Seroprevalence Estimates of Latent and Acute Toxoplasma Infections in HIV+ People—Call for Action in Underprivileged Communities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Data Extraction and Assessment of Quality
2.3. Statistical Analysis
3. Results
3.1. Study Characteristics
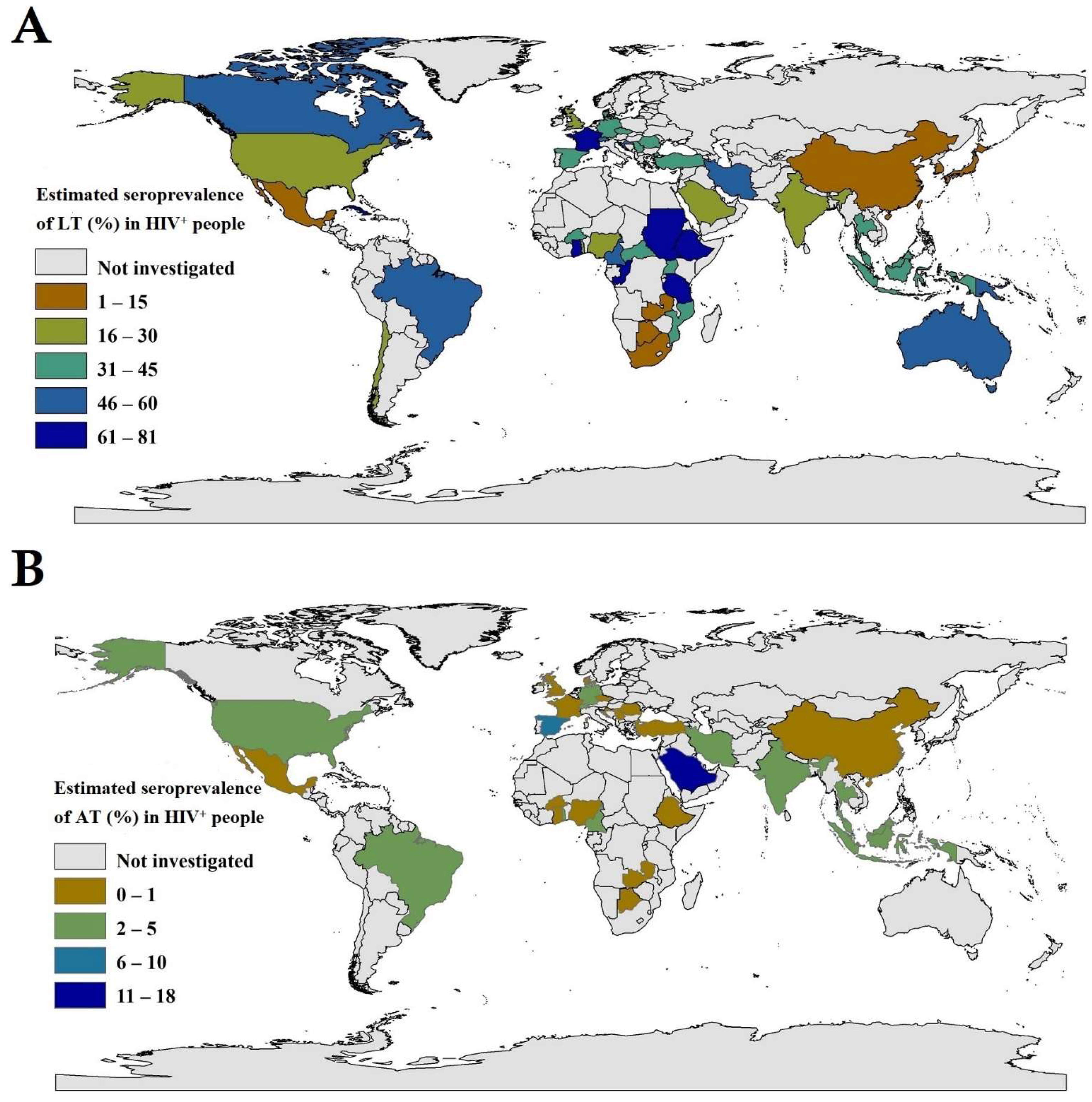
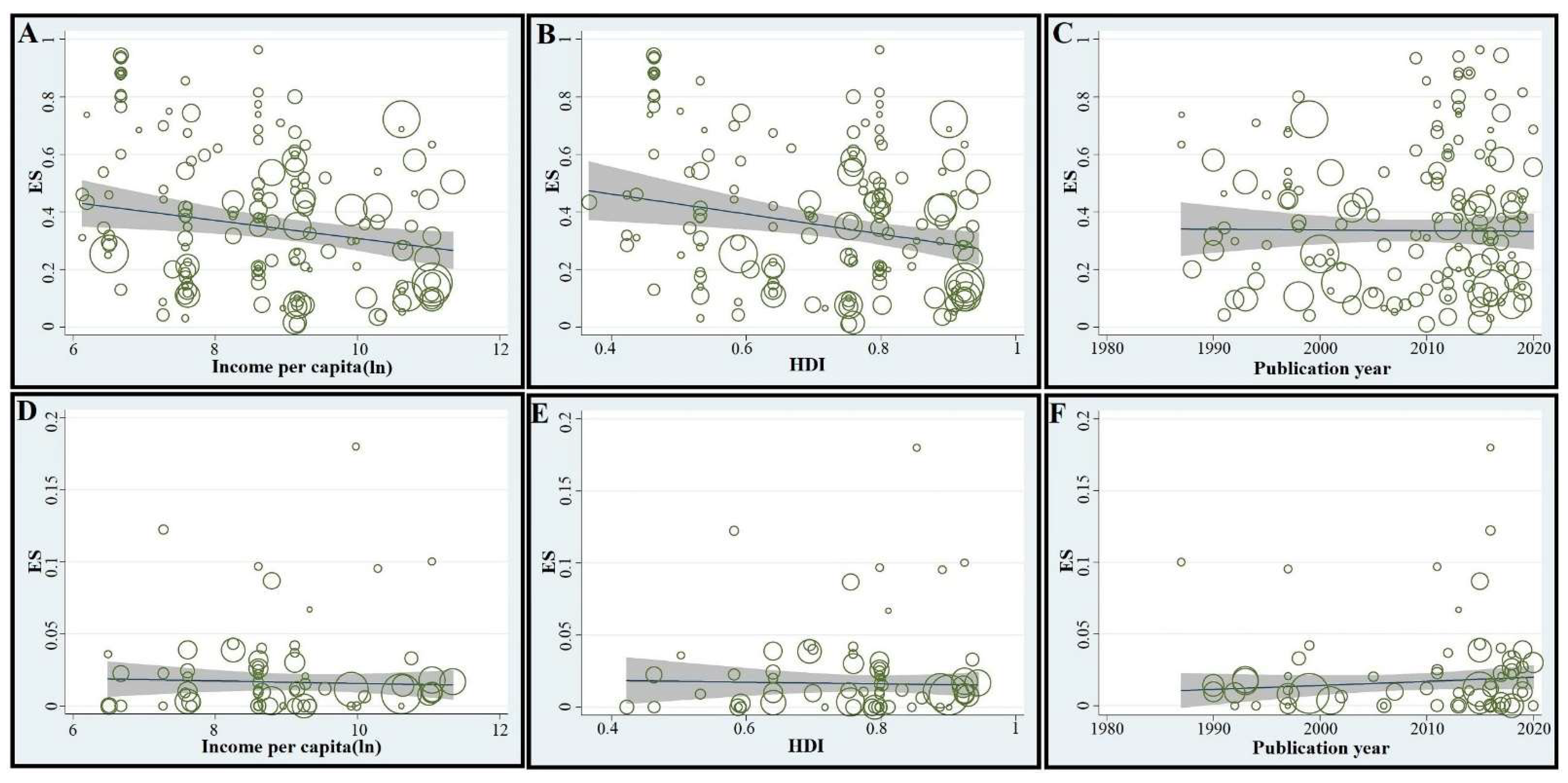
3.2. Global and Regional Seroprevalence Estimates in the LT-Group of HIV+ People, and Associated Socio-Demographic Aspects and Risk Factors
3.3. Global and Regional Seroprevalence Estimates in the AT-Group of HIV+ People, and Associated Socio-Demographic Aspects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Belanger, F.; Derouin, F.; Grangeot-Keros, L.; Meyer, L.; HEMOCO and SEROCO Study Groups. Incidence and risk factors of toxoplasmosis in a cohort of human immunodeficiency virus-infected patients: 1988–1995. Clin. Infect. Dis. 1999, 28, 575–581. [Google Scholar] [CrossRef] [Green Version]
- Luft, B.J.; Remington, J.S. Toxoplasmic encephalitis in AIDS. Clin. Infect. Dis. 1992, 15, 211–222. [Google Scholar] [CrossRef]
- Richards, F.O.; Kovacs, J.A.; Luft, B.J. Preventing toxoplasmic encephalitis in persons infected with human immunodeficiency virus. Clin. Infect. Dis. 1995, 21, S49–S56. [Google Scholar] [CrossRef]
- Robert-Gangneux, F.; Dardé, M.-L. Epidemiology of and diagnostic strategies for toxoplasmosis. Clin. Microbiol. Rev. 2012, 25, 264–296. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basavaraju, A. Toxoplasmosis in HIV infection: An overview. Trop. Parasitol. 2016, 6, 129–135. [Google Scholar] [CrossRef] [Green Version]
- Foroutan, M.; Rostami, A.; Majidiani, H.; Riahi, S.M.; Khazaei, S.; Badri, M.; Yousefi, E. A systematic review and meta-analysis of the prevalence of toxoplasmosis in hemodialysis patients in Iran. Epidemiol. Health 2018, 40, e2018016. [Google Scholar] [CrossRef] [PubMed]
- Rostami, A.; Riahi, S.M.; Contopoulos-Ioannidis, D.G.; Gamble, H.R.; Fakhri, Y.; Shiadeh, M.N.; Foroutan, M.; Behniafar, H.; Taghipour, A.; Maldonado, Y.A. Acute Toxoplasma infection in pregnant women worldwide: A systematic review and meta-analysis. PLoS Negl. Trop. Dis. 2019, 13, e0007807. [Google Scholar] [CrossRef] [Green Version]
- Rostami, A.; Riahi, S.M.; Gamble, H.R.; Fakhri, Y.; Shiadeh, M.N.; Danesh, M.; Behniafar, H.; Paktinat, S.; Foroutan, M.; Mokdad, A.H. Global prevalence of latent toxoplasmosis in pregnant women: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2020, 26, 673–683. [Google Scholar] [CrossRef] [PubMed]
