Contribution of HIV/AIDS-Related Human and Social Sciences Research to a Better Understanding of the Challenges of Hepatitis B Prevention, Diagnosis and Care
Abstract
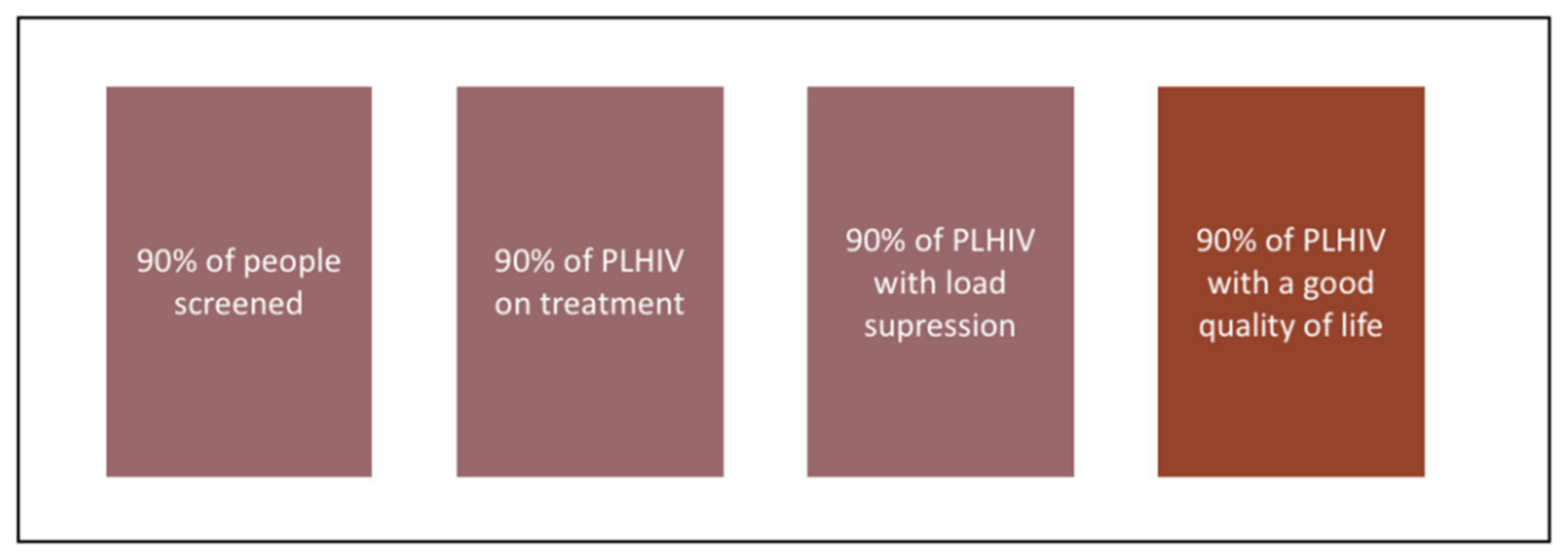
1. Introduction
2. Prevention of Hepatitis B Infection: Access to Screening
3. How to Guarantee Retention in Care of People Diagnosed with HBV?
4. Clinical Trials and Cohort Monitoring: Integrating Quality of Life
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The Lancet Global Health. The hidden threat of hepatitis B. Lancet Global Health 2016, 4, e502. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. WHO Guidelines on Hepatitis B and C Testing; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- ONUSIDA. 90-90-90. Une Cible Ambitieuse de Traitement Pour Aider à Mettre Fin à L’épidémie du Sida [Internet]. ONUSIDA. 2014. Available online: https://www.unaids.org/sites/default/files/media_asset/90-90-90_fr.pdf (accessed on 12 March 2021).
