severe symptoms (5%) | a | −22.29 b | −22.83 *** | −22.58 *** | −21.37 *** | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
McDonald, S.E.; O’Connor, K.E.; Matijczak, A.; Tomlinson, C.A.; Applebaum, J.W.; Murphy, J.L.; Zsembik, B.A. Attachment to Pets Moderates Transitions in Latent Patterns of Mental Health Following the Onset of the COVID-19 Pandemic: Results of a Survey of U.S. Adults. Animals 2021, 11, 895. https://doi.org/10.3390/ani11030895
McDonald SE, O’Connor KE, Matijczak A, Tomlinson CA, Applebaum JW, Murphy JL, Zsembik BA. Attachment to Pets Moderates Transitions in Latent Patterns of Mental Health Following the Onset of the COVID-19 Pandemic: Results of a Survey of U.S. Adults. Animals. 2021; 11(3):895. https://doi.org/10.3390/ani11030895
Chicago/Turabian StyleMcDonald, Shelby E., Kelly E. O’Connor, Angela Matijczak, Camie A. Tomlinson, Jennifer W. Applebaum, Jennifer L. Murphy, and Barbara A. Zsembik. 2021. "Attachment to Pets Moderates Transitions in Latent Patterns of Mental Health Following the Onset of the COVID-19 Pandemic: Results of a Survey of U.S. Adults" Animals 11, no. 3: 895. https://doi.org/10.3390/ani11030895
APA StyleMcDonald, S. E., O’Connor, K. E., Matijczak, A., Tomlinson, C. A., Applebaum, J. W., Murphy, J. L., & Zsembik, B. A. (2021). Attachment to Pets Moderates Transitions in Latent Patterns of Mental Health Following the Onset of the COVID-19 Pandemic: Results of a Survey of U.S. Adults. Animals, 11(3), 895. https://doi.org/10.3390/ani11030895