- Shiadeh, M.N.; Esfandyari, S.; Ashrafmansouri, M.; Mirzapour, A.; Taghipour, A.; Spotin, A.; Arefkhah, N.; Gamble, R.; Safa, A.; Rostami, A. The prevalence of latent and acute toxoplasmosis in HIV-infected pregnant women: A systematic review and meta-analysis. Microb. Pathog. 2020, 149, 104549. [Google Scholar] [CrossRef]
- Nourollahpour Shiadeh, M.; Rostami, A.; Pearce, B.; Gholipourmalekabadi, M.; Newport, D.J.; Danesh, M.; Mehravar, S.; Seyyedtabaei, S. The correlation between Toxoplasma gondii infection and prenatal depression in pregnant women. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1829–1835. [Google Scholar] [CrossRef]
- Hill, D.; Dubey, J. Toxoplasma gondii: Transmission, diagnosis and prevention. Clin. Microbiol. Infect. 2002, 8, 634–640. [Google Scholar] [CrossRef] [Green Version]
- Munoz, M.; Liesenfeld, O.; Heimesaat, M.M. Immunology of Toxoplasma Gondii. Immunol. Rev. 2011, 240, 269–285. [Google Scholar] [CrossRef] [PubMed]
- Shearer, G.; Bernstein, D.; Tung, K.; Via, C.; Redfield, R.; Salahuddin, S.; Gallo, R. A model for the selective loss of major histocompatibility complex self-restricted T cell immune responses during the development of acquired immune deficiency syndrome (AIDS). J. Immunol. 1986, 137, 2514–2521. [Google Scholar] [PubMed]
- Khan, I.A.; Hwang, S.; Moretto, M. Toxoplasma gondii: CD8 T cells cry for CD4 help. Front. Cell. Infect. Microbiol. 2019, 9, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nissapatorn, V.; Lee, C.; Quek, K.F.; Leong, C.L.; Mahmud, R.; Abdullah, K.A. Toxoplasmosis in HIV/AIDS patients: A current situation. Jpn. J. Infect. Dis. 2004, 57, 160–165. [Google Scholar] [PubMed]
- Dzitko, K.; Staczek, P.; Gatkowska, J.; Dlugonska, H. Toxoplasma gondii: Serological recognition of reinfection. Exp. Parasitol. 2006, 112, 134–137. [Google Scholar] [CrossRef]
- Wang, Z.-D.; Liu, H.-H.; Ma, Z.-X.; Ma, H.-Y.; Li, Z.-Y.; Yang, Z.-B.; Zhu, X.-Q.; Xu, B.; Wei, F.; Liu, Q. Toxoplasma gondii infection in immunocompromised patients: A systematic review and meta-analysis. Front. Microbiol. 2017, 8, 389. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, J.E.; Benson, C.; Holmes, K.K.; Brooks, J.T.; Pau, A.; Masur, H.; National Institutes of Health; Centers for Disease Control and Prevention (CDC); HIV Medicine Association of the Infectious Diseases Society of America. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents. MMWR Recomm. Rep. 2009, 58, 1–207. [Google Scholar]
- Rostami, A.; Keshavarz, H.; Shojaee, S.; Mohebali, M.; Meamar, A.R. Frequency of Toxoplasma gondii in HIV positive patients from West of Iran by ELISA and PCR. Iran. J. Parasitol. 2014, 9, 474–481. [Google Scholar]