- Bourdillon, F.; Brücker, G.; Tabuteau, D. Traité de Santé Publique; Lavoisier: Cachan, France, 2020. [Google Scholar]
- Lebossé, F.; Zoulim, F. Vaccination contre le virus de l’hépatite B et prévention du cancer du foie. Bull. Cancer 2021, 108, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Thanh Thi Le, X.; Ishizumi, A.; Thi Thu Nguyen, H.; Thi Duong, H.; Thi Thanh Dang, H.; Manh Do, C.; Thi Pham, Q.; Thi Le, H.; Iijima, M.; Tohme, R.A.; et al. Social and behavioral determinants of attitudes towards and practices of hepatitis B vaccine birth dose in Vietnam. Vaccine 2020, 38, 8343–8350. [Google Scholar] [CrossRef] [PubMed]
- Chan, O.K.; Suen, S.S.H.; Lao, T.T.-H.; Leung, V.K.T.; Yeung, S.W.; Leung, T.Y. Determinants of hepatitis B vaccine uptake among pregnant Chinese women in Hong Kong. Int. J. Gynecol. Obstetr. 2009, 106, 232–235. [Google Scholar] [CrossRef]
- Pan, C.Q.; Duan, Z.; Dai, E.; Zhang, S.; Han, G.; Wang, Y.; Zhang, H.; Zou, H.; Zhu, B.; Zhao, W.; et al. Tenofovir to Prevent Hepatitis B Transmission in Mothers with High Viral Load. N. Engl. J. Med. 2016, 374, 2324–2334. [Google Scholar] [CrossRef] [PubMed]
- Stevens, C.E.; Toy, P.; Kamili, S.; Taylor, P.E.; Tong, M.J.; Xia, G.-L.; Vyas, G.N. Eradicating hepatitis B virus: The critical role of preventing perinatal transmission. Biologicals 2017, 50, 3–19. [Google Scholar] [CrossRef]
- Lemoine, M.; Shimakawa, Y.; Njie, R.; Taal, M.; Ndow, G.; Chemin, I.; Ghosh, S.; Njai, H.F.; Jeng, A.; Sow, A.; et al. Acceptability and feasibility of a screen-and-treat programme for hepatitis B virus infection in The Gambia: The Prevention of Liver Fibrosis and Cancer in Africa (PROLIFICA) study. Lancet Global Health 2016, 4, 559–567. [Google Scholar] [CrossRef]
- Bruchon-Schweitzer, M. Des croyances aux comportements: Conceptions et modèles. In Psychologie de la Santé Concepts, Méthodes et Modèles; Dunod: Paris, France, 2014; pp. 373–432. [Google Scholar]
- Milhabet, I.; Desrichard, O.; Verlhiac, J.-F. Comparaison sociale et perception des risques: l’optimisme comparatif. In Perspectives Cognitives et Conduites Sociales; Presses Universitaires de Rennes: Rennes, France, 2002; pp. 215–245. [Google Scholar]
- Mabire, X.; Puppo, C.; Morel, S.; Mora, M.; Rojas Castro, D.; Chas, J.; Cua, E.; Pintado, C.; Suzan-Monti, M.; Spire, B.; et al. Pleasure and PrEP: Pleasure-Seeking Plays a Role in Prevention Choices and Could Lead to PrEP Initiation. Am. J. Mens Health 2019, 13, 155798831982739. [Google Scholar] [CrossRef]
- Girard, G. Risque VIH et réflexivité. Logiques de prévention chez des gais séropositifs. Sci. Soc. Santé 2016, 34, 81–107. [Google Scholar] [CrossRef]
- Grémy, I. Les comportements d’adaptation aux risques de transmission du VIH dans différentes populations. Méd. Mal. Infect. 2005, 35, 306–313. [Google Scholar] [CrossRef]
- Potez, C.; Bridou, M.; Fouéré, S.; Montreuil, M. Le rôle des facteurs psychologiques dans la réalisation d’une démarche de dépistage du VIH. Ann. Méd. Psychol. Rev. Psychiatr. 2018, 176, 559–566. [Google Scholar] [CrossRef]
- Préau, M. De la perception des risques à la réduction des risques sexuels dans le champ du VIH/Sida: Du discours médical aux normes sociales. Carnets GRePS 2013, 5, 76–88. [Google Scholar]
