Chronic Wasting Due to Liver and Rumen Flukes in Sheep
Abstract
Simple Summary
Abstract
1. Introduction
2. Fasciolidae with Emphasis on the Common Liver Fluke
2.1. Distribution of and Anatomical Differences between Fasciola Species
2.2. Life Cycle of Fasciola spp.
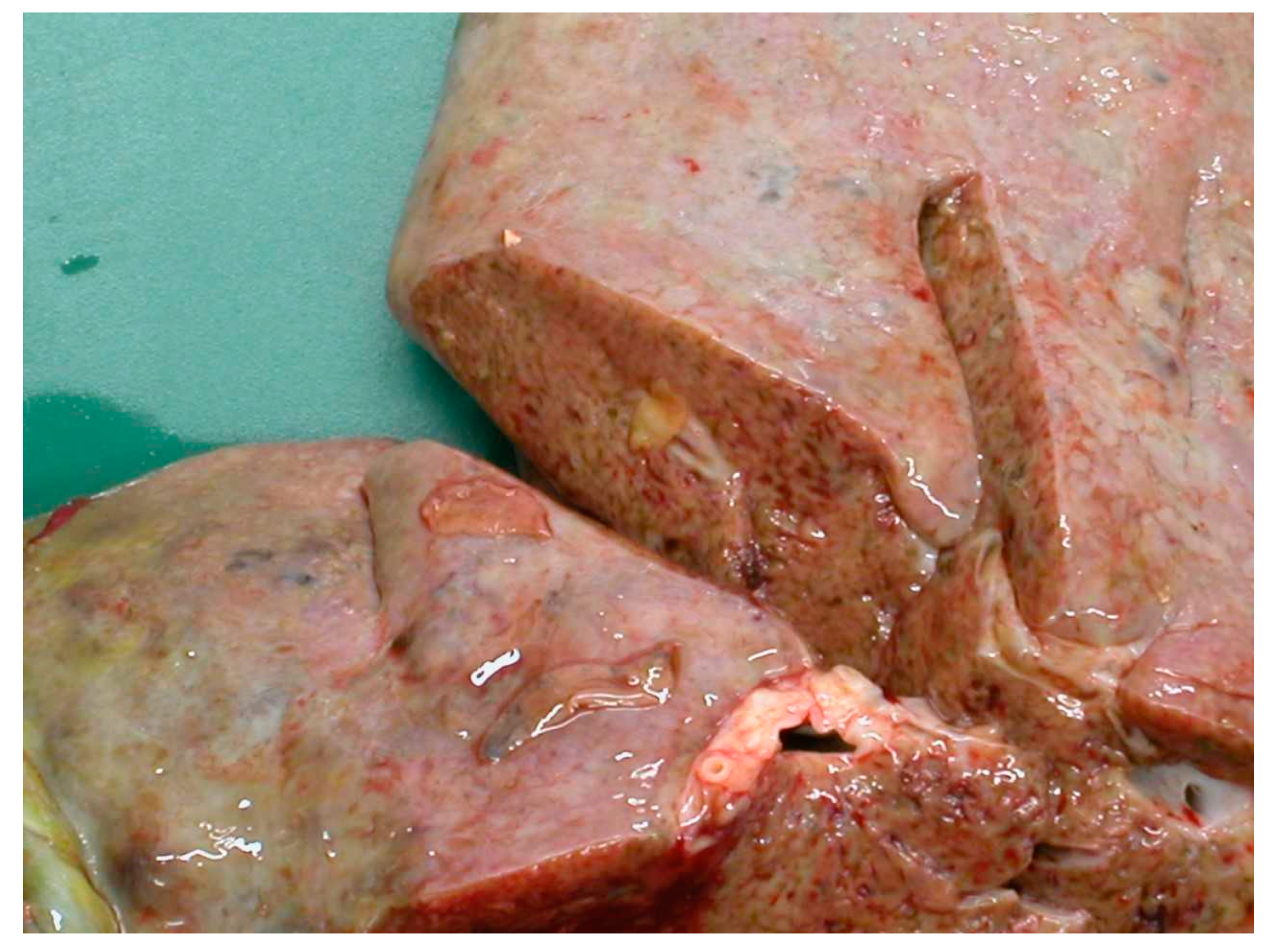
2.3. Clinical Features of Fasciolosis
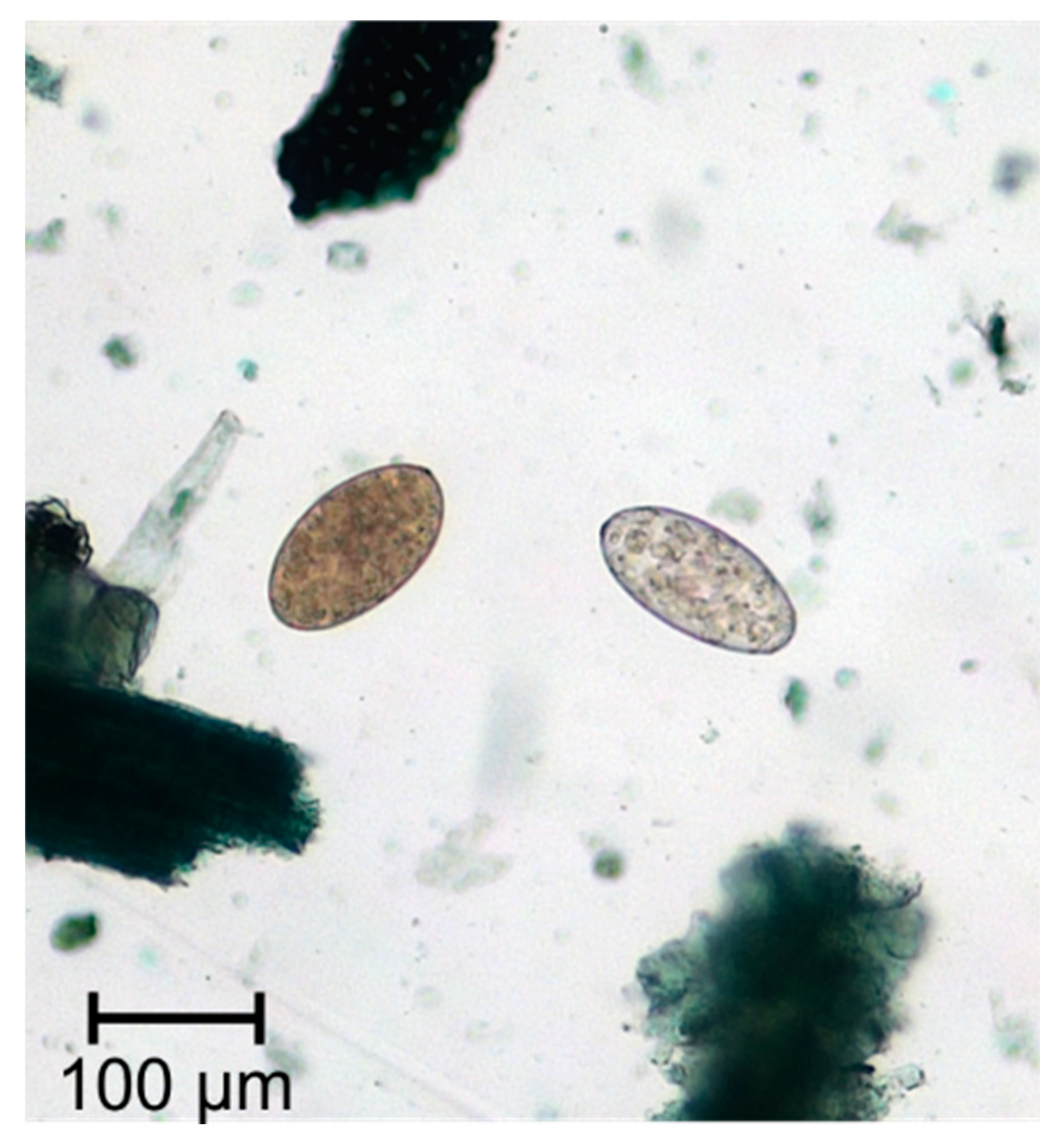
2.4. Diagnosis of Fasciola spp.
2.5. Treatment of Fasciola spp. and Drug Resistance
2.6. Make Use of Genomic Resources to Unravel Resistance Mechanisms
2.7. Strategies towards a Fasciola Vaccince
3. Dicrocoelium spp. (Lancet Flukes)
3.1. Dicrocoelium Species and Their Global Distribution
3.2. Life Cycle of Dicrocoelium Dendriticum
3.3. Clinical Features of Dicrocoeliosis
3.4. Diagnosis of Dicrocoelium Infections
3.5. Treatment and Prevention of Dicrocoeliosis
3.6. Genomic Resources and Their Potential Use for Control of Dicrocoelium spp. Infections in Livestock
4. Paramphistomidae as Rumen and Liver Flukes
4.1. Species and Distribution of Paramphistomidae
4.2. Life Cycle of Paramphistomidae
4.3. Epidemiology and Clinical Features of Infections with Paramphistomidae
4.4. Diagnosis of Rumen Flukes
4.5. Treatment and Prevention of Rumen Fluke Infections
4.6. Available Omics Data on Rumen Fluke
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cribb, T.H.; Bray, R.A.; Olson, P.D.; Littlewood, D.T. Life cycle evolution in the digenea: A new perspective from phylogeny. Adv. Parasitol. 2003, 54, 197–254. [Google Scholar] [PubMed]
- Mas-Coma, S.; Valero, M.A.; Bargues, M.D. Effects of climate change on animal and zoonotic helminthiases. Rev. Sci. Tech. 2008, 27, 443–457. [Google Scholar] [CrossRef]
- Morley, N.J.; Lewis, J.W. Thermodynamics of cercarial development and emergence in trematodes. Parasitology 2013, 140, 1211–1224. [Google Scholar] [CrossRef]
- Rojo-Vázquez, F.A.; Meana, A.; Valcárcel, F.; Martínez-Valladares, M. Update on trematode infections in sheep. Vet. Parasitol. 2012, 189, 15–38. [Google Scholar] [CrossRef]
- Walker, S.M.; Johnston, C.; Hoey, E.M.; Fairweather, I.; Borgsteede, F.H.; Gaasenbeek, C.P.; Prodohl, P.A.; Trudgett, A. Potential role of hares in the spread of liver fluke in the Netherlands. Vet. Parasitol. 2011, 177, 179–181. [Google Scholar] [CrossRef]
- Charlier, J.; Rinaldi, L.; Musella, V.; Ploeger, H.W.; Chartier, C.; Vineer, H.R.; Hinney, B.; von Samson-Himmelstjerna, G.; Băcescu, B.; Mickiewicz, M.; et al. Initial assessment of the economic burden of major parasitic helminth infections to the ruminant livestock industry in Europe. Prev. Vet. Med. 2020, 182, 105103. [Google Scholar] [CrossRef] [PubMed]
- Mas-Coma, S.; Bargues, M.D.; Valero, M.A. Diagnosis of human fascioliasis by stool and blood techniques: Update for the present global scenario. Parasitology 2014, 141, 1918–1946. [Google Scholar] [CrossRef]
- Mas-Coma, S.; Valero, M.A.; Bargues, M.D. Fasciola, lymnaeids and human fascioliasis, with a global overview on disease transmission, epidemiology, evolutionary genetics, molecular epidemiology and control. Adv. Parasitol. 2009, 69, 41–146. [Google Scholar]
- Deplazes, P.; Eckert, J.; von Samson-Himmelstjerna, G.; Zahner, H.; Joachim, A.; Mathis, A.; Taubert, A.; Strube, C. Parasitologie für die Tiermedizin, 4th ed.; Thieme-Verlag: Stuttgart, Germany, 2020; p. 172ff. [Google Scholar]
- Taylor, M.A.; Coop, R.L.; Wall, R.L. Veterinary Parasitology, 4th ed.; Wiley-Blackwell: Chichester, UK, 2016; pp. 74–80, 84–85, 383–387. [Google Scholar]
