In Vitro Reduction of Interleukin-8 Response to Enterococcus faecalis by Escherichia coli Strains Isolated from the Same Polymicrobial Urines
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients, Urinary Specimens and Bacterial Strains
2.2. Cells Culture
2.3. Interleukin-8 Stimulation Assay
2.4. ELISA
2.5. Generation of UPEC Mutants
2.6. MIC Determination to Ciprofloxacin of UPEC Strains
2.7. Biotypes and Virulence Genotyping/Phenotyping of UPEC Strains
2.8. Sequencing of gyrA QRDR of UPEC Strains
2.9. Statistical Analysis
3. Results
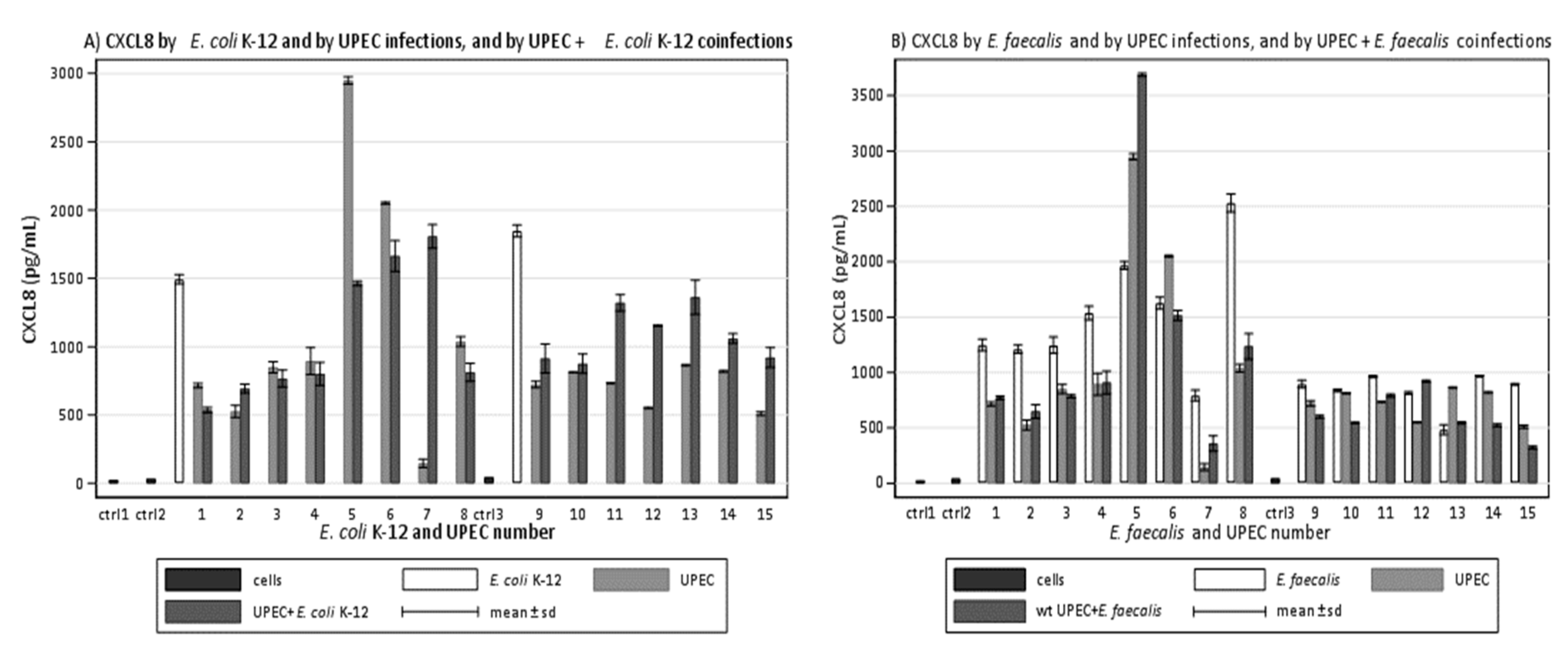
3.1. Clinical UPEC Induce Less CXCL8 Than E. coli K-12 during In Vitro Infections
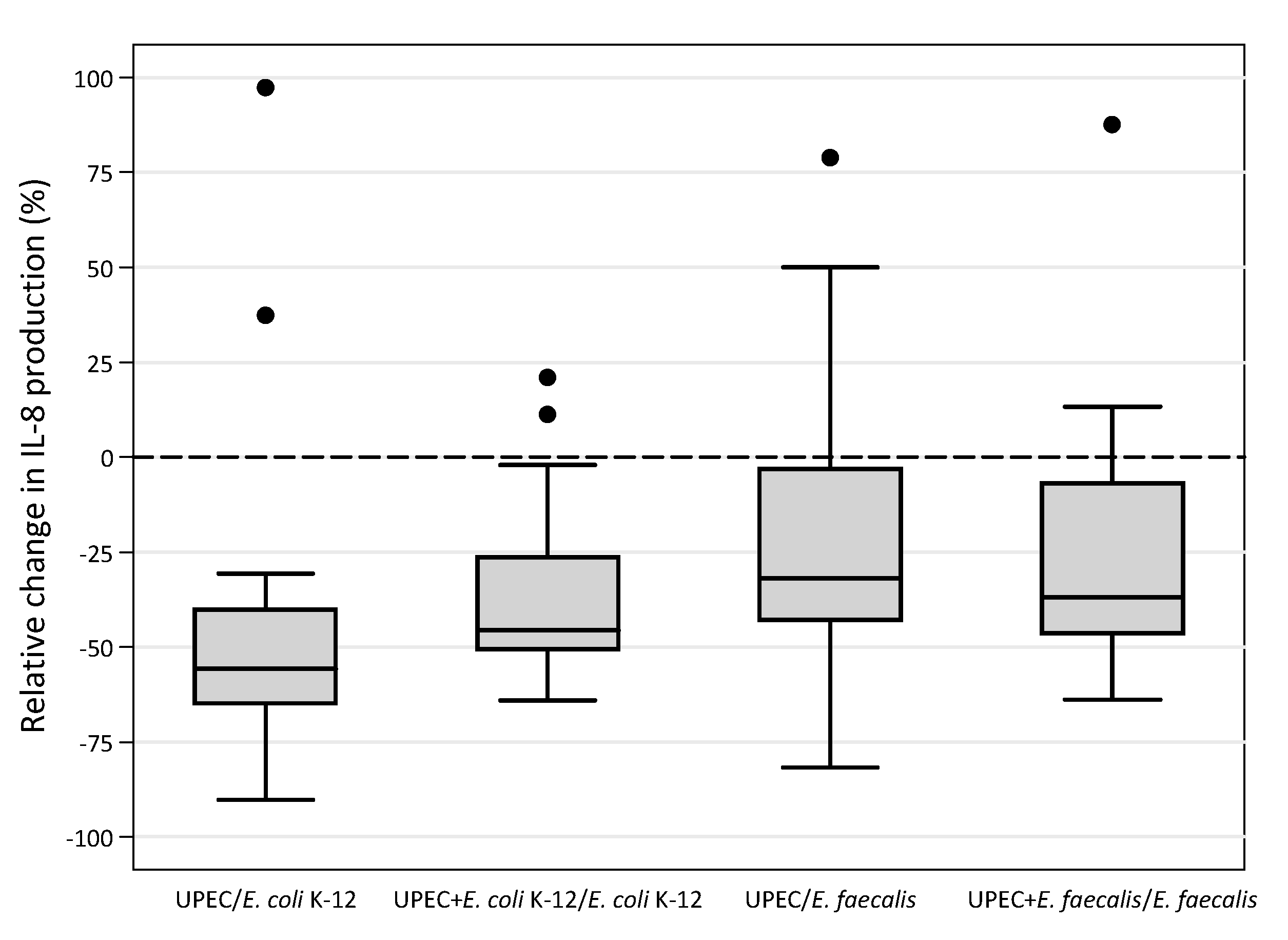
3.2. Clinical UPEC Limit CXCL8 Induced by E. coli K-12 during In Vitro Coinfections
3.3. Clinical UPEC Induce Less CXCL8 Than Clinical E. faecalis during In Vitro Infections
3.4. Clinical UPEC Limit CXCL8 Induced by Clinical E. faecalis during In Vitro Coinfections
3.5. Effect of Treatment with Ciprofloxacin on Ciprofloxacin Susceptibility and Virulence Factors of UPEC
3.6. Mutations in the QRDR of gyrA of Seven UPEC Induced to FQ Resistance
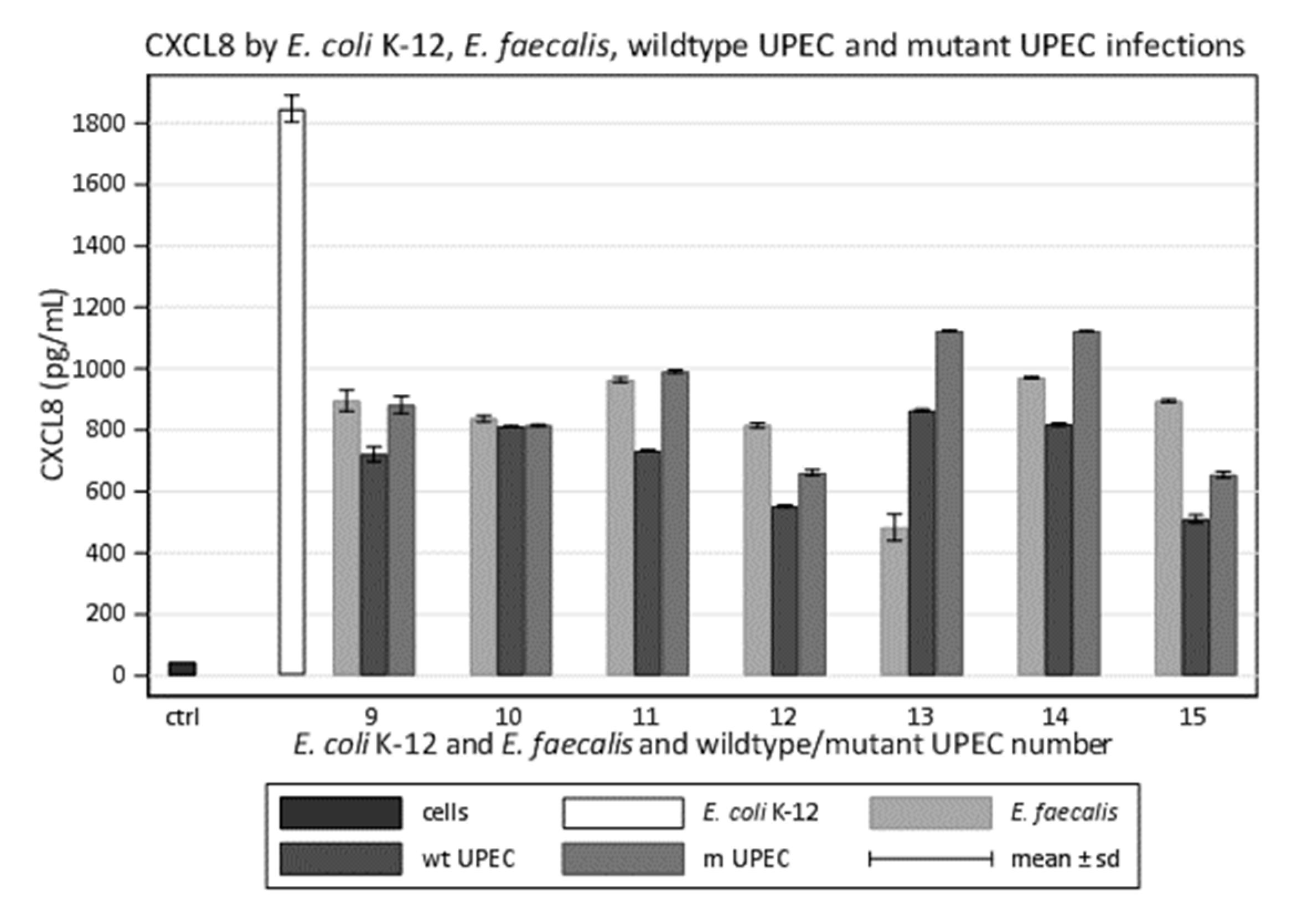
3.7. UPEC Mutants Induce More CXCL8 Than Wildtypes during In Vitro Infections
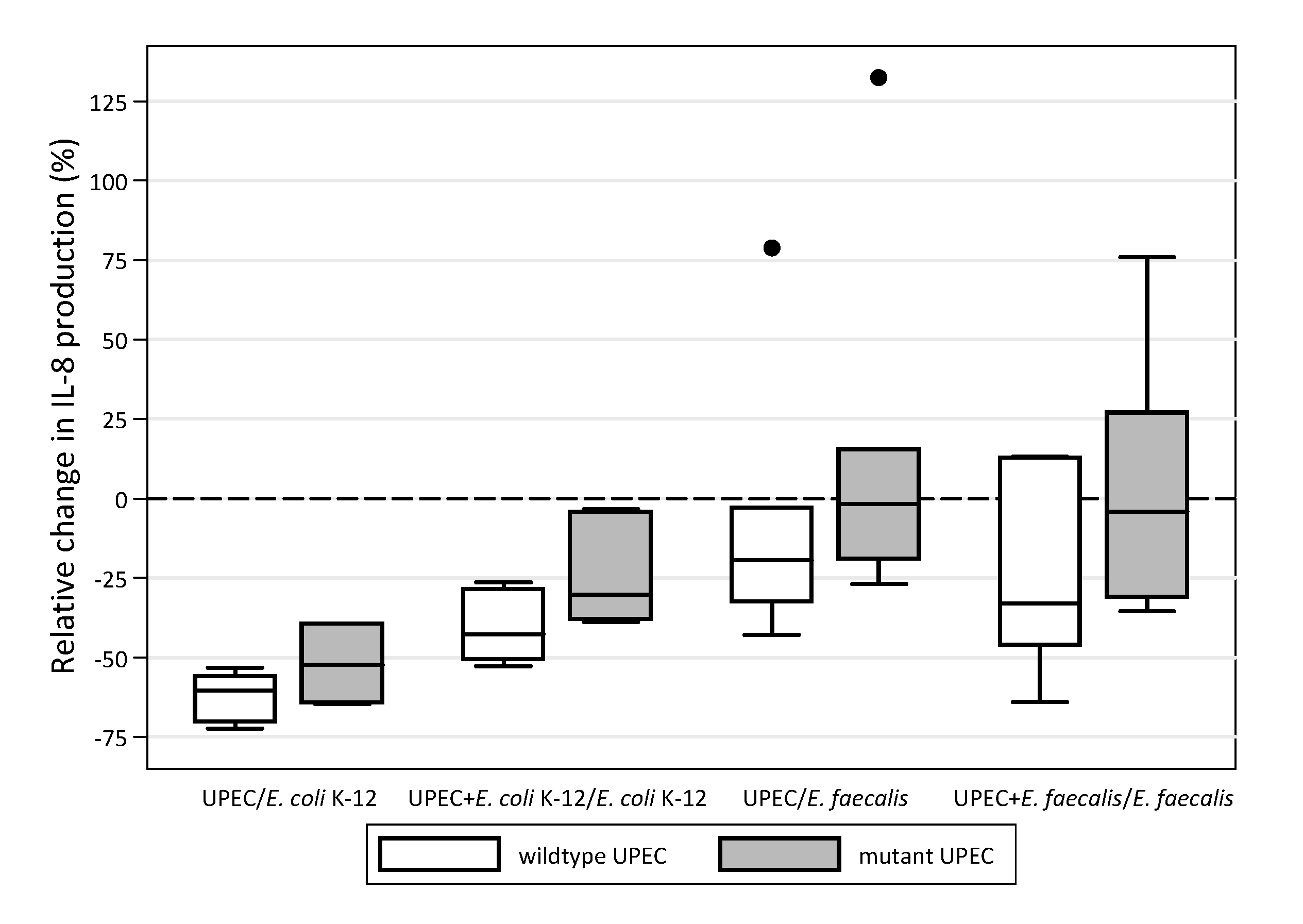
3.8. UPEC Mutants Modulate Less Than Wildtypes during In Vitro Coinfections
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef]
- Tay, W.H.; Chong, K.K.; Kline, K.A. Polymicrobial-Host Interactions during infection. J. Mol. Biol. 2016, 428, 3355–3371. [Google Scholar] [CrossRef] [PubMed]
- Brogden, K.A.; Guthmiller, J.M.; Taylor, C.E. Human polymicrobial infections. Lancet 2005, 365, 253–255. [Google Scholar] [CrossRef]
