Field Evaluation of the Performance of Two Rapid Diagnostic Tests for Meningitis in Niger and Burkina Faso
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview
2.2. Performance of the RDTs
2.3. RDT Feasibility and Acceptability
2.4. Sample Size
2.5. Ethical Considerations
3. Results
3.1. RDT Performance
3.2. RDT Feasibility and Acceptability
4. Discussion
Performance of the RDTs
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Meningococcal vaccines: WHO position paper, November 2011. Wkly. Epidemiol. Rec. 2011, 18, 521–539. [Google Scholar]
- Boisier, P.; Maïnassara, H.B.; Sidikou, F.; Djibo, S.; Kairo, K.K.; Chanteau, S. Case-fatality ratio of bacterial meningitis in the African meningitis belt: We can do better. Vaccine 2007, 25, A24–A29. [Google Scholar] [CrossRef] [PubMed]
- Van de Beek, D. Progress and challenges in bacterial meningitis. Lancet 2012, 380, 1623–1624. [Google Scholar] [CrossRef]
- Molesworth, A.M.; Thomson, M.C.; Connor, S.J.; Cresswell, M.P.; Morse, A.P.; Shears, P.; Hart, C.A.; Cuevas, L.E. Where is the meningitis belt? Defining an area at risk of epidemic meningitis in Africa. Trans. R. Soc. Trop. Med. Hyg. 2002, 96, 242–249. [Google Scholar] [CrossRef]
- Harrison, L.H.; Pelton, S.I.; Wilder-Smith, A.; Holst, J.; Safadi, M.A.; Vazquez, J.A.; Taha, M.K.; LaForce, F.M.; Von Gottberg, A.; Borrow, R.; et al. The Global Meningococcal Initiative: Recommendations for reducing the global burden of meningococcal disease. Vaccine 2011, 29, 3363–3371. [Google Scholar] [CrossRef] [PubMed]
- Halperin, S.A.; Bettinger, J.A.; Greenwood, B.; Harrison, L.H.; Jelfs, J.; Ladhani, S.N.; McIntyre, P.; Ramsay, M.E.; Sáfadi, M.A. The changing and dynamic epidemiology of meningococcal disease. Vaccine 2012, 30, B26–B36. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Defeating Meningitis by 2030: Baseline Situation Analysis; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/immunization/research/BSA_20feb2019.pdf?ua=1 (accessed on 13 April 2021).
- Soeters, H.M.; Diallo, A.O.; Bicaba, B.W.; Kadadé, G.; Dembélé, A.Y.; Acyl, M.A.; Nikiema, C.; Sadji, A.Y.; Poy, A.N.; Lingani, C.; et al. Bacterial Meningitis Epidemiology in Five Countries in the Meningitis Belt of Sub-Saharan Africa, 2015–2017. J. Infect. Dis. 2019, 220 (Suppl. 4), S165–S174. [Google Scholar] [CrossRef] [PubMed]
- Gessner, B.D.; Mueller, J.E.; Yaro, S. African meningitis belt pneumococcal disease epidemiology indicates a need for an effective serotype 1 containing vaccine, including for older children and adults. BMC Infect. Dis. 2010, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Pneumococcal meningitis outbreaks in sub-Saharan Africa. Wkly. Epidemiol. Rec. 2016, 91, 298–302. [Google Scholar]
