Abstract
Antibiotic resistance is one of the biggest challenges for the clinical sector and industry, environment and societal development. One of the most important pathogens responsible for severe nosocomial infections is Acinetobacter baumannii, a Gram-negative bacterium from the Moraxellaceae family, due to its various resistance mechanisms, such as the β-lactamases production, efflux pumps, decreased membrane permeability and altered target site of the antibiotic. The enormous adaptive capacity of A. baumannii and the acquisition and transfer of antibiotic resistance determinants contribute to the ineffectiveness of most current therapeutic strategies, including last-line or combined antibiotic therapy. In this review, we will present an update of the antibiotic resistance profiles and underlying mechanisms in A. baumannii and the current progress in developing innovative strategies for combating multidrug-resistant A. baumannii (MDRAB) infections.
1. Introduction
The global spread of antimicrobial resistance (AMR) is one of the global challenges of the 21st century. It is estimated that by 2050, infections caused by resistant strains will lead to 300 million deaths prematurely [1]. Bacterial strains can be naturally resistant to a particular antibiotic or become resistant through the acquisition of resistance determinants [2]. Although there are multiple causes of the resistance phenomenon, it is considered that AMR is an old phenomenon, with an accelerated evolution triggered by the abusive use of antibiotics [3]. Given the extreme mobility of antibiotic resistance genes (ARGs) and their boundaryless dissemination from humans to animals/clinical to environmental reservoirs and vice versa, reducing threats is a difficult task to achieve.
In recent years, the resistance phenomenon was encountered in most common bacterial strains causing infections, associated with an increased risk of morbidity, mortality, high treatment costs and long periods of hospitalization. One of the ESKCAPE pathogens responsible for nosocomial and community-acquired infections is Acinetobacter baumannii, a Gram-negative, non-motile, non-fermentative and non-sporulated bacterium from the Moraxellaceae family [4]. A. baumannii is part of the A. baumannii–A. calcoaceticus complex (Acb), initially including four species: A. calcoaceticus, A. baumannii, A. nosocomialis and A. pittii [5]. Subsequently, several other species have been proposed for inclusion in this complex: A. seifertii [6], A. lactucae [7] and Acinetobacter species “between 1 and 3”. Species between “1 and 3” are phenotypically identical and highly similar genotypically, thus sensitive tests are needed to differentiate them [8]. The Acb complex has become one of the biggest challenges in hospitals, primarily due to its increased resistance to carbapenems and other antibiotics, with minimal treatment options. Risk factors for colonization and infection with species within the Acb complex are extended periods of hospitalization, admission to ICUs, mechanical ventilation or exposure to antimicrobial agents [9]. Of all the species in the Acb complex, A. baumannii is the most widespread in hospitals. Two of the many reasons for the success of MDRAB strains are the association with chronic nosocomial infections and their unique ability to survive in extreme environmental conditions. Its reputation is mainly due to its association with severe infections caused to the US military during the wars in Afghanistan and Iraq, which is why it has been called “Iraqibacter” [10]. A. baumannii causes various infections, including pneumonia, urinary tract infections, skin and soft tissue infections or nosocomial meningitis [11]. Due to its extended resistome and virolome, evasion of the host’s immune effectors, ability to grow in biofilms, to survive in extreme environmental conditions, and to switch to latent growth forms with a minimal metabolic rate, the treatment options are limited, rendering A. baumannii one of the most critical and fearful pathogens [12,13]. In this review, we will present the antibiotic resistance profiles of A. baumannii strains, the main mechanisms (enzymatic and non-enzymatic) of antibiotic resistance (AR), as well as an update regarding the perspectives of new therapeutic strategies efficient against MDRAB. In addition, the discussion section will present the main challenges of therapeutic strategies and the need for further studies in response to existing limitations.
2. AR Profiles of A. baumannii Strains
Studies over the past 20 years have shown that A. baumannii has globally emerged as a highly troublesome nosocomial pathogen revealing multidrug resistance (MDR), extensively drug–resistant and pandrug-resistant phenotypes. Several studies revealed the involvement of aminoglycoside resistance genes, methyltransferases [14] and class 2 β-lactamases in the genesis of the MDR phenotypes [15]. Analysis of AR of several A. baumannii isolates collected from different intensive care units revealed high resistance to the most commonly used antibiotics [16,17]. Several studies reported high carbapenem, aminoglycoside and colistin resistance of A. baumannii strains [18,19,20,21,22,23,24,25,26,27,28,29,30,31] (Table 1). The carbapenem resistance was associated with the overexpression of OXA-51 [32] and OXA-23 [33,34] class D carbapenemases as well as of metallo-β-lactamases (MBLs) [35]. The OXA-51 and OXA-40 class D β-lactamases (CHLD) were involved in ceftazidime resistance [36,37]. Several studies revealed the association of the blaOXA-23 gene with the compound transposon Tn2006 [38] and with the insertion sequence ISAba1 located upstream of the blaOXA-23- gene that increases the carbapenem resistance expression level [39,40].

Table 1.
Antibiotic resistance (AR) profiles of A. baumannii *.
Many studies highlight the involvement with a very high frequency of resistant A. baumannii strains in different types of infections and the need to monitor the antibiotic consumption. The enormous adaptability of resistant strains, supported by the acquisition and dissemination of resistance and virulence markers, is a global problem that requires an imperative understanding of bacterial resistance mechanisms.
3. Short Characterization of the Molecular Mechanisms of AR
Resistance to antibiotics is not a recent phenomenon. Since 1942, shortly after discovering and using penicillin to fight bacterial infections, several strains of Staphylococcus spp. with different AR levels have been reported [45]. The introduction of a high number of new antibiotics and the implicit high level of antibiotic consumption globally has led to the development of numerous bacterial mechanisms to inactivate the action of antibiotics. The abusive consumption of antibiotics in the last 30 years has determined a selective pressure favorable for the spread of the resistance phenomenon. Currently, treating bacterial infections requires increasing doses of antibiotics and prolonged hospitalization [46]. Bacterial resistance is a natural result of the interaction of microorganisms with the environmental niche. Over time, bacteria have developed an arsenal of mechanisms to ensure their survival in a hostile environment. Thus, it is considered that bacterial strains resistant to one or more antimicrobial compounds have an intrinsic resistance (IR), mediated by the resistance determinants [47]. Generally, IR is based on the production of the enzymes that can eliminate the antimicrobial compound or prevent its intracellular binding to the target site. This ability of bacteria is characterized by maintaining a level of resistance to the antimicrobial compound, even in the absence of the previous contact [48].
Bacteria use two genetic mechanisms of defense against antibiotics: mutations, which usually interfere with the mechanism of action of the compound and the acquisition of exogenous genetic material, through horizontal gene transfer (HGT) [49]. Regarding the acquisition of exogenous material, bacteria can acquire and disseminate genes with an essential role in the spread of AR, through mobile genetic elements (MGE) [47]. The main mechanisms of AR are enzymatic (β-lactamases production) and non-enzymatic (alteration of membrane permeability, activation of efflux pumps and alteration of the target site).
3.1. Enzymatic Mechanisms
β-lactamases
β-Lactamases are versatile enzymes revealed by bacteria from different sources with a limited range of molecular structures. The characteristic feature of these enzymes is the ability to hydrolyze chemical compounds with a β-lactam ring, thus inactivating the antibacterial compound [47]. Although first described by Abraham and Chain in 1940 [50], molecular phylogenetic analyses suggest that β-lactamases are ancestral enzymes dating back about two billion years [51]. In contrast, plasmids encoding β-lactamases appeared millions of years ago [52]. β-Lactams antibiotics act by acetylating a serine site in the structure of penicillin-binding proteins (PBPs) [53]. In Gram-positive bacteria, the primary mechanism of β-lactam resistance is the alteration of PBP affinity for these antibiotics, while maintaining physiological functions [54]. The strategy of low-affinity mutant PBP synthesis is a primary mechanism of resistance [55]. In Gram-negative bacteria, β-lactamase synthesis is the main mechanism of resistance to β-lactam antibiotics. The first enzyme with β-lactamase activity was discovered in Bacillus coli by Abraham and Chain in 1940, considered today as the chromosomally encoded cephalosporinase in Escherichia coli. Subsequently, the synthesis of β-lactamases as a mechanism of resistance in Gram-negative bacteria became very common, with the discovery of several chromosomal-encoded inducible enteric β-lactamase-producing bacteria [56]. The prevalence of β-lactamase synthesis in Gram-negative bacteria has been favored by the occurrence of transferable plasmids encoding a wide range of enzymes involved in the spread of β-lactam resistance. β-lactamases were classified based on molecular [57] and functional [58,59] structure analysis. Ambler grouped the β-lactamases into four classes (A, B, C and D), depending on the amino acid sequences. For classes A, C and D, the active enzyme site contains serine and class B includes Zn-dependent metallo-enzymes [57]. In the functional classification of Bush, Jacoby and Medeiros, β-lactamases are divided into three groups, depending on the degraded β-lactam substrate and the effects of inhibitors. The first group includes class C cephalosporinases from the molecular structure classification. The second group comprises β-lactamases other than those from the first group, which have serine at the active site. The third group includes MBLs corresponding to class B of Ambler’s classification. All four β-lactamases Ambler classes have been identified in A. baumannii strains.
Class A β-lactamases are the most frequent cause of β-lactam resistance [60]. These enzymes are inhibited by clavulanate and can hydrolyze penicillins and cephalosporins more efficiently than carbapenems [61]. Phenotypic and biochemical analyses have led to the identification of several functional groups of class A β-lactamases, currently known over 2000, mostly identified in Gram-negative bacilli [62]. Functional types of class A β-lactamases have different molecular variants that demonstrate their ability to hydrolyze cephalosporins and carbapenems [62,63]. In A. baumannii, many class A β-lactamases such as TEM, GES, CTX-M, SHV, SCO, PER, CARB, VEB or KPC were found (Table 2). Of these, most are broad-spectrum β-lactamases (ESBL) (SHV-5, PER-1, PER-2, PER-7, TEM-92, CTX-M-15, VEB-1, GES-14, CARB -10, CTX-M-2) and some are narrow-spectrum (TEM-1, SCO-1).
In contrast to class A enzymes in which the enzyme active site contains serine, class B β-lactamases or MBLs have Zn or another heavy metal in the catalytic site [64]. MBLs are part of the third group of functional classification developed by Bush and Jacoby and have the ability to hydrolyze almost all β-lactam antibiotics except monobactams [61]. Because of the metal from the active enzyme site, the enzymatic activity of these types of β-lactamases can be inhibited by chelating agents such as ethylenediaminetetraacetic acid (EDTA) [65]. There have been reported several MBLs, such as imipenemases (IMPs) [66], Verona integron-encoded MBL (VIM) [67], Sao Paolo MBL (SPM) [68], imipenemase from Germany (GIM) [69], MBL from New Delhi (NDM) [70], Seoul imipenemase (SIM), Australian imipenemase (AIM) and imipenemase from Florence (FIM) [71]. In A. baumannii, a wide range of MBLs has been identified (Table 2).
Class C β-lactamases are encoded by the ampC gene found in Enterobacteriaceae and functionally is a non-inducible cephalosporinase framed by Bush and Jacoby into group 1 [72,73,74]. These β-lactamases may confer resistance to cephamycins, penicillins or cephalosporins [61]. Investigation of 105 MDRAB strains from China demonstrated the presence of the blaampC gene in 65 strains [75]. An analysis of 23 A. baumannii strains from Taiwan revealed the presence of ampC-type β-lactamases in all strains [76].
Class D β-lactamases or CHLD also called oxacillinases (OXA) due to their ability to hydrolyze oxacillin, have serine in the active catalytic site and are included in functional group two of the Bush and Jacoby classification [59]. Over 400 OXA enzymes have been characterized, mostly having the ability to hydrolyze carbapenems. In A. baumannii, the presence of OXA-type β-lactamases which hydrolyze carbapenems is one of the significant mechanisms of resistance [77,78]. OXA enzymes such as OXA-23, OXA-24/40, OXA-58, OXA-143 and OXA-235 are among the most prevalent in A. baumannii strains (Table 2). OXA-23 was identified in Scotland [79], later disseminated globally, now reaching a high frequency in A. baumannii isolates [38,80,81,82]. Genes encoding OXA-type β-lactamases have been identified mainly chromosomally or plasmid located in A. baumannii strains [83,84].

Table 2.
Main β–lactamases in A. baumannii strains.
Table 2.
Main β–lactamases in A. baumannii strains.
| Class/Group | Enzyme | Location | References |
|---|---|---|---|
| Class A β-lactamases | CTX-M (-2, -15, -43) | C, P a | [85,86,87,88,89,90,91] |
| TEM (-1, -92, -116) | P | [92,93,94,95,96,97,98] | |
| GES (-1, -5, -11, -14, -15) | P | [99,100,101,102] | |
| PER (-1, -2, -3, -7) | C, P | [103,104,105,106] | |
| VEB (-1, -3, -7) | C | [104,107] | |
| KPC (-2, -3, -10) | – | [108,109,110] | |
| SCO-1 | P | [111] | |
| CARB (-4, -10) | C, P | [112,113] | |
| SHV (-5, -12) | C | [114,115] | |
| Class B β-lactamases | IMP (-1, -2, -4, -5, -6, -8, -10, -11, -14, -19, -24) | I | [116,117,118,119,120,121,122,123,124] |
| VIM (-1, -2, -3, -4, -6, -11) | I | [121,125,126] | |
| NDM (-1, -2, -3) | C, P | [127,128,129,130] | |
| SIM-1 | I | [131] | |
| SPM-1 | P | [68] | |
| GIM-1 | I, P | [69] | |
| FIM-1 | C | [71] | |
| Class C β-lactamases | AmpC | C | [132,133,134] |
| Class D β-lactamases | OXA-23-like (-23, -27, -49, -73, -102, -103, -105, -133, -134, -146, -165- OXA-171, -225, -239) | C, P | [35,135,136,137,138] |
| OXA-40/24-like (-40, -25, -26, -72, -139, -160, -207) | C, P | [138,139,140] | |
| OXA-51-like (-51, OXA-64– OXA-71, OXA-75– OXA-80, OXA-82- OXA-84, OXA-86– OXA-95, OXA-98– OXA-100, -104, OXA-106– OXA-113, OXA-115– OXA-117, OXA-120– OXA-128, OXA-130– OXA-132, -138, -144, OXA-148– OXA-150, OXA-172– OXA-180, OXA-194– OXA-197, OXA-200– OXA-203, -206, -208, -216, -217, -219, -223, -241, -242, OXA-248– OXA-250, -254) | C, P | [32,141,142,143,144,145,146] | |
| OXA-58-like (-58, -96, -97, -164) | C, P | [122,147,148,149] | |
| OXA-143-like (-143, -182, -231, -253, -255 | P | [150,151,152,153] | |
| OXA-48-like (-48, -48b, -162, -163, -181, -199, -204, -232, -244, -245, -247). | C, P | [154,155,156,157,158] | |
| OXA-235 | C, P | [159] |
a C—chromosomally; P—plasmid; I—integron; “–”—unknown.
Aminoglycosides (AGs) are among the most important antibiotic classes used to treat nosocomial infections caused by A. baumannii strains [160]. Enzymatic modification of AGs through production of aminoglycoside-modifying enzymes (AMEs) is the main mechanism of resistance in A. baumannii. Depending on the mechanism by which it acts, AMEs are classified into acetyltransferases, phosphotransferases and nucleotidyl transferases [161,162]. The main AMEs involved in AGR in A. baumannii are aac (3′)-I, aph (3′)-I, aph (3′)-VI, aac (6′)-Ib, ant (2″)-Ia, ant (3′)–I, aac(3)-Ia [aacC1], aac(3)-IIa [aacC2], aac(6′)-Ib [aacA4], aac(6′)-Ih, aac(6′)-Im, aph(3′)-Ia [aphA1], aph(3′)-VIa [aphA6], ant(3″)Ia [aadA1] and ant(2″)-Ia [aadB], aac(6′)-I ad, aac(6′)-II and ant(4′)-I [163,164,165,166,167,168,169,170,171,172,173]. Genes encoding AMEs can be transferred as part of gene cassettes in the case of integrons, as well as through conjugation mechanisms [174]. Other resistance mechanisms are 16S ribosomal methylases [175,176]. Methyltransferases produce changes at A1408 and G1405 of the small 16S ribosomal unit, which are considered essential for the interaction of the antibiotic with the ribosome and lead to AR [177].