- Griffiths, E.C.; Pedersen, A.B.; Fenton, A.; Petchey, O.L. The nature and consequences of coinfection in humans. J. Infect. 2011, 63, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Stacy, A.; McNally, L.; Darch, S.E.; Brown, S.P.; Whiteley, M. The biogeography of polymicrobial infection. Nat. Rev. Microbiol. 2016, 14, 93–105. [Google Scholar] [CrossRef]
- Keogh, D.; Tay, W.H.; Ho, Y.Y.; Dale, J.L.; Chen, S.; Umashankar, S.; Williams, R.B.H.; Chen, S.L.; Dunny, G.M.; Kline, K.A. Enterococcal metabolites cues facilitate interspecies niche modulation and polymicrobial infection. Cell Host Microbe 2016, 20, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Wellington, S.; Greenberg, E.P. Quorum sensing selectivity and the potential for interspecies cross talk. mBio 2019, 10, e00146-19. [Google Scholar] [CrossRef] [PubMed]
- Chandler, J.R.; Heilmann, S.; Mittler, J.E.; Greenberg, E.P. Acyl-omoserine lactone-dependent eavesdropping promotes competition in a laboratory co-colture model. ISME J. 2012, 6, 2219–2228. [Google Scholar] [CrossRef]
- Foxman, B. The epidemiology of urinary tract infection. Nat. Rev. Urol. 2010, 7, 653–660. [Google Scholar] [CrossRef]
- Nielsen, K.L.; Dynesen, P.; Larsen, P.; Frimodt-Møller, N. Faecal Escherichia coli form patients with E. coli urinary tract infection and healthy controls who have never had a urinary tract infection. J. Med. Microbiol. 2014, 63, 582–589. [Google Scholar] [CrossRef]
- Saverino, D.; Schito, A.M.; Mannini, A.; Penco, S.; Bassi, A.M.; Piatti, G. Quinolone/Fuoroquinolone susceptibility in Escherichia coli correlates with human polymicrobial bacteriuria and with in vitro interleukin-8 suppression. FEMS Immunol. Med. Microbiol. 2010, 61, 84–93. [Google Scholar] [CrossRef]