- Lingani, C.; Bergeron-Caron, C.; Stuart, J.M.; Fernandez, K.; Djingarey, M.H.; Ronveaux, O.; Schnitzler, J.C.; Perea, W.A. Meningococcal Meningitis Surveillance in the African Meningitis Belt, 2004–2013. Clin. Infect. Dis. 2015, 61 (Suppl. 5), S410–S415. [Google Scholar] [CrossRef] [PubMed]
- Feagins, A.R.; Ronveaux, O.; Taha, M.K.; Caugant, D.A.; Smith, V.; Fernandez, K.; Glennie, L.; Fox, L.M.; Wang, X. Next generation rapid diagnostic tests for meningitis diagnosis. J. Infect. 2020, 81, 712–718. [Google Scholar] [CrossRef] [PubMed]
- Chanteau, S.; Dartevelle, S.; Mahamane, A.E.; Djibo, S.; Boisier, P.; Nato, F. New rapid diagnostic tests for Neisseria meningitidis serogroups A, W135, C, and Y. PLoS Med. 2006, 3, e337. [Google Scholar] [CrossRef] [PubMed]
- Agnememel, A.; Traincard, F.; Dartevelle, S.; Mulard, L.; Mahamane, A.E.; Oukem-Boyer, O.O.; Denizon, M.; Kacou, N.A.; Dosso, M.; Gake, B.; et al. Development and evaluation of a dipstick diagnostic test for Neisseria meningitidis serogroup X. J. Clin. Microbiol. 2015, 53, 449–454. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Haddar, C.H.; Terrade, A.; Verhoeven, P.; Njanpop-Lafourcade, B.M.; Dosso, M.; Sidikou, F.; Mahamane, A.E.; Lombart, J.P.; Razki, A.; Hong, E.; et al. Validation of a New Rapid Detection Test for Detection of Neisseria meningitidis A/C/W/X/Y Antigens in Cerebrospinal Fluid. J. Clin. Microbiol. 2020, 58, e01699-19. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Contrôle des Epidémies de Méningite en Afrique. Guide de Référence Rapide à L’intention des Autorités Sanitaires et des Soignants. Organisation Mondiale de la Santé [Control of Meningitis Epidemics in Africa. Quick Reference Guide for Health Authorities and Caregivers]; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Nam, J. Comparison of validity of assessment methods using indices of adjusted agreement: Comparison of validity of assessment methods. Stat. Med. 2007, 26, 620–632. [Google Scholar] [CrossRef] [PubMed]
- Sidikou, F.; Zaneidou, M.; Alkassoum, I.; Schwartz, S.; Issaka, B.; Obama, R.; Lingani, C.; Tate, A.; Ake, F.; Sakande, S.; et al. Emergence of epidemic Neisseria meningitidis serogroup C in Niger, 2015: An analysis of national surveillance data. Lancet Infect. Dis. 2016, 16, 1288–1294. [Google Scholar] [CrossRef]
- World Health Organization. Epidemic meningitis control in countries of the African meningitis belt, 2019. Wkly. Epidemiol. Rec. 2020, 95, 133–144. [Google Scholar]
- World Health Organization. Epidemic meningitis control in countries of the African meningitis belt, 2018. Wkly. Epidemiol. Rec. 2019, 94, 179–188. [Google Scholar]
- Funk, A.; Uadiale, K.; Kamau, C.; Caugant, D.A.; Ango, U.; Greig, J. Sequential Outbreaks Due to a New Strain of Neisseria Meningitidis Serogroup C in Northern Nigeria, 2013–2014. PLoS Curr. 2014. Available online: https://currents.plos.org/outbreaks/?p=40715 (accessed on 13 April 2021). [CrossRef] [PubMed]