- Sari, Y.; Haryati, S.; Raharjo, I.; Prasetyo, A.A. Toxoplasma and viral antibodies among HIV patients and inmates in central Java, Indonesia. Southeast Asian J. Trop. Med. Public Health 2015, 46, 977–985. [Google Scholar]
- Mirambo, M.M.; Kivambe, C.; Mushi, M.F.; Zinga, M.; Mngumi, E.B.; Mtebe, M.; Mshana, S.E. High seroprevalence of specific Toxoplasma gondii IgG antibodies among HIV/AIDS patients with immunological failure attending a tertiary hospital in northwestern Tanzania. Tanzan. J. Health Res. 2016, 18, 1–4. [Google Scholar]
- Zeleke, A.J.; Melsew, Y.A. Seroprevalence of Toxoplasma gondii and associated risk factors among HIV-infected women within reproductive age group at Mizan Aman General Hospital, Southwest Ethiopia: A cross sectional study. BMC Res. Notes 2017, 10, 70. [Google Scholar] [CrossRef] [Green Version]
- Hoshina, T.; Horino, T.; Saiki, E.; Aonuma, H.; Sawaki, K.; Miyajima, M.; Lee, K.; Nakaharai, K.; Shimizu, A.; Hosaka, Y. Seroprevalence and associated factors of Toxoplasma gondii among HIV-infected patients in Tokyo: A cross sectional study. J. Infect. Chemother. 2020, 26, 33–37. [Google Scholar] [CrossRef]
- Wang, Z.-D.; Wang, S.-C.; Liu, H.-H.; Ma, H.-Y.; Li, Z.-Y.; Wei, F.; Zhu, X.-Q.; Liu, Q. Prevalence and burden of Toxoplasma gondii infection in HIV-infected people: A systematic review and meta-analysis. Lancet HIV 2017, 4, e177–e188. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Villard, O.; Cimon, B.; L’ollivier, C.; Fricker-Hidalgo, H.; Godineau, N.; Houze, S.; Paris, L.; Pelloux, H.; Villena, I.; Candolfi, E. Serological diagnosis of Toxoplasma gondii infection: Recommendations from the French National Reference Center for Toxoplasmosis. Diagn. Microbiol. Infect. Dis. 2016, 84, 22–33. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). List of Member States by WHO Region and Mortality Stratum. 2003. Available online: https://www.who.int/mental_health/neurology/annexes_neuro_disorders_public_h_challenges.pdf (accessed on 15 December 2020).
- Munn, Z.; Moola, S.; Riitano, D.; Lisy, K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int. J. Health Policy Manag. 2014, 3, 123–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- DerSimonian, R.; Kacker, R. Random-effects model for meta-analysis of clinical trials: An update. Contemp. Clin. Trials 2007, 28, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Barendregt, J.J.; Doi, S.A.; Lee, Y.Y.; Norman, R.E.; Vos, T. Meta-analysis of prevalence. J. Epidemiol. Commun. Health 2013, 67, 974–978. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Number of People (All Ages) Living with HIV Estimates by WHO Region. 2019. Available online: https://apps.who.int/gho/data/view.main.22100WHO?lang=en (accessed on 15 December 2020).