- Drew, S.J.; Poutanen, S.M.; Mazzulli, T.; McGeer, A.J.; Sarabia, A.; Pong-Porter, S.; Rzayev, Y.; Willey, B.; Green, K.; Low, D.E. Decreased prevalence of virulence factors among ciprofloxacin-resistant uropathogenic Escherichia coli isolates. J. Clin. Microbiol. 2005, 43, 4218–4220. [Google Scholar] [CrossRef][Green Version]
- Takahashi, A.; Muratani, T.; Yasuda, M.; Takahashi, S.; Monden, K.; Ishikawa, K.; Kiyota, H.; Arakawa, S.; Matsumoto, T.; Shima, H. Genetic profiles of fluoroquinolone-resistant Escherichia coli isolates obtained from patients with cystitis: Phylogeny, virulence factors, PAIusp subtypes, and mutation patterns. J. Clin. Microbiol. 2009, 47, 791–795. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Blattner, F.R.; Plunkett, G.; Bloch, C.A.; Perna, N.T.; Burland, V.; Riley, M.; Collado-Vides, J.; Glasner, J.D.; Rode, C.K.; Mayhew, G.F. The complete genome sequence of Escherichia coli K-12. Science 1997, 277, 1453–1462. [Google Scholar] [CrossRef] [PubMed]
- Hunstad, D.A.; Justice, S.S.; Hung, C.S.; Lauer, S.R.; Hultgren, S.J. Suppression of bladder epithelial cytokine responses by uropathogenic Escherichia coli. Infect. Immun. 2005, 73, 3999–4006. [Google Scholar] [CrossRef]
- Cirz, R.T.; Chin, J.K.; Andes, D.R.; de Crécy-Lagard, V.; Craig, W.A.; Romesberg, F.E. Inhibition of mutation and combating the evolution of antibiotic resistance. PLoS Biol. 2005, 3, e176. [Google Scholar] [CrossRef]
- Thi, T.D.; López, E.; Rodríguez-Rojas, A.; Rodríguez-Beltrán, J.; Couce, A.; Guelfo, J.R.; Castaneda-García, A.; Jesus Blázquez, J. Effect of recA inactivation on mutagenesis of Escherichia coli exposed to sublethal concentrations of antimicrobials. J. Antimicrob. Chemother. 2011, 66, 531–538. [Google Scholar] [CrossRef]