3.2. Non-Enzymatic Mechanisms
3.2.1. Activation of the Efflux Pumps
A. baumannii efflux systems are encoded by chromosomal genes responsible for resistance to several antimicrobial agents in case of overexpression [178]. Genes encoding the efflux mechanisms of specific agents are usually found in MGEs (transposons, integrons, plasmids), their acquisition from other organisms contributing to resistance. MDR efflux systems are generally encoded by chromosomal genes that are expressed constitutively, contributing to IR or expressed following mutation and leading to acquired resistance [179,180].
In A. baumannii, four categories of efflux pumps were identified: RND superfamily (resistance–nodulation–division superfamily), MATE (multidrug and toxic compound extrusion family), MFS (major facilitator superfamily) and SMR (small multidrug resistance transporters) [77]. Of the four efflux systems, the RND system is more represented in A. baumannii, which includes the AdeABC pump, with an essential role in resistance to antimicrobial agents, especially aminoglycosides. The AdeABC pump consists of three components: the inner membrane of the pump (AdeA), the major AdeB fusion protein and the outer membrane factor (AdeC) [181]. AdeABC is encoded by the adeRS operon, whose expression occurs when the efflux pump is exposed to an excessive concentration of toxic agents or antibiotics, leading to an MDR phenotype [182]. Overexpression of the adeABC efflux system is caused either by insertion of the ISAba1 element upstream of the adeABC operon or by punctiform mutations in the adeR and adeS genes [183]. Point mutations in the adeRS operon regulate AdeABC activity, causing resistance to several antibiotics such as aminoglycosides, β-lactams, fluoroquinolones, tetracyclines, macrolides and chloramphenicol [175,184]. The adeRS operon is also involved in A. baumannii biofilm formation. Inactivation of the adeRS operon inhibits the biofilm formation due to decreased expression of the AdeABC efflux pump [185]. The RND family also includes the AdeFGH and AdeIJK efflux pumps, which are associated with tigecycline resistance [183] and the transcriptional regulators AdeL and AdeN control their expression [186,187].
Another category of efflux pumps encountered in A. baumannii is MATE. This family includes the AbeM efflux pump, characterized by Su et al. They reported the involvement of AbeM, along with other efflux pumps, in resistance to norfloxacin, ofloxacin, ciprofloxacin, gentamicin, doxorubicin, triclosan and imipenem [188,189,190].
The MFS superfamily plays an essential role in the resistance of A. baumannii to different antibiotics. CraA is an efflux pump involved in the intrinsic chloramphenicol resistance of A. baumannii strains [191]. Ribbera and colleagues reported the involvement of tet(A) gene in the tetracycline resistance [192]. Recently, Foong and colleagues have shown that overexpression of tet(A) and tet(G) genes confers resistance to doxycycline, minocycline and tetracycline. It has also been observed that tet(A) acts additively with efflux pumps in the RND system, acting as a determinant of tigecycline resistance. Tet(A) gene is involved in the efflux of tigecycline into the periplasm, being subsequently eliminated by the AdeABC and AdeIJK pumps from the outer membrane. The synergistic mechanism of tet(A) gene with pumps from the RND family has an important role in the efflux of tigecycline in A. baumannii [193]. Other examples of efflux pumps from the MFS family are AmvA, which confers resistance to different classes of antibiotics, disinfectants and dyes [194] and AbaF, which is associated with fosfomycin resistance [195]. Recently, Perez-Varela and collaborators identified a new efflux pump from the MFS family, later called AbaQ, with role in virulence. Subsequent analyses have shown that AbaQ is the first pump in the MFS family involved in the outflow of quinolone-type antibiotics [196].
SMR is another efflux pump category described in A. baumannii, which includes AbeS, an efflux pump whose role was initially characterized by Srinivasan and coworkers, reporting its involvement in resistance to a several antibiotics and dyes, and subsequently, by Lytvynenko and colleagues, who analyzed the molecular basis of the multiple specificities of AbeS [197,198].
3.2.2. Decreased Membrane Permeability
Decreasing the degree of membrane permeability may increase the AR. The pores of the outer membrane have an essential role in the resistance and virulence of A. baumannii strains, by mediating the transport of the molecules [199]. In A. baumannii, decreased membrane porin density (Omp22–23, Omp43, Omp44, Omp47, Omp33–36, Omp37 and CarO) is associated with increased carbapenem resistance [200,201,202,203,204,205,206,207,208,209]. Another described membrane porin involved in the pathogenesis of A. baumannii strains is OmpA. Smani and colleagues reported the association of this porin with aztreonam, chloramphenicol and nalidixic acid resistance [210] and recent studies have highlighted the role of OmpA in increasing the virulence [211], in lung infections, sepsis—and increased the mortality [212,213].
3.2.3. Changing the Target Site
Alteration of the target site of the antibiotic is an essential mechanism of bacterial resistance. In general, this mechanism is based on random point mutations that have a minimal impact on bacterial cell homeostasis. Mutations can occur in any species and have recently been shown in H. pylori and S. aureus strains. The 23S ribosomal RNA mutations in H. pylori cause resistance to clarithromycin [214]. Studies have shown that point mutations in the same nucleotide sequence are associated with increased linezolid resistance [215]. Given the reports on the expansion of the resistance phenomenon, including against last-line antibiotics, we will only present the mutation-mediated resistance mechanisms of A. baumannii strains to the most common antibiotic classes used in the treatment of the infections.
One of the most discussed examples through point mutations is rifampin resistance (RIF). Rifampin blocks RNA polymerase activity. The region to which rifampin binds is a highly conserved enzymatic structure in the β subunit of RNA polymerase encoded by the rpoB gene. After the attachment to the binding site, the antibiotic molecule blocks the transcription by inhibiting nascent RNA [216]. It has been observed that increased resistance to rifampin is associated with the occurrence of point mutations in the rpoB gene, which result in various changes in the amino acid chain [217]. In A. baumannii, rifampin resistance can also be mediated by the arr-2 gene encoding an ADP-ribosyltransferase, found within class 1 integrons.
Another example induced by point mutations is fluoroquinolones resistance. Fluoroquinolones act by inhibiting the DNA gyrase and topoisomerase IV enzymes encoded by gyrA and parC genes. In A. baumannii, the most common fluoroquinolone resistance mechanism is represented by the spontaneous mutations in the gyrA, gyrB and parC genes encoding gyrase and topoisomerase IV. The investigation of 56 A. baumannii strains harvested from 23 hospitals showed a strong association of fluoroquinolone resistance with triple mutations in the gyrA, gyrB and parC genes [218]. Ardebili et al. demonstrated the correlation of fluoroquinolones resistance with mutations in the DNA gyrase and topoisomerase IV encoding genes, after analyzing 55 isolates of A. baumannii [219], and more recently, in case of 23 strains investigated in Cairo [220]. Some clinical studies have shown that single parC or gyr mutations often lead to reduced susceptibility to fluoroquinolones, but without full resistance. In addition, additional target mutations will generate full clinical resistance, with high MICs breakpoints [221,222]. Other resistance mutations occur in regulatory genes that control the expression of outer membrane proteins and efflux pumps [221].
Fluoroquinolone resistance is also mediated by plasmid-mediated quinolone-resistance genes (PMQR), either through the QNR protein, a pentapeptide that protects target enzymes from antibiotic action [223] or through an aminoglycoside-modifying mutant enzyme [224].
Extensive use of colistin as last-resort treatment led to the development of colistin resistance. Regarding the colistin action, it is believed that colisting binding to lipopolysaccharides (LPS) in the outer membrane of Gram-negative bacteria causes changes in the structure of the phospholipid bilayer that leads to cell death by installing an osmotic imbalance [225]. Despite that, in 1970, it was replaced with other antibiotics due to side effects such as nephrotoxicity and neurotoxicity [226]. However, the severity of nosocomial infections forced the use of colistin as last-resort treatment [227]. Consequently, the extensive use of colistin caused the emergence of resistance, first observed in 1999 in the Czech Republic [228] and later globally. In A. baumannii, two mechanisms of colistin resistance have been described: i) modification of the lipid A from LPS by mutations in the PmrAB two-component system and ii) loss of LPS production capacity due to mutations in the lpxA, lpxC and lpxD genes. In 2009, Adams et al. analyzed the sequences of PmrAB components in A. baumannii-susceptible and resistant strains. They found mutations in the pmrA and pmrB genes in the case of resistant strains [229]. This finding led to the idea of the role of PmrAB component in regulating the colistin susceptibility of A. baumannii, by regulating the NaxD deacetylase transcription and the modification of lipid A by β-galactosamine deacetylase [230]. Mutational inactivation of the lpxA, lpxC and lpxD genes, which are involved in the LPS biosynthesis, results in the loss of antibacterial activity of colistin.
All these complex resistance mechanisms highlight the imperative need to analyze the AMR in A. baumannii, in order to respond to current challenges by developing innovative, practical therapeutic approaches.
4. Innovative Strategies for Treatment of A. baumannii Infections
Studies conducted in recent years highlight the unique involvement of A. baumannii strains in increasing the severity of nosocomial infections and, implicitly, their associated morbidity and mortality rates. Analysis of the resistance profiles of A. baumannii strains reveals the spread of the MDR phenomenon to most common antibiotics, including last-line ones [21,25]. As an alternative to this phenomenon, studies have initially focused on the approach of combined therapies such as minocycline/tigecycline [231,232], colistin/tigecycline [233], colistin/rifampin [234], polymyxin B-combined therapy [235]. All of these alternatives have only limited effects in case of nosocomial infection treatment, inevitably leading to a selective pressure that increases the resistance level of bacterial strains. Therefore, in the long run, combined antibiotic therapy may not be feasible in clinical settings. Given that A. baumannii strains are resistant to almost all antibiotics used [229], the research direction must be in line with the “post-antibiotic era”, emphasizing the development of innovative strategies to control MDRAB spreading. Next, we will present the most innovative therapies, such as new antimicrobial peptides, phage therapy, and CRISPR Cas system (Clustered regularly interspaced short palindromic repeats) developed to prevent the spread of MDRAB strains.
4.1. Antimicrobial Peptides (AMP)
Antimicrobial peptides may represent an alternative to antibiotics in the control of MDRAB strains spread. AMP is a class of compounds widespread in the living world as part of the innate immunity, acting as a primary barrier against infectious agents such as viruses, bacteria and fungi [236,237]. AMPs also play an essential role in regulating immune processes such as activating and recruiting immune system cells, angiogenesis and inflammation [238]. AMPs are amphipathic molecules with a positive electric charge, having a length of about 11–50 amino acid residues [238,239]. The main mechanisms of antimicrobial action of AMPs are the ability to cause cell membrane and cell wall damage, the inhibition of protein synthesis, nucleic acids and the induction of apoptosis and necrosis [240]. Due to these properties, AMPs have been considered an alternative to the use of antibiotics for limiting the spread and decreasing the infection rate and mortality control measures of nosocomial infections.
Cathelicidins are a group of AMPs detected in the immune system of some vertebrates that have in their structure two domains involved in antimicrobial activity [241]. One of the best-known cathelicidins is Cath-BF, isolated from the venous glands of the species Bungatus fasciatus. Starting from Cath-BF, several derived forms, such as ZY4 and Cath A, have been obtained and tested for antimicrobial activity. Other cathelicidins with antimicrobial activity, identified in the venous glands, are OH-CATH30, from the venom of king cobra and myrtoxin, from Myrmecia pilosula [242,243]. In vitro and in vivo studies have revealed the antimicrobial activity of these compounds, manifested by inhibition of planktonic and biofilm bacterial growth, eradication of persistent bacterial cells and inhibition of the inflammatory process [242,244,245]. However, despite the proven antimicrobial activity, further studies are needed to obtain information about expression sites and the influence of these peptides on microbial and host cells [241]. Compounds with similar activity have been identified in the venom of some scorpion species and tested against antibiotic-resistant bacteria. In the case of Leiurus quinquestriatus, a broad antimicrobial activity of the tested compounds was observed. However, there is not enough information regarding the interaction of these compounds with specific molecules of some microorganisms [246]. A high antimicrobial activity was observed for AMPs obtained from Vespa affinis (mastoparan) [247], Capra hircus (minibactenecins) [248], Lucilla serricata (sarcotoxin) [249] and from Rana catesbeiana (ranalexin and danalexin) [250]. However, despite the antimicrobial activity on A. baumannii strains of these compounds, further in vivo studies are needed to improve the pharmacokinetic properties for systemic administration, as well as to find solutions to avoid their degradation by proteases. Jakiewicz et al. studied the antimicrobial activity of eight peptides on A. baumannii strains. Among these, CAMEL and pexiganan showed potent antimicrobial and anti-biofilm activity. CAMEL is a hybrid AMP consisting of cecropin from Hyalophora cecropia and melittin from Apis mellifera. This study demonstrates the potential of these compounds to act against resistant strains [251]. Intense activity against biofilms have been observed in cecropins identified in Musca domestica [252], myxinidin isolated from Myxine glutinosa [253] and in the complex of AMPs (Fly larvae immune peptides) from Calliphora vicina [254]. Natural AMPs can be a starting point for the biosynthesis of AMPs with similar functions, being an attractive therapeutic option for the prevention and control of A. baumannii infections. Such examples of synthetic AMP are stapled AMP [255] and PNA (RXR) 4 XB, an antisense nucleic acid peptide compound [256] with intense bactericidal activity. However, the need for high doses to increase efficacy leads to the need for further in vivo studies to observe possible side effects. To be considered for therapy, AMPs must have a broad spectrum of action, high specificity and low cytotoxicity levels to mammalian cells [257]. The primary limitations that hinder the approval of systemic use of AMPs are sensitivity to enzymatic digestion and high toxicity, which is why most AMPs are applied topically and not orally or intravenously [258,259]. It has also been observed that certain physiological conditions, such as high concentrations of salts and serum components, can exert adverse effects on AMPs [260]. Compared to the conventional use of antibiotics, production costs for AMPs are much higher, which is why research is moving towards peptides as short as possible with stable properties [261]. Some studies reveal the appearance of AMPs resistant strains [262], the best-known example being A. baumannii resistance to colistin [21,25]. Currently, research is aimed at developing technologies to improve the efficiency of AMPs in vivo, especially in terms of increasing the specificity against the infectious agents, decreasing cytotoxicity to mammalian cells, increasing stability and lowering production costs. The newest AMPs studied to elucidate their therapeutic efficacy against A. baumannii strains are summarized in Table 3.

Table 3.
Antimicrobial Peptides (AMPs) with antimicrobial activity against A. baumannii.
4.2. Bacteriophages Therapy
Bacteriophages are viral parasites able to infect bacteria by recognizing surface receptors, injecting their genetic material into the host and replicating using the host cellular machinery [281]. Phages exhibit ecological and genetic effects on bacteria at the population level, and these effects can impact plasmid stability [282,283]. Phages may enhance the persistence of ARGs as an adaptation strategy to restrictive environmental conditions, e.g., wastewater aggressively treated using UV, temperature or pH. However, genetically modified phages could be used to increase antibiotic susceptibility of resistant strains. The alarming increase in the resistance rates has also led to the revival of phage therapy to increase the susceptibility level of bacteria by eliminating resistance and virulence markers [284]. Phages do not exert adverse effects on the patient’s microbiome and have a high degree of selectivity and specificity for pathogens [285]. In addition, research has shown that phage therapy has a high potential to represent an effective and safe treatment against MDRAB strains [286,287]. A high number of experiments were performed both in vitro and in vivo, the main results being summarized in Table 4.

Table 4.
Bacteriophages therapy against A. baumannii strains.
Bacteriophage therapy represents a promising tool in fighting MDR A. baumannii strains. Analyzation of the data summarized in Table 4 highlights that both in vitro and in vivo studies demonstrate the high efficiency, increasing the survival rate of organisms infected with A. baumannii strains. Based on the results obtained on animal models in the last ten years, numerous studies have focused on understanding the effectiveness of this therapy against chronic infections in the hospital units, as revealed by different clinical trials [284,301,302,303,304]. Schooley et al. have used phagotherapy in a patient with necrotic pancreatitis caused by an MDRAB strain [305].