- Massari, V.; Lapostolle, A.; Grupposo, M.-C.; Dray-Spira, R.; Costagliola, D.; Chauvin, P. Les freins au dépistage du VIH dans l’agglomération parisienne en 2010: Une analyse transversale multiniveaux de la cohorte SIRS. Rev. d’Épidémiol. Santé Publ. 2014, 62, S174–S175. [Google Scholar] [CrossRef]
- Chesney, M.A.; Smith, A.W. Critical delays in HIV testing and care: The potential role of stigma. Am. Behav. Sci. 1999, 42, 1162–1174. [Google Scholar] [CrossRef]
- Lieber, E.; Li, L.; Wu, Z.; Rotheram-Borus, M.J.; Guan, J. The National Institute of Mental Health (NIMH) Collaborative HIV Prevention Trial Group. HIV/STD Stigmatization Fears as Health-Seeking Barriers in China. AIDS Behav. 2006, 10, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Kra, K.O.; Aba, A.; Effi-Angbo, A.O.; Koné, K.D.; Kadiané, K.N.J. A-21: Les raisons du non partage du statut sérologique chez les personnes vivant avec le VIH en Afrique noire. Méd. Mal. Infect. 2014, 44, 24. [Google Scholar] [CrossRef]
- Laguette, V.; Préau, M. Stigmate de la maladie et divulgation du statut: Enjeux individuels et sociaux. Carnets GRePS 2015, 6, 31–36. [Google Scholar]
- Kippax, S.; Race, K. Sustaining safe practice: Twenty years on. Soc. Sci. Med. 2003, 57, 1–12. [Google Scholar] [CrossRef]
- Puppo, C.; Spire, B.; Morel, S.; Génin, M.; Béniguel, L.; Costagliola, D.; Ghosn, J.; Mabire, X.; Molina, J.M.; Rojas Castro, D.; et al. How PrEP users constitute a community in the MSM population through their specific experience and management of stigmatization. The example of the French ANRS-PREVENIR study. AIDS Care 2020, 32, 32–39. [Google Scholar] [CrossRef]
- Préau, M.; Rojas Castro, D.; Spire, B.; Mora, M.; Le Gall, J.-M. Quelle place pour les recherches interventionnelles en prévention du VIH, enjeux théoriques et méthodologiques pour la psychologie sociale de la santé. In Psychologie de la Santé Applications et Interventions; Dunod: Paris, France, 2014; pp. 149–169. [Google Scholar]
- Greacen, T.; Simon, A.; Troisoeufs, A.; Champenois, K. Les enjeux de l’autotest VIH en officine perçus par des pharmaciens et des populations concernées en France. Santé Publ. 2020, 32, 229–237. [Google Scholar] [CrossRef]
- Dah, T.T.E.; Couderc, C.; Coulibaly, A.; kouamé, M.J.-B.; Agboyibor, M.K.; Traoré, I.; Maradan, G.; Rojas Castro, D.; Mensah, E.; Anoma, C.; et al. Hepatitis B Virus Prevalence and Vaccination in Men Who Have Sex with Men in West Africa (CohMSM ANRS 12324—Expertise France). Open Forum Infect. Dis. 2019, 6, 249. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.; Shimakawa, Y.; Ndow, G.; Sow, A.; Tamba, S.; Njie, R.; Lo, G.; Ghosh, S.; Toure-Kane, C.; Ka, M.; et al. Prévention de la fibrose et du cancer du foie liés au virus de l’hépatite B en Afrique: Le projet Prolifica. Med. Sci. 2019, 35, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Haute Autorité de Santé. Actualisation des Actes de Biologie Médicale Relatifs au Diagnostic et à la Prise en Charge des Hépatites B, C et D [Internet]. Saint Denis: Haute Autorité de Santé. 2017. Available online: https://www.has-sante.fr/upload/docs/application/pdf/2017-01/dir1/argumentaire_hepatites-b-c-d_vd.pdf (accessed on 1 April 2021).