- World Health Organization. Specifications for a Rapid Diagnostic Test for Meningitis, African Meningitis Belt; World Health Organization: Geneva, Switzerland, 2016; Available online: https://www.who.int/publications/m/item/specifications-for-a-rapid-diagnostic-test-for-meningitis-african-meningitis-belt (accessed on 13 April 2021).
- World Health Organization. Defeating Meningitis by 2030: A Global Roadmap; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/m/item/defeating-meningitis-by-2030-a-global-road-map (accessed on 13 April 2021).
- World Health Organization. Meeting Report: Developing a New Generation RDTs for Meningitis; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
| Characteristics | N | % | |
|---|---|---|---|
| Total patients | 327 | 100 | |
| Recruitment country | Burkina Faso | 81 | 25 |
| Niger | 246 | 75 | |
| Recruitment period | Epidemic | 198 | 61 |
| Non-epidemic | 129 | 39 | |
| Age—average (range) | 9 years (3 months—86 years) | ||
| Symptoms | Sudden onset of fever | 316 | 97 |
| Abdominal pain | 181 | 55 | |
| Confusion and disorientation | 180 | 55 | |
| Joint pain | 136 | 42 | |
| Stiff neck | 116 | 36 | |
| Bulging fontanelle | 10 | 3 | |
| Petechial rash | 1 | 0 | |
| other meningeal signs | 18 | 6 | |
| Nm RDT results | All serogroups | 106 | 32 |
| NmA | 9 | 3 | |
| NmC | 56 | 17 | |
| NmW | 2 | 1 | |
| NmX | 40 | 12 | |
| NmY | 1 | 0 | |
| Negative | 221 | 68 | |
| Sp RDT results | Positive | 28 | 9 |
| Negative | 295 | 91 | |
| PCR Negative/RDT Negative | PCR Positive/RDT Positive | PCR Negative/RDT Positive | PCR Positive/RDT Negative | Total | Sensitivity (%) | 95% CI | Specificity (%) | 95% CI | PPV (%) | 95% CI | NPV (%) | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RDT at health center | All Nm | 217 | 82 | 24 | 4 | 327 | 95 | (89;99) | 90 | (86;94) | 77 | (68;85) | 98 | (95;100) |
| NmA | 318 | 0 | 9 | 0 | 327 | NA | 97 | (95;99) | NA | 100 | (99;100) | |||
| NmC | 266 | 50 | 6 | 4 | 326 | 93 | (82;98) | 98 | (95;99) | 89 | (78;96) | 99 | (96;100) | |
| NmW | 324 | 0 | 2 | 0 | 326 | NA | 99 | (98;100) | NA | 100 | (99;100) | |||
| NmX | 284 | 29 | 11 | 3 | 327 | 91 | (75;98) | 96 | (93;98) | 73 | (56;85) | 99 | (97;100) | |
| NmY | 324 | 0 | 1 | 0 | 325 | NA | 100 | (98;100) | NA | 100 | (99;100) | |||
| Sp | 293 | 24 | 4 | 2 | 323 | 92 | (75;99) | 99 | (97;100) | 86 | (67;96) | 99 | (98;100) | |
| RDT at NRL | All Nm | 108 | 28 | 6 | 2 | 144 | 93 | (78;99) | 95 | (89;98) | 82 | (66;93) | 98 | (94;100) |
| NmA | 141 | 0 | 6 | 0 | 147 | NA | 96 | (91;99) | NA | 100 | (97;100) | |||
| NmC | 127 | 16 | 2 | 1 | 146 | 94 | (71;100) | 98 | (95;100) | 89 | (65;99) | 99 | (96;100) | |
| NmW | 142 | 0 | 3 | 0 | 145 | NA | 98 | (94;100) | NA | 100 | (97;100) | |||