Contrary to these studies, there are other reports of the inefficiency of phages in treating bacterial infections [306,307], which suggests that the clinical use of phages requires standardization. One of the most significant challenges in phage therapy is the resistance of bacterial strains to phage action [308,309,310]. In bacterial communities, resistance is a dynamic process when the antibacterial agent is biologic, as is the case with phages. On the other hand, phages exert a selective competition on bacteria. This two-way interaction causes a co-evolution that results in bacteria acquiring resistance mechanisms that can block the cycle of lytic infection [308,309]. Bacteria can acquire resistance to phages following cellular surface changes represented by point mutations in phage binding receptors [311]. Another mechanism of resistance is the outer membrane vesicles to which phages can bind due to surface structures, similar to those of parental cells. Binding of phages to these vesicles during invasion decreases the likelihood of cell infection [308]. In addition, a significant impact has the restriction–modification systems, the most common defense mechanisms in bacteria that can degrade foreign DNA, including double-stranded DNA phages [312]. Another concern in the use of phage therapy is the lack of standardization of phage preparation methods. An incomplete purification of host bacterial phages can lead to an unwanted transfer of bacterial toxins such as endotoxins or exotoxins [313]. Particular attention should be paid to combination therapy with phages and lysins. Once the dose needed to increase antimicrobial action has been determined, the mechanisms of action and elimination from the body must be established [314]. Stimulation by the phage of the immune response and adaptive immune systems, as well as their presence in the bloodstream, may influence the effectiveness of phage therapy [313]. Van Belleghen et al. observed the process of phages’ opsonization by binding to the surface of invasive bacteria that can lead to neutralization of phages by the secondary adaptive immune response. Thus, the recognition of circulating phages can lead to their elimination. In addition, phages can be detected in the systemic circulation by tissue proteases or the reticuloendothelial system and delivered to the liver and spleen where degradation occurs [313].
Further studies are required to understand phage biology clearly and to better control clinical trials to standardize phagotherapy.
4.3. CRISPR System-a New Approach in the “Post-Antibiotic Era”?
As mentioned previously, the current strategies used to combat MDRAB infections have many limitations. In the recent years, one of the most attractive alternatives to combat bacterial resistance is the use of CRISPR (clustered regularly interspaced short palindromic repeat) system described for the first time in 1987, by Ishino et al. [315]. CRISPR/Cas is an immune defense system encountered in bacteria able to recognize and degrade foreign nucleic acids through associated caspases.
One of the most significant advantages of this system is its high specificity, based on the existence of short, repetitive sequences in CRISPR loci separated from each other by single sequences of 26–72 pairs of lengths derived from MGEs such as plasmids or transposons [316]. The defense mechanism against exogenous genetic elements is accomplished in three stages: acquisition, expression and interference [317]. The acquisition stage involves the insertion into repetitive loci of the host chromosome of single sequences (spacers) derived from MGEs, separated by repetitive sequences. The expression consists of transcribing the complex formed of repetitive and spacer sequences into a single RNA transcript that will be further processed by caspases in short CRISPR RNAs. Caspases, including ribonucleases, are a family of protease enzymes, playing essential roles in programmed cell death [318]. In the interference phase, foreign nucleic acids are identified based on complementarity with CRISPR RNAs, and their degradation is accomplished by caspases [319]. Discrimination between self and non-self is accomplished through sequences from the foreign nucleic acid called protospacers. These sequences are placed between some sequence motifs called PAMs (adjacent protospacer motif). Direct target recognition is achieved only by identifying these sequence motifs not stored in CRISPR loci, so there is no risk of degradation of its nucleic acid [320] (Figure 1).
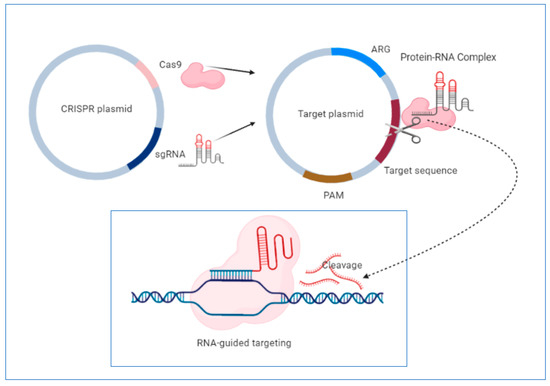
Figure 1.
Schematic representation of clustered regularly interspaced short palindromic repeat (CRISPR)-based targeting of mobile genetic elements (MGEs). This system contains the cas9 nuclease, sgRNA transcript and other structural elements. In the first stage, sgRNA forms a complex with Cas 9 nuclease. The sgRNA transcript guide cas9 nuclease to introduce double-stranded breaks at the ends of the target DNA, leading to cleavage. Direct target recognition is achieved by recognizing protospacer adjacent motifs (PAM), short DNA sequences that are not found in CRISPR loci, so there is no risk of self-degradation. This system can be used to edit the genome of several antibiotic-resistant bacterial strains, leading to the removal of resistance determinants. Figure created with https://biorender.com/.
In A. baumannii, two types of CRISPR systems were identified within MGEs containing different spacer sequences. In addition, the distribution of some analyzed isolates in different clusters was observed, suggesting that this system was acquired by HGT throughout evolution [321,322]. Karah et al. analyzed 76 A. baumannii isolates to study the I-Fb subtype of the CRISPR system. Forty types of CRISPR sequences were revealed, two being found mostly in 35.52% of the analyzed isolates, suggesting the existence of two primary clones. The spacer sequences are arranged in chronological order of their inclusion from the invading nucleic acids so that the old ones are positioned at the end. This temporal positioning of the sequences allows the use of the CRISPR system for the micro- and macroepidemiological classification of clinical isolates [323].
These results have opened new perspectives regarding the possibility of using the CRISPR system for subtyping A. baumannii strains [320,324,325,326,327,328,329,330,331,332]. Wang et al. developed a CRISPR platform that allows rapid genomic editing by introducing deletions, insertions, and point mutations to analyze the mechanisms involved in oxidative stress (OxyR) in A. baumannii strains. For the introduction of deletions, the authors constructed a CRISPR plasmid in which they incorporated the CRISPR elements from Streptococcus pyogenes. To repair double-strand breaks, they used RecA recombinase from A. baumannii. The introduced mutations in the oxyR gene and its deletion, lead to a high susceptibility level of A. baumannii strains to oxidative stress, demonstrating the importance of this gene as a central transcriptional regulator of the response to oxidative stress [333]. Mangas et al., conducted an in silico study to analyze the pan-genome of 2500 A. baumannii strains. Depending on the number of shared genes, the authors observed that genomes are divided into two broad groups. The group of strains with a lower number of genes shows the sequences and genes characteristic of the CRISPR system, genes specific to the toxin–antitoxin system and genes involved in the biofilm formation, which is why it is considered that the CRISPR system may have an essential role in virulence. Unlike the strains from group two, positive for a high number of plasmids, the strains from the first group contain mainly genes involved in regulating the elements of the CRISPR system. This finding led to the idea that the CRISPR system may be involved in the restriction of the plasmid entry into bacterial cells [334]. Karlapudi et al. conducted an in silico study to understand the role of the AbaI gene in biofilm formation in A. baumannii. For this, they used a series of genetic editing tools to create AbaI gene knockouts. The analyzed tools (CHOCHOP, CCTop, E-CRISP, CRISPR Direct, Off-Spotter, Crispr-era) can provide information about the target sequences, specific primers, existing mutations, the location of the target sequence in order to perform the knockout, as well as the necessary sgRNA sequences for performing genomic editing experiments [335]. The information obtained from the in silico genomic experiments demonstrates the need to improve genetic editing tools. In addition, further studies should consider the construction of sgRNA with a custom design, depending on the diversity of cell types.
Despite the notable results obtained from using the CRISPR system to combat antibiotic resistance, however, controlling bacterial populations using this strategy has some limitations. First of all, the appearance of mutations outside the target represents a significant limitation of the CRISPR system. In addition to cleaving target sequences, the CRISPR system can act on identical or homologous DNA sequences, leading to mutations in unwanted sites, called off-target mutations. Mutations outside the target can lead to cell death or transformation, which is why it is recommended to select target sites at which as few mutations can occur outside the target [336].
Another challenge in using the CRISPR system in controlling bacterial populations is the need for PAM sequences that are involved in differentiating between self and non-self. There is a limitation of the number of target sites due to the need for these sequences. Because the CRISPR system requires specific PAM sequences to function, their genetic engineering processing can eliminate this limitation [336].
Another major limitation in using the CRISPR system in the control of bacterial populations is represented by the delivery of the protein–RNA complex through the bacterial membrane. There is the problem of delivering the CRISPR system in the case of both Gram-negative and Gram-positive bacteria. It has been observed that the techniques used to encapsulate the gRNA-protein complex have a significant impact on loading and packaging efficiency, thus limiting their practical use [337,338]. Consequently, studies have focused on the use of phages as a vehicle for the delivery of the CRISPR system at the target level. This strategy involves encapsulating the CRISPR system in the capsid of inert phages [326,327]. Starting from phages as a delivery vehicle of the CRISPR system in vitro, the problem of controlling bacterial populations using the CRISPR system in vivo was raised. Starting from the fact that oral administration of phages for targeting bacteria in the intestinal tract was used successfully [331], one strategy is to use phages as a vehicle for delivering the CRISPR system in the intestinal microbiota, for eliminating the ARGs. However, it is required to have a collection of phages specially designed to target ARGs, to establish the optimal concentration required and to know the several barriers that occur in vivo, such as inactivation of bacteriophages by gastric acid, neutralization of phages by the spleen and the immune system [332].
5. Discussion
The mentioned studies highlighted the particular involvement of A. baumannii strains in different infections types, as well as the need to implement appropriate infection control measures to limit the spread and decrease the infection rate and mortality. Data summarized in Table 1 and Table 2, emphasize that in the great majority of A. baumannii isolates, the primary mechanism of AR is represented by the production of diverse β-lactamases, from all four Ambler classes, both chromosomal and plasmidial. Among these, CHLDs seems to be mostly related to the occurrence of MDR phenotypes in A. baumannii. Although colistin was initially one of the leading antibiotics in the treatment of nosocomial infections caused by A. baumannii, a gradual increase of colistin resistance in clinical isolates, reaching even 100% in some studies has been revealed [19,21,25]. The origin of the clinical isolates demonstrates the wide dissemination of infections, the A. baumannii resistant strains being isolated mostly from tracheal aspirates, tracheal secretions, burn wounds, blood, urine or cerebrospinal fluid (Table 1). In addition, most of the patients were admitted to ICUs, which highlights the severity of infections caused by A. baumannii, which can cause increased morbidity, hospitalization length and costs, as well as mortality.
To date, a significant challenge in the clinic is to develop methods to establish the appropriate MIC values needed to increase treatment efficiency. Most laboratories are not able to determine MIC values accurately and reproducibly enough and to eliminate variations. One cause of variations in MIC values is the existence of several strategies and methods to determine these values. Terwee et al. studied the differences obtained in MIC values following the use of several methods that fall into two general categories: “anchor” methods and distribution-based methods. Anchor methods use an external criterion to establish a significant change (patient opinion), and distribution-based methods use statistical data to determine the MIC value. In the case of applying the two strategies, Terwee et al. observed significant differences in MIC values [339]. These significant differences could be closely related to population characteristics such as age, the severity of the condition and treatment and the method used. In this situation, several factors that contribute to variability make it difficult for clinicians to establish a single MIC value or at least a range of values as small as possible [339].The semiautomatic susceptibility detectors often provide truncated MIC values. The same problem exists with gradient tests, such as the E-test, which may omit a certain percentage of resistant strains, leading to treatment failure in the clinic [340]. Even if the susceptibility tests are performed correctly, variations may occur due to discontinuous results reported at a specific interval, usually at a 2-fold scalar dilution. When variations occur, MIC values may exceed these intervals, leading to incorrect doses of antibiotics, which may be harmful to the patient [341].
For this reason, it is imperative to standardize the methodology for identifying MIC values in microbiology laboratories. The standardization process is essential for prescribing a correct treatment, controlling severe infections, and for stopping the expansion of the resistance phenomenon.
Moreover, the in vitro susceptibility tests used for prescribing a treatment do not provide information about the bacteriostatic or bactericidal activity of an antibiotic [342].
Bacteriostatic activity refers to the inhibition of bacterial growth, and bactericidal activity refers to the killing of bacteria. In reality, there is no particular antibiotic that either inhibit or kill bacteria. In patients with inflammatory and immunocompromised diseases, it is critical to identify the minimum bactericidal concentration (MBC). MBC is the lowest concentration of antibiotic that kills bacteria, reducing bacterial colonies by up to 99% [343]. Whether we are talking about the curing strategy, based on the identification of MIC values or the identification of MBC in order to eradicate bacteria, there are advantages and disadvantages in both treatment strategies. In the case of diseases such as endocarditis [344], meningitis [345], osteomyelitis [346] and neutropenia [347], the use of bactericidal action is recommended. High bacterial concentrations, the presence of dormant bacteria with high resistance, low immune competence of the body and low ability to penetrate the antibiotic are some factors that lead to the need to use agents with bactericidal activity to achieve complete sterilization of the infectious outbreak., The use of bactericidal agents is recommended in some clinical situations, but there are disadvantages to bactericidal action. The rapid action of bactericidal agents can have adverse clinical consequences, such as the discharge of endotoxins following bacterial lysis. Rapid eradication of bacteria can lead to cell wall fragments and pneumolysins, which can exacerbate the immune response, the release of prostaglandins and high mortality rates in meningitis [348]. Therefore, the risk of a significant inflammatory reaction due to bacterial lysis must be considered.
The heterogeneity and increased efficiency of the resistance mechanisms of A. baumannii strains against almost all existing antibiotics threatens with the transition to the “post-antibiotic era”, indicating the acute need to search for new therapeutic approaches. One of the challenges that hinder the success of the treatment of severe infections is the emergence of the phenomenon of heteroresistance. Heteroresistance occurs when subpopulations of isogenic bacteria exhibit lower susceptibility than the general population [349]. In A. baumannii, heteroresistance has been reported in antibiotics such as aminoglycosides, tobramycin, gentamicin and imipenem [350,351], but also in other antimicrobial agents such as AMPs [352]. Currently, the biggest threat is the reporting of colistin heteroresistance, which implies the existence of resistant subpopulations in a susceptible isolate (MIC ≤ 2 mg/L) by in vitro susceptibility tests [353]. In the case of severe nosocomial infections produced by heteroresistant strains in the clinic, colistin treatment may cause resistance expansion and, thus, treatment failure [354]. For detection of the phenomenon of heteroresistance, various methods are used, such as BMD (broth microdilution), E-test or PAP (population analysis profile) [353]. The use of appropriate susceptibility tests to identify heterogeneous subpopulations is essential for the success of clinical treatment. The study by Caglan et al. highlighted differences between the results obtained after the application of BMD and E-test. Using E-test, the resistance to colistin was 4.2%, while by the BMD method, a percentage of 25.8% was obtained, analyzing the same isolates. Therefore, in the case of the E-test, a large part of the resistant strains has not been identified, which is a significant mistake in the clinic [340]. Thus, clinicians should keep in mind that although the use of gradient tests is more comfortable, the results can be confusing and can negatively influence patients’ treatment.
Another problem that clinicians need to consider is the emergence of heteroresistance in patients who do not have a history of colistin treatment. However, it is more common in patients who have received treatment [355]. The emergence of heteroresistance to a range of antibiotics, including last-line antibiotics, significantly impedes the management of severe nosocomial infections caused by MDRAB strains and requires increased clinical attention to identify resistant subpopulations.
6. Conclusions
Different MDR microorganisms, among which A. baumannii are opportunistic pathogens, able to compete in new environments where previously only commensals or non-pathogenic microorganisms existed. The survival and persistence in nosocomial environments characterized by high antimicrobial pressure have led to the emergence of A. baumannii as a key pathogen, whereas a few decades ago, it caused practically no disease. The incidence of MDR and virulent clones of A. baumannii is also increasing worldwide, at least in these specific settings.
One of the clinic’s difficult challenges is establishing the correct MIC values based on which to prescribe a correct treatment. The existence of numerous factors that influence the MIC values such as the lack of standardization of the methodology makes the success of the therapy difficult. Increased attention should be paid to factors that may influence MIC values such as patient characteristics (age, disease severity) and methods applied. In addition, identifying MIC values and MBC values can provide clinicians with additional information about the antibiotics needed to prescribe the most appropriate treatment.