- Fairweather, I.; Brennan, G.P.; Hanna, R.E.B.; Robinson, M.W.; Skuce, P.J. Drug resistance in liver flukes. Int. J. Parasitol. Drugs Drug Resist. 2020, 12, 39–59. [Google Scholar] [CrossRef]
- Calvani, N.E.D. and J. Šlapeta. Fasciola Species Introgression: Just a Fluke or Something More? Trends Parasitol. 2020, 37, 25–34. [Google Scholar]
- Cwiklinski, K.; O’Neill, S.M.; Donnelly, S.; Dalton, J.P. A prospective view of animal and human Fasciolosis. Parasite Immunol. 2016, 38, 558–568. [Google Scholar] [CrossRef]
- Howell, A.K.; Williams, D.J.L. The Epidemiology and Control of Liver Flukes in Cattle and Sheep. Vet. Clin. N. Am Food Anim. Pract. 2020, 36, 109–123. [Google Scholar] [CrossRef]
- Dixon, K.E. The physiology of excystment of the metacercaria of Fasciola hepatica L. Parasitology 1966, 56, 431–456. [Google Scholar] [CrossRef]
- Forbes, A. Liver fluke infections in cattle and sheep. Livestock 2017, 22, 250–256. [Google Scholar] [CrossRef][Green Version]
- Naveed, A.; Shahzad, A.K.; Tunio, M.T. Incidence of liver fluke infestation and pathological examination in sheep (Ovis aries) in Mirpur Azad Jammu and Kashmir. PAB 2019, 8, 750–761. [Google Scholar]
- Rushton, B.; Murray, M. Hepatic pathology of a primary experimental infection of Fasciola hepatica in sheep. J. Comp. Pathol. 1977, 87, 459–470. [Google Scholar] [CrossRef]
- Williams, D. Update on liver fluke in sheep. Practice 2020, 42, 341–347. [Google Scholar] [CrossRef]
- Kozat, S.; Denizhan, V. Glucose, lipid, and lipoprotein levels in sheep naturally infected with Fasciola hepatica. J. Parasitol. 2010, 96, 657–659. [Google Scholar] [CrossRef]
- Blood, D.C.; Radostits, O.M.; Arundel, J.H.; Gay, C.C. Diseases caused by helminth parasites. In Veterinary Medicine: A Textbook of the Diseases of Cattle, Sheep, Pigs, Goats and Horses, 7th ed.; Bailliere Tindall: London, UK, 1989; pp. 1016–1028. [Google Scholar]
- Hawkins, C.D.; Morris, R.S. Depression of productivity in sheep infected with Fasciola hepatica. Vet. Parasitol. 1978, 4, 341–351. [Google Scholar] [CrossRef]
- Sargison, N.D.; Scott, P.R. Diagnosis and economic consequences of triclabendazole resistance in Fasciola hepatica in a sheep flock in south-east Scotland. Vet. Record. 2011, 168, 159. [Google Scholar] [CrossRef]
- Sargison, N.D. Fluke diseases of UK ruminant livestock Part 1: Life cycles, economic consequences and diagnosis. UK Vet. Livest. 2008, 13, 59–67. [Google Scholar] [CrossRef]
- Al-Saffar, T.M. Some haematological changes in sheep with chronic fascioliasis in Mosul. AL-Qadisiyah J. Vet. Med. Sci. 2008, 7, 6–9. [Google Scholar]
- Von Samson-Himmelstjerna, G.; Hiepe, T. Paramphistomose. In Klinik der Schaf-und Ziegenkrankheiten, 1st ed.; Bostedt, H., Ganter, M., Hiepe, T., Eds.; Georg Thieme Verlag: Stuttgart, Germany, 2018. [Google Scholar]
- Fouda, T.; Youssef Mohammed, A.; Al-Ashkar, M.R. Chronic Fascioliasis as Cause of Unthriftiness in Sheep with Reference to its Impacts on Blood Constituents. J. Anim. Res. 2013, 3, 209–221. [Google Scholar]
- Mavrogianni, V.S.; Papadopoulos, E.; Spanos, S.A.; Mitsoura, A.; Ptochos, S.; Gougoulis, D.A.; Barbagianni, M.S.; Kyriazakis, I.; Fthenakis, G.C. Trematode infections in pregnant ewes can predispose to mastitis during the subsequent lactation period. Res. Vet. Sci. 2014, 96, 171–179. [Google Scholar] [CrossRef]
- Joachim, A.; Ali, S.F.; Daugschies, A. Fasciola hepatica alters coagulation parameters in sheep plasma in vivo and in vitro. Parasitol. Res. 2003, 89, 53–58. [Google Scholar]