| NmX | 132 | 12 | 0 | 1 | 145 | 92 | (64;100) | 100 | (97;100) | 100 | (74;100) | 99 | (96;100) | |
| NmY | 144 | 0 | 2 | 0 | 146 | NA | 99 | (95;100) | NA | 100 | (98;100) | |||
| Sp | 138 | 8 | 0 | 1 | 147 | 89 | (52;100) | 100 | (97;100) | 100 | (63;100) | 99 | (96;100) | |
| PCR Negative/RDT Negative | PCR Positive/RDT Positive | PCR Negative/RDT Positive | PCR Positive/RDT Negative | Total | Sensitivity (%) | 95% CI | Specificity (%) | 95% CI | PPV (%) | 95% CI | NPV (%) | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2018 | All Nm | 80 | 16 | 17 | 1 | 114 | 94 | (71;100) | 83 | (73;89) | 49 | (31;67) | 99 | (93;100) |
| NmA | 106 | NA | 8 | NA | 114 | NA | NA | 93 | (87;97) | NA | NA | 100 | (97;100) | |
| NmC | 110 | 4 | NA | NA | 114 | 100 | (40;100) | 100 | (97;100) | 100 | (40;100) | 100 | (97;100) | |
| NmW | 112 | NA | 1 | NA | 113 | NA | NA | 99 | (95;100) | NA | NA | 100 | (97;100) | |
| NmX | 93 | 12 | 8 | 1 | 114 | 92 | (64;100) | 92 | (85;97) | 60 | (36;81) | 99 | (94;100) | |
| NmY | 114 | NA | NA | NA | 114 | NA | NA | 100 | (97;100) | NA | NA | 100 | (97;100) | |
| Sp | 108 | 4 | 1 | 113 | 100 | (40;100) | 99 | (95;100) | 80 | (28;100) | 100 | (97;100) | ||
| 2019 | All Nm | 135 | 64 | 7 | 3 | 209 | 96 | (88;99) | 95 | (90;98) | 90 | (81;96) | 98 | (94;100) |
| NmA | 208 | NA | 1 | NA | 209 | NA | NA | 100 | (97;100) | NA | NA | 100 | (98;100) | |
| NmC | 154 | 45 | 5 | 4 | 208 | 92 | (80;98) | 97 | (93;99) | 90 | (78;97) | 98 | (94;99) | |
| NmW | 208 | NA | 1 | NA | 209 | NA | NA | 100 | (97;100) | NA | NA | 100 | (98;100) | |
| NmX | 188 | 17 | 3 | 1 | 209 | 94 | (73;100) | 98 | (96;100) | 85 | (62;97) | 100 | (97;100) | |
| NmY | 207 | NA | 1 | NA | 208 | NA | NA | 100 | (97;100) | NA | NA | 100 | (98;100) | |
| Sp | 182 | 20 | 3 | 2 | 207 | 91 | (71;99) | 98 | (95;100) | 87 | (66;97) | 99 | (96;100) | |
| PCR Negative/RDT Negative | PCR Positive/RDT Positive | PCR Negative/RDT Positive | PCR Positive/RDT Negative | Total | Sensitivity (%) | 95% CI | Specificity (%) | 95% CI | PPV (%) | 95% CI | NPV (%) | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Epidemic period | All Nm | 123 | 64 | 8 | 3 | 198 | 96 | (88;99) | 94 | (88;97) | 89 | (79;95) | 98 | (93;100) |
| NmA | 197 | NA | 1 | NA | 198 | NA | NA | 100 | (97;100) | NA | NA | 100 | (98;100) | |
| NmC | 143 | 45 | 5 | 4 | 197 | 92 | (80;98) | 97 | (92;99) | 90 | (78;97) | 97 | (93;99) | |
| NmW | 197 | NA | 1 | NA | 198 | NA | NA | 100 | (97;100) | NA | NA | 100 | (98;100) | |
| NmX | 176 | 17 | 4 | 1 | 198 | 94 | (73;100) | 98 | (94;99) | 81 | (58;95) | 99 | (97;100) | |
| NmY | 196 | NA | 1 | NA | 197 | NA | NA | 100 | (97;100) | NA | NA | 100 | (98;100) | |
| Sp | 174 | 17 | 3 | 2 | 196 | 90 | (67;99) | 98 | (95;100) | 85 | (62;97) | 99 | (96;100) | |