The emergence of heteroresistance in some bacterial subpopulations is another challenge in the management of infections caused by A. baumannii.
The enormous adaptability of A. baumannii, as well as the very diverse mechanisms for the acquisition and transfer of AR determinants, contribute to the inefficiency of most current therapeutic strategies, determining the transition to the “post-antibiotic era” and highlighting the necessity to develop new therapeutic approaches. The latest strategies include obtaining the use of AMPs, bacteriophage therapy and CRISPR technology. Although experiments have shown the potential of these strategies in combating MDRAB, there are several challenges, such as the narrow spectrum of action, low specificity, high cytotoxicity, sensitivity to enzymatic degradation and bacterial resistance. These limitations must be addressed in future studies to develop efficient strategies for the optimal management of MDRAB infections.
Author Contributions
M.C.C. conceived and corrected the manuscript. M.C.C., I.G., I.B.C. and C.O.V. contributed to the literature survey and revised the manuscript. C.O.V. drafted the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The financial support of the Research Projects PN-III-P4-ID-PCCF-2016-0114 and PN-III-P1.1-PD-2016-1798 awarded by UEFISCDI is gratefully acknowledged. The funding had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- O’Neill, J. Tackling Drug-Resistance Infections Globally: Final Report and Recommendations. The Review on Antimicrobial Resistance; Government of the United Kingdom: London, UK, 2016; pp. 1–84. [Google Scholar]
- Monserrat-Martinez, A.; Gambin, Y.; Sierecki, E. Thinking Outside the Bug: Molecular Targets and Strategies to Overcome Antibiotic Resistance. Int. J. Mol. Sci. 2019, 20, 1255. [Google Scholar] [CrossRef] [PubMed]
- Holmes, A.H.; Moore, L.S.P.; Sundsfjord, A.; Steinbakk, M.; Regmi, S.; Karkey, A.; Guerin, P.J.; Piddock, L.J.V. Understanding the Mechanisms and Drivers of Antimicrobial Resistance. Lancet 2016, 387, 176–187. [Google Scholar] [CrossRef]
- Eze, E.C.; Chenia, H.Y.; El Zowalaty, M.E. Acinetobacter Baumannii Biofilms: Effects of Physicochemical Factors, Virulence, Antibiotic Resistance Determinants, Gene Regulation, and Future Antimicrobial Treatments. Infect. Drug Resist. 2018, 11, 2277–2299. [Google Scholar] [CrossRef] [PubMed]
- Nemec, A.; Krizova, L.; Maixnerova, M.; van der Reijden, T.J.K.; Deschaght, P.; Passet, V.; Vaneechoutte, M.; Brisse, S.; Dijkshoorn, L. Genotypic and Phenotypic Characterization of the Acinetobacter Calcoaceticus-Acinetobacter Baumannii Complex with the Proposal of Acinetobacter Pittii Sp. Nov. (Formerly Acinetobacter Genomic Species 3) and Acinetobacter Nosocomialis Sp. Nov. (formerly Acinetobacter genomic species 13TU). Res. Microbiol. 2011, 162, 393–404. [Google Scholar] [CrossRef]
- Nemec, A.; Krizova, L.; Maixnerova, M.; Sedo, O.; Brisse, S.; Higgins, P.G. Acinetobacter Seifertii Sp. Nov., a Member of the Acinetobacter Calcoaceticus-Acinetobacter Baumannii Complex Isolated from Human Clinical Specimens. Int. J. Syst. Evol. Microbiol. 2015, 65, 934–942. [Google Scholar] [CrossRef]
- Cosgaya, C.; Marí-Almirall, M.; Van Assche, A.; Fernández-Orth, D.; Mosqueda, N.; Telli, M.; Huys, G.; Higgins, P.G.; Seifert, H.; Lievens, B.; et al. Acinetobacter Dijkshoorniae Sp. Nov., a Member of the Acinetobacter Calcoaceticus-Acinetobacter Baumannii Complex Mainly Recovered from Clinical Samples in Different Countries. Int. J. Syst. Evol. Microbiol. 2016, 66, 4105–4111. [Google Scholar] [CrossRef]
- Gerner-Smidt, P.; Tjernberg, I. Acinetobacter in Denmark: II. Molecular Studies of the Acinetobacter Calcoaceticus-Acinetobacter Baumannii Complex. APMIS 1993, 101, 826–832. [Google Scholar] [CrossRef]
- Maragakis, L.L.; Perl, T.M. Acinetobacter Baumannii: Epidemiology, Antimicrobial Resistance, and Treatment Options. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2008, 46, 1254–1263. [Google Scholar] [CrossRef]
- Peleg, A.Y.; Seifert, H.; Paterson, D.L. Acinetobacter Baumannii: Emergence of a Successful Pathogen. Clin. Microbiol. Rev. 2008, 21, 538–582. [Google Scholar] [CrossRef]
- Dijkshoorn, L.; Nemec, A.; Seifert, H. An Increasing Threat in Hospitals: Multidrug-Resistant Acinetobacter Baumannii. Nat. Rev. Microbiol. 2007, 5, 939–951. [Google Scholar] [CrossRef]
- Willyard, C. The Drug-Resistant Bacteria That Pose the Greatest Health Threats. Nature 2017, 15. [Google Scholar] [CrossRef] [PubMed]
- Barth, V.C.J.; Rodrigues, B.Á.; Bonatto, G.D.; Gallo, S.W.; Pagnussatti, V.E.; Ferreira, C.A.S.; de Oliveira, S.D. Heterogeneous Persister Cells Formation in Acinetobacter Baumannii. PLoS ONE 2013, 8, e84361. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, S.; Khyriem, A.B.; Bhattacharya, P.; Bhattacharjee, A.; Joshi, S.R. High-Level Aminoglycoside Resistance in Acinetobacter Baumannii Recovered from Intensive Care Unit Patients in Northeastern India. Indian J. Med. Microbiol. 2018, 36, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Kwon, N.Y.; Kim, J.D.; Pai, H.J. The Resistance Mechanisms of B-Lactam Antimicrobials in Clinical Isolates of Acinetobacter Baumannii. Korean J. Intern. Med. 2002, 17, 94–99. [Google Scholar] [CrossRef]
- Maniatis, A.N.; Pournaras, S.; Orkopoulou, S.; Tassios, P.T.; Legakis, N.J. Multiresistant Acinetobacter Baumannii Isolates in Intensive Care Units in Greece. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2003, 9, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Turton, J.F.; Kaufmann, M.E.; Warner, M.; Coelho, J.; Dijkshoorn, L.; van der Reijden, T.; Pitt, T.L. A Prevalent, Multiresistant Clone of Acinetobacter Baumannii in Southeast England. J. Hosp. Infect. 2004, 58, 170–179. [Google Scholar] [CrossRef]
- Yau, W.; Owen, R.J.; Poudyal, A.; Bell, J.M.; Turnidge, J.D.; Yu, H.H.; Nation, R.L.; Li, J. Colistin Hetero-Resistance in Multidrug-Resistant Acinetobacter Baumannii Clinical Isolates from the Western Pacific Region in the SENTRY Antimicrobial Surveillance Programme. J. Infect. 2009, 58, 138–144. [Google Scholar] [CrossRef]
- Rodríguez, C.H.; Nastro, M.; Famiglietti, A. Carbapenemases in Acinetobacter Baumannii. Review of Their Dissemination in Latin America. Rev. Argent. Microbiol. 2018, 50, 327–333. [Google Scholar] [CrossRef]
- Rodríguez, C.H.; Nastro, M.; Fiorilli, G.; Dabos, L.; Lopez Calvo, J.; Fariña, M.E.; Vay, C.; Famiglietti, A. Trends in the Resistance Profiles of Acinetobacter Baumannii Endemic Clones in a University Hospital of Argentina. J. Chemother. 2016, 28, 25–27. [Google Scholar] [CrossRef]
- D’Onofrio, V.; Conzemius, R.; Varda-Brkić, D.; Bogdan, M.; Grisold, A.; Gyssens, I.C.; Bedenić, B.; Barišić, I. Epidemiology of Colistin-Resistant, Carbapenemase-Producing Enterobacteriaceae and Acinetobacter Baumannii in Croatia. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2020, 81, 104263. [Google Scholar] [CrossRef]
- Makke, G.; Bitar, I.; Salloum, T.; Panossian, B.; Alousi, S.; Arabaghian, H.; Medvecky, M.; Hrabak, J.; Merheb-Ghoussoub, S.; Tokajian, S. Whole-Genome-Sequence-Based Characterization of Extensively Drug-Resistant Acinetobacter Baumannii Hospital Outbreak. mSphere 2020, 5. [Google Scholar] [CrossRef] [PubMed]
- Mammina, C.; Palma, D.M.; Bonura, C.; Aleo, A.; Fasciana, T.; Sodano, C.; Saporito, M.A.; Verde, M.S.; Calà, C.; Cracchiolo, A.N.; et al. Epidemiology and Clonality of Carbapenem-Resistant Acinetobacter Baumannii from an Intensive Care Unit in Palermo, Italy. BMC Res. Notes 2012, 5, 365. [Google Scholar] [CrossRef] [PubMed]
- Nowak, J.; Zander, E.; Stefanik, D.; Higgins, P.G.; Roca, I.; Vila, J.; McConnell, M.J.; Cisneros, J.M.; Seifert, H. High Incidence of Pandrug-Resistant Acinetobacter Baumannii Isolates Collected from Patients with Ventilator-Associated Pneumonia in Greece, Italy and Spain as Part of the MagicBullet Clinical Trial. J. Antimicrob. Chemother. 2017, 72, 3277–3282. [Google Scholar] [CrossRef] [PubMed]
- Dahdouh, E.; Gómez-Gil, R.; Pacho, S.; Mingorance, J.; Daoud, Z.; Suárez, M. Clonality, Virulence Determinants, and Profiles of Resistance of Clinical Acinetobacter Baumannii Isolates Obtained from a Spanish Hospital. PLoS ONE 2017, 12, e0176824. [Google Scholar] [CrossRef]
- Simo Tchuinte, P.L.; Rabenandrasana, M.A.N.; Kowalewicz, C.; Andrianoelina, V.H.; Rakotondrasoa, A.; Andrianirina, Z.Z.; Enouf, V.; Ratsima, E.H.; Randrianirina, F.; Collard, J.-M. Phenotypic and Molecular Characterisations of Carbapenem-Resistant Acinetobacter Baumannii Strains Isolated in Madagascar. Antimicrob. Resist. Infect. Control 2019, 8, 31. [Google Scholar] [CrossRef]
- Shamsizadeh, Z.; Nikaeen, M.; Nasr Esfahani, B.; Mirhoseini, S.H.; Hatamzadeh, M.; Hassanzadeh, A. Detection of Antibiotic Resistant Acinetobacter Baumannii in Various Hospital Environments: Potential Sources for Transmission of Acinetobacter Infections. Environ. Health Prev. Med. 2017, 22, 44. [Google Scholar] [CrossRef]
- da Silva, K.E.; Maciel, W.G.; Croda, J.; Cayô, R.; Ramos, A.C.; de Sales, R.O.; Kurihara, M.N.L.; Vasconcelos, N.G.; Gales, A.C.; Simionatto, S. A High Mortality Rate Associated with Multidrug-Resistant Acinetobacter Baumannii ST79 and ST25 Carrying OXA-23 in a Brazilian Intensive Care Unit. PLoS ONE 2018, 13, e0209367. [Google Scholar] [CrossRef]
- Arhoune, B.; Oumokhtar, B.; Hmami, F.; El Fakir, S.; Moutaouakkil, K.; Chami, F.; Bouharrou, A. Intestinal Carriage of Antibiotic Resistant Acinetobacter Baumannii among Newborns Hospitalized in Moroccan Neonatal Intensive Care Unit. PLoS ONE 2019, 14, e0209425. [Google Scholar] [CrossRef]
- Tafreshi, N.; Babaeekhou, L.; Ghane, M. Antibiotic Resistance Pattern of Acinetobacter Baumannii from Burns Patients: Increase in Prevalence of Bla (OXA-24-like) and Bla (OXA-58-like) Genes. Iran. J. Microbiol. 2019, 11, 502–509. [Google Scholar] [CrossRef]
- Araújo Lima, A.V.; da Silva, S.M.; do Nascimento Júnior, J.A.A.; Correia, M.D.S.; Luz, A.C.; Leal-Balbino, T.C.; da Silva, M.V.; Lima, J.L.D.C.; Maciel, M.A.V.; Napoleão, T.H.; et al. Occurrence and Diversity of Intra- and Interhospital Drug-Resistant and Biofilm-Forming Acinetobacter Baumannii and Pseudomonas Aeruginosa. Microb. Drug Resist. 2020. [Google Scholar] [CrossRef]
- Hu, W.S.; Yao, S.-M.; Fung, C.-P.; Hsieh, Y.-P.; Liu, C.-P.; Lin, J.-F. An OXA-66/OXA-51-like Carbapenemase and Possibly an Efflux Pump Are Associated with Resistance to Imipenem in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2007, 51, 3844–3852. [Google Scholar] [CrossRef] [PubMed]
- Mammina, C.; Bonura, C.; Aleo, A.; Calà, C.; Caputo, G.; Cataldo, M.C.; Di Benedetto, A.; Distefano, S.; Fasciana, T.; Labisi, M.; et al. Characterization of Acinetobacter Baumannii from Intensive Care Units and Home Care Patients in Palermo, Italy. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2011, 17, E12–E15. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pajand, O.; Hojabri, Z.; Nahaei, M.R.; Hajibonabi, F.; Pirzadeh, T.; Aghazadeh, M.; Fasciana, T.; Bonura, C.; Mammina, C. In Vitro Activities of Tetracyclines against Different Clones of Multidrug-Resistant Acinetobacter Baumannii Isolates from Two Iranian Hospitals. Int. J. Antimicrob. Agents 2014, 476–478. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mendes, R.E.; Bell, J.M.; Turnidge, J.D.; Castanheira, M.; Jones, R.N. Emergence and Widespread Dissemination of OXA-23, -24/40 and -58 Carbapenemases among Acinetobacter spp. in Asia-Pacific Nations: Report from the SENTRY Surveillance Program. J. Antimicrob. Chemother. 2009, 63, 55–59. [Google Scholar] [CrossRef]
- Vahaboglu, H.; Budak, F.; Kasap, M.; Gacar, G.; Torol, S.; Karadenizli, A.; Kolayli, F.; Eroglu, C. High Prevalence of OXA-51-Type Class D Beta-Lactamases among Ceftazidime-Resistant Clinical Isolates of Acinetobacter spp.: Co-Existence with OXA-58 in Multiple Centres. J. Antimicrob. Chemother. 2006, 58, 537–542. [Google Scholar] [CrossRef]
- Lolans, K.; Rice, T.W.; Munoz-Price, L.S.; Quinn, J.P. Multicity Outbreak of Carbapenem-Resistant Acinetobacter Baumannii Isolates Producing the Carbapenemase OXA-40. Antimicrob. Agents Chemother. 2006, 50, 2941–2945. [Google Scholar] [CrossRef]
- Mugnier, P.D.; Poirel, L.; Naas, T.; Nordmann, P. Worldwide Dissemination of the BlaOXA-23 Carbapenemase Gene of Acinetobacter Baumannii. Emerg. Infect. Dis. 2010, 16, 35–40. [Google Scholar] [CrossRef]
- Chagas, T.P.G.; Carvalho, K.R.; de Oliveira Santos, I.C.; Carvalho-Assef, A.P.D.; Asensi, M.D. Characterization of Carbapenem-Resistant Acinetobacter Baumannii in Brazil (2008–2011): Countrywide Spread of OXA-23-Producing Clones (CC15 and CC79). Diagn. Microbiol. Infect. Dis. 2014, 79, 468–472. [Google Scholar] [CrossRef]
- Pagano, M.; Martins, A.F.; Machado, A.B.M.P.; Barin, J.; Barth, A.L. Carbapenem-Susceptible Acinetobacter Baumannii Carrying the ISAba1 Upstream BlaOXA-51-like Gene in Porto Alegre, Southern Brazil. Epidemiol. Infect. 2013, 141, 330–333. [Google Scholar] [CrossRef]