- Clermont, O.; Bonacorsi, S.; Bingen, E. Rapid and simple determination of the Escherichia coli phylogenetic group. Appl. Environ. Microbiol. 2000, 66, 4555–4558. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.R.; Stell, A.L. Extended virulence genotypes of Escherichia coli strains from patients with urosepsis in relation to phylogeny and host compromise. J. Infect. Dis. 2000, 181, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Siek, K.E.; Giddings, C.W.; Doetkott, C.; Johnson, T.J.; Fakhr, M.K.; Nolan, L.K. Comparison of Escherichia coli isolates implicated in human urinary tract infection and avian colibacillosis. Microbiology 2005, 151, 2097–2110. [Google Scholar] [CrossRef]
- Bland, M. An Introduction to Medical Statistics, 4th ed.; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Wilcoxon, F. Individual comparisons by ranking methods. Biometrics 1945, 1, 80–83. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research; Chapman & Hall/CRC: London, UK, 1991. [Google Scholar]
- Chambers, J.M.; Cleveland, W.S.; Kleiner, B. Graphical Methods for Data Analysis; Wadsworth: Belmont, CA, USA, 1983. [Google Scholar]
- Kline, K.A.; Schwartz, D.J.; Gilbert, N.M.; Hultgren, S.J.; Lewis, A.L. Immune modulation by Group B Streptococcus influences host susceptibility to urinary tract infection by uropathogenic Escherichia coli. Infect. Immun. 2012, 80, 4186–4194. [Google Scholar] [CrossRef]
- Tien, B.Y.Q.; Goh, H.M.S.; Chong, K.K.L.; Bhaduri-Tagore, S.; Holec, S.; Dress, R.; Ginhoux, F.; Ingersoll, M.A.; Williams, R.B.H.; Kline, K.A. Enterococcus faecalis promotes innate immune suppression and polymicrobial catheter-associated urinary tract infection. Infect. Immun. 2017, 85, e00378-17. [Google Scholar] [CrossRef]
- Armbruster, C.E.; Smith, S.N.; Johnson, A.O.; DeOrnellas, V.; Eaton, K.A.; Yep, A.; Mody, L.; Wu, W.; Mobley, H.L.T. The pathogenic potential of Proteus mirabilis is enhanced by other uropathogens during polymicrobial urinary tract infection. Infect. Immun. 2017, 85, e00808-16. [Google Scholar] [CrossRef]