- Flanagan, A.M.; Edgar, H.W.; Forster, F.; Gordon, A.; Hanna, R.E.; McCoy, M.; Brennan, G.P.; Fairweather, I. Standardisation of a coproantigen reduction test (CRT) protocol for the diagnosis of resistance to triclabendazole in Fasciola hepatica. Vet. Parasitol. 2011, 176, 34–42. [Google Scholar] [CrossRef]
- Arifin, M.I.; Höglund, J.; Novobilský, A. Comparison of molecular and conventional methods for the diagnosis of Fasciola hepatica infection in the field. Vet. Parasitol. 2016, 232, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Gordon, D.K.; Zadoks, R.N.; Stevenson, H.; Sargison, N.D.; Skuce, P.J. On farm evaluation of the coproantigen ELISA and coproantigen reduction test in Scottish sheep naturally infected with Fasciola hepatica. Vet. Parasitol. 2012, 187, 436–444. [Google Scholar] [CrossRef]
- Hanna, R.E.; McMahon, C.; Ellison, S.; Edgar, H.W.; Kajugu, P.E.; Gordon, A.; Irwin, D.; Barley, J.P.; Malone, F.E.; Brennan, G.P.; et al. Fasciola hepatica: A comparative survey of adult fluke resistance to triclabendazole, nitroxynil and closantel on selected upland and lowland sheep farms in Northern Ireland using faecal egg counting, coproantigen ELISA testing and fluke histology. Vet. Parasitol. 2015, 207, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Afshan, K.; Qayyum, M.; Rizvi, S.S.R.; Mukhtar, M.; Mushtaq, M.; Miller, J.E. Serological and coprological comparison for rapid diagnosis of Fasciola hepatica infection in small ruminants from sub-tropical area of Pakistan. Small Ruminant Res. 2013, 113, 267–272. [Google Scholar] [CrossRef]
- Reichel, M.P. Performance characteristics of an enzyme-linked immunosorbent assay for the detection of liver fluke (Fasciola hepatica) infection in sheep and cattle. Vet. Parasitol. 2002, 107, 65–72. [Google Scholar] [CrossRef]
- Molloy, J.B.; Anderson, G.R.; Fletcher, T.I.; Landmann, J.; Knight, B.C. Evaluation of a commercially available enzyme-linked immunosorbent assay for detecting antibodies to Fasciola hepatica and Fasciola gigantica in cattle, sheep and buffaloes in Australia. Vet. Parasitol. 2005, 130, 207–212. [Google Scholar] [CrossRef]
- Overend, D.J.; Bowen, F.L. Resistance of Fasciola hepatica to triclabendazole. Aust. Vet. J. 1995, 72, 275–276. [Google Scholar] [CrossRef] [PubMed]
- McNulty, S.N.; Tort, J.F.; Rinaldi, G.; Fischer, K.; Rosa, B.A.; Smircich, P.; Fontenla, S.; Choi, Y.J.; Tyagi, R.; Hallsworth-Pepin, K.; et al. Genomes of Fasciola hepatica from the Americas Reveal Colonization with Neorickettsia Endobacteria Related to the Agents of Potomac Horse and Human Sennetsu Fevers. PLoS Genet. 2017, 13, e1006537. [Google Scholar] [CrossRef]
- Cwiklinski, K.; Dalton, J.P.; Dufresne, P.J.; La Course, J.; Williams, D.J.; Hodgkinson, J.; Paterson, S. The Fasciola hepatica genome: Gene duplication and polymorphism reveals adaptation to the host environment and the capacity for rapid evolution. Genome Biol. 2015, 16, 71. [Google Scholar] [CrossRef]
- Pandey, T.; Ghosh, A.; Todur, V.N.; Rajendran, V.; Kalita, P.; Kalita, J.; Shukla, R.; Chetri, P.B.; Shukla, H.; Sonkar, A.; et al. Draft Genome of the Liver Fluke Fasciola gigantica. ACS Omega 2020, 5, 11084–11091. [Google Scholar] [CrossRef] [PubMed]
- McVeigh, P.; McCammick, E.; McCusker, P.; Wells, D.; Hodgkinson, J.; Paterson, S.; Mousley, A.; Marks, N.J.; Maule, A.G. Profiling G protein-coupled receptors of Fasciola hepatica identifies orphan rhodopsins unique to phylum Platyhelminthes. Int. J. Parasitol. Drugs Drug Resist. 2018, 8, 87–103. [Google Scholar] [CrossRef] [PubMed]
