Helicobacter pylori and Respiratory Diseases: 2021 Update
Abstract
1. Introduction
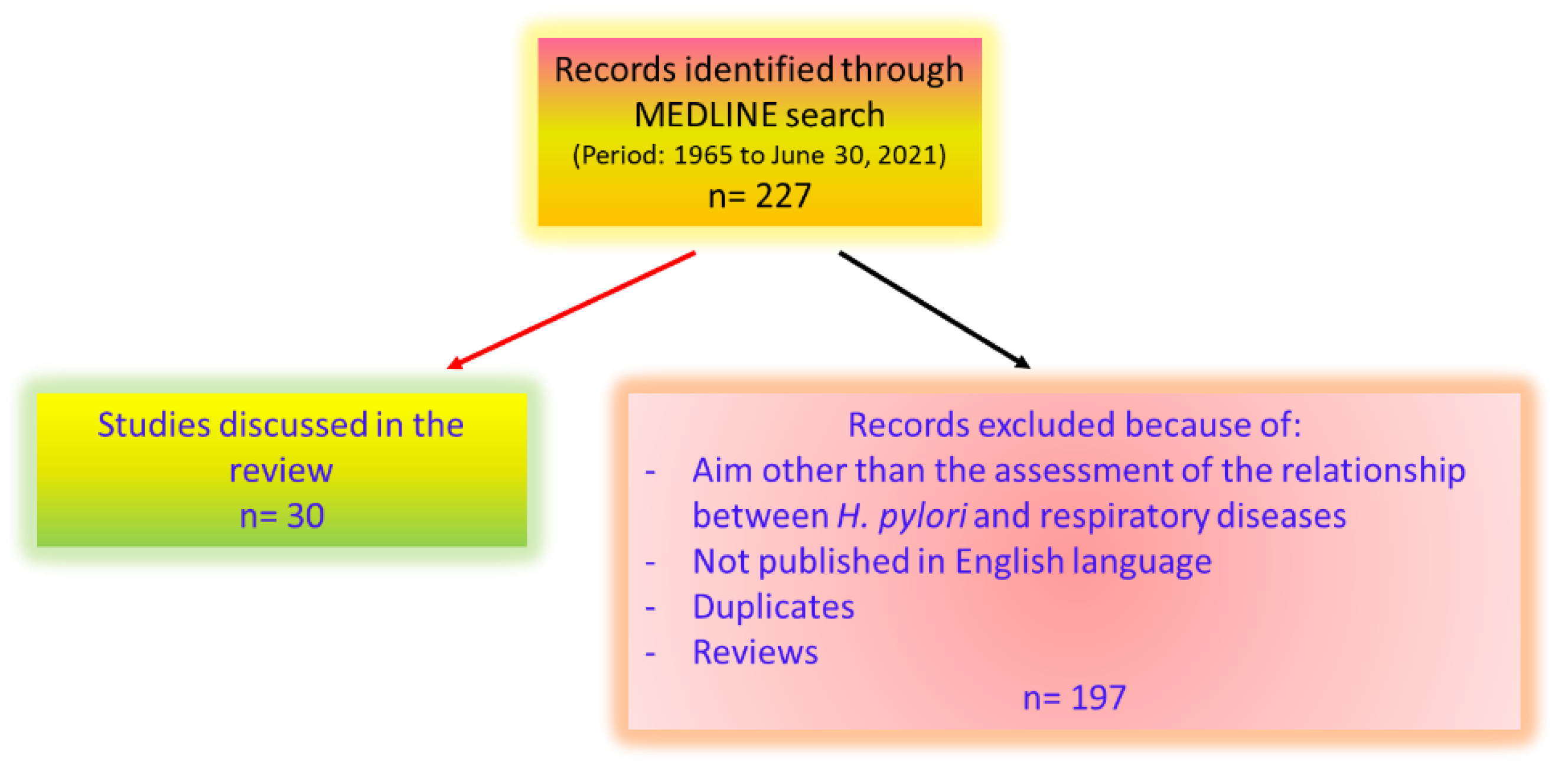
2. Materials and Methods
3. Results
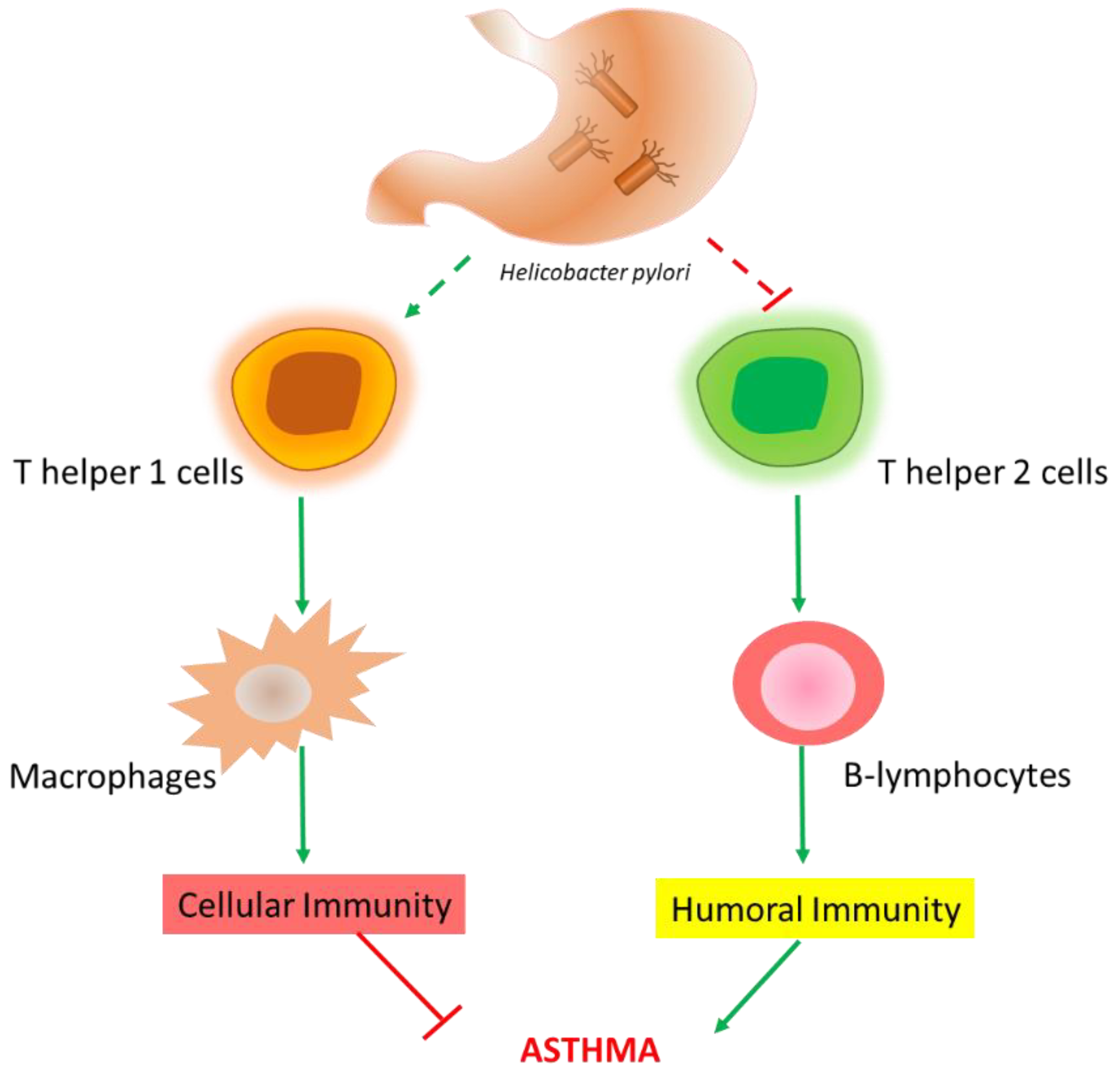
3.1. H. pylori Infection and Asthma
3.2. H. pylori Infection and Chronic Obstructive Pulmonary Disease
| Respiratory Disease | Result | Reference | Publication Year | |
|---|---|---|---|---|
| Meta-analysis of 18 studies | Negative association with H. pylori infection | [16] | 2021 | |
| ASTHMA | Case-control study including 10,000 patients | Only in obese patients H. pylori associated with 30–40% OR of asthma ↓ | [17] | 2019 |
| Cohort study | 16% of children uninfected at 2 and 10 years developed asthma at 16 years versus none of the children with H. pylori at 2 years | [19] | 2020 | |
| CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD) | Case-control study including patients with type 2 diabetes mellitus and controls | In diabetics, seropositivity was significantly associated with chronic bronchitis | [31] | 2020 |
| Retrospective cohort study (Taiwan) | Significant association between H. pylori and COPD | [32] | 2017 | |
| Case-control study (Korea, country with high burden of H. pylori) | No association between H. pylori and COPD | [33] | 2016 |
3.3. H. pylori Infection and Bronchiectasis
3.4. H. pylori Infection and Lung Cancer
3.5. H. pylori Infection and Tuberculosis
3.6. H. pylori Infection and Cystic Fibrosis
3.7. H. pylori Infection and Sarcoidosis
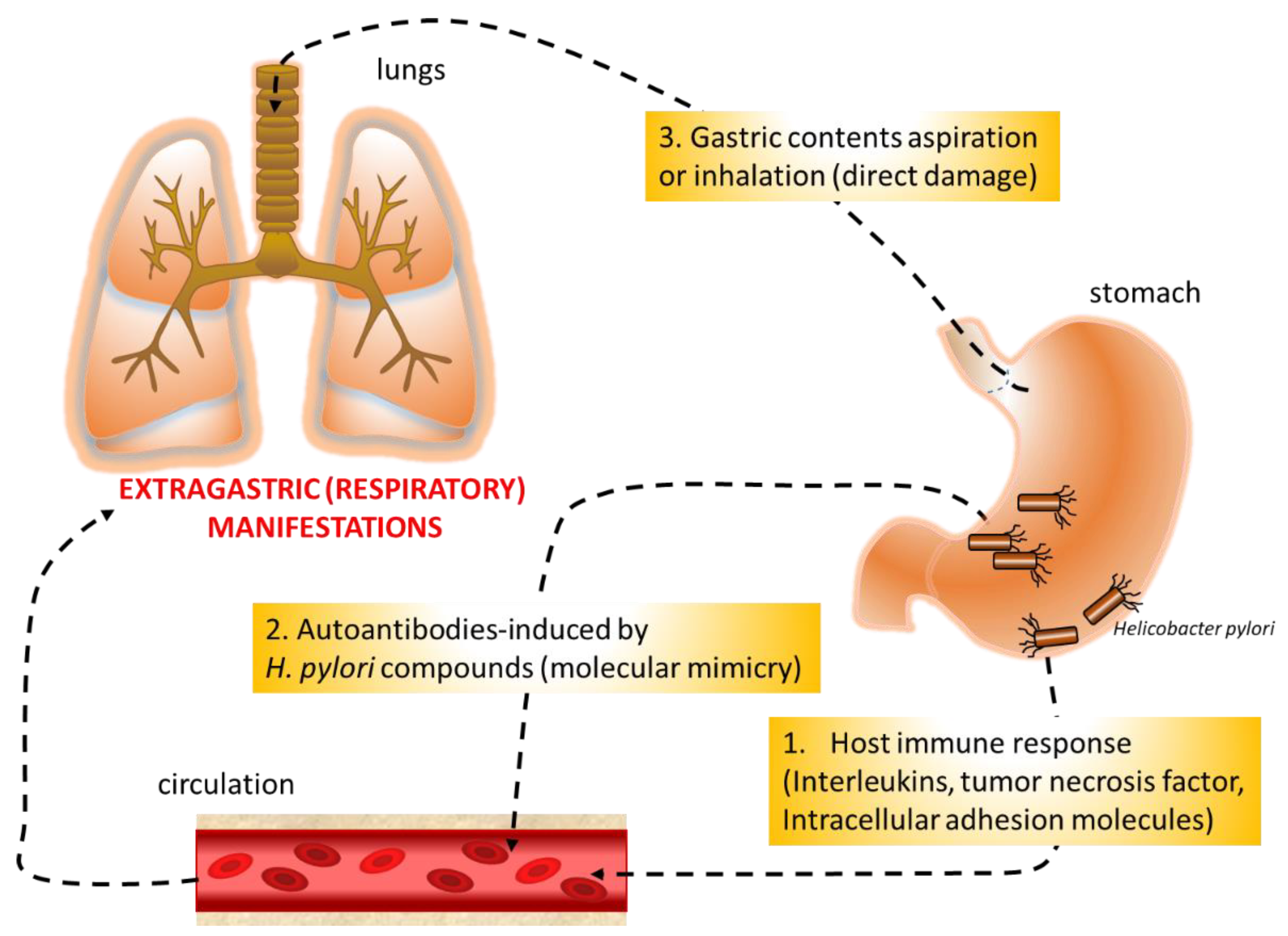
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- McColl, K.E. Clinical practice. Helicobacter pylori infection. N. Engl. J. Med. 2010, 362, 1597–1604. [Google Scholar] [CrossRef]
- Delport, W.; van der Merwe, S.W. The transmission of Helicobacter pylori: The effects of analysis method and study population on inference. Best Pract. Res. Clin. Gastroenterol. 2007, 21, 215–236. [Google Scholar] [CrossRef][Green Version]
- Fagoonee, S.; Pellicano, R. Helicobacter pylori: Molecular basis for colonization and survival in gastric environment and resistance to antibiotics. A short review. Infect. Dis. 2019, 51, 399–408. [Google Scholar] [CrossRef]
- Charitos, I.A.; D’Agostino, D.; Topi, S.; Bottalico, L. 40 years of Helicobacter pylori: A revolution in biomedical thought. Gastroenterol. Insights 2021, 12, 111–135. [Google Scholar] [CrossRef]
- Pellicano, R.; Ribaldone, D.G.; Fagoonee, S.; Astegiano, M.; Saracco, G.M.; Mégraud, F. A 2016 panorama of Helicobacter pylori infection: Key messages for clinicians. Panminerva Med. 2016, 58, 304–317. [Google Scholar] [CrossRef]