- Akira, S.; Uematsu, S.; Takeuchi, O. Pathogen recognition and innate immunity. Cell 2006, 124, 783–801. [Google Scholar] [CrossRef]
- O’Brien, G.C.; Wang, J.H.; Redmond, H.P. Bacterial lipoprotein induces resistance to Gram-negative sepsis in TLR4-deficient mice via enhanced bacterial clearance. J. Immunol. 2005, 174, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Santo, S.; Nomura, F.; Kawai, T.; Takeuchi, O.; Muhlradt, P.F.; Takeda, K.; Akira, S. Synergy and cross-tolerance between Toll like receptor (TLR) 2- and TLR4-mediated signaling pathway. J. Immunol. 2000, 165, 7096–7101. [Google Scholar]
- Wang, J.H.; Doyle, M.; Manning, B.J.; Blankson, S.; Wu, Q.D.; Power, C.; Cahill, R.; Redmond, H.P. Bacterial lip-oprotein induces endotoxin-independent tolerance to septic shock. J. Immunol. 2003, 170, 14–18. [Google Scholar] [CrossRef]
- Medveded, A.E.; Kopydlowski, K.M.; Vogel, S.N. Inhibition of lipopolysaccharide-induced signal transduc-tion in endotoxin tolerized mouse macrophages: Dysregulation of cytokine, chemokine, and Toll-like receptor 2 and 4 gene expression. J. Immunol. 2000, 164, 5564–5574. [Google Scholar] [CrossRef]
- Schilling, J.D.; Martin, S.M.; Hunstad, D.A.; Patel, K.P.; Mulvey, M.A.; Justice, S.S.; Lorenz, R.G.; Hultgren, S.J. CD14- and Toll-like receptor-dependent activation of bladder epithelial cells by lipopolysaccharide and Type 1 piliated Escherichia coli. Infect. Immun. 2003, 71, 1470–1480. [Google Scholar] [CrossRef][Green Version]
- Wiersinga, W.J.; Leopold, S.J.; Cranendonk, D.R.; van der Poll, T. Host innate immune responses to sepsis. Virulence 2014, 5, 36–44. [Google Scholar] [CrossRef]