- Lieveld, F.I.; Vlerken, L.G.; van Siersema, P.D.; van Erpecum, K.J. Patient adherence to antiviral treatment for chronic hepatitis B and C: A systematic review. Ann. Hepatol. 2013, 12, 380–391. [Google Scholar] [CrossRef]
- Moatti, J.-P.; Spire, B. Les enjeux économiques et sociaux de l’infection par le VIH à l’ère des multithérapies antirétrovirales: Apports des sciences humaines et sociales. Med. Sci. 2003, 19, 878–884. [Google Scholar] [CrossRef]
- Remor, E. Systematic Review of the Psychometric Properties of the Questionnaire to Evaluate the Adherence to HIV Therapy (CEAT-VIH). Patient 2013, 6, 61–73. [Google Scholar] [CrossRef]
- Spire, B.; Duran, S.; Souville, M.; Leport, C.; Raffi, F.; Moatti, J.-P. Adherence to highly active antiretroviral therapies (HAART) in HIV-infected patients: From a predictive to a dynamic approach. Soc. Sci. Med. 2002, 54, 1481–1496. [Google Scholar] [CrossRef]
- Duran, S.; Peytavin, G.; Carrieri, P.; Raffi, F.; Ecobichon, J.-L.; Pereira, E.; Cassuto, G.P.; Spire, B.; Leport, C. The detection of non-adherence by self-administered questionnaires can be optimized by protease inhibitor plasma concentration determination. AIDS 2003, 17, 1096–1099. [Google Scholar] [CrossRef]
- Ferreira, C.; Gay, M.-C.; Regnier-Aeberhard, F.; Bricaire, F. Les représentations de la maladie et des effets secondaires du traitement antirétroviral comme déterminants de l’observance chez les patients VIH. Ann. Méd. Psychol. Rev. Psychiatr. 2010, 168, 25–33. [Google Scholar] [CrossRef][Green Version]
- Duran, S.; Spire, B.; Raffi, F.; Walter, V.; Bouhour, D.; Journot, V.; Cailleton, V.; Leport, C.; Moatti, J.P. Self-Reported Symptoms After Initiation of a Protease Inhibitor in HIV-Infected Patients and Their Impact on Adherence to HAART. HIV Clin. Trials 2001, 2, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Carrieri, M.P.; Leport, C.; Protopopescu, C.; Cassuto, J.-P.; Bouvet, E.; Peyramond, D.; Raffi, F.; Moatti, J.P.; Cheê, G.; Spire, B. Factors Associated with Nonadherence to Highly Active Antiretroviral Therapy: A 5-Year Follow-Up Analysis with Correction for the Bias Induced by Missing Data in the Treatment Maintenance Phase. JAIDS 2006, 41, 477–485. [Google Scholar] [CrossRef]
- Spire, B.; Carrieri, P.; Sopha, P.; Protopopescu, C.; Prak, N.; Quillet, C.; Ngeth, C.; Ferradini, L.; Delfraissy, J.F.; Laureillard, D. Adherence to antiretroviral therapy in patients enrolled in a comprehensive care program in Cambodia: A 24-month follow-up assessment. Antivir. Ther. 2008, 5, 697–703. [Google Scholar]
- Bernier, A.; Yattassaye, A.; Beaulieu-Prévost, D.; Otis, J.; Henry, E.; Flores-Aranda, J.; Massie, L.; Préau, M.; Keita, B.D. Empowering Malian women living with HIV regarding serostatus disclosure management: Short-term effects of a community-based intervention. Patient Educ. Counsel. 2018, 101, 248–255. [Google Scholar] [CrossRef]
- Préau, M.; Morin, M. L’évaluation psychosociale de la qualité de vie des personnes infectées par le VIH. Prat. Psychol. 2005, 11, 387–402. [Google Scholar] [CrossRef]
- Bruchon-Schweitzer, M.; Boujut, É. Bonheur, satisfaction de la vie, bien-être, santé et qualité de vie. In Psychologie de la Santé Concepts, Méthodes et Modèles; Dunod: Paris, France, 2014; pp. 3–82, (Psycho Sup). [Google Scholar]