- Hunter, J.P.; Saratzis, A.; Sutton, A.J.; Boucher, R.H.; Sayers, R.D.; Bown, M.J. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014, 67, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Dubey, J. Toxoplasma gondii oocyst survival under defined temperatures. J. Parasitol. 1998, 84, 862–865. [Google Scholar] [CrossRef]
- Rostami, A.; Seyyedtabaei, S.J.; Aghamolaie, S.; Behniafar, H.; Lasjerdi, Z.; Abdolrasouli, A.; Mehravar, S.; Alvarado-Esquivel, C. Seroprevalence and risk factors associated with Toxoplasma gondii infection among rural communities in Northern Iran. Rev Inst. Med. Trop. São Paulo 2016, 58, 70. [Google Scholar] [CrossRef] [Green Version]
- Kapperud, G.; Jenum, P.A.; Stray-Pedersen, B.; Melby, K.K.; Eskild, A.; Eng, J. Risk factors for Toxoplasma gondii infection in pregnancy: Results of a prospective case-control study in Norway. Am. J. Epidemiol. 1996, 144, 405–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baril, L.; Ancelle, T.; Goulet, V.; Thulliez, P.; Tirard-Fleury, V.; Carme, B. Risk factors for Toxoplasma infection in pregnancy: A case-control study in France. Scand. J. Infect. Dis. 1999, 31, 305–309. [Google Scholar]
- Boyer, K.M.; Holfels, E.; Roizen, N.; Swisher, C.; Mack, D.; Remington, J.; Withers, S.; Meier, P.; McLeod, R.; Group, T.S. Risk factors for Toxoplasma gondii infection in mothers of infants with congenital toxoplasmosis: Implications for prenatal management and screening. Am. J. Obstetr. Gynecol. 2005, 192, 564–571. [Google Scholar] [CrossRef]
- Jones, J.L.; Dargelas, V.; Roberts, J.; Press, C.; Remington, J.S.; Montoya, J.G. Risk factors for Toxoplasma gondii infection in the United States. Clin. Infect. Dis. 2009, 49, 878–884. [Google Scholar] [CrossRef] [Green Version]
- Gao, X.-J.; Zhao, Z.-J.; He, Z.-H.; Wang, T.; Yang, T.-B.; Chen, X.-G.; Shen, J.-L.; Wang, Y.; Lv, F.-L.; Hide, G. Toxoplasma gondii infection in pregnant women in China. Parasitology 2012, 139, 139–147. [Google Scholar] [CrossRef]
- Li, M.; Wu, J. Toxoplasma infection among pregnant women in Zhoushan city, Zhejiang Province. Chin. J. Health Educ. 2002, 18, 734–735. [Google Scholar]
- Cook, A.; Holliman, R.; Gilbert, R.; Buffolano, W.; Zufferey, J.; Petersen, E.; Jenum, P.; Foulon, W.; Semprini, A.; Dunn, D. Sources of Toxoplasma infection in pregnant women: European multicentre case-control study Commentary: Congenital toxoplasmosis—further thought for food. BMJ 2000, 321, 142–147. [Google Scholar] [CrossRef] [Green Version]
- Mahami-Oskouei, M.; Moradi, M.; Fallah, E.; Hamidi, F.; Akbari, N.A.R. Molecular detection and genotyping of Toxoplasma gondii in chicken, beef, and lamb meat consumed in Northwestern Iran. Iran. J. Parasitol. 2017, 12, 38–45. [Google Scholar]
- Jiang, C.; Li, Z.; Chen, P.; Chen, L. The seroprevalence of Toxoplasma gondii in Chinese population with cancer: A systematic review and meta-analysis. Medicine 2015, 94, e2274. [Google Scholar] [CrossRef] [PubMed]
- Robert-Gangneux, F.; Meroni, V.; Dupont, D.; Botterel, F.; Garcia, J.M.A.; Brenier-Pinchart, M.-P.; Accoceberry, I.; Akan, H.; Abbate, I.; Boggian, K.; et al. Toxoplasmosis in transplant recipients, Europe, 2010–2014. Emerg. Infect. Dis. 2018, 24, 1497–1504. [Google Scholar] [CrossRef] [PubMed]
- Rostami, A.; Karanis, P.; Fallahi, S. Advances in serological, imaging techniques and molecular diagnosis of Toxoplasma gondii infection. Infection 2018, 46, 303–315. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health (NIH). Guidelines for the Prevention and Treatment of Opportunistic Infections in Adults and Adolescents with HIV, Toxoplasma gondii Encephalitis. Available online: https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-opportunistic-infection/Toxoplasma-gondii-encephalitis?view=full (accessed on 22 June 2021).