- Buzás, G.M. Helicobacter pylori and non-alcoholic fatty liver disease. Minerva Gastroenterol. Dietol. 2020, 66, 267–279. [Google Scholar] [CrossRef]
- Pellicano, R.; Ianiro, G.; Fagoonee, S.; Settanni, C.R.; Gasbarrini, A. Review: Extragastric diseases and Helicobacter pylori. Helicobacter 2020, 25 (Suppl. 1), e12741. [Google Scholar] [CrossRef]
- Doulberis, M.; Papaefthymiou, A.; Polyzos, S.A.; Bargiotas, P.; Liatsos, C.; Srivastava, D.S.; Zavos, C.; Katsinelos, P.; Kountouras, J. Association between active Helicobacter pylori infection and glaucoma: A systematic review and meta-analysis. Microorganisms 2020, 8, 894. [Google Scholar] [CrossRef]
- Doulberis, M.; Kotronis, G.; Gialamprinou, D.; Polyzos, S.A.; Papaefthymiou, A.; Katsinelos, P.; Kountouras, J. Alzheimer’s disease and gastrointestinal microbiota; impact of Helicobacter pylori infection involvement. Int. J. Neurosci. 2021, 131, 289–301. [Google Scholar] [CrossRef]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori infection—The Maastricht V/Florence Consensus Report. European Helicobacter and Microbiota Study Group and Consensus panel. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef]
- Forum of International Respiratory Societies. The Global Impact of Respiratory Disease—Second Edition. Sheffield, European Respiratory Society. 2017. Available online: www.https://www.who.int/gard/publications/The_Global_Impact_of_Respiratory_Disease.pdf (accessed on 30 June 2021).
- Arismendi Sosa, A.C.; Salinas Ibáñez, A.G.; Pérez Chaca, M.V.; Penissi, A.B.; Gómez, N.N.; Vega, A.E. Study of Helicobacter pylori infection on lung using an animal model. Microb. Pathog. 2018, 123, 410–418. [Google Scholar] [CrossRef]
- Dharmage, S.C.; Perret, J.L.; Custovic, A. Epidemiology of asthma in children and adults. Front. Pediatr. 2019, 7, 246. [Google Scholar] [CrossRef]
- Fullerton, D.; Britton, J.R.; Lewis, S.A.; Pavord, I.D.; McKeever, T.M.; Fogarty, A.W. Helicobacter pylori and lung function, asthma, atopy and allergic disease—A population-based cross-sectional study in adults. Int. J. Epidemiol. 2009, 38, 419–426. [Google Scholar] [CrossRef][Green Version]
- Tsang, K.W.; Lam, W.K.; Chan, K.N.; Hu, W.; Wu, A.; Kwok, E.; Zheng, L.; Wong, B.C.; Lam, S.K. Helicobacter pylori sero-prevalence in asthma. Respir. Med. 2000, 94, 756–759. [Google Scholar] [CrossRef][Green Version]
- Blaser, M.J.; Chen, Y.; Reibman, J. Does Helicobacter pylori protect against asthma and allergy? Gut 2008, 57, 561–567. [Google Scholar] [CrossRef]
- Chen, Y.; Zhan, X.; Wang, D. Association between Helicobacter pylori and risk of childhood asthma: A meta-analysis of 18 observational studies. J. Asthma 2021, 8, 1–11. [Google Scholar] [CrossRef]