- Kotze, A.C.; Hunt, P.W.; Skuce, P.; von Samson-Himmelstjerna, G.; Martin, R.J.; Sager, H.; Krücken, J.; Hodgkinson, J.; Lespine, A.; Jex, A.R.; et al. Recent advances in candidate-gene and whole-genome approaches to the discovery of anthelmintic resistance markers and the description of drug/receptor interactions. Int. J. Parasitol. Drugs Drug Resist. 2014, 4, 164–184. [Google Scholar] [CrossRef]
- Beesley, N.J.; Caminade, C.; Charlier, J.; Flynn, R.J.; Hodgkinson, J.E.; Martinez-Moreno, A.; Martinez-Valladares, M.; Perez, J.; Rinaldi, L.; Williams, D.J.L. Fasciola and fasciolosis in ruminants in Europe: Identifying research needs. Transbound. Emerg. Dis. 2018, 65, 199–216. [Google Scholar] [CrossRef]
- Zafra, R.; Buffoni, L.; Pérez-Caballero, R.; Molina-Hernández, V.; Ruiz-Campillo, M.T.; Pérez, J.; Martínez-Moreno, Á.; Martínez Moreno, F.J. Efficacy of a multivalent vaccine against Fasciola hepatica infection in sheep. Vet. Res. 2021, 52, 13. [Google Scholar] [CrossRef]
- Flynn, R.J.; Mulcahy, G.; Elsheikha, H.M. Coordinating innate and adaptive immunity in Fasciola hepatica infection: Implications for control. Vet. Parasitol. 2010, 169, 235–240. [Google Scholar] [CrossRef]
- Toet, H.; Piedrafita, D.M.; Spithill, T.W. Liver fluke vaccines in ruminants: Strategies, progress and future opportunities. Int. J. Parasitol. 2014, 44, 915–927. [Google Scholar] [CrossRef]
- van Riet, E.; Hartgers, F.C.; Yazdanbakhsh, M. Chronic helminth infections induce immunomodulation: Consequences and mechanisms. Immunobiology 2007, 21, 475–490. [Google Scholar] [CrossRef]
- McManus, D.P. Recent Progress in the Development of Liver Fluke and Blood Fluke Vaccines. Vaccines 2020, 8, 553. [Google Scholar] [CrossRef]
- Piacenza, L.; Acosta, D.; Basmadjian, I.; Dalton, J.P.; Carmona, C. Vaccination with cathepsin L proteinases and with leucine aminopeptidase induces high levels of protection against fascioliasis in sheep. Infect. Immun. 1999, 67, 1954–1961. [Google Scholar] [CrossRef] [PubMed]
- Maggioli, G.; Acosta, D.; Silveira, F.; Rossi, S.; Giacaman, S.; Basika, T.; Gayo, V.; Rosadilla, D.; Roche, L.; Tort, J.; et al. The recombinant gut-associated M17 leucine aminopeptidase in combination with different adjuvants confers a high level of protection against Fasciola hepatica infection in sheep. Vaccine. 2011, 29, 9057–9063. [Google Scholar] [CrossRef]
- Acosta, D.; Cancela, M.; Piacenza, L.; Roche, L.; Carmona, C.; Tort, J.F. Fasciola hepatica leucine aminopeptidase, a promising candidate for vaccination against ruminant fasciolosis. Mol. Biochem. Parasitol. 2008, 158, 52–64. [Google Scholar] [CrossRef]
- Dominguez, M.F.; González-Miguel, J.; Carmona, C.; Dalton, J.P.; Cwiklinski, K.; Tort, J.; Siles-Lucas, M. Low allelic diversity in vaccine candidate genes from different locations sustain hope for Fasciola hepatica immunization. Vet. Parasitol. 2018, 258, 46–52. [Google Scholar] [CrossRef]
- Otranto, D.; Traversa, D. A review of dicrocoeliosis of ruminants including recent advances in the diagnosis and treatment. Vet. Parasitol. 2002, 107, 317–335. [Google Scholar] [CrossRef]
- Beck, M.; Goater, C.; Colwell, D. Comparative recruitment, morphology and reproduction of a generalist trematode, Dicrocoelium dendriticum, in three species of host. Parasitology 2015, 142, 1297–1305. [Google Scholar] [CrossRef]