- Rakita, R.M.; Vanek, N.N.; Jacques-Palaz, K.; Mee, M.; Mariscalco, M.M.; Dunny, G.M.; Snuggs, M.; Van Winkle, W.B.; Simon, S.I. Enterococcus faecalis bearing aggregation substance is resistant to killing by human neutrophils despite phagocytosis and neutrophil activation. Infect. Immun. 1999, 67, 6067–6075. [Google Scholar] [CrossRef]
- Stickler, D.J. Bacterial biofilms in patients with indwelling urinary catheters. Nat. Clin. Pract. Urol. 2008, 5, 598–608. [Google Scholar] [CrossRef] [PubMed]
- Guiton, P.S.; Hung, C.S.; Hancock, L.E.; Caparon, M.G.; Hultgren, S.J. Enterococcal biofilm formation and virulence in an optimized murine model of foreign body-associated urinary tract infections. Infect. Immun. 2010, 78, 4166–4175. [Google Scholar] [CrossRef]
- Wang, S.; Ng, L.H.M.; Chow, W.L.; Lee, Y.K. Infant intestinal Enterococcus faecalis down-regulates inflammatory responses in human intestinal cell lines. World J. Gastroenterol. 2008, 14, 1067–1076. [Google Scholar] [CrossRef]
- Tsaganos, T.; Pelekanou, A.; Skiadas, I.; Giamarellos-Bourboulis, E.J. Differences in cytokine stimulation between methicillin-susceptible and methicillin-resistant Staphylococcus aureus in an experimental endocarditis model. J. Infect. Chemother. 2013, 19, 272–278. [Google Scholar] [CrossRef]
- Giamarellos-Bourboulis, E.J.; Tzepi, I.; Tsovolou, I.; Spyridaki, A.; Tsaganos, T.; Vaki, I.; Kotsaki, A.; Polychronopoulos, V. Impact of multidrug resistance on experimental empyema by Pseudomonas aeruginosa. Respiration 2011, 82, 46–53. [Google Scholar] [CrossRef]
- Bristianou, M.; Panagou, C.; Adamis, T.; Raftogiannis, M.; Antonopoulou, A.; Chrisofos, M.; Galani, I.; Kanellakopoulou, K.; Tsaganos, T.; Giamarellos-Bourboulis, E.J. The impact of multidrug resistance on the pathogenicity of Escherichia coli: An experimental study. Int. J. Antimicrob. Agents 2008, 31, 216–223. [Google Scholar] [CrossRef]