- Ben Othman, A.; Zribi, M.; Masmoudi, A.; Abdellatif, S.; Ben Lakhal, S.; Fendri, C. Multiresistance and Endemic Status of Acinetobacter Baumannii Associated with Nosocomial Infections in a Tunisian Hospital: A Critical Situation in the Intensive Care Units. Braz. J. Microbiol. 2011, 42, 415–422. [Google Scholar] [CrossRef]
- Akbari, M.; Niakan, M.; Taherikalani, M.; Feizabadi, M.M.; Azadi, N.A.; Soroush, S.; Emaneini, M.; Abdolkarimi, A.; Maleki, A.; Hematian, A. Rapid Identification of Iranian Acinetobacter Baumannii Strains by Single PCR Assay Using BLA Oxa-51 -like Carbapenemase and Evaluation of the Antimicrobial Resistance Profiles of the Isolates. Acta Microbiol. Immunol. Hung. 2010, 57, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Çiftci, I.H.; Aşik, G.; Karakeçe, E.; Öksüz, L.; Yaǧci, S.; Sesli Çetin, E.; Özdemir, M.; Atasoy, A.R.; Koçoǧlu, E.; Gül, M.; et al. Distribution of Bla OXA Genes in Acinetobacter Baumannii Strains: A Multicenter Study. Mikrobiyol. Bul. 2013, 47, 592–602. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lopes, B.S.; Gallego, L.; Amyes, S.G.B. Multi-Drug Resistance Profiles and the Genetic Features of Acinetobacter Baumannii Isolates from Bolivia. J. Infect. Dev. Ctries. 2013, 7, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Rammelkamp, C.H.; Maxon, T. Resistance of Staphylococcus Aureus to the Action of Penicillin. Proc. Soc. Exp. Biol. Med. 1942, 51, 386–389. [Google Scholar] [CrossRef]
- Sultan, I.; Rahman, S.; Jan, A.T.; Siddiqui, M.T.; Mondal, A.H.; Haq, Q.M.R. Antibiotics, Resistome and Resistance Mechanisms: A Bacterial Perspective. Front. Microbiol. 2018, 9, 2066. [Google Scholar] [CrossRef] [PubMed]
- Munita, J.M.; Arias, C.A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 2016, 4. [Google Scholar] [CrossRef]
- D’Costa, V.M.; King, C.E.; Kalan, L.; Morar, M.; Sung, W.W.L.; Schwarz, C.; Froese, D.; Zazula, G.; Calmels, F.; Debruyne, R.; et al. Antibiotic Resistance Is Ancient. Nature 2011, 477, 457–461. [Google Scholar] [CrossRef]
- Wright, G.D. Molecular Mechanisms of Antibiotic Resistance. Chem. Commun. 2011, 47, 4055–4061. [Google Scholar] [CrossRef]
- Abraham, E.P.; Chain, E. An Enzyme from Bacteria Able to Destroy Penicillin. 1940. Rev. Infect. Dis. 1988, 10, 677–678. [Google Scholar]
- Hall, B.G.; Barlow, M. Evolution of the Serine Beta-Lactamases: Past, Present and Future. Drug Resist. Updat. Rev. Comment. Antimicrob. Anticancer Chemother. 2004, 7, 111–123. [Google Scholar] [CrossRef]
- Barlow, M.; Hall, B.G. Phylogenetic Analysis Shows That the OXA Beta-Lactamase Genes Have Been on Plasmids for Millions of Years. J. Mol. Evol. 2002, 55, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Frère, J.M.; Duez, C.; Ghuysen, J.M.; Vandekerkhove, J. Occurrence of a Serine Residue in the Penicillin-Binding Site of the Exocellular DD-Carboxy-Peptidase-Transpeptidase from Streptomyces R61. FEBS Lett. 1976, 70, 257–260. [Google Scholar] [CrossRef]
- Massova, I.; Mobashery, S. Kinship and Diversification of Bacterial Penicillin-Binding Proteins and Beta-Lactamases. Antimicrob. Agents Chemother. 1998, 42, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.F.; Mobashery, S. β-Lactam Resistance Mechanisms: Gram-Positive Bacteria and Mycobacterium Tuberculosis. Cold Spring Harb. Perspect. Med. 2016, 6. [Google Scholar] [CrossRef]
- Matthew, M.; Harris, A.M. Identification of Beta-Lactamases by Analytical Isoelectric Focusing: Correlation with Bacterial Taxonomy. J. Gen. Microbiol. 1976, 94, 55–67. [Google Scholar] [CrossRef]
- Ambler, R.P. The Structure of Beta-Lactamases. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 1980, 289, 321–331. [Google Scholar] [CrossRef]
- Bush, K.; Jacoby, G.A.; Medeiros, A.A. A Functional Classification Scheme for Beta-Lactamases and Its Correlation with Molecular Structure. Antimicrob. Agents Chemother. 1995, 39, 1211–1233. [Google Scholar] [CrossRef]
- Bush, K.; Jacoby, G.A. Updated Functional Classification of Beta-Lactamases. Antimicrob. Agents Chemother. 2010, 54, 969–976. [Google Scholar] [CrossRef]
- Bush, K. Proliferation and Significance of Clinically Relevant β-Lactamases. Ann. N. Y. Acad. Sci. 2013, 1277, 84–90. [Google Scholar] [CrossRef]
- Jeon, J.H.; Lee, J.H.; Lee, J.J.; Park, K.S.; Karim, A.M.; Lee, C.-R.; Jeong, B.C.; Lee, S.H. Structural Basis for Carbapenem-Hydrolyzing Mechanisms of Carbapenemases Conferring Antibiotic Resistance. Int. J. Mol. Sci. 2015, 16, 9654–9692. [Google Scholar] [CrossRef]
- Naas, T.; Dortet, L.; Iorga, B.I. Structural and Functional Aspects of Class A Carbapenemases. Curr. Drug Targets 2016, 17, 1006–1028. [Google Scholar] [CrossRef] [PubMed]
- Bush, K. The ABCD’s of β-Lactamase Nomenclature. J. Infect. Chemother. Off. J. Jpn. Soc. Chemother. 2013, 19, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Palzkill, T. Metallo-β-Lactamase Structure and Function. Ann. N. Y. Acad. Sci. 2013, 1277, 91–104. [Google Scholar] [CrossRef] [PubMed]
- Aoki, N.; Ishii, Y.; Tateda, K.; Saga, T.; Kimura, S.; Kikuchi, Y.; Kobayashi, T.; Tanabe, Y.; Tsukada, H.; Gejyo, F.; et al. Efficacy of Calcium-EDTA as an Inhibitor for Metallo-β-Lactamase in a Mouse Model of Pseudomonas Aeruginosa Pneumonia. Antimicrob. Agents Chemother. 2010, 54, 4582–4588. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, Y.; Murakami, M.; Suzuki, K.; Ito, H.; Wacharotayankun, R.; Ohsuka, S.; Kato, N.; Ohta, M. A Novel Integron-like Element Carrying the Metallo-Beta-Lactamase Gene BlaIMP. Antimicrob. Agents Chemother. 1995, 39, 1612–1615. [Google Scholar] [CrossRef] [PubMed]
- Lauretti, L.; Riccio, M.L.; Mazzariol, A.; Cornaglia, G.; Amicosante, G.; Fontana, R.; Rossolini, G.M. Cloning and Characterization of BlaVIM, a New Integron-Borne Metallo-Beta-Lactamase Gene from a Pseudomonas Aeruginosa Clinical Isolate. Antimicrob. Agents Chemother. 1999, 43, 1584–1590. [Google Scholar] [CrossRef] [PubMed]
- Toleman, M.A.; Simm, A.M.; Murphy, T.A.; Gales, A.C.; Biedenbach, D.J.; Jones, R.N.; Walsh, T.R. Molecular Characterization of SPM-1, a Novel Metallo-β-Lactamase Isolated in Latin America: Report from the SENTRY Antimicrobial Surveillance Programme. J. Antimicrob. Chemother. 2002, 50, 673–679. [Google Scholar] [CrossRef]
- Castanheira, M.; Toleman, M.A.; Jones, R.N.; Schmidt, F.J.; Walsh, T.R. Molecular Characterization of a Beta-Lactamase Gene, BlaGIM-1, Encoding a New Subclass of Metallo-Beta-Lactamase. Antimicrob. Agents Chemother. 2004, 48, 4654–4661. [Google Scholar] [CrossRef]
- Yong, D.; Toleman, M.A.; Giske, C.G.; Cho, H.S.; Sundman, K.; Lee, K.; Walsh, T.R. Characterization of a New Metallo-Beta-Lactamase Gene, Bla(NDM-1), and a Novel Erythromycin Esterase Gene Carried on a Unique Genetic Structure in Klebsiella Pneumoniae Sequence Type 14 from India. Antimicrob. Agents Chemother. 2009, 53, 5046–5054. [Google Scholar] [CrossRef]
- Pollini, S.; Maradei, S.; Pecile, P.; Olivo, G.; Luzzaro, F.; Docquier, J.-D.; Rossolini, G.M. FIM-1, a New Acquired Metallo-β-Lactamase from a Pseudomonas Aeruginosa Clinical Isolate from Italy. Antimicrob. Agents Chemother. 2013, 57, 410–416. [Google Scholar] [CrossRef]
- Jacoby, G.A. AmpC Beta-Lactamases. Clin. Microbiol. Rev. 2009, 22, 161–182. [Google Scholar] [CrossRef] [PubMed]
- Thomson, K.S. Extended-Spectrum-Beta-Lactamase, AmpC, and Carbapenemase Issues. J. Clin. Microbiol. 2010, 48, 1019–1025. [Google Scholar] [CrossRef] [PubMed]
- Gordon, N.C.; Wareham, D.W. Multidrug-Resistant Acinetobacter Baumannii: Mechanisms of Virulence and Resistance. Int. J. Antimicrob. Agents 2010, 35, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Liu, B.; Chen, Y.; Huang, H.; Wang, G.; Li, F.; Ni, Z. Molecular Characterization of Ambler Class A to D β-Lactamases, ISAba1, and Integrons Reveals Multidrug-Resistant Acinetobacter spp. Isolates in Northeastern China. J. Chemother. 2016, 28, 469–475. [Google Scholar] [CrossRef]
- Lin, M.-F.; Chang, K.-C.; Lan, C.-Y.; Chou, J.; Kuo, J.-W.; Chang, C.-K.; Liou, M.-L. Molecular Epidemiology and Antimicrobial Resistance Determinants of Multidrug-Resistant Acinetobacter Baumannii in Five Proximal Hospitals in Taiwan. Jpn. J. Infect. Dis. 2011, 64, 222–227. [Google Scholar]
- Lin, M.-F.; Lan, C.-Y. Antimicrobial Resistance in Acinetobacter Baumannii: From Bench to Bedside. World J. Clin. Cases 2014, 2, 787–814. [Google Scholar] [CrossRef]
- Nowak, P.; Paluchowska, P. Acinetobacter Baumannii: Biology and Drug Resistance—Role of Carbapenemases. Folia Histochem. Cytobiol. 2016, 54, 61–74. [Google Scholar] [CrossRef][Green Version]
- Lyon, J.A. Imipenem/Cilastatin: The First Carbapenem Antibiotic. Drug Intell. Clin. Pharm. 1985, 19, 895–899. [Google Scholar]
- Périchon, B.; Goussard, S.; Walewski, V.; Krizova, L.; Cerqueira, G.; Murphy, C.; Feldgarden, M.; Wortman, J.; Clermont, D.; Nemec, A.; et al. Identification of 50 Class D β-Lactamases and 65 Acinetobacter-Derived Cephalosporinases in Acinetobacter spp. Antimicrob. Agents Chemother. 2014, 58, 936–949. [Google Scholar] [CrossRef]
- Al Atrouni, A.; Hamze, M.; Jisr, T.; Lemarié, C.; Eveillard, M.; Joly-Guillou, M.-L.; Kempf, M. Wide Spread of OXA-23-Producing Carbapenem-Resistant Acinetobacter Baumannii Belonging to Clonal Complex II in Different Hospitals in Lebanon. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2016, 52, 29–36. [Google Scholar] [CrossRef]
- Davandeh, I.; Eraç, B.; Aydemir, S.Ş. Investigation of Class-d Beta-Lactamases Causing Carbapenem Resistance in Clinical Acinetobacter Baumannii Isolates. Turk. J. Med. Sci. 2017, 47, 1661–1666. [Google Scholar] [CrossRef] [PubMed]
- Evans, B.A.; Amyes, S.G.B. OXA β-Lactamases. Clin. Microbiol. Rev. 2014, 27, 241–263. [Google Scholar] [CrossRef] [PubMed]
- Donald, H.M.; Scaife, W.; Amyes, S.G.; Young, H.K. Sequence Analysis of ARI-1, a Novel OXA Beta-Lactamase, Responsible for Imipenem Resistance in Acinetobacter Baumannii 6B92. Antimicrob. Agents Chemother. 2000, 44, 196–199. [Google Scholar] [CrossRef] [PubMed]
- Potron, A.; Munoz-Price, L.S.; Nordmann, P.; Cleary, T.; Poirel, L. Genetic Features of CTX-M-15-Producing Acinetobacter Baumannii from Haiti. Antimicrob. Agents Chemother. 2011, 55, 5946–5948. [Google Scholar] [CrossRef]
- Gupta, R.; Malik, A.; Rizvi, M.; Ahmed, M. Presence of Metallo-Beta-Lactamases (MBL), Extended-Spectrum Beta-Lactamase (ESBL) & AmpC Positive Non-Fermenting Gram-Negative Bacilli among Intensive Care Unit Patients with Special Reference to Molecular Detection of Bla(CTX-M) & Bla(AmpC) Genes. Indian J. Med. Res. 2016, 144, 271–275. [Google Scholar] [CrossRef]
- Beriş, F.Ş.; Budak, E.E.; Gülek, D.; Uzun, A.; Çizmeci, Z.; Mengeloğlu, F.Z.; Direkel, Ş.; Çetinkol, Y.; Ay Altıntop, Y.; Iraz, M.; et al. [Investigation of the frequency and distribution of beta-lactamase genes in the clinical isolates of Acinetobacter baumannii collected from different regions of Turkey: A multicenter study]. Mikrobiyol. Bull. 2016, 50, 511–521. [Google Scholar] [CrossRef][Green Version]
- Freitas, D.Y.; Araújo, S.; Folador, A.R.C.; Ramos, R.T.J.; Azevedo, J.S.N.; Tacão, M.; Silva, A.; Henriques, I.; Baraúna, R.A. Extended Spectrum Beta-Lactamase-Producing Gram-Negative Bacteria Recovered From an Amazonian Lake Near the City of Belém, Brazil. Front. Microbiol. 2019, 10, 364. [Google Scholar] [CrossRef]
- Alyamani, E.J.; Khiyami, M.A.; Booq, R.Y.; Alnafjan, B.M.; Altammami, M.A.; Bahwerth, F.S. Molecular Characterization of Extended-Spectrum Beta-Lactamases (ESBLs) Produced by Clinical Isolates of Acinetobacter Baumannii in Saudi Arabia. Ann. Clin. Microbiol. Antimicrob. 2015, 14, 38. [Google Scholar] [CrossRef]
- Mayanskiy, N.; Chebotar, I.; Alyabieva, N.; Kryzhanovskaya, O.; Savinova, T.; Turenok, A.; Bocharova, Y.; Lazareva, A.; Polikarpova, S.; Karaseva, O. Emergence of the Uncommon Clone ST944/ST78 Carrying Bla(OXA-40-like) and Bla(CTX-M-like) Genes Among Carbapenem-Nonsusceptible Acinetobacter Baumannii in Moscow, Russia. Microb. Drug Resist. 2017, 23, 864–870. [Google Scholar] [CrossRef]
- Zago, M.C.B.; Viana, G.F.; Ecker, A.B.S.; Nishiyama, S.A.B.; Zarpellon, M.N.; Dias, J.R.C.; Cardoso, C.L.; Tognim, M.C.B. First Report of CTX-M-15-Producing Acinetobacter Baumannii in Brazil. J. Hosp. Infect. 2016, 298–299. [Google Scholar] [CrossRef]
- Krizova, L.; Poirel, L.; Nordmann, P.; Nemec, A. TEM-1 β-Lactamase as a Source of Resistance to Sulbactam in Clinical Strains of Acinetobacter Baumannii. J. Antimicrob. Chemother. 2013, 68, 2786–2791. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Ling, B.; Zhou, L. Prevalence of 16S RRNA Methylase, Modifying Enzyme, and Extended-Spectrum Beta-Lactamase Genes among Acinetobacter Baumannii Isolates. J. Chemother. 2015, 27, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Ibrahimagić, A.; Kamberović, F.; Uzunović, S.; Bedenić, B.; Idrizović, E. Molecular Characteristics and Antibiotic Resistance of Acinetobacter Baumanniibeta-Lactamase-Producing Isolates, a Predominance of Intrinsic BlaOXA-51, and Detection of TEM and CTX-M Genes. Turk. J. Med. Sci. 2017, 47, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, J.; Yu, P.; Ge, P.; Jiang, Y.; Xu, R.; Chen, R.; Liu, X. Identification of Antibiotic Resistance Genes in the Multidrug-Resistant Acinetobacter Baumannii Strain, MDR-SHH02, Using Whole-Genome Sequencing. Int. J. Mol. Med. 2017, 39, 364–372. [Google Scholar] [CrossRef]