- Ness-Jensen, E.; Langhammer, A.; Hveem, K.; Lu, Y. Helicobacter pylori in relation to asthma and allergy modified by abdominal obesity: The HUNT study in Norway. World Allergy Organ. J. 2019, 12, 100035. [Google Scholar] [CrossRef]
- Tsigalou, C.; Konstantinidis, T.G.; Cassimos, D.; Karvelas, A.; Grapsa, A.; Tsalkidis, A.; Panopoulou, M.; Tsakris, A. Inverse association between Helicobacter pylori infection and childhood asthma in Greece: A case-control study. Germs 2019, 9, 182–187. [Google Scholar] [CrossRef]
- Melby, K.K.; Carlsen, K.L.; Håland, G.; Samdal, H.H.; Carlsen, K.H. Helicobacter pylori in early childhood and asthma in adolescence. BMC Res. Notes 2020, 13, 79. [Google Scholar] [CrossRef]
- Zuo, Z.T.; Ma, Y.; Sun, Y.; Bai, C.Q.; Ling, C.H.; Yuan, F.L. The protective effects of Helicobacter pylori infection on allergic asthma. Int. Arch. Allergy Immunol. 2021, 182, 53–64. [Google Scholar] [CrossRef]
- Parsons, J.P.; Mastronarde, J.G. Gastroesophageal reflux disease and asthma. Curr. Opin. Pulm. Med. 2010, 16, 60–63. [Google Scholar] [CrossRef]
- Nijevitch, A.A.; Loguinovskaya, V.V.; Tyrtyshnaya, L.V.; Sataev, V.U.; Ogorodnikova, I.N.; Nuriakhmetova, A.N. Helicobacter pylori infection and reflux esophagitis in children with chronic asthma. J. Clin. Gastroenterol. 2004, 38, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Miftahussurur, M.; Nusi, I.A.; Graham, D.Y.; Yamaoka, Y. Helicobacter, hygiene, atopy, and asthma. Front. Microbiol. 2017, 8, 1034. [Google Scholar] [CrossRef] [PubMed]
- MacLeod, M.; Papi, A.; Contoli, M.; Beghé, B.; Celli, B.R.; Wedzicha, J.A.; Fabbri, M.L. Chronic obstructive pulmonary disease exacerbation fundamentals: Diagnosis, treatment, prevention and disease impact. Respirology 2021, 26, 532–551. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, S.; Jørgensen, T.; Andersen, L.P.; Bonnevie, O. Association of Helicobacter pylori infection with lifestyle, chronic disease, body indices, and age at menarche in Danish adults. Scand. J. Public Health 2000, 28, 32–40. [Google Scholar] [CrossRef]
- Caselli, M.; Zaffoni, E.; Ruina, M.; Sartori, S.; Trevisani, L.; Ciaccia, A.; Alvisi, V.; Fabbri, L.; Papi, A. Helicobacter pylori and chronic bronchitis. Scand. J. Gastroenterol. 1999, 34, 828–830. [Google Scholar] [CrossRef]
- Jun, Z.J.; Lei, Y.; Shimizu, Y.; Dobashi, K.; Mori, M. High seroprevalence of Helicobacter pylori in chronic bronchitis among Chinese population. Tohoku J. Exp. Med. 2006, 208, 327–331. [Google Scholar] [CrossRef]
- Roussos, A.; Philippou, N.; Krietsepi, V.; Anastasakou, E.; Alepopoulou, D.; Koursarakos, P.; Iliopoulos, I.; Gourgoulianis, K. Helicobacter pylori seroprevalence in patients with chronic obstructive pulmonary disease. Respir. Med. 2005, 99, 279–284. [Google Scholar] [CrossRef]