- Troussier, T.; Tourette-Turgis, C. La qualité de la vie sexuelle et affective favorise la prévention chez les personnes vivant avec le VIH. Sexologies 2006, 15, 165–175. [Google Scholar] [CrossRef]
- Levy, A.R.; Kowdley, K.V.; Iloeje, U.; Tafesse, E.; Mukherjee, J.; Gish, R.; Bzowej, N.; Briggs, A.H. The Impact of Chronic Hepatitis B on Quality of Life: A Multinational Study of Utilities from Infected and Uninfected Persons. Value Health 2008, 11, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Ong, S.C.; Mak, B.; Aung, M.O.; Li, S.-C.; Lim, S.-G. Health-related quality of life in chronic hepatitis B patients. Hepatology 2008, 47, 1108–1117. [Google Scholar] [CrossRef] [PubMed]
- Bondini, S.; Kallman, J.; Dan, A.; Younoszai, Z.; Ramsey, L.; Nader, F.; Younossi, Z.M. Health-related quality of life in patients with chronic hepatitis B. Liver Int. 2007, 27, 1119–1125. [Google Scholar] [CrossRef]
- Lam, E.T.; Lam, C.L.; Lai, C.; Yuen, M.; Fong, D.Y.; So, T.M. Health-related quality of life of Southern Chinese with chronic hepatitis B infection. Health Qual. Life Outcomes 2009, 7, 1–10. [Google Scholar] [CrossRef]
- Préau, M.; Doumergue, M.D.; Protière, C.; Goujard, C.; Mora, M.; Muller, L.; Lelievre, J.D.; Raffi, F.; Spire, B.; Lambotte, O. Acceptability of HIV Cure-related trials: The challenges for physicians and people living with HIV (ANRS-APSEC). AIDS Care 2018, 30, 914–920. [Google Scholar] [CrossRef]
- Ferez, S.; Pappous, A.; Ruffié, S. Activité Physique et Sportive des PVVIH: De L’intérêt de la Pratique à L’accès à la Pratique (Revue de Littérature). Retos. Nuevas Tend. Educ. Física Deporte Recreación 2010, 18, 77–83. [Google Scholar]
- Rojas Castro, D.; Le Gall, J.-M.; Jablonski, O. Améliorer la santé des personnes séropositives au VIH: SERONET, un nouvel outil de l’approche communautaire. Santé Publ. 2009, 21, 129. [Google Scholar] [CrossRef]
- Beaulieu, M. Modélisation de la Qualité de vie des Femmes Vivant avec le VIH au Québec. Master’s Thesis, Université du Québec à Montréal, Montréal, QC, Canada, 2008. [Google Scholar]
- Marsicano, E.; Dray-Spira, R.; Lert, F.; Aubrière, C.; Spire, B.; Hamelin, C. Multiple discriminations experienced by people living with HIV in France: Results from the ANRS-Vespa2 study. AIDS Care 2014, 26, S97–S106. [Google Scholar] [CrossRef]
- Brégigeon, S.; Lions, C.; Zaegel-Faucher, O.; Laroche, H.; Martinet, P.; Bertone, H.; Blanco-Betancourt, C.; Orticoni, M.; Soavi, M.J.; Poizot-Martin, I. Consultation « santé sexuelle et affective »: Quelles attentes pour les personnes vivant avec le VIH? Sexologies 2019, 28, 20–24. [Google Scholar] [CrossRef]
- El Fane, M.; Bensghir, R.; Sbai, S.; Chakib, A.; Kadiri, N.; Ayouch, A.; Himmich, H. Quality of sexual life for people living with HIV (PLWHA). Sexologies 2011, 20, 158–162. [Google Scholar] [CrossRef]
- Lazarus, J.V.; Safreed-Harmon, K.; Barton, S.E.; Costagliola, D.; Dedes, N.; del Amo Valero, J.; Gatell, J.M.; Baptista-Leite, R.; Mendão, L.; Porter, K.; et al. Beyond viral suppression of HIV—The new quality of life frontier. BMC Med. 2016, 14, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Barger, D.; Leleux, O.; Conte, V.; Sapparrart, V.; Gapillout, M.; Crespel, I.; Erramouspe, M.; Delveaux, S.; Dabis, F.; Bonnet, F. Integrating Electronic Patient-Reported Outcome Measures into Routine HIV Care and the ANRS CO3 Aquitaine Cohort’s Data Capture and Visualization System (QuAliV): Protocol for a Formative Research Study. JMIR Res. Protoc. 2018, 7, e147. [Google Scholar] [CrossRef]