- Malek, E.A. Occurrence of Dicrocoelium hospes in Mali and Senegal, West Africa. J. Helminthol. 1980, 54, 45–46. [Google Scholar] [CrossRef] [PubMed]
- Manga-González, M.; Ferreras, M. Dicrocoeliidae Family: Major Species Causing Veterinary Diseases. In Digenetic Trematodes, 2nd ed.; Toledo, R., Fried, B., Eds.; Springer: Cham, Switzerland, 2019; pp. 279–319. ISBN 978-3-030-18615-9. [Google Scholar]
- Manga-González, M.Y.; González-Lanza, C.; Cabanas, E.; Campo, R. Contributions to and review of dicrocoeliosis, with special reference to the intermediate hosts of Dicrocoelium dendriticum. Parasitology 2001, 123, 91–114. [Google Scholar] [CrossRef]
- Mitterer, K.E. Untersuchungen zum Schlüpfen der Miracidien des Kleinen Leberegels Dicrocoelium dendriticum. Z. Parasitenkd. 1975, 48, 35–45. [Google Scholar] [CrossRef]
- Ractliffe, L.H. Hatching of Dicrocoelium lanceolatum eggs. Exp. Parasitol. 1968, 23, 67–78. [Google Scholar] [CrossRef]
- Köse, M.; Eser, M.; Kartal, K.; Bozkurt, M.F. Infections of Larval Stages of Dicrocoelium dendriticum and Brachylaima sp. in Brown Garden Snail, Helix aspersa, in Turkey. Korean J. Parasitol. 2015, 53, 647–651. [Google Scholar] [CrossRef][Green Version]
- Tverdokhlebov, P.T. Significance of different types of pastures in the infection of animals by Dicrocoelium. Byulleten’ Vsesoyuznogo Instituta Gel’ mintologii im. K. I. Skryabina 1970, 4, 147–149. [Google Scholar]
- Manga-González, M.Y.; González-Lanza, C. Field and experimental studies on Dicrocoelium dendriticum and dicrocoeliasis in northern Spain. J. Helminthol. 2005, 79, 291–302. [Google Scholar] [CrossRef]
- Theodoridis, Y.; Duncan, J.L.; MacLean, J.M.; Himonas, C.A. Pathophysiological studies on Dicrocoelium dendriticum infection in sheep. Vet. Parasitol. 1991, 39, 61–66. [Google Scholar] [CrossRef]
- Manga-González, M.Y.; Ferreras, M.C.; Campo, R.; González-Lanza, C.; Pérez, V.; García-Marín, J.F. Hepatic marker enzymes, biochemical parameters and pathological effects in lambs experimentally infected with Dicrocoelium dendriticum (Digenea). Parasitol. Res. 2004, 93, 344–355. [Google Scholar] [CrossRef] [PubMed]
- Calamel, M.; Giauffret, A. Interprétation des résultats dans le diagnostic coproscopique de la dicrocoliose. Rec. Méd. Vét. 1976, 152, 99–104. [Google Scholar]
- Rojo-Vázquez, F.A.; Cordero-del-Campillo, M.; Diez Baños, P.; Chaton-Schaffner, M. Relation existant entre le nombre d’oeufs dans les feces et la charge parasitaire lors des infestations naturelles a Dicrocoelium dendriticum chez les ovins. Rev. Méd. Vét. 1981, 132, 601–607. [Google Scholar]
- Ambrosi, M. La diagnostica coprologica nelle elmintiasi di allevamento: Caso delle distomatosi dei ruminanti. Praxis Vet. 1991, 12, 17–20. [Google Scholar]
- Wolff, K.; Hauser, B.; Wild, P. Dicrocoeliose des Schafes: Untersuchungen zur Pathogenese und zur Regeneration der Leber nach Therapie. Berl. Münch. Tierärztl. Wochenschr. 1984, 97, 378–387. [Google Scholar]
- Hohorst, W.; Lämmler, G. Experimentelle Dicrocoeliose-Studien. Z. Tropenmed. Parasitol. 1962, 13, 377–397. [Google Scholar] [PubMed]
- Sargison, N.D.; Baird, G.J.; Sotiraki, S.; Gilleard, J.S.; Busin, V. Hepatogenous photosensitisation in Scottish sheep casued by Dicrocoelium dendriticum, Vet. Parasitol. 2012, 189, 233–237. [Google Scholar]
- Camara, L.; Pfister, K.; Aeschlimann, A. Analyse histopathologique de foie de bovin infesté par Dicrocoelium dendriticum. Vet. Res. 1996, 27, 87–92. [Google Scholar] [PubMed]