- Roussos, A.; Tsimpoukas, F.; Anastasakou, E.; Alepopoulou, D.; Paizis, I.; Philippou, N. Helicobacter pylori seroprevalence in patients with chronic bronchitis. J. Gastroenterol. 2002, 37, 332–335. [Google Scholar] [CrossRef]
- Siva, R.; Birring, S.S.; Berry, M.; Rowbottom, A.; Pavord, I.D. Peptic ulceration, Helicobacter pylori seropositivity and chronic obstructive pulmonary disease. Respirology 2013, 18, 728–731. [Google Scholar] [CrossRef]
- Bener, A.; Ağan, A.F.; Al-Hamaq, A.O.A.A.; Barisik, C.C.; Öztürk, M.; Ömer, A. Prevalence of Helicobacter pylori infection among type 2 diabetes mellitus. Adv. Biomed. Res. 2020, 9, 27. [Google Scholar] [CrossRef]
- Peng, Y.H.; Chen, C.K.; Su, C.H.; Liao, W.C.; Muo, C.H.; Hsia, T.C.; Sung, F.C.; Lai, C.H.; Kao, C.H. Increased risk of chronic obstructive pulmonary disease among patients with Helicobacter pylori infection: A population-based cohort study. Clin. Respir. J. 2017, 11, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Kim, J.W.; Lee, J.K.; Heo, E.Y.; Chung, H.S.; Kim, D.K. Association between Helicobacter pylori seropositivity and mild to moderate COPD: Clinical implications in an Asian country with a high prevalence of H. pylori. Int. J. Chronic Obstr. Pulm. Dis. 2016, 31, 2055–2062. [Google Scholar] [CrossRef]
- Lee, H.Y.; Kang, H.R.; Lee, J.K.; Heo, E.Y.; Choi, S.H.; Kim, D.K. The effect of Helicobacter pylori infection on the decline of lung function in a health screening population. Ann. Palliat. Med. 2020, 9, 3115–3122. [Google Scholar] [CrossRef] [PubMed]
- Bennett, D.; Fossi, A.; Chiarello, G.; Metella Refini, R.; Luzzi, L.; Paladini, P.; Materozzi, M.; Figura, N.; Nuti, R.; Rottoli, P. Helicobacter pylori infection does not impact on lung transplant outcome. Lung 2019, 197, 95–99. [Google Scholar] [CrossRef]
- Samareh Fekri, M.; Hashemi Bajgani, S.M.; Rasti, A.; Yazdani, R.; Mollaie, H.R. Detection of Helicobacter pylori in bronchoalveolar lavage of patients with chronic obstructive pulmonary disease by real time polymerase chain reaction. Jundishapur J. Microbiol. 2014, 8, e14551. [Google Scholar] [CrossRef]
- O’Donnell, A.E. Bronchiectasis update. Curr. Opin. Infect. Dis. 2018, 31, 194–198. [Google Scholar] [CrossRef]
- Patrucco, F.; Venezia, L.; Gavelli, F.; Pellicano, R.; Solidoro, P. Alpha1-antitrypsin deficiency: What’s new after European Respiratory Society Statement. Panminerva Med. 2018, 60, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Tsang, K.W.; Lam, S.K.; Lam, W.K.; Karlberg, J.; Wong, B.C.; Hu, W.H.; Yew, W.W.; Ip, M.S. High seroprevalence of Helicobacter pylori in active bronchiectasis. Am. J. Respir. Crit. Care Med. 1998, 158, 1047–1051. [Google Scholar] [CrossRef]