- Rajapakse, S.; Weeratunga, P.; Rodrigo, C.; de Silva, N.L.; Fernando, S.D. Prophylaxis of human toxoplasmosis: A systematic review. Pathog. Glob. Health 2017, 111, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Manuel, L.; Santos-Gomes, G.; Noormahomed, E.V. Human toxoplasmosis in Mozambique: Gaps in knowledge and research opportunities. Parasites Vectors 2020, 13, 1–10. [Google Scholar] [CrossRef] [PubMed]
| WHO Region/Country | No. of Datasets | No. of HIV+ People Screened (Total) | No. of HIV+ People with LT | Pooled Sero- Prevalence (95% CI) | Estimated No. of HIV+ People with LT * |
|---|---|---|---|---|---|
| Global | 155 | 44,473 | 14,913 | 37.4 (33.4–41.4) | 14,174,600 (12,658,600–15,690,600) |
| South Americas | 9 | 2905 | 1270 | 46.2 (23.6–69.6) | 877,800 (448,400–1,322,400) |
| Brazil | 8 | 650 | 1203 | 48.8 (23.5–74.5) | 439,200 (211,500–670,500) |
| Chile | 1 | 255 | 67 | 26.3 (21.0–32.1) | 18,673 (14,910–22,791) |
| Africanregion | 49 | 9504 | 3967 | 46.2 (37.7–54.70) | 11,873,400 (9,688,900–14,057,900) |
| Ethiopia | 12 | 1778 | 1396 | 80.5 (66.3–91.6) | 555,450 (457,740–632,040) |
| Nigeria | 12 | 2149 | 709 | 30.3 (19.2–42.7) | 575,700 (364,800–811,300) |
| Burkina Faso | 5 | 2548 | 691 | 30.7 (25.5–36.2) | 29,472 (24,480–34,752) |
| Cameroon | 3 | 293 | 167 | 54.5 (37.5–71.1) | 294,300 (202,500–383,940) |
| Ghana | 2 | 519 | 365 | 70.6 (66.6–74.4) | 232,980 (219,780–245,520) |
| Uganda | 2 | 316 | 134 | 42.3 (36.9–47.8) | 592,200 (516,600–669,200) |
| South Africa | 2 | 407 | 62 | 13.5 (10.3–17.0) | 1,039,000 (793,100–1,309,000) |
| Zambia | 2 | 256 | 14 | 5.2 (2.7–8.4) | 62,400 (32,400–100,800) |
| Mozambique | 2 | 258 | 110 | 42.5 (36.5–47.7) | 935,000 (803,000–1,049,400) |
| Tanzania | 1 | 38 | 26 | 68.4 (51.3–82.5) | 1,094,400 (820,800–1,320,000) |
| Canary island (Spain) | 1 | 157 | 56 | 35.7 (28.2–43.7) | 49,000 (39,480–61,180) |
| Botswana | 1 | 46 | 3 | 6.5 (1.4–17.9) | 24,050 (5180–66,230) |
| Togo | 1 | 56 | 14 | 25.0 (14.4–38.4) | 27,500 (15,840–42,240) |
| Congo | 1 | 375 | 75 | 22.0 (19.1–26.4) | 19,580 (16,999–23,496) |
| Congo (Democratic Republic of the) | 1 | 38 | 28 | 73.6 (52.5–94.6) | 331,200 (236,250–425,700) |
| Central African Republic | 1 | 270 | 117 | 43.3 (37.3–49.5) | 47,630 (41,030–54,450) |
| Eastern Mediterranean | 23 | 3151 | 1271 | 45.8 (36.3–55.5) | 183,200 (145,200–222,000) |
| Iran | 19 | 2886 | 1148 | 45.7 (35.3–56.3) | 27,877 (21,533–34,343) |
| Saudi Arabia | 1 | 50 | 15 | 30.0 (17.9–44.6) | 3,900 (2327–5798) |
| Bahrain | 1 | 76 | 16 | 21.1 (12.5–31.9) | 55 (32–83) |
| Morocco | 1 | 95 | 59 | 62.1 (51.6–71.9) | 13,041 (10,836–15,099) |
| Sudan | 1 | 44 | 33 | 75.0 (59.7–86.8) | 44,250 (35,223–51,212) |
| European region | 20 | 8786 | 4109 | 41.1 (33.0–49.4) | 1,027,500 (825,000–1,235,000) |
| Spain | 4 | 1707 | 562 | 30.7 (9.4–57.7) | 46,050 (14,100–86,550) |
| Turkey | 2 | 788 | 352 | 45.2 (41.7–48.7) | 6690 (6172–7207) |
| United Kingdom | 2 | 609 | 164 | 26.9 (23.4–30.5) | 27,330 (23,774–30,988) |
| France | 2 | 1715 | 1237 | 72.5 (70.3–74.6) | 130,500 (126,540–134,280) |
| Austria | 2 | 659 | 377 | 57.3 (53.5–61.1) | 5157 (4815–5499) |
| Romania | 2 | 224 | 69 | 30.5 (24.6–36.8) | 5490 (4428–6624) |
| Czech Republic | 2 | 1302 | 20 | 40.0 (37.4–42.7) | 1760 (1645–1879) |
| Croatia | 1 | 166 | 86 | 51.8 (43.9–59.6) | 829 (702–953) |
| Germany | 1 | 183 | 64 | 35.0 (28.1–42.4) | 30,450 (24,447–36,888) |
| Denmark | 1 | 503 | 223 | 44.3 (39.9–48.8) | 2746 (2474–3025) |
| Switzerland | 1 | 715 | 360 | 50.3 (46.6–54.1) | 10,060 (9320–10,820) |
| Serbia | 1 | 288 | 127 | 44.1 (38.3–50.0) | 1323 (1149–1500) |