- Rehbein, S.; Kokott, S.; Lindner, T. Evaluation of techniques for the enumeration of Dicrocoelium eggs in sheep faeces. Zent. Vet. A 1999, 46, 133–139. [Google Scholar] [CrossRef]
- Naeemipour, M.; Hashemitabar, G.R.; Dastjerdi, K.; Mojaver, M.J.; Mohammadi, H.R. Comparison of Fecal Egg Counts and ELISA for the diagnosis of Dicrocoelium dendriticum Infection. Pol. J. Vet. Sci. 2016, 19, 573–580. [Google Scholar] [CrossRef]
- González-Lanza, C.; Manga-González, M.Y.; Campo, R.; Del-Pozo, P.; Sandoval, H.; Oleaga, A.; Ramajo, V. IgG antibody response to ES or somatic antigens of Dicrocoelium dendriticum (Trematoda) in experimentally infected sheep. Parasitol. Res. 2000, 86, 472–479. [Google Scholar] [CrossRef]
- Onar, E. Efficacy of thiophanate and albendazole against natural infections of Dicrocoelium dendriticum, Fasciola hepatica, and gastrointestinal nematodes and cestodes in sheep, and gastrointestinal nematodes and cestodes in sheep. Vet. Parasitol. 1990, 35, 139–145. [Google Scholar] [CrossRef]
- Güralp, N.; Tinar, R. Trematodiasis in Turkey: Comparative efficacy of triclabendazole and niclofolan against natural infections of Fasciola hepatica and F. gigantica in sheep. J. Helminthol. 1984, 58, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Camlitepe, Y.; Aksoy, V. Distribution and Conservation Status of the European Red Wood Ant Species Formica pratensis Retzius, 1783 (Hymenoptera, Formicidae) in (European) Turkey. J. Entomol. Res. Soc. 2019, 21, 199–211. [Google Scholar]
- Manga-González, M.; Quiroz-Romero, H.; Gonzalez-Lanza, C.; Minambres, B.; Ochoa, P. Strategic control of Dicrocoelium dendriticum (Digenea) egg excretion by naturally infected sheep. Vet. Med. 2010, 55, 19–29. [Google Scholar] [CrossRef]
- Horak, I.G. Paramphistomiasis of domestic ruminants. Adv. Parasitol. 1971, 9, 33–72. [Google Scholar] [PubMed]
- Silvestre, A.; Sauvè, C.; Cabaret, J. Caprine Paramphistomum daubneyi (Trematoda) infection in Europe. Vet. Rec. 2000, 146, 674–675. [Google Scholar] [CrossRef] [PubMed]
- Gordon, D.K.; Roberts, L.C.P.; Lean, N. Identification of the rumen fluke, Calicophoron daubneyi, in GB livestock: Possible implications for liver fluke diagnosis. Vet. Parasitol. 2013, 195, 65–71. [Google Scholar] [CrossRef]
- Ferreras, M.C.; Gonzalez-Lanza, C.; Perez, V. Clicophoron daubneyi (Paramphistomidae) in slaughtered cattle in Castilla Y León (Spain). Vet. Parasitol. 2014, 199, 268–271. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Warleta, M.; Lladosa, S.; Castro-Hermida, J.A. Bovine paramphistomosis in Galicia (Spain): Prevalence, intensity, aetiology and geospatioal distribution of the infection. Vet. Parasitol. 2014, 191, 252–263. [Google Scholar] [CrossRef]
- Zintl, A.; Carcia-Campos, A.; Trudgett, A. Bovine paramphistomes in Ireland. Vet. Parasitol. 2014, 204, 199–208. [Google Scholar] [CrossRef]
- Malrait, K.; Verschave, S.; Skuce, P. Novel insights into the pathogenic importance, diagnosis and treatment of the rumen fluke (Caliphoron daubneyi) in cattle. Vet. Parasitol. 2015, 207, 134–139. [Google Scholar] [CrossRef]
- Martinez-Ibeas, A.M.; Munita, M.P.; Lawlor, K.D.; Sekiya, M.; Mulcahy, G.; Sayers, R. Rumen fluke in Irish sheep: Prevalence, risk factors and molecular identification of two paramphistome species. BMC Vet. Res. 2016, 12, 1–11. [Google Scholar] [CrossRef]
- Jones, R.A.; Brophy, P.M.; Mitchell, E.S.; Williams, H.W. Rumen fluke (Calicophoron daubneyi) on Welsh farms: Prevalence, risk factors and observations on co-infection with Fasciola hepatica. Parasitology 2017, 144, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Ploeger, H.W.; Ankum, L.; Moll, L. Presence and species identity of rumen flukes in cattle and sheep in the Netherlands. Vet. Parasitol. 2017, 243, 42–46. [Google Scholar] [CrossRef]