- Tsang, K.W.; Lam, W.K.; Kwok, E.; Chan, K.N.; Hu, W.H.; Ooi, G.C.; Zheng, L.; Wong, B.C.; Lam, S.K. Helicobacter pylori and upper gastrointestinal symptoms in bronchiectasis. Eur. Respir. J. 1999, 14, 1345–1350. [Google Scholar] [CrossRef]
- Angrill, J.; Sánchez, N.; Agustí, C.; Guilemany, J.M.; Miquel, R.; Gomez, J.; Torres, A. Does Helicobacter pylori have a pathogenic role in bronchiectasis? Respir. Med. 2006, 100, 1202–1207. [Google Scholar] [CrossRef][Green Version]
- Gülhan, M.; Ozyilmaz, E.; Tarhan, G.; Demirağ, F.; Capan, N.; Ertürk, A.; Canbakan, S.; Ayaşlioğlu, E.; Gülhan, E.; Ahmed, K. Helicobacter pylori in bronchiectasis: A polymerase chain reaction assay in bronchoalveolar lavage fluid and bronchiectatic lung tissue. Arch. Med. Res. 2007, 38, 317–321. [Google Scholar] [CrossRef]
- Aydın Teke, T.; Akyön, Y.; Yalcin, E.; Ozen, H.; Doğru, D.; Kiper, N.; Ozcelik, U. Does Helicobacter pylori play a role in the pathogenesis of non-cystic fibrosis bronchiectasis? Pediatr. Int. 2016, 58, 894–898. [Google Scholar] [CrossRef]
- Sun, S.; Schiller, J.; Gazdar, A. Lung cancer in never smokers—A different disease. Nat. Rev. Cancer 2007, 7, 778–790. [Google Scholar] [CrossRef] [PubMed]
- Philippou, N.; Koursarakos, P.; Anastasakou, E.; Krietsepi, V.; Mavrea, S.; Roussos, A.; Alepopoulou, D.; Iliopoulos, I. Helicobacter pylori seroprevalence in patients with lung cancer. World J. Gastroenterol. 2004, 10, 3342–3344. [Google Scholar] [CrossRef] [PubMed]
- Najafizadeh, K.; Falah Tafti, S.; Shiehmorteza, M.; Saloor, M.; Jamali, M. H pylori seroprevalence in patients with lung cancer. World J. Gastroenterol. 2007, 13, 2349–2351. [Google Scholar] [CrossRef] [PubMed]
- Koshiol, J.; Flores, R.; Lam, T.K.; Taylor, P.R.; Weinstein, S.J.; Virtamo, J.; Albanes, D.; Perez-Perez, G.; Caporaso, N.E.; Blaser, M.J. Helicobacter pylori seropositivity and risk of lung cancer. PLoS ONE 2012, 7, e32106. [Google Scholar] [CrossRef]
- Behroozian, R.; Moradkhan, E. The assessment of probable relationship between lung cancer and Helicobacter pylori infection. Trop. Gastroenterol. 2010, 31, 34–36. [Google Scholar] [PubMed]
- Ece, F.; Hatabay, N.F.; Erdal, N.; Gedik, C.; Guney, C.; Aksoy, F. Does Helicobacter pylori infection play a role in lung cancer? Respir. Med. 2005, 99, 1258–1262. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gocyk, W.; Nikliński, T.; Olechnowicz, H.; Duda, A.; Bielański, W.; Konturek, P.C.; Konturek, S.J. Helicobacter pylori, gastrin and cyclooxygenase-2 in lung cancer. Med. Sci. Monit. 2000, 6, 1085–1092. [Google Scholar]