| South-East AsianRegion | 18 | 5232 | 1582 | 29.8 (22.0–38.3) | 1,132,400 (836,000–1,455,400) |
| India | 10 | 2773 | 532 | 24.1 (16.8–32.2) | 530,200 (369,600–708,400) |
| Indonesia | 4 | 1131 | 447 | 38.5 (32.2–45.0) | 246,400 (206,080–288,000) |
| Thailand | 3 | 1328 | 603 | 37.5 (20.8–56.0) | 180,000 (99,840–268,800) |
| North America and the Caribbean | 12 | 7202 | 1150 | 25.5 (19.2–32.4) | 433,500 (326,400–550,800) |
| USA | 8 | 5862 | 889 | 18.3 (13.3–23.9) | 201,300 (146,300–262,900) |
| Mexico | 2 | 187 | 91 | 10.6 (8.8–12.6) | 24,380 (20,240–25,980) |
| Canada | 1 | 1074 | 14 | 48.7 (41.5–55.9) | 30,681 (26,148–35,217) |
| Cuba | 1 | 79 | 56 | 70.9 (59.6–80.6) | 21,979 (18,476–24,986) |
| Western PacificRegion | 24 | 7630 | 1530 | 18.4 (12.4–25.3) | 349,600 (235,600–480,700) |
| China | 10 | 3768 | 598 | 12.2 (5.5–20.9) | 109,800 (49,500–188,100) |
| Malaysia | 6 | 1507 | 511 | 36.1 (18.4–56.1) | 31,407 (16,008–48,807) |
| Japan | 4 | 680 | 67 | 9.9 (6.4–14.0) | 2970 (1920–4200) |
| Taiwan | 1 | 550 | 56 | 10.2 (7.8–13.0) | 4896 (3744–6240) |
| South-Korea | 1 | 173 | 7 | 4.0 (1.6–8.2) | 1800 (720–3690) |
| Singapore | 1 | 771 | 183 | 23.7 (20.8–26.9) | 1872 (1643–2125) |
| Papua New Guinea | 1 | 181 | 108 | 59.7 (52.1–66.9) | 26,865 (23,445–30,105) |
| Variable/Subgroups | No. of Datasets | Total No. of HIV+ People Screened | No. of HIV+ People with LT | Pooled Sero-Prevalence % (95% CI) | No. of HIV+ People with AT | Pooled Sero-Prevalence % (95% CI) | ||
|---|---|---|---|---|---|---|---|---|
| LT | AT | LT | AT | |||||
| Income | ||||||||
| Low | 27 | 5 | 5950 | 973 | 2675 | 58.2 (46.2–69.8) | 8 | 0.4 (0.0–1.9) |
| Lower middle | 35 | 13 | 7168 | 3389 | 2350 | 34.5 (27.0–42.3) | 72 | 1.8 (0.7–3.2) |
| Upper middle | 55 | 28 | 13,980 | 5764 | 4682 | 36.0 (29.2–43.1) | 105 | 1.4 (0.7–2.3) |
| High | 38 | 20 | 17,375 | 7579 | 5206 | 28.0 (21.3–35.2) | 104 | 1.2 (0.6–1.9) |
| HDI | ||||||||
| Low | 42 | 8 | 7969 | 1307 | 3533 | 51.9 (42.8–60.8) | 23 | 1.4 (0.1–3.7) |
| Medium | 22 | 12 | 5556 | 3462 | 1554 | 29.3 (20.9–38.4) | 64 | 1.5 (0.6–2.6) |
| High | 47 | 25 | 13,405 | 6858 | 45269 | 38.0 (22.6–33.1) | 109 | 1.3 (0.6–2.2) |
| Very high | 44 | 21 | 17,543 | 6078 | 4557 | 27.6 (22.6–33.1) | 93 | 1.3 (0.7–2.0) |
| Type of study | ||||||||
| Cross sectional | 95 | 44 | 24,576 | 8739 | 7941 | 38.7 (33.6–44.0) | 148 | 1.2 (0.7–1.8) |
| Case-control | 32 | 10 | 5204 | 1895 | 2059 | 40.4 (30.7–50.6) | 36 | 2.6 (0.8–5.0) |
| Prospective cohort | 9 | 4 | 3534 | 1591 | 1151 | 36.6 (19.1–56.1) | 34 | 2.1 (1.1–3.4) |
| Retrospective cohort | 19 | 8 | 11,159 | 5480 | 3762 | 26.5 (17.1–37.2) | 71 | 1.0 (0.3–1.0) |
| Criteria for AT | ||||||||
| IgG and IgM | na | 50 | na | 9872 | na | na | 166 | 1.2 (0.7–1.8) |
| Seroconversion | na | 12 | na | 6715 | na | na | 88 | 1.2 (0.8–1.7) |
| IgG avidity | na | 2 | na | 961 | na | na | 28 | 1.7 (1.0–2.7) |
| Antigen detection | na | 2 | na | 157 | na | na | 7 | 3.5 (1.0–7.2) |
| Year | ||||||||
| 1980–2000 | 35 | 17 | 11,920 | 5894 | 4282 | 37.5 (29.4–46.0) | 82 | 1.2 (0.6–1.9) |
| 2000–2005 | 14 | 3 | 6366 | 1095 | 1823 | 26.2 (17.3–36.2) | 6 | 0.5 (0.0–1.6) |
| 2006–2010 | 17 | 4 | 2893 | 726 | 803 | 28.7 (15.7–43.8) | 5 | 0.4 (0.0–1.2) |
| 2011–2015 | 49 | 16 | 12,386 | 4212 | 4475 | 45.3 (37.4–53.3) | 90 | 1.7 (0.7–3.2) |
| 2016–2020 | 40 | 26 | 10,908 | 5688 | 3530 | 35.6 (27.8–43.9) | 106 | 1.5 (0.7–2.5) |
| Sample size | ||||||||
| ≤99 | 45 | 20 | 2987 | 1338 | 1269 | 41.5 (33.7–49.6) | 55 | 2.9 (1.2–5.1) |
| 100–300 | 65 | 27 | 11,526 | 4782 | 4807 | 43.1 (36.3–50.1) | 77 | 1.0 (0.4–1.8) |
| 301–500 | 22 | 10 | 8372 | 4016 | 2067 | 22.0 (14.5–30.7) | 72 | 1.6 (1.0–2.4) |