- Wenzel, C.; Küchler, A.; Strube, C.; Knubben-Scheizer, G. Paramphistomidosis—An overview on epidemiology and clinical signs. Tierarztl. Prax. Ausg. G. Grosstiere Nutztiere 2019, 47, 184–191. [Google Scholar]
- Roden, E.; Großmann, T.; Ganter, M. Endoparasitosen bei kleinen Wiederkäuern und Alpakas in Norddeutschland. In Proceedings of the Tagung der DVG-Fachgruppe “Parasitologie und parasitäre Krankheiten”, Hannover, Germany, 12–14 June 2017; ISBN 978-3-86345-372-5. [Google Scholar]
- Deplazes, P.; Eckert, J.; von Samson-Himmelstjerna, G.; Zahner, H. Lehrbuch der Parasitologie für die Tiermedizin, 3rd ed.; Enke-Verlag: Stuttgart, Germany, 2013; p. 152ff. [Google Scholar]
- Rolfe, P.F.; Boray, J.C.; Collins, G.H. Pathology of infection with Paramphistomum ichikawai in sheep. Int. J. Parasitol. 1994, 24, 995–1004. [Google Scholar] [CrossRef]
- Lotfy, W.M.; Brant, S.V.; Ashmawy, K.I.; Devkota, R.; Mkoji, G.M.; Loker, E.S. A molecular approach for identification of paramphistomes from Africa and Asia. Vet. Parasitol. 2010, 174, 234–240. [Google Scholar] [CrossRef]
- Vihan, V.S. Diseases of Small Ruminant, 1st ed.; Satish Serial Publishing House: Delhi, India, 2010; pp. 255–259. [Google Scholar]
- Durie, P.H. The paramphistomes (Trematoda) of Australian ruminants. Aust. J. Zool. 1953, 1, 193–222. [Google Scholar] [CrossRef]
- Wiedosari, E.; Graydon, R.; Copeman, D.B. Comaprative Pathological Study of Hepatic Changes Induced by Fasciola gigantica and Gigantocotyle explanatum in Javanese Thin-tailed Sheep. J. Comp. Path. 1991, 105, 147–155. [Google Scholar] [CrossRef]
- Sreedevi, C.; Devi, V.R.; Annapurna, P.; Malkondaiah, P. Incidence and pathological study of Explanatum explanatum (Creplin, 1847) Fukui, 1929 in goats in Andhra Pradesh, India. J. Parasit. Dis. 2017, 41, 750–753. [Google Scholar] [CrossRef]
- Uddin, M.Z.; Farjana, T.; Begum, N.; Mondal, M.M.H. Prevalence of amphistomes in black Bengal goats in Mymensingh district. Bangl. J. Vet. Med. 2006, 4, 103–106. [Google Scholar] [CrossRef][Green Version]
- Godara, R.; Katoch, R.; Yadav, A.; Rastogi, A. Epidemiology of paramphistomosis in sheep and goats in Jammu, India. J. Parasit. Dis. 2014, 38, 423–428. [Google Scholar] [CrossRef]
- Biggeri, A.; Catelan, D.; Dreassi, E.; Rinaldi, L.; Musella, V.; Veneziano, V.; Cringoli, G. Multivariate spatially-structured variability of ovine helminth infections. Geospat. Health 2007, 2, 97–104. [Google Scholar] [CrossRef]
- Cringoli, G.; Taddei, R.; Rinaldi, L.; Veneziano, V.; Musella, V.; Cascone, C.; Sibilio, G.; Malone, J.B. Use of remote sensing and geographical information systems to identify environmental features that influence the distribution of paramphistomosis in sheep from the southern Italian Apennines. Vet. Parasitol. 2004, 122, 15–26. [Google Scholar] [CrossRef]
- Toolan, D.P.; Mitchell, G.; Searle, K.; Sheehan, M.; Skuce, P.J.; Zadoks, R.N. Bovine and ovine rumen fluke in Ireland—Prevalence, risk factors and species identity based on passive veterinary surveillance and abattoir findings. Vet. Parasitol. 2015, 212, 168–174. [Google Scholar] [CrossRef]
- Boray, J.C. Studies on intestinal amphistomosis in cattle. Aust. Vet. J. 1959, 35, 282–287. [Google Scholar] [CrossRef]