- Mounika, P. Helicobacter pylori Infection and Risk of Lung Cancer: A Meta-Analysis. Lung Cancer Int. 2013, 2013, 131869. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bustamante-Rengifo, J.A.; Astudillo-Hernandez, M.; Crespo-Ortiz, M. Effect of Helicobacter pylori and helminth coinfection on the immune response to Mycobacterium tuberculosis. Curr. Microbiol. 2021, 78, 3351–3371. [Google Scholar] [CrossRef]
- Mitchell, H.M.; Li, Y.Y.; Hu, P.J.; Liu, Q.; Chen, M.; Du, G.G.; Wang, Z.J.; Lee, A.; Hazell, S.L. Epidemiology of Helicobacter pylori in southern China: Identification of early childhood as the critical period for acquisition. J. Infect. Dis. 1992, 166, 149–153. [Google Scholar] [CrossRef]
- Filippou, N.; Roussos, A.; Tsimpoukas, F.; Tsimogianni, A.; Anastasakou, E.; Mavrea, S. Helicobacter pylori seroprevalence in patients with pulmonary tuberculosis. J. Clin. Gastroenterol. 2002, 34, 189–190. [Google Scholar] [CrossRef]
- Sanaka, M.; Kuyama, Y.; Iwasaki, M.; Hanada, Y.; Tsuchiya, A.; Haida, T.; Hirama, S.; Yamaoka, S.; Yamanaka, M. No difference in seroprevalences of Helicobacter pylori infection between patients with pulmonary tuberculosis and those without. J. Clin. Gastroenterol. 1998, 27, 331–334. [Google Scholar] [CrossRef]
- Sanaka, M.; Kuyama, Y.; Yamanaka, M.; Iwasaki, M. Decrease in serum concentrations of Helicobacter pylori IgG antibodies during antituberculosis therapy: The possible eradication by rifampicin and streptomycin. Am. J. Gastroenterol. 1999, 94, 1983–1984. [Google Scholar] [CrossRef] [PubMed]
- Ribaldone, D.G.; Fagoonee, S.; Astegiano, M.; Durazzo, M.; Morgando, A.; Sprujevnik, T.; Giordanino, C.; Baronio, M.; De Angelis, C.; Saracco, G.M.; et al. Rifabutin-based rescue therapy for Helicobacter pylori eradication: A long-term prospective study in a large cohort of difficult-to-treat patients. J. Clin. Med. 2019, 8, 199. [Google Scholar] [CrossRef]
- Azuma, T.; Konishi, J.; Tanaka, Y.; Hirai, M.; Ito, S.; Kato, T.; Kohli, Y. Contribution of HLA-DQA gene to host’s response against Helicobacter pylori. Lancet 1994, 343, 542–543. [Google Scholar] [CrossRef]
- Goldfeld, A.E.; Delgado, J.C.; Thim, S.; Bozon, M.V.; Uglialoro, A.M.; Turbay, D.; Cohen, C.; Yunis, E.J. Association of an HLA-DQ allele with clinical tuberculosis. JAMA 1998, 279, 226–228. [Google Scholar] [CrossRef]
- Drzymała-Czyż, S.; Kwiecień, J.; Pogorzelski, A.; Rachel, M.; Banasiewicz, T.; Pławski, A.; Szczawińska-Popłonyk, A.; Herzig, K.H.; Walkowiak, J. Prevalence of Helicobacter pylori infection in patients with cystic fibrosis. J. Cyst. Fibros. 2013, 12, 761–765. [Google Scholar] [CrossRef][Green Version]