| Non epidemic period | All Nm | 94 | 18 | 16 | 1 | 129 | 95 | (74;100) | 86 | (78;92) | 53 | (35;70) | 99 | (94;100) |
| NmA | 121 | NA | 8 | NA | 129 | NA | NA | 94 | (88;97) | NA | NA | 100 | (97;100) | |
| NmC | 123 | 5 | 1 | NA | 129 | 100 | (48;100) | 99 | (96;100) | 83 | (36;100) | 100 | (97;100) | |
| NmW | 127 | NA | 1 | NA | 128 | NA | NA | 99 | (96;100) | NA | NA | 100 | (97;100) | |
| NmX | 108 | 12 | 7 | 2 | 129 | 86 | (57;98) | 94 | (88;98) | 63 | (38;84) | 98 | (94;100) | |
| NmY | 128 | NA | NA | NA | 128 | NA | NA | 100 | (97;100) | NA | NA | 100 | (97;100) | |
| Sp | 119 | 7 | 1 | NA | 127 | 100 | (59;100) | 99 | (95;100) | 88 | (47;100) | 100 | (97;100) | |
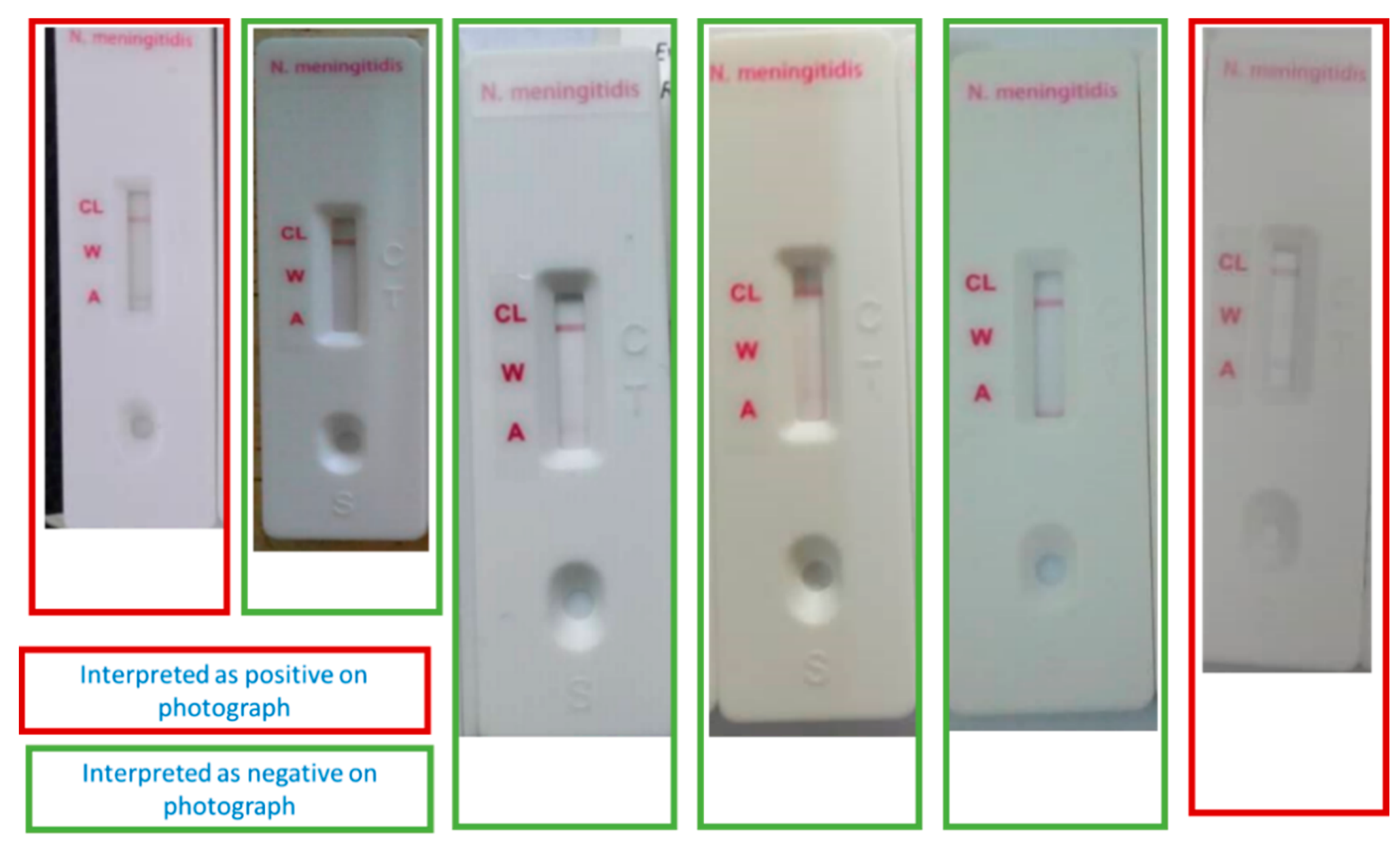
| Test | Photo Reading Negative/RDT Negative | Photo Reading Positive/RDT Positive | Photo Reading Negative/RDT Positive | Photo Reading Positive/RDT Negative | Total | Concordance (%) | Kappa Coefficient | |
|---|---|---|---|---|---|---|---|---|
| RDTs at health centers | All Nm | 36 | 17 | 11 | 1 | 65 | 82 | 61 |
| NmA | 64 | 2 | 6 | 1 | 73 | 90 | 32 | |
| NmC | 71 | 1 | 3 | 0 | 75 | 96 | 39 | |
| NmW | 68 | 1 | 0 | 4 | 73 | 95 | 32 | |
| NmX | 53 | 13 | 4 | 0 | 70 | 94 | 83 | |
| NmY | 71 | 0 | 0 | 0 | 71 | 100 | NA | |
| Sp | 66 | 5 | 1 | 1 | 73 | 97 | 82 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rondy, M.; Tamboura, M.; Sidikou, F.; Yameogo, I.; Dinanibe, K.; Sawadogo, G.; Kambire, C.; Mainassara, H.; Mahamane, A.E.; Bienvenu, B.; et al. Field Evaluation of the Performance of Two Rapid Diagnostic Tests for Meningitis in Niger and Burkina Faso. Microorganisms 2021, 9, 832. https://doi.org/10.3390/microorganisms9040832
Rondy M, Tamboura M, Sidikou F, Yameogo I, Dinanibe K, Sawadogo G, Kambire C, Mainassara H, Mahamane AE, Bienvenu B, et al. Field Evaluation of the Performance of Two Rapid Diagnostic Tests for Meningitis in Niger and Burkina Faso. Microorganisms. 2021; 9(4):832. https://doi.org/10.3390/microorganisms9040832
Chicago/Turabian StyleRondy, Marc, Mamadou Tamboura, Fati Sidikou, Issaka Yameogo, Kambire Dinanibe, Guetwende Sawadogo, Chantal Kambire, Halima Mainassara, Ali Elhaj Mahamane, Baruani Bienvenu, and et al. 2021. "Field Evaluation of the Performance of Two Rapid Diagnostic Tests for Meningitis in Niger and Burkina Faso" Microorganisms 9, no. 4: 832. https://doi.org/10.3390/microorganisms9040832
APA StyleRondy, M., Tamboura, M., Sidikou, F., Yameogo, I., Dinanibe, K., Sawadogo, G., Kambire, C., Mainassara, H., Mahamane, A. E., Bienvenu, B., Moussa, H., Ouedraogo, R., Fernandez, K., Taha, M.-K., & Ronveaux, O. (2021). Field Evaluation of the Performance of Two Rapid Diagnostic Tests for Meningitis in Niger and Burkina Faso. Microorganisms, 9(4), 832. https://doi.org/10.3390/microorganisms9040832