- Spiegel, B.M.R.; Bolus, R.; Han, S.; Tong, M.; Esrailian, E.; Talley, J.; Tran, T.; Smith, J.; Karsan, H.A.; Durazo, F.; et al. Development and validation of a disease-targeted quality of life instrument in chronic hepatitis B: The hepatitis B quality of life instrument, version 1.0. Hepatology 2007, 46, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Préau, M.; Marcellin, F.; Carrieri, M.P.; Lert, F.; Obadia, Y.; Spire, B. Health-related quality of life in French people living with HIV in 2003: Results from the national ANRS-EN12-VESPA Study. AIDS 2007, 21, S19–S27. [Google Scholar] [CrossRef] [PubMed]
- Marcellin, F.; Préau, M.; Ravaux, I.; Dellamonica, P.; Spire, B.; Carrieri, M.P. Self-Reported Fatigue and Depressive Symptoms as Main Indicators of the Quality of Life (QOL) of Patients Living with HIV and Hepatitis C: Implications for Clinical Management and Future Research. HIV Clin. Trials 2007, 8, 320–327. [Google Scholar] [CrossRef]
- Préau, M.; Protopopescu, C.; Spire, B.; Dellamonica, P.; Poizot-Martin, I.; Villes, V. La qualité de vie des patients co-infectés par le VIH et le VHC. Rev. d’Épidémiol. Santé Publ. 2006, 54, 33–43. [Google Scholar] [CrossRef]
- Li, Y.; Rapkin, B. Classification and regression tree uncovered hierarchy of psychosocial determinants underlying quality-of-life response shift in HIV/AIDS. J. Clin. Epidemiol. 2009, 62, 1138–1147. [Google Scholar] [CrossRef] [PubMed]
- Sprangers, M.A.G.; Schwartz, C.E. Integrating response shift into health-related quality of life research: A theoretical model. Soc. Sci. Med. 1999, 48, 1507–1515. [Google Scholar] [CrossRef]
- Demange, É.; Henry, É.; Préau, M. De la Recherche en Collaboration à la Recherche Communautaire: Un Guide Méthodologique; ANRS: Paris, France, 2012; Pantin (14 rue Scandicci, 93500); Coalition PLUS. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bauquier, C.; Préau, M. Contribution of HIV/AIDS-Related Human and Social Sciences Research to a Better Understanding of the Challenges of Hepatitis B Prevention, Diagnosis and Care. Microorganisms 2021, 9, 1166. https://doi.org/10.3390/microorganisms9061166
Bauquier C, Préau M. Contribution of HIV/AIDS-Related Human and Social Sciences Research to a Better Understanding of the Challenges of Hepatitis B Prevention, Diagnosis and Care. Microorganisms. 2021; 9(6):1166. https://doi.org/10.3390/microorganisms9061166
Chicago/Turabian StyleBauquier, Charlotte, and Marie Préau. 2021. "Contribution of HIV/AIDS-Related Human and Social Sciences Research to a Better Understanding of the Challenges of Hepatitis B Prevention, Diagnosis and Care" Microorganisms 9, no. 6: 1166. https://doi.org/10.3390/microorganisms9061166
APA StyleBauquier, C., & Préau, M. (2021). Contribution of HIV/AIDS-Related Human and Social Sciences Research to a Better Understanding of the Challenges of Hepatitis B Prevention, Diagnosis and Care. Microorganisms, 9(6), 1166. https://doi.org/10.3390/microorganisms9061166