- Yahav, J.; Samra, Z.; Blau, H.; Dinari, G.; Chodick, G.; Shmuely, H. Helicobacter pylori and Clostridium difficile in cystic fibrosis patients. Dig. Dis. Sci. 2006, 51, 2274–2279. [Google Scholar] [CrossRef]
- Israel, N.R.; Khanna, B.; Cutler, A.; Perry, M.; Caplan, D.; Weatherly, M.; Gold, B.D. Seroprevalence of Helicobacter pylori infection in cystic fibrosis and its cross-reactivity with anti-pseudomonas antibodies. J. Pediatr. Gastroenterol. Nutr. 2000, 30, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Wen, G.; Deng, S.; Song, W.; Jin, H.; Xu, J.; Liu, X.; Xie, R.; Song, P.; Tuo, B. Helicobacter pylori infection downregulates duodenal CFTR and SLC26A6 expressions through TGFβ signaling pathway. BMC Microbiol. 2018, 18, 87. [Google Scholar] [CrossRef]
- Vahid, B.; Spodik, M.; Braun, K.N.; Ghazi, L.J.; Esmaili, A. Sarcoidosis of gastrointestinal tract: A rare disease. Dig. Dis. Sci. 2007, 52, 3316–3320. [Google Scholar] [CrossRef] [PubMed]
- Iannuzzi, M.C.; Rybicki, B.A.; Teirstein, A.S. Sarcoidosis. N. Engl. J. Med. 2007, 357, 2153–2165. [Google Scholar] [CrossRef] [PubMed]
- Herndon, B.L.; Vlach, V.; Dew, M.; Willsie, S.K. Helicobacter pylori-related immunoglobulins in sarcoidosis. J. Investig. Med. 2004, 52, 137–143. [Google Scholar] [CrossRef]
- Koyama, S.; Nagashima, F. Idiopathic granulomatous gastritis with multiple aphthoid ulcers. Intern. Med. 2003, 42, 691–695. [Google Scholar] [CrossRef]
- Pope, J.B.; Danford, J.R. Symptomatic gastric sarcoidosis and Helicobacter pylori infection. J. Am. Board Fam. Pract. 1996, 9, 451–454. [Google Scholar]
- Hill, B.A. The environment and disease: Association or causation. Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef]
- Hooi, J.K.Y.; Lai, W.Y.; Ng, W.K.; Suen, M.M.Y.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.S.; Wu, J.C.Y.; et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017, 153, 420–429. [Google Scholar] [CrossRef]
- Halbert, R.J.; Natoli, J.L.; Gano, A.; Badamgarav, E.; Buist, A.S.; Mannino, D.M. Global burden of COPD: Systematic review and meta-analysis. Eur. Respir. J. 2006, 28, 523–532. [Google Scholar] [CrossRef] [PubMed]
- De Groot, P.; Munden, R.F. Lung cancer epidemiology, risk factors, and prevention. Radiol. Clin. N. Am. 2012, 50, 863–876. [Google Scholar] [CrossRef] [PubMed]
- Isaeva, G.; Isaeva, R. Molecular methods for the detection of Helicobacter pylori. Minerva Biotecnol. 2020, 32, 182–187. [Google Scholar] [CrossRef]
- Chey, W.D.; Wong, B.C.; Practice Parameters Committee of the American College of Gastroenterology. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am. J. Gastroenterol. 2007, 102, 1808–1825. [Google Scholar] [CrossRef]