- Correia, S.; Poeta, P.; Hébraud, M.; Capelo, J.L.; Igrejas, G. Mechanisms of quinolone action and resistance: Where do we stand? J. Med. Microbiol. 2017, 66, 551–559. [Google Scholar] [CrossRef]
- Cirl, C.; Wieser, A.; Yadav, M.; Duerr, S.; Schubert, S.; Fisher, H.; Stappert, D.; Wantia, N.; Rodriguez, N.; Wagner, H.; et al. Subversion of Toll-like receptor signaling by a unique family of bacterial Toll/interleukin-1 receptor domain-containing proteins. Nat. Med. 2008, 14, 399–406. [Google Scholar] [CrossRef]
- Zou, J.; Baghdayan, A.S.; Payne, S.J.; Shankar, N. A TIR domain protein from E. faecalis attenuates MyD88-mediated signaling and NF-κB activation. PLoS ONE 2014, 9, e112010. [Google Scholar] [CrossRef]

| Infection | UPEC/ K-12 | UPEC+K-12/ K-12 | UPEC/ E. faecalis | UPEC+E. faecalis/ E. faecalis |
|---|---|---|---|---|
| a UPEC/K-12 | 1.000 | |||
| b UPEC+K-12/K-12 | 0.161 | 1.000 | ||
| c UPEC/E. faecalis | 0.432 | 0.286 | 1.000 | |
| d UPEC+E. faecalis/E. faecalis | 0.357 | 0.343 | 0.786 * | 1.000 |
| Median (%) | Percentiles 25/75 (%) | Median (%) | Percentiles 25/75 (%) | Observed * p-Value | |||
|---|---|---|---|---|---|---|---|
| a UPEC/K-12 | −55.7 | −64.8/−40.2 | vs. | UPEC+K-12/K-12 | −45.6 | −50.6/−26.3 | 0.334 |
| UPEC/E. faecalis | −31.8 | −42.9/−3.0 | 0.054 | ||||
| UPEC+E. faecalis/E. faecalis | −36.9 | −46.4/−6.7 | 0.061 | ||||
| b UPEC+K-12/K-12 | −45.6 | −50.6/−26.3 | vs. | UPEC/E. faecalis | −31.8 | −42.9/−3.0 | 0.027 |
| UPEC+E. faecalis/E. faecalis | −36.9 | −46.4/−6.7 | 0.140 | ||||
| c UPEC/E. faecalis | −31.8 | −42.9/−3.0 | vs. | d UPEC+E. faecalis/E. faecalis | −36.9 | −46.4/−6.7 | 0.733 |
| Wildtype UPEC | Mutant UPEC | ||||
|---|---|---|---|---|---|
| Median (%) | Percentiles 25/75 (%) | Median (%) | Percentiles 25/75 (%) | Observed p-Value | |