- Abdar, M.H.; Taheri-Kalani, M.; Taheri, K.; Emadi, B.; Hasanzadeh, A.; Sedighi, A.; Pirouzi, S.; Sedighi, M. Prevalence of Extended-Spectrum Beta-Lactamase Genes in Acinetobacter Baumannii Strains Isolated from Nosocomial Infections in Tehran, Iran. GMS Hyg. Infect. Control 2019, 14, Doc02. [Google Scholar] [CrossRef]
- Asgin, N.; Otlu, B.; Cakmakliogullari, E.K.; Celik, B. High Prevalence of TEM, VIM, and OXA-2 Beta-Lactamases and Clonal Diversity among Acinetobacter Baumannii Isolates in Turkey. J. Infect. Dev. Ctries. 2019, 13, 794–801. [Google Scholar] [CrossRef]
- Agoba, E.E.; Govinden, U.; Peer, A.K.C.; Osei Sekyere, J.; Essack, S.Y. ISAba1 Regulated OXA-23 Carbapenem Resistance in Acinetobacter Baumannii Strains in Durban, South Africa. Microb. Drug Resist. 2018, 24, 1289–1295. [Google Scholar] [CrossRef]
- Al-Agamy, M.H.; Jeannot, K.; El-Mahdy, T.S.; Shibl, A.M.; Kattan, W.; Plésiat, P.; Courvalin, P. First Detection of GES-5 Carbapenemase-Producing Acinetobacter Baumannii Isolate. Microb. Drug Resist. 2017, 23, 556–562. [Google Scholar] [CrossRef]
- Chihi, H.; Bonnin, R.A.; Bourouis, A.; Mahrouki, S.; Besbes, S.; Moussa, M.B.; Belhadj, O.; Naas, T. GES-11-Producing Acinetobacter Baumannii Clinical Isolates from Tunisian Hospitals: Long-Term Dissemination of GES-Type Carbapenemases in North Africa. J. Glob. Antimicrob. Resist. 2016, 5, 47–50. [Google Scholar] [CrossRef]
- Mabrouk, A.; Grosso, F.; Botelho, J.; Achour, W.; Ben Hassen, A.; Peixe, L. GES-14-Producing Acinetobacter Baumannii Isolates in a Neonatal Intensive Care Unit in Tunisia Are Associated with a Typical Middle East Clone and a Transferable Plasmid. Antimicrob. Agents Chemother. 2017. [Google Scholar] [CrossRef]
- El-Shazly, S.; Dashti, A.; Vali, L.; Bolaris, M.; Ibrahim, A.S. Molecular Epidemiology and Characterization of Multiple Drug-Resistant (MDR) Clinical Isolates of Acinetobacter Baumannii. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2015, 41, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Aly, M.M.; Abu Alsoud, N.M.; Elrobh, M.S.; Al Johani, S.M.; Balkhy, H.H. High Prevalence of the PER-1 Gene among Carbapenem-Resistant Acinetobacter Baumannii in Riyadh, Saudi Arabia. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2016, 35, 1759–1766. [Google Scholar] [CrossRef] [PubMed]
- Pasterán, F.; Rapoport, M.; Petroni, A.; Faccone, D.; Corso, A.; Galas, M.; Vázquez, M.; Procopio, A.; Tokumoto, M.; Cagnoni, V. Emergence of PER-2 and VEB-1a in Acinetobacter Baumannii Strains in the Americas. Antimicrob. Agents Chemother. 2006, 3222–3224. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bonnin, R.A.; Potron, A.; Poirel, L.; Lecuyer, H.; Neri, R.; Nordmann, P. PER-7, an Extended-Spectrum Beta-Lactamase with Increased Activity toward Broad-Spectrum Cephalosporins in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2011, 55, 2424–2427. [Google Scholar] [CrossRef] [PubMed]
- Al-Hassan, L.; El Mahallawy, H.; Amyes, S.G.B. First Report of Bla(PER-3) in Acinetobacter Baumannii. Int. J. Antimicrob. Agents. 2013, 93–94. [Google Scholar] [CrossRef]
- Huang, L.-Y.; Chen, T.-L.; Lu, P.-L.; Tsai, C.-A.; Cho, W.-L.; Chang, F.-Y.; Fung, C.-P.; Siu, L.K. Dissemination of Multidrug-Resistant, Class 1 Integron-Carrying Acinetobacter Baumannii Isolates in Taiwan. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2008, 14, 1010–1019. [Google Scholar] [CrossRef]
- Azimi, L.; Talebi, M.; Pourshafie, M.-R.; Owlia, P.; Rastegar Lari, A. Characterization of Carbapenemases in Extensively Drug Resistance Acinetobacter Baumannii in a Burn Care Center in Iran. Int. J. Mol. Cell. Med. 2015, 4, 46–53. [Google Scholar]
- Robledo, I.E.; Aquino, E.E.; Santé, M.I.; Santana, J.L.; Otero, D.M.; León, C.F.; Vázquez, G.J. Detection of KPC in Acinetobacter spp. in Puerto Rico. Antimicrob. Agents Chemother. 2010, 54, 1354–1357. [Google Scholar] [CrossRef]
- Martinez, T.; Martinez, I.; Vazquez, G.J.; Aquino, E.E.; Robledo, I.E. Genetic Environment of the KPC Gene in Acinetobacter Baumannii ST2 Clone from Puerto Rico and Genomic Insights into Its Drug Resistance. J. Med. Microbiol. 2016, 65, 784–792. [Google Scholar] [CrossRef]
- Poirel, L.; Corvec, S.; Rapoport, M.; Mugnier, P.; Petroni, A.; Pasteran, F.; Faccone, D.; Galas, M.; Drugeon, H.; Cattoir, V.; et al. Identification of the Novel Narrow-Spectrum Beta-Lactamase SCO-1 in Acinetobacter spp. from Argentina. Antimicrob. Agents Chemother. 2007, 51, 2179–2184. [Google Scholar] [CrossRef]
- Potron, A.; Poirel, L.; Croizé, J.; Chanteperdrix, V.; Nordmann, P. Genetic and Biochemical Characterization of the First Extended-Spectrum CARB-Type Beta-Lactamase, RTG-4, from Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2009, 53, 3010–3016. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, M.S.; Piñeiro, S.; Centrón, D. Novel Insights about Class 2 Integrons from Experimental and Genomic Epidemiology. Antimicrob. Agents Chemother. 2010, 54, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Naas, T.; Namdari, F.; Réglier-Poupet, H.; Poyart, C.; Nordmann, P. Panresistant Extended-Spectrum Beta-Lactamase SHV-5-Producing Acinetobacter Baumannii from New York City. J. Antimicrob. Chemother. 2007, 1174–1176. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huang, Z.; Mao, P.; Chen, Y.; Wu, L.; Wu, J. Study on the molecular epidemiology of SHV type beta-lactamase-encoding genes of multiple-drug-resistant acinetobacter baumannii. Zhonghua Liu Xing Bing Xue Za Zhi 2004, 25, 425–427. [Google Scholar]
- Potron, A.; Poirel, L.; Nordmann, P. Emerging Broad-Spectrum Resistance in Pseudomonas Aeruginosa and Acinetobacter Baumannii: Mechanisms and Epidemiology. Int. J. Antimicrob. Agents 2015, 45, 568–585. [Google Scholar] [CrossRef]
- Gales, A.C.; Tognim, M.C.B.; Reis, A.O.; Jones, R.N.; Sader, H.S. Emergence of an IMP-like Metallo-Enzyme in an Acinetobacter Baumannii Clinical Strain from a Brazilian Teaching Hospital. Diagn. Microbiol. Infect. Dis. 2003, 45, 77–79. [Google Scholar] [CrossRef]
- Riccio, M.L.; Franceschini, N.; Boschi, L.; Caravelli, B.; Cornaglia, G.; Fontana, R.; Amicosante, G.; Rossolini, G.M. Characterization of the Metallo-Beta-Lactamase Determinant of Acinetobacter Baumannii AC-54/97 Reveals the Existence of Bla(IMP) Allelic Variants Carried by Gene Cassettes of Different Phylogeny. Antimicrob. Agents Chemother. 2000, 44, 1229–1235. [Google Scholar] [CrossRef]
- Chu, Y.W.; Afzal-Shah, M.; Houang, E.T.; Palepou, M.I.; Lyon, D.J.; Woodford, N.; Livermore, D.M. IMP-4, a Novel Metallo-Beta-Lactamase from Nosocomial Acinetobacter spp. Collected in Hong Kong between 1994 and 1998. Antimicrob. Agents Chemother. 2001, 45, 710–714. [Google Scholar] [CrossRef]
- Yamamoto, M.; Nagao, M.; Matsumura, Y.; Matsushima, A.; Ito, Y.; Takakura, S.; Ichiyama, S. Interspecies Dissemination of a Novel Class 1 Integron Carrying BlaIMP-19 among Acinetobacter Species in Japan. J. Antimicrob. Chemother. 2011, 66, 2480–2483. [Google Scholar] [CrossRef]
- Lee, M.-F.; Peng, C.-F.; Hsu, H.-J.; Chen, Y.-H. Molecular Characterisation of the Metallo-Beta-Lactamase Genes in Imipenem-Resistant Gram-Negative Bacteria from a University Hospital in Southern Taiwan. Int. J. Antimicrob. Agents 2008, 32, 475–480. [Google Scholar] [CrossRef]
- Koh, T.H.; Sng, L.-H.; Wang, G.C.Y.; Hsu, L.-Y.; Zhao, Y. IMP-4 and OXA Beta-Lactamases in Acinetobacter Baumannii from Singapore. J. Antimicrob. Chemother. 2007, 59, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Tognim, M.C.B.; Gales, A.C.; Penteado, A.P.; Silbert, S.; Sader, H.S. Dissemination of IMP-1 Metallo- Beta -Lactamase-Producing Acinetobacter Species in a Brazilian Teaching Hospital. Infect. Control Hosp. Epidemiol. 2006, 27, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Cayô, R.; Rodrigues-Costa, F.; Matos, A.P.; Carvalhaes, C.G.; Jové, T.; Gales, A.C. Identification of a New Integron Harboring Bla(IMP-10) in Carbapenem-Resistant Acinetobacter Baumannii Clinical Isolates. Antimicrob. Agents Chemother. 2015, 3687–3689. [Google Scholar] [CrossRef] [PubMed]
- Papa, A.; Koulourida, V.; Souliou, E. Molecular Epidemiology of Carbapenem-Resistant Acinetobacter Baumannii in a Newly Established Greek Hospital. Microb. Drug Resist. 2009, 15, 257–260. [Google Scholar] [CrossRef]
- Tsakris, A.; Ikonomidis, A.; Pournaras, S.; Tzouvelekis, L.S.; Sofianou, D.; Legakis, N.J.; Maniatis, A.N. VIM-1 Metallo-Beta-Lactamase in Acinetobacter Baumannii. Emerg. Infect. Dis. 2006, 12, 981–983. [Google Scholar] [CrossRef]
- Bonnin, R.A.; Poirel, L.; Naas, T.; Pirs, M.; Seme, K.; Schrenzel, J.; Nordmann, P. Dissemination of New Delhi Metallo-β-Lactamase-1-Producing Acinetobacter Baumannii in Europe. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2012, 18, E362-5. [Google Scholar] [CrossRef]
- Voulgari, E.; Politi, L.; Pitiriga, V.; Dendrinos, J.; Poulou, A.; Georgiadis, G.; Tsakris, A. First Report of an NDM-1 Metallo-β-Lactamase-Producing Acinetobacter Baumannii Clinical Isolate in Greece. Int. J. Antimicrob. Agents. 2016, 761–762. [Google Scholar] [CrossRef]
- Espinal, P.; Fugazza, G.; López, Y.; Kasma, M.; Lerman, Y.; Malhotra-Kumar, S.; Goossens, H.; Carmeli, Y.; Vila, J. Dissemination of an NDM-2-Producing Acinetobacter Baumannii Clone in an Israeli Rehabilitation Center. Antimicrob. Agents Chemother. 2011, 55, 5396–5398. [Google Scholar] [CrossRef]
- Kumar, M. Identification of a Novel NDM Variant, BlaNDM-3, From a Multidrug-Resistant Acinetobacter Baumannii. Infect. Control Hosp. Epidemiol. 2016, 747–748. [Google Scholar] [CrossRef][Green Version]
- Lee, K.; Yum, J.H.; Yong, D.; Lee, H.M.; Kim, H.D.; Docquier, J.-D.; Rossolini, G.M.; Chong, Y. Novel Acquired Metallo-Beta-Lactamase Gene, Bla(SIM-1), in a Class 1 Integron from Acinetobacter Baumannii Clinical Isolates from Korea. Antimicrob. Agents Chemother. 2005, 49, 4485–4491. [Google Scholar] [CrossRef]
- Segal, H.; Nelson, E.C.; Elisha, B.G. Genetic Environment and Transcription of AmpC in an Acinetobacter Baumannii Clinical Isolate. Antimicrob. Agents Chemother. 2004, 48, 612–614. [Google Scholar] [CrossRef] [PubMed]
- Hujer, K.M.; Hamza, N.S.; Hujer, A.M.; Perez, F.; Helfand, M.S.; Bethel, C.R.; Thomson, J.M.; Anderson, V.E.; Barlow, M.; Rice, L.B.; et al. Identification of a New Allelic Variant of the Acinetobacter Baumannii Cephalosporinase, ADC-7 Beta-Lactamase: Defining a Unique Family of Class C Enzymes. Antimicrob. Agents Chemother. 2005, 49, 2941–2948. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Liu, X. Detection of AmpC β-Lactamases in Acinetobacter Baumannii in the Xuzhou Region and Analysis of Drug Resistance. Exp. Ther. Med. 2015, 10, 933–936. [Google Scholar] [CrossRef]
- Poirel, L.; Figueiredo, S.; Cattoir, V.; Carattoli, A.; Nordmann, P. Acinetobacter Radioresistens as a Silent Source of Carbapenem Resistance for Acinetobacter spp. Antimicrob. Agents Chemother. 2008, 52, 1252–1256. [Google Scholar] [CrossRef] [PubMed]
- Boo, T.W.; Crowley, B. Detection of BlaOXA-58 and BlaOXA-23-like Genes in Carbapenem-Susceptible Acinetobacter Clinical Isolates: Should We Be Concerned? J. Med. Microbiol. 2009, 839–841. [Google Scholar] [CrossRef]
- Kaitany, K.-C.J.; Klinger, N.V.; June, C.M.; Ramey, M.E.; Bonomo, R.A.; Powers, R.A.; Leonard, D.A. Structures of the Class D Carbapenemases OXA-23 and OXA-146: Mechanistic Basis of Activity against Carbapenems, Extended-Spectrum Cephalosporins, and Aztreonam. Antimicrob. Agents Chemother. 2013, 57, 4848–4855. [Google Scholar] [CrossRef] [PubMed]
- Afzal-Shah, M.; Woodford, N.; Livermore, D.M. Characterization of OXA-25, OXA-26, and OXA-27, Molecular Class D Beta-Lactamases Associated with Carbapenem Resistance in Clinical Isolates of Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2001, 45, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Bou, G.; Oliver, A.; Martínez-Beltrán, J. OXA-24, a Novel Class D Beta-Lactamase with Carbapenemase Activity in an Acinetobacter Baumannii Clinical Strain. Antimicrob. Agents Chemother. 2000, 44, 1556–1561. [Google Scholar] [CrossRef]
- Santillana, E.; Beceiro, A.; Bou, G.; Romero, A. Crystal Structure of the Carbapenemase OXA-24 Reveals Insights into the Mechanism of Carbapenem Hydrolysis. Proc. Natl. Acad. Sci. USA 2007, 104, 5354–5359. [Google Scholar] [CrossRef]
- Brown, S.; Young, H.K.; Amyes, S.G.B. Characterisation of OXA-51, a Novel Class D Carbapenemase Found in Genetically Unrelated Clinical Strains of Acinetobacter Baumannii from Argentina. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2005, 11, 15–23. [Google Scholar] [CrossRef]