| 501–1000 | 16 | 7 | 11,132 | 4651 | 3530 | 29.9 (19.7–41.1) | 57 | 0.9 (0.3–2.0) |
| >1000 | 7 | 2 | 10,456 | 2918 | 3241 | 29.8 (14.7–47.7) | 28 | 1.0 (0.6–1.3) |
| Risk of bias | ||||||||
| Low | 118 | 50 | 42,227 | 16,736 | 13,984 | 36.1 (31.6–40.6) | 249 | 1.2 (0.8–1.6) |
| Moderate | 37 | 16 | 2246 | 969 | 967 | 41.8 (33.4–41.4) | 40 | 2.8 (1.0–5.4) |
| Serological methods | ||||||||
| ELISA | 125 | na | 35,286 | na | 11,736 | 35.5 (31.1–40.1) | na | na |
| IFAT | 9 | na | 2828 | na | 1486 | 57.2 (47.0–67.1) | na | na |
| LAT | 5 | na | 658 | na | 395 | 61.9 (40.9–80.8) | na | na |
| MEIA | 5 | na | 1631 | na | 321 | 30.1 (14.3–48.8) | na | na |
| SFT | 6 | na | 3199 | na | 706 | 30.5 (14.9–48.9) | na | na |
| Other (MAT, CFT, ELFA or DAT) | 5 | na | 871 | na | 269 | 40.2 (15.4–68.0) | na | na |
| Variables (Number of Studies) | No. of HIV+ People | No. Seropositive for T. gondii | Pooled Sero- Prevalence (95% CI) | OR (95% CI) | Heterogeneity I2 (%) | Publication Bias p Value |t| |
|---|---|---|---|---|---|---|
| Gender (34) | 89.1 | 0.25 | ||||
| Female | 5806 | 2106 | 35.16 (34.28, 36.03) | 1 | ||
| Male | 7826 | 2363 | 29.44 (28.60, 30.28) | 0.78 (0.55–1.12) | ||
| Residence (9) | 36.9 | 0.44 | ||||
| Urban | 1472 | 820 | 59.73 (57.61, 61.84) | 1 | ||
| Rural | 283 | 166 | 67.29 (63.16, 71.42) | 1.45 (0.76–2.75) | ||
| Close contact with dog (3) | 90.1 | 0.98 | ||||
| No | 531 | 141 | 17.47 (14.89, 20.05) | 1 | ||
| Yes | 235 | 56 | 16.36 (12.46, 20.26) | 2.69 (0.55–13.18) | ||
| Close contact with cats (15) | 84.0 | 0.31 | ||||
| No | 1753 | 919 | 76.52 (74.94, 78.10) | 1 | ||
| Yes | 1039 | 611 | 75.39 (73.13, 77.64) | 1.79 (0.91–3.50) | ||
| Contact with soil (5) | 67.2 | 0.5 | ||||
| No | 442 | 219 | 46.84 (43.18, 50.49) | 1 | ||
| Yes | 316 | 236 | 83.92 (80.26, 87.58) | 3.01 (1.50–6.04) | ||
| Consumption of raw meat (15) | 78.5 | 0.88 | ||||
| No | 1626 | 892 | 68.09 (66.65, 69.53) | 1 | ||
| Yes | 1016 | 699 | 85.28 (83.54, 87.02) | 2.01 (1.19–3.39) | ||
| Consumption of raw/unwashed vegetable (8) | 13.7 | 0.26 | ||||
| No | 493 | 411 | 88.79 (86.14, 91.43) | 1 | ||
| Yes | 756 | 653 | 95.28 (93.82, 96.74) | 1.04 (0.68–1.6) | ||
| Drinking untreated water (5) | 45.5 | 0.19 | ||||
| No | 835 | 612 | 82.19 (79.95, 84.44) | 1 | ||
| Yes | 298 | 207 | 83.64 (80.24, 87.03) | 1.19 (0.67–2.11) | ||
| Number of CD4+ cells (29) | ||||||
| ≥ 500 | 1733 | 440 | 18.48 (16.88, 20.09) | 1 | ||
| 200–500 | 3625 | 1201 | 33.82 (32.68, 34.97) | 1.71 (1.08–2.72) | 50.9 | 0.71 |
| < 200 | 2511 | 700 | 21.97 (20.57, 23.36) | 1.04 (0.79–1.37) | 77.2 | 0.51 |
| Age (36) | ||||||
| < 20 | 1064 | 181 | 13.81 (11.86, 15.77) | 1 | ||
| 20–40 | 6824 | 2393 | 39.59 (38.70, 40.47) | 1.63 (1.15–2.61) | 42.3 | 0.06 |
| 40–60 | 2968 | 1295 | 46.33 (44.93, 47.74) | 2.49 (1.62–3.82) | 54.2 | 0.09 |
| >60 | 181 | 75 | 43.78 (37.19, 50.36) | 2.39 (1.56–3.66) | 0 | 0.48 |
| WHO Regions/Country | No. of Datasets | No. of HIV+ People Screened (Total) | No. of HIV+ People Estimated to Have AT | Pooled Prevalence (95% CI) | Estimated No. of HIV+ People with AT * |
|---|---|---|---|---|---|
| Global | 65 | 17,705 | 289 | 1.3 (0.9–1.8) | 492,700 (341,100–682,200) |
| South Americas | 4 | 863 | 20 | 2.0 (0.1–5.4) | 38,000 (1900–102,600) |
| Brazil | 4 | 863 | 20 | 2.0 (0.1–5.4) | 38,000 (1900–102,600) |
| Africanregion | 15 | 2505 | 32 | 0.9 (0.2–1.2) | 231,300 (51,400–308,400) |
| Burkina Faso | 2 | 497 | 0 | 0.1 (0.0–0.4) | 96 (0–384) |
| Cameroon | 2 | 223 | 14 | 5.4 (2.7–8.9) | 29,160 (14,580–48,060) |
| Ghana | 2 | 519 | 1 | 0.1 (0.0–0.8) | 330 (0–2640) |
| South Africa | 2 | 407 | 7 | 1.4 (0.4–2.9) | 107,800 (30,800–223,300) |