| a UPEC/K-12 | −60.3 | −70.1/−55.7 | −52.2 | −64.2/−39.2 | 0.018 |
| b UPEC+K-12/K-12 | −42.6 | −50.6/−28.5 | −30.2 | −37.8/−4.0 | 0.018 |
| c UPEC/E. faecalis | −19.4 | −32.3/−3.0 | −1.6 | −18.9/15.6 | 0.018 |
| d UPEC+E. faecalis/E. faecalis | −33.0 | −46.0/13.0 | −4.0 | −30.9/27.1 | 0.028 |
| Overall | −40.1 | −55.0/−20.5 | −25.2 | −39.1/−1.9 | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piatti, G.; De Ferrari, L.; Schito, A.M.; Riccio, A.M.; Penco, S.; Cassia, S.; Bruzzone, M.; Ceppi, M. In Vitro Reduction of Interleukin-8 Response to Enterococcus faecalis by Escherichia coli Strains Isolated from the Same Polymicrobial Urines. Microorganisms 2021, 9, 1501. https://doi.org/10.3390/microorganisms9071501
Piatti G, De Ferrari L, Schito AM, Riccio AM, Penco S, Cassia S, Bruzzone M, Ceppi M. In Vitro Reduction of Interleukin-8 Response to Enterococcus faecalis by Escherichia coli Strains Isolated from the Same Polymicrobial Urines. Microorganisms. 2021; 9(7):1501. https://doi.org/10.3390/microorganisms9071501
Chicago/Turabian StylePiatti, Gabriella, Laura De Ferrari, Anna Maria Schito, Anna Maria Riccio, Susanna Penco, Sebastiano Cassia, Marco Bruzzone, and Marcello Ceppi. 2021. "In Vitro Reduction of Interleukin-8 Response to Enterococcus faecalis by Escherichia coli Strains Isolated from the Same Polymicrobial Urines" Microorganisms 9, no. 7: 1501. https://doi.org/10.3390/microorganisms9071501
APA StylePiatti, G., De Ferrari, L., Schito, A. M., Riccio, A. M., Penco, S., Cassia, S., Bruzzone, M., & Ceppi, M. (2021). In Vitro Reduction of Interleukin-8 Response to Enterococcus faecalis by Escherichia coli Strains Isolated from the Same Polymicrobial Urines. Microorganisms, 9(7), 1501. https://doi.org/10.3390/microorganisms9071501