- Héritier, C.; Poirel, L.; Fournier, P.-E.; Claverie, J.-M.; Raoult, D.; Nordmann, P. Characterization of the Naturally Occurring Oxacillinase of Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2005, 49, 4174–4179. [Google Scholar] [CrossRef] [PubMed]
- Aly, M.; Tayeb, H.T.; Al Johani, S.M.; Alyamani, E.J.; Aldughaishem, F.; Alabdulkarim, I.; Balkhy, H.H. Genetic Diversity of OXA-51-like Genes among Multidrug-Resistant Acinetobacter Baumannii in Riyadh, Saudi Arabia. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2014, 33, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Evans, B.A.; Hamouda, A.; Towner, K.J.; Amyes, S.G.B. OXA-51-like Beta-Lactamases and Their Association with Particular Epidemic Lineages of Acinetobacter Baumannii. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2008, 14, 268–275. [Google Scholar] [CrossRef]
- Rafei, R.; Pailhoriès, H.; Hamze, M.; Eveillard, M.; Mallat, H.; Dabboussi, F.; Joly-Guillou, M.-L.; Kempf, M. Molecular Epidemiology of Acinetobacter Baumannii in Different Hospitals in Tripoli, Lebanon Using Bla(OXA-51-like) Sequence Based Typing. BMC Microbiol. 2015, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- Evans, B.A.; Brown, S.; Hamouda, A.; Findlay, J.; Amyes, S.G.B. Eleven Novel OXA-51-like Enzymes from Clinical Isolates of Acinetobacter Baumannii. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2007, 1137–1138. [Google Scholar] [CrossRef]
- Poirel, L.; Marqué, S.; Héritier, C.; Segonds, C.; Chabanon, G.; Nordmann, P. OXA-58, a Novel Class D {beta}-Lactamase Involved in Resistance to Carbapenems in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2005, 49, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Mansour, W.; Bouallegue, O.; Nordmann, P. Carbapenem-Resistant Acinetobacter Baumannii Isolates from Tunisia Producing the OXA-58-like Carbapenem-Hydrolyzing Oxacillinase OXA-97. Antimicrob. Agents Chemother. 2008, 52, 1613–1617. [Google Scholar] [CrossRef]
- Higgins, P.G.; Schneiders, T.; Hamprecht, A.; Seifert, H. In Vivo Selection of a Missense Mutation in AdeR and Conversion of the Novel BlaOXA-164 Gene into BlaOXA-58 in Carbapenem-Resistant Acinetobacter Baumannii Isolates from a Hospitalized Patient. Antimicrob. Agents Chemother. 2010, 54, 5021–5027. [Google Scholar] [CrossRef]
- Higgins, P.G.; Poirel, L.; Lehmann, M.; Nordmann, P.; Seifert, H. OXA-143, a Novel Carbapenem-Hydrolyzing Class D Beta-Lactamase in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2009, 53, 5035–5038. [Google Scholar] [CrossRef]
- Kim, C.-K.; Lee, Y.; Lee, H.; Woo, G.-J.; Song, W.; Kim, M.-N.; Lee, W.-G.; Jeong, S.H.; Lee, K.; Chong, Y. Prevalence and Diversity of Carbapenemases among Imipenem-Nonsusceptible Acinetobacter Isolates in Korea: Emergence of a Novel OXA-182. Diagn. Microbiol. Infect. Dis. 2010, 68, 432–438. [Google Scholar] [CrossRef]
- Gionco, B.; Pelayo, J.S.; Venancio, E.J.; Cayô, R.; Gales, A.C.; Carrara-Marroni, F.E. Detection of OXA-231, a New Variant of BlaOXA-143, in Acinetobacter Baumannii from Brazil: A Case Report. J. Antimicrob. Chemother. 2012, 2531–2532. [Google Scholar] [CrossRef] [PubMed]
- Mostachio, A.K.; Levin, A.S.; Rizek, C.; Rossi, F.; Zerbini, J.; Costa, S.F. High Prevalence of OXA-143 and Alteration of Outer Membrane Proteins in Carbapenem-Resistant Acinetobacter spp. Isolates in Brazil. Int. J. Antimicrob. Agents 2012, 39, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Oteo, J.; Hernández, J.M.; Espasa, M.; Fleites, A.; Sáez, D.; Bautista, V.; Pérez-Vázquez, M.; Fernández-García, M.D.; Delgado-Iribarren, A.; Sánchez-Romero, I.; et al. Emergence of OXA-48-Producing Klebsiella Pneumoniae and the Novel Carbapenemases OXA-244 and OXA-245 in Spain. J. Antimicrob. Chemother. 2013, 68, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Potron, A.; Poirel, L.; Nordmann, P. Origin of OXA-181, an Emerging Carbapenem-Hydrolyzing Oxacillinase, as a Chromosomal Gene in Shewanella Xiamenensis. Antimicrob. Agents Chemother. 2011, 55, 4405–4407. [Google Scholar] [CrossRef] [PubMed]
- Zong, Z. Discovery of Bla(OXA-199), a Chromosome-Based Bla(OXA-48)-like Variant, in Shewanella Xiamenensis. PLoS ONE 2012, 7, e48280. [Google Scholar] [CrossRef] [PubMed]
- Potron, A.; Rondinaud, E.; Poirel, L.; Belmonte, O.; Boyer, S.; Camiade, S.; Nordmann, P. Genetic and Biochemical Characterisation of OXA-232, a Carbapenem-Hydrolysing Class D β-Lactamase from Enterobacteriaceae. Int. J. Antimicrob. Agents 2013, 41, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Castanheira, M.; Carrër, A.; Rodriguez, C.P.; Jones, R.N.; Smayevsky, J.; Nordmann, P. OXA-163, an OXA-48-Related Class D β-Lactamase with Extended Activity toward Expanded-Spectrum Cephalosporins. Antimicrob. Agents Chemother. 2011, 55, 2546–2551. [Google Scholar] [CrossRef]
- Boyd, D.A.; Mataseje, L.F.; Pelude, L.; Mitchell, R.; Bryce, E.; Roscoe, D.; Embree, J.; Katz, K.; Kibsey, P.; Lavallee, C.; et al. Results from the Canadian Nosocomial Infection Surveillance Program for Detection of Carbapenemase-Producing Acinetobacter spp. in Canadian Hospitals, 2010–2016. J. Antimicrob. Chemother. 2019, 74, 315–320. [Google Scholar] [CrossRef]
- Zhou, Y.; Yu, H.; Guo, Q.; Xu, X.; Ye, X.; Wu, S.; Guo, Y.; Wang, M. Distribution of 16S RRNA Methylases among Different Species of Gram-Negative Bacilli with High-Level Resistance to Aminoglycosides. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2010, 29, 1349–1353. [Google Scholar] [CrossRef]
- Ramirez, M.S.; Tolmasky, M.E. Aminoglycoside Modifying Enzymes. Drug Resist. Update Rev. Comment. Antimicrob. Anticancer Chemother. 2010, 13, 151–171. [Google Scholar] [CrossRef]
- Tada, T.; Miyoshi-Akiyama, T.; Kato, Y.; Ohmagari, N.; Takeshita, N.; Hung, N.V.; Phuong, D.M.; Thu, T.A.; Binh, N.G.; Anh, N.Q.; et al. Emergence of 16S RRNA Methylase-Producing Acinetobacter Baumannii and Pseudomonas Aeruginosa Isolates in Hospitals in Vietnam. BMC Infect. Dis. 2013, 13, 251. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.-T.; Zhou, Y.; Yang, L.; Xu, Y. Multidrug-Resistant Genes of Aminoglycoside-Modifying Enzymes and 16S RRNA Methylases in Acinetobacter Baumannii Strains. Genet. Mol. Res. 2014, 13, 3842–3849. [Google Scholar] [CrossRef] [PubMed]
- Heidary, M.; Salimi Chirani, A.; Khoshnood, S.; Eslami, G.; Atyabi, S.M.; Nazem, H.; Fazilati, M.; Hashemi, A.; Soleimani, S. Molecular Detection of Aminoglycoside-Modifying Enzyme Genes in Acinetobacter Baumannii Clinical Isolates. Acta Microbiol. Immunol. Hung. 2017, 64, 143–150. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hujer, K.M.; Hujer, A.M.; Hulten, E.A.; Bajaksouzian, S.; Adams, J.M.; Donskey, C.J.; Ecker, D.J.; Massire, C.; Eshoo, M.W.; Sampath, R.; et al. Analysis of Antibiotic Resistance Genes in Multidrug-Resistant Acinetobacter Sp. Isolates from Military and Civilian Patients Treated at the Walter Reed Army Medical Center. Antimicrob. Agents Chemother. 2006, 50, 4114–4123. [Google Scholar] [CrossRef] [PubMed]
- Nigro, S.J.; Post, V.; Hall, R.M. Aminoglycoside Resistance in Multiply Antibiotic-Resistant Acinetobacter Baumannii Belonging to Global Clone 2 from Australian Hospitals. J. Antimicrob. Chemother. 2011, 66, 1504–1509. [Google Scholar] [CrossRef] [PubMed]
- Aghazadeh, M.; Rezaee, M.A.; Nahaei, M.R.; Mahdian, R.; Pajand, O.; Saffari, F.; Hassan, M.; Hojabri, Z. Dissemination of Aminoglycoside-Modifying Enzymes and 16S RRNA Methylases among Acinetobacter Baumannii and Pseudomonas Aeruginosa Isolates. Microb. Drug Resist. 2013, 19, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Hasani, A.; Sheikhalizadeh, V.; Ahangarzadeh Rezaee, M.; Rahmati-Yamchi, M.; Hasani, A.; Ghotaslou, R.; Goli, H.R. Frequency of Aminoglycoside-Modifying Enzymes and ArmA Among Different Sequence Groups of Acinetobacter Baumannii in Iran. Microb. Drug Resist. 2016, 22, 347–353. [Google Scholar] [CrossRef]
- Sheikhalizadeh, V.; Hasani, A.; Ahangarzadeh Rezaee, M.; Rahmati-Yamchi, M.; Hasani, A.; Ghotaslou, R.; Goli, H.R. Comprehensive Study to Investigate the Role of Various Aminoglycoside Resistance Mechanisms in Clinical Isolates of Acinetobacter Baumannii. J. Infect. Chemother. Off. J. Jpn. Soc. Chemother. 2017, 23, 74–79. [Google Scholar] [CrossRef]
- Salimizand, H.; Zomorodi, A.R.; Mansury, D.; Khakshoor, M.; Azizi, O.; Khodaparast, S.; Baseri, Z.; Karami, P.; Zamanlou, S.; Farsiani, H.; et al. Diversity of Aminoglycoside Modifying Enzymes and 16S RRNA Methylases in Acinetobacter Baumannii and Acinetobacter Nosocomialis Species in Iran; Wide Distribution of AadA1 and ArmA. Infect. Genet. Evol. J. Mol. Epidemiol. Evol. Genet. Infect. Dis. 2018, 66, 195–199. [Google Scholar] [CrossRef]
- Shooshtari, F.S.; Navidifar, T.; Amin, M.; Goodarzi, H. Coexistence of Genes Encoding Aminoglycoside Modifying Enzymes among Clinical Acinetobacter Baumannii Isolates in Ahvaz, Southwest Iran. Acta Microbiol. Immunol. Hung. 2019, 1–9. [Google Scholar] [CrossRef]
- Akers, K.S.; Chaney, C.; Barsoumian, A.; Beckius, M.; Zera, W.; Yu, X.; Guymon, C.; Keen, E.F., 3rd; Robinson, B.J.; Mende, K.; et al. Aminoglycoside Resistance and Susceptibility Testing Errors in Acinetobacter Baumannii-Calcoaceticus Complex. J. Clin. Microbiol. 2010, 48, 1132–1138. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Arakawa, Y. 16S Ribosomal RNA Methylation: Emerging Resistance Mechanism against Aminoglycosides. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2007, 45, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Garneau-Tsodikova, S.; Labby, K.J. Mechanisms of Resistance to Aminoglycoside Antibiotics: Overview and Perspectives. Medchemcomm 2016, 7, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Magnet, S.; Courvalin, P.; Lambert, T. Resistance-Nodulation-Cell Division-Type Efflux Pump Involved in Aminoglycoside Resistance in Acinetobacter Baumannii Strain BM4454. Antimicrob. Agents Chemother. 2001, 45, 3375–3380. [Google Scholar] [CrossRef]
- Wong, D.; Nielsen, T.B.; Bonomo, R.A.; Pantapalangkoor, P.; Luna, B.; Spellberg, B. Clinical and Pathophysiological Overview of Acinetobacter Infections: A Century of Challenges. Clin. Microbiol. Rev. 2017, 30, 409–447. [Google Scholar] [CrossRef]
- Savic, M.; Lovric, J.; Tomic, T.I.; Vasiljevic, B.; Conn, G.L. Determination of the Target Nucleosides for Members of Two Families of 16S RRNA Methyltransferases That Confer Resistance to Partially Overlapping Groups of Aminoglycoside Antibiotics. Nucleic Acids Res. 2009, 37, 5420–5431. [Google Scholar] [CrossRef]
- Chen, H.; Cao, J.; Zhou, C.; Liu, H.; Zhang, X.; Zhou, T. Biofilm Formation Restrained by Subinhibitory Concentrations of Tigecyclin in Acinetobacter Baumannii Is Associated with Downregulation of Efflux Pumps. Chemotherapy 2017, 62, 128–133. [Google Scholar] [CrossRef]
- Butaye, P.; Cloeckaert, A.; Schwarz, S. Mobile Genes Coding for Efflux-Mediated Antimicrobial Resistance in Gram-Positive and Gram-Negative Bacteria. Int. J. Antimicrob. Agents 2003, 22, 205–210. [Google Scholar] [CrossRef]
- Poole, K. Efflux-Mediated Antimicrobial Resistance. J. Antimicrob. Chemother. 2005, 56, 20–51. [Google Scholar] [CrossRef]
- Coyne, S.; Courvalin, P.; Périchon, B. Efflux-Mediated Antibiotic Resistance in Acinetobacter spp. Antimicrob. Agents Chemother. 2011, 55, 947–953. [Google Scholar] [CrossRef]
- Yoon, E.-J.; Chabane, Y.N.; Goussard, S.; Snesrud, E.; Courvalin, P.; Dé, E.; Grillot-Courvalin, C. Contribution of Resistance-Nodulation-Cell Division Efflux Systems to Antibiotic Resistance and Biofilm Formation in Acinetobacter Baumannii. MBio 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- Marchand, I.; Damier-Piolle, L.; Courvalin, P.; Lambert, T. Expression of the RND-Type Efflux Pump AdeABC in Acinetobacter Baumannii Is Regulated by the AdeRS Two-Component System. Antimicrob. Agents Chemother. 2004, 48, 3298–3304. [Google Scholar] [CrossRef]
- Damier-Piolle, L.; Magnet, S.; Brémont, S.; Lambert, T.; Courvalin, P. AdeIJK, a Resistance-Nodulation-Cell Division Pump Effluxing Multiple Antibiotics in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2008, 52, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Richmond, G.E.; Evans, L.P.; Anderson, M.J.; Wand, M.E.; Bonney, L.C.; Ivens, A.; Chua, K.L.; Webber, M.A.; Sutton, J.M.; Peterson, M.L.; et al. The Acinetobacter Baumannii Two-Component System AdeRS Regulates Genes Required for Multidrug Efflux, Biofilm Formation, and Virulence in a Strain-Specific Manner. MBio 2016, 7, e00430-16. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, N.; Bouchier, C.; Courvalin, P.; Périchon, B. Expression of the Resistance-Nodulation-Cell Division Pump AdeIJK in Acinetobacter Baumannii Is Regulated by AdeN, a TetR-Type Regulator. Antimicrob. Agents Chemother. 2012, 56, 2504–2510. [Google Scholar] [CrossRef]