| Ethiopia | 1 | 150 | 0 | 1.1 (0.2–2.4) | 7590 (1380–16,560) |
| Nigeria | 1 | 111 | 1 | 0.9 (0.1–4.9) | 17,100 (1900–93,100) |
| Zambia | 1 | 69 | 0 | 0.1 (0.0–5.2) | 1200 (0–62,400) |
| Canary island (Spain) | 1 | 157 | 1 | 0.6 (0.0–3.5) | 840 (0–4900) |
| Botswana | 1 | 46 | 0 | 0.1 (0.0–7.7) | 370 (0–28,490) |
| Togo | 1 | 56 | 2 | 3.6 (0.4–12.3) | 3960 (440–13,530) |
| Eastern Mediterranean | 15 | 2125 | 51 | 1.8 (0.7–3.3) | 7200 (2800–13,200) |
| Iran | 13 | 1999 | 42 | 1.5 (0.6–2.7) | 915 (366–1647) |
| Saudi Arabia | 1 | 50 | 9 | 18.0 (8.6–31.4) | 2340 (1118–4082) |
| Bahrain | 1 | 76 | 0 | 0.1 (0.0–4.7) | 2 (0–12.2) |
| European region | 15 | 6447 | 67 | 0.6 (0.2–1.3) | 15,000 (5000–32,500) |
| Turkey | 2 | 788 | 0 | 0.1 (0.0–0.2) | 15 (0–29.6) |
| France | 2 | 1715 | 14 | 0.3 (0.0–0.7) | 540 (0–1260) |
| Romania | 2 | 224 | 2 | 0.1 (0.0–1.0) | 18 (0–180) |
| Czech Republic | 2 | 1302 | 14 | 0.8 (0.3–1.4) | 35 (13–61) |
| Spain | 1 | 63 | 6 | 9.5 (3.6–19.6) | 14,250 (5400–29,400) |
| United Kingdom | 1 | 500 | 7 | 1.4 (0.6–2.9) | 1422 (609–2946) |
| Croatia | 1 | 166 | 2 | 1.2 (0.1–4.3) | 19 (2–69) |
| Germany | 1 | 183 | 6 | 3.3 (1.2–7.0) | 2871 (1044–6090) |
| Denmark | 1 | 503 | 4 | 0.8 (0.2–2.0) | 49 (12–124) |
| Switzerland | 1 | 715 | 12 | 1.7 (0.9–2.9) | 340 (180–580) |
| Serbia | 1 | 288 | 0 | 0.1 (0.0–1.3) | 3 (0–39) |
| North America and the Caribbean | 5 | 1729 | 28 | 1.6 (0.5–3.1) | 27,200 (8500–52,700) |
| USA | 4 | 1637 | 27 | 1.7 (0.5–3.6) | 18,700 (5500–39,600) |
| Mexico | 1 | 92 | 1 | 1.1 (0.1–5.9) | 2530 (230–13,570) |
| South-East Asian Region | 9 | 3605 | 85 | 1.3 (0.9–1.8) | 49,400 (34,200–68,400) |
| India | 5 | 1730 | 27 | 1.6 (0.4–3.4) | 35,200 (8800–74,800) |
| Indonesia | 3 | 737 | 29 | 3.9 (2.5–5.4) | 24,960 (16,000–34,560) |
| Thailand | 2 | 1138 | 29 | 1.5 (0.8–2.3) | 7200 (3840–11,040) |
| Western Pacific Region | 3 | 441 | 6 | 1.2 (0.2–2.6) | 22,800 (3800–49,400) |
| Malaysia | 2 | 182 | 3 | 1.5 (0.1–4.1) | 1305 (87–3567) |
| China | 1 | 259 | 3 | 1.2 (0.2–3.3) | 10,800 (1800–29,700) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rostami, A.; Riahi, S.M.; Abdollahzadeh Sagha, S.; Taghipour, A.; Sepidarkish, M.; Mohammadnia-Afrouzi, M.; Ebrahimpour, S.; Hotez, P.J.; Gamble, R.; Gasser, R.B. Seroprevalence Estimates of Latent and Acute Toxoplasma Infections in HIV+ People—Call for Action in Underprivileged Communities. Microorganisms 2021, 9, 2034. https://doi.org/10.3390/microorganisms9102034
Rostami A, Riahi SM, Abdollahzadeh Sagha S, Taghipour A, Sepidarkish M, Mohammadnia-Afrouzi M, Ebrahimpour S, Hotez PJ, Gamble R, Gasser RB. Seroprevalence Estimates of Latent and Acute Toxoplasma Infections in HIV+ People—Call for Action in Underprivileged Communities. Microorganisms. 2021; 9(10):2034. https://doi.org/10.3390/microorganisms9102034
Chicago/Turabian StyleRostami, Ali, Seyed Mohammad Riahi, Shayan Abdollahzadeh Sagha, Ali Taghipour, Mahdi Sepidarkish, Mousa Mohammadnia-Afrouzi, Soheil Ebrahimpour, Peter J. Hotez, Ray Gamble, and Robin B. Gasser. 2021. "Seroprevalence Estimates of Latent and Acute Toxoplasma Infections in HIV+ People—Call for Action in Underprivileged Communities" Microorganisms 9, no. 10: 2034. https://doi.org/10.3390/microorganisms9102034
APA StyleRostami, A., Riahi, S. M., Abdollahzadeh Sagha, S., Taghipour, A., Sepidarkish, M., Mohammadnia-Afrouzi, M., Ebrahimpour, S., Hotez, P. J., Gamble, R., & Gasser, R. B. (2021). Seroprevalence Estimates of Latent and Acute Toxoplasma Infections in HIV+ People—Call for Action in Underprivileged Communities. Microorganisms, 9(10), 2034. https://doi.org/10.3390/microorganisms9102034