- Millar, M.; Colloff, A.; Scholes, S. Disease associated with immature paramphistome infection. Vet. Rec. 2012, 171, 509–510. [Google Scholar]
- Mason, C.; Stevenson, H.; Cox, A.; Dick, I. Disease associated with immature paramphistome infection in sheep. Vet. Rec. 2013, 170, 343–344. [Google Scholar] [CrossRef]
- Duignan, G.; Fagan, J.; Joyce, C.; Casey, M. Diagnosing acute larval paramphistomosis in ruminants. Vet. Rec. 2017, 180, 618. [Google Scholar]
- Ghatani, S.; Shylla, J.A.; Roy, B.; Tandon, V. Multilocus sequence evaluation for differentiation species of the trematode Family Gastrothylacidae, with a note on the utility of mitochondrial COI motifs in species identification. Gene 2014, 548, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhao, Y.; Wang, L.; Feng, H.; Tan, L.; Lei, W.; Zhao, P.; Hu, M.; Fang, R. Analysis of the complete Fischoederius elongatus (Paramphistomidae, Trematoda) mitochondrial genome. Parasites Vectors 2015, 8, 279. [Google Scholar] [CrossRef]
- Paraud, C.; Gaudin, C.; Pors, I.; Chartier, C. Efficacy of oxyclozanide against the rumen fluke Calicophoron daubneyi in experimentally infected goats. Vet. J. 2009, 180, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Sey, O. A review of chemotherapy of paramphistomosi of domestic ruminants in Europe. Parasites Hung. 1989, 22, 51–55. [Google Scholar]
- Arias, M.S.; Sanchis, J.; Francisco, I.; Francisco, R.; Pineiro, P.; Cazapal-Monteiro, C.; Cortinas, F.J.; Suárez, J.L.; Sánchez-Andrade, R.; Paz-Silva, A. The efficacy of four anthelmintics against Calicophoron daubneyi in naturally infected dairy cattle. Vet. Parasitol. 2013, 197, 126–129. [Google Scholar] [CrossRef]
- Dewilde, S.; Ioanitescu, A.I.; Kiger, L.; Gilany, K.; Marden, M.C.; Van Doorslaer, S.; Vercruysse, J.; Pesce, A.; Nardini, M.; Bolognesi, M.; et al. The hemoglobins of the trematodes Fasciola hepatica and Paramphistomum epiclitum: A molecular biological, physico-chemical, kinetic, and vaccination study. Protein Sci. 2008, 17, 1653–1662. [Google Scholar] [CrossRef]
- Choudhary, V.; Garg, S.; Chourasia, R.; Hasnani, J.J.; Patel, P.V.; Shah, T.M.; Bhatt, V.D.; Mohapatra, A.; Blake, D.P.; Joshi, C.G. Transcriptome analysis of the adult rumen fluke Paramphistomum cervi following next generation sequencing. Gene 2015, 570, 64–70. [Google Scholar] [CrossRef]
- Huson, K.M.; Atcheson, E.; Oliver, N.A.M.; Best, P.; Barley, J.P.; Hanna, R.E.B.; McNeilly, T.N.; Fang, Y.; Haldenby, S.; Paterson, S.; et al. Transcriptome and secretome analysis of intra-mammalian life-stages of the emerging helminth pathogen, Calicophoron daubneyi reveals adaptation to a unique host environment. Mol. Cell. Proteom. 2020, in press. [Google Scholar]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kahl, A.; von Samson-Himmelstjerna, G.; Krücken, J.; Ganter, M. Chronic Wasting Due to Liver and Rumen Flukes in Sheep. Animals 2021, 11, 549. https://doi.org/10.3390/ani11020549
Kahl A, von Samson-Himmelstjerna G, Krücken J, Ganter M. Chronic Wasting Due to Liver and Rumen Flukes in Sheep. Animals. 2021; 11(2):549. https://doi.org/10.3390/ani11020549
Chicago/Turabian StyleKahl, Alexandra, Georg von Samson-Himmelstjerna, Jürgen Krücken, and Martin Ganter. 2021. "Chronic Wasting Due to Liver and Rumen Flukes in Sheep" Animals 11, no. 2: 549. https://doi.org/10.3390/ani11020549
APA StyleKahl, A., von Samson-Himmelstjerna, G., Krücken, J., & Ganter, M. (2021). Chronic Wasting Due to Liver and Rumen Flukes in Sheep. Animals, 11(2), 549. https://doi.org/10.3390/ani11020549