- Ribaldone, D.G.; Fagoonee, S.; Hickman, I.; Altruda, F.; Saracco, G.M.; Pellicano, R. Helicobacter pylori infection and ischemic heart disease: Could experimental data lead to clinical studies? Minerva Cardioangiol. 2016, 64, 686–696. [Google Scholar]
- Kienesberger, S.; Cox, L.M.; Livanos, A.; Zhang, X.S.; Chung, J.; Perez-Perez, G.I.; Gorkiewicz, G.; Zechner, E.L.; Blaser, M.J. Gastric Helicobacter pylori infection affects local and distant microbial populations and host responses. Cell Rep. 2016, 14, 1395–1407. [Google Scholar] [CrossRef]
- Malfertheiner, M.V.; Kandulski, A.; Schreiber, J.; Malfertheiner, P. Helicobacter pylori infection and the respiratory system: A systematic review of the literature. Digestion 2011, 84, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Chmiela, M.; Gonciarz, W. Molecular mimicry in Helicobacter pylori infections. World J. Gastroenterol. 2017, 23, 3964–3977. [Google Scholar] [CrossRef]
- Testerman, T.L.; Morris, J. Beyond the stomach: An updated view of Helicobacter pylori pathogenesis, diagnosis, and treatment. World J. Gastroenterol. 2014, 20, 12781–12808. [Google Scholar] [CrossRef]
- Negrini, R.; Lisato, L.; Zanella, I.; Cavazzini, L.; Gullini, S.; Villanacci, V.; Poiesi, C.; Albertini, A.; Ghielmi, S. Helicobacter pylori infection induces antibodies cross-reacting with human gastric mucosa. Gastroenterology 1991, 101, 437–445. [Google Scholar] [CrossRef]
- Santacroce, L.; Charitos, I.A.; Ballini, A.; Inchingolo, F.; Luperto, P.; De Nitto, E.; Topi, S. The human respiratory system and its microbiome at a glimpse. Biology 2020, 9, 318. [Google Scholar] [CrossRef] [PubMed]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of Pubmed, Scopus, Web of Science, and Google Scholar: Strengths and weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durazzo, M.; Adriani, A.; Fagoonee, S.; Saracco, G.M.; Pellicano, R. Helicobacter pylori and Respiratory Diseases: 2021 Update. Microorganisms 2021, 9, 2033. https://doi.org/10.3390/microorganisms9102033
Durazzo M, Adriani A, Fagoonee S, Saracco GM, Pellicano R. Helicobacter pylori and Respiratory Diseases: 2021 Update. Microorganisms. 2021; 9(10):2033. https://doi.org/10.3390/microorganisms9102033
Chicago/Turabian StyleDurazzo, Marilena, Alessandro Adriani, Sharmila Fagoonee, Giorgio Maria Saracco, and Rinaldo Pellicano. 2021. "Helicobacter pylori and Respiratory Diseases: 2021 Update" Microorganisms 9, no. 10: 2033. https://doi.org/10.3390/microorganisms9102033
APA StyleDurazzo, M., Adriani, A., Fagoonee, S., Saracco, G. M., & Pellicano, R. (2021). Helicobacter pylori and Respiratory Diseases: 2021 Update. Microorganisms, 9(10), 2033. https://doi.org/10.3390/microorganisms9102033