- Coyne, S.; Rosenfeld, N.; Lambert, T.; Courvalin, P.; Périchon, B. Overexpression of Resistance-Nodulation-Cell Division Pump AdeFGH Confers Multidrug Resistance in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2010, 54, 4389–4393. [Google Scholar] [CrossRef]
- Su, X.-Z.; Chen, J.; Mizushima, T.; Kuroda, T.; Tsuchiya, T. AbeM, an H+-Coupled Acinetobacter Baumannii Multidrug Efflux Pump Belonging to the MATE Family of Transporters. Antimicrob. Agents Chemother. 2005, 49, 4362–4364. [Google Scholar] [CrossRef]
- Hou, P.F.; Chen, X.Y.; Yan, G.F.; Wang, Y.P.; Ying, C.M. Study of the Correlation of Imipenem Resistance with Efflux Pumps AdeABC, AdeIJK, AdeDE and AbeM in Clinical Isolates of Acinetobacter Baumannii. Chemotherapy 2012, 58, 152–158. [Google Scholar] [CrossRef]
- Rumbo, C.; Gato, E.; López, M.; Ruiz de Alegría, C.; Fernández-Cuenca, F.; Martínez-Martínez, L.; Vila, J.; Pachón, J.; Cisneros, J.M.; Rodríguez-Baño, J.; et al. Contribution of Efflux Pumps, Porins, and β-Lactamases to Multidrug Resistance in Clinical Isolates of Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2013, 57, 5247–5257. [Google Scholar] [CrossRef]
- Roca, I.; Marti, S.; Espinal, P.; Martínez, P.; Gibert, I.; Vila, J. CraA, a Major Facilitator Superfamily Efflux Pump Associated with Chloramphenicol Resistance in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2009, 53, 4013–4014. [Google Scholar] [CrossRef]
- Ribera, A.; Roca, I.; Ruiz, J.; Gibert, I.; Vila, J. Partial Characterization of a Transposon Containing the Tet(A) Determinant in a Clinical Isolate of Acinetobacter Baumannii. J. Antimicrob. Chemother. 2003, 52, 477–480. [Google Scholar] [CrossRef] [PubMed]
- Foong, W.E.; Wilhelm, J.; Tam, H.-K.; Pos, K.M. Tigecycline Efflux in Acinetobacter Baumannii Is Mediated by TetA in Synergy with RND-Type Efflux Transporters. J. Antimicrob. Chemother. 2020. [Google Scholar] [CrossRef] [PubMed]
- Rajamohan, G.; Srinivasan, V.B.; Gebreyes, W.A. Molecular and Functional Characterization of a Novel Efflux Pump, AmvA, Mediating Antimicrobial and Disinfectant Resistance in Acinetobacter Baumannii. J. Antimicrob. Chemother. 2010, 65, 1919–1925. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Sharma, R.; Bhattacharyya, T.; Bhando, T.; Pathania, R. Fosfomycin Resistance in Acinetobacter Baumannii Is Mediated by Efflux through a Major Facilitator Superfamily (MFS) Transporter-AbaF. J. Antimicrob. Chemother. 2017, 72, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Varela, M.; Corral, J.; Aranda, J.; Barbé, J. Functional Characterization of AbaQ, a Novel Efflux Pump Mediating Quinolone Resistance in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- Srinivasan, V.B.; Rajamohan, G.; Gebreyes, W.A. Role of AbeS, a Novel Efflux Pump of the SMR Family of Transporters, in Resistance to Antimicrobial Agents in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2009, 53, 5312–5316. [Google Scholar] [CrossRef]
- Lytvynenko, I.; Brill, S.; Oswald, C.; Pos, K.M. Molecular Basis of Polyspecificity of the Small Multidrug Resistance Efflux Pump AbeS from Acinetobacter Baumannii. J. Mol. Biol. 2016, 428, 644–657. [Google Scholar] [CrossRef]
- Lee, C.-R.; Lee, J.H.; Park, M.; Park, K.S.; Bae, I.K.; Kim, Y.B.; Cha, C.-J.; Jeong, B.C.; Lee, S.H. Biology of Acinetobacter Baumannii: Pathogenesis, Antibiotic Resistance Mechanisms, and Prospective Treatment Options. Front. Cell. Infect. Microbiol. 2017, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- Bou, G.; Cerveró, G.; Domínguez, M.A.; Quereda, C.; Martínez-Beltrán, J. Characterization of a Nosocomial Outbreak Caused by a Multiresistant Acinetobacter Baumannii Strain with a Carbapenem-Hydrolyzing Enzyme: High-Level Carbapenem Resistance in A. Baumannii Is Not Due Solely to the Presence of Beta-Lactamases. J. Clin. Microbiol. 2000, 38, 3299–3305. [Google Scholar] [CrossRef] [PubMed]
- Dupont, M.; Pagès, J.-M.; Lafitte, D.; Siroy, A.; Bollet, C. Identification of an OprD Homologue in Acinetobacter Baumannii. J. Proteome Res. 2005, 4, 2386–2390. [Google Scholar] [CrossRef] [PubMed]
- Quale, J.; Bratu, S.; Landman, D.; Heddurshetti, R. Molecular Epidemiology and Mechanisms of Carbapenem Resistance in Acinetobacter Baumannii Endemic in New York City. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2003, 37, 214–220. [Google Scholar] [CrossRef] [PubMed]
- del Mar Tomás, M.; Beceiro, A.; Pérez, A.; Velasco, D.; Moure, R.; Villanueva, R.; Martínez-Beltrán, J.; Bou, G. Cloning and Functional Analysis of the Gene Encoding the 33- to 36-Kilodalton Outer Membrane Protein Associated with Carbapenem Resistance in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2005, 49, 5172–5175. [Google Scholar] [CrossRef] [PubMed]
- Hood, M.I.; Jacobs, A.C.; Sayood, K.; Dunman, P.M.; Skaar, E.P. Acinetobacter Baumannii Increases Tolerance to Antibiotics in Response to Monovalent Cations. Antimicrob. Agents Chemother. 2010, 54, 1029–1041. [Google Scholar] [CrossRef] [PubMed]
- Mussi, M.A.; Limansky, A.S.; Viale, A.M. Acquisition of Resistance to Carbapenems in Multidrug-Resistant Clinical Strains of Acinetobacter Baumannii: Natural Insertional Inactivation of a Gene Encoding a Member of a Novel Family of Beta-Barrel Outer Membrane Proteins. Antimicrob. Agents Chemother. 2005, 49, 1432–1440. [Google Scholar] [CrossRef]
- Mussi, M.A.; Relling, V.M.; Limansky, A.S.; Viale, A.M. CarO, an Acinetobacter Baumannii Outer Membrane Protein Involved in Carbapenem Resistance, Is Essential for L-Ornithine Uptake. FEBS Lett. 2007, 581, 5573–5578. [Google Scholar] [CrossRef]
- Siroy, A.; Molle, V.; Lemaître-Guillier, C.; Vallenet, D.; Pestel-Caron, M.; Cozzone, A.J.; Jouenne, T.; Dé, E. Channel Formation by CarO, the Carbapenem Resistance-Associated Outer Membrane Protein of Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2005, 49, 4876–4883. [Google Scholar] [CrossRef]
- Catel-Ferreira, M.; Coadou, G.; Molle, V.; Mugnier, P.; Nordmann, P.; Siroy, A.; Jouenne, T.; Dé, E. Structure-Function Relationships of CarO, the Carbapenem Resistance-Associated Outer Membrane Protein of Acinetobacter Baumannii. J. Antimicrob. Chemother. 2011, 66, 2053–2056. [Google Scholar] [CrossRef]
- Jin, J.S.; Kwon, S.-O.; Moon, D.C.; Gurung, M.; Lee, J.H.; Kim, S.I.; Lee, J.C. Acinetobacter Baumannii Secretes Cytotoxic Outer Membrane Protein A via Outer Membrane Vesicles. PLoS ONE 2011, 6, e17027. [Google Scholar] [CrossRef]
- Smani, Y.; Fàbrega, A.; Roca, I.; Sánchez-Encinales, V.; Vila, J.; Pachón, J. Role of OmpA in the Multidrug Resistance Phenotype of Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2014, 58, 1806–1808. [Google Scholar] [CrossRef]
- Espinal, P.; Pantel, A.; Rolo, D.; Marti, S.; López-Rojas, R.; Smani, Y.; Pachón, J.; Vila, J.; Lavigne, J.-P. Relationship Between Different Resistance Mechanisms and Virulence in Acinetobacter Baumannii. Microb. Drug Resist. 2019, 25, 752–760. [Google Scholar] [CrossRef]
- Sánchez-Encinales, V.; Álvarez-Marín, R.; Pachón-Ibáñez, M.E.; Fernández-Cuenca, F.; Pascual, A.; Garnacho-Montero, J.; Martínez-Martínez, L.; Vila, J.; Tomás, M.M.; Cisneros, J.M.; et al. Overproduction of Outer Membrane Protein A by Acinetobacter Baumannii as a Risk Factor for Nosocomial Pneumonia, Bacteremia, and Mortality Rate Increase. J. Infect. Dis. 2017, 215, 966–974. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Unno, Y.; Kawakami, S.; Ubagai, T.; Ono, Y. Virulence Characteristics of Acinetobacter Baumannii Clinical Isolates Vary with the Expression Levels of Omps. J. Med. Microbiol. 2017, 66, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Eghbali, Z.; Mojtahedi, A.; Moien Ansar, M.; Fakhrieh Asl, S.; Aminian, K. Detection of 23SrRNA Mutations Strongly Related to Clarithromycin Resistance in Helicobacter Pylori Strains Isolated From Patients in the North of Iran. Jundishapur J. Microbiol. 2016, 9, e29694. [Google Scholar] [CrossRef] [PubMed]
- Gu, B.; Kelesidis, T.; Tsiodras, S.; Hindler, J.; Humphries, R.M. The Emerging Problem of Linezolid-Resistant Staphylococcus. J. Antimicrob. Chemother. 2013, 68, 4–11. [Google Scholar] [CrossRef]
- Campbell, E.A.; Korzheva, N.; Mustaev, A.; Murakami, K.; Nair, S.; Goldfarb, A.; Darst, S.A. Structural Mechanism for Rifampicin Inhibition of Bacterial Rna Polymerase. Cell 2001, 104, 901–912. [Google Scholar] [CrossRef]
- Floss, H.G.; Yu, T.-W. Rifamycin-Mode of Action, Resistance, and Biosynthesis. Chem. Rev. 2005, 105, 621–632. [Google Scholar] [CrossRef]
- Park, S.; Lee, K.M.; Yoo, Y.S.; Yoo, J.S.; Yoo, J.I.; Kim, H.S.; Lee, Y.S.; Chung, G.T. Alterations of GyrA, GyrB, and ParC and Activity of Efflux Pump in Fluoroquinolone-Resistant Acinetobacter Baumannii. Osong Public Health Res. Perspect. 2011, 2, 164–170. [Google Scholar] [CrossRef]
- Ardebili, A.; Lari, A.R.; Beheshti, M.; Lari, E.R. Association between Mutations in GyrA and ParC Genes of Acinetobacter Baumannii Clinical Isolates and Ciprofloxacin Resistance. Iran. J. Basic Med. Sci. 2015, 18, 623–626. [Google Scholar]
- Hamed, S.M.; Elkhatib, W.F.; El-Mahallawy, H.A.; Helmy, M.M.; Ashour, M.S.; Aboshanab, K.M.A. Multiple Mechanisms Contributing to Ciprofloxacin Resistance among Gram Negative Bacteria Causing Infections to Cancer Patients. Sci. Rep. 2018, 8, 12268. [Google Scholar] [CrossRef]
- Hooper, D.C. Fluoroquinolone Resistance among Gram-Positive Cocci. Lancet Infect. Dis. 2002, 2, 530–538. [Google Scholar] [CrossRef]
- Schmitz, F.J.; Hofmann, B.; Hansen, B.; Scheuring, S.; Lückefahr, M.; Klootwijk, M.; Verhoef, J.; Fluit, A.; Heinz, H.P.; Köhrer, K.; et al. Relationship between Ciprofloxacin, Ofloxacin, Levofloxacin, Sparfloxacin and Moxifloxacin (BAY 12-8039) MICs and Mutations in GrlA, GrlB, GyrA and GyrB in 116 Unrelated Clinical Isolates of Staphylococcus Aureus. J. Antimicrob. Chemother. 1998, 41, 481–484. [Google Scholar] [CrossRef] [PubMed]
- Albornoz, E.; Tijet, N.; De Belder, D.; Gomez, S.; Martino, F.; Corso, A.; Melano, R.G.; Petroni, A. QnrE1, a Member of a New Family of Plasmid-Located Quinolone Resistance Genes, Originated from the Chromosome of Enterobacter Species. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Robicsek, A.; Strahilevitz, J.; Jacoby, G.A.; Macielag, M.; Abbanat, D.; Park, C.H.; Bush, K.; Hooper, D.C. Fluoroquinolone-Modifying Enzyme: A New Adaptation of a Common Aminoglycoside Acetyltransferase. Nat. Med. 2006, 12, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Zavascki, A.P.; Goldani, L.Z.; Li, J.; Nation, R.L. Polymyxin B for the Treatment of Multidrug-Resistant Pathogens: A Critical Review. J. Antimicrob. Chemother. 2007, 60, 1206–1215. [Google Scholar] [CrossRef] [PubMed]
- Reed, M.D.; Stern, R.C.; O’Riordan, M.A.; Blumer, J.L. The Pharmacokinetics of Colistin in Patients with Cystic Fibrosis. J. Clin. Pharmacol. 2001, 41, 645–654. [Google Scholar] [CrossRef] [PubMed]
- Bialvaei, A.Z.; Samadi Kafil, H. Colistin, Mechanisms and Prevalence of Resistance. Curr. Med. Res. Opin. 2015, 31, 707–721. [Google Scholar] [CrossRef]
- Hejnar, P.; Kolár, M.; Hájek, V. Characteristics of Acinetobacter Strains (Phenotype Classification, Antibiotic Susceptibility and Production of Beta-Lactamases) Isolated from Haemocultures from Patients at the Teaching Hospital in Olomouc. Acta Univ. Palacki. Olomuc. Fac. Med. 1999, 142, 73–77. [Google Scholar]
- Adams, M.D.; Nickel, G.C.; Bajaksouzian, S.; Lavender, H.; Murthy, A.R.; Jacobs, M.R.; Bonomo, R.A. Resistance to Colistin in Acinetobacter Baumannii Associated with Mutations in the PmrAB Two-Component System. Antimicrob. Agents Chemother. 2009, 53, 3628–3634. [Google Scholar] [CrossRef]
- Chin, C.-Y.; Gregg, K.A.; Napier, B.A.; Ernst, R.K.; Weiss, D.S. A PmrB-Regulated Deacetylase Required for Lipid A Modification and Polymyxin Resistance in Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2015, 59, 7911–7914. [Google Scholar] [CrossRef]
- Koomanachai, P.; Kim, A.; Nicolau, D.P. Pharmacodynamic Evaluation of Tigecycline against Acinetobacter Baumannii in a Murine Pneumonia Model. J. Antimicrob. Chemother. 2009, 63, 982–987. [Google Scholar] [CrossRef]
- Castanheira, M.; Mendes, R.E.; Jones, R.N. Update on Acinetobacter Species: Mechanisms of Antimicrobial Resistance and Contemporary in Vitro Activity of Minocycline and Other Treatment Options. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2014, 59 (Suppl. 6), S367–S373. [Google Scholar] [CrossRef] [PubMed]
- Peck, K.R.; Kim, M.J.; Choi, J.Y.; Kim, H.S.; Kang, C.-I.; Cho, Y.K.; Park, D.W.; Lee, H.J.; Lee, M.S.; Ko, K.S. In Vitro Time-Kill Studies of Antimicrobial Agents against Blood Isolates of Imipenem-Resistant Acinetobacter Baumannii, Including Colistin- or Tigecycline-Resistant Isolates. J. Med. Microbiol. 2012, 61, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Aydemir, H.; Akduman, D.; Piskin, N.; Comert, F.; Horuz, E.; Terzi, A.; Kokturk, F.; Ornek, T.; Celebi, G. Colistin vs. the Combination of Colistin and Rifampicin for the Treatment of Carbapenem-Resistant Acinetobacter Baumannii Ventilator-Associated Pneumonia. Epidemiol. Infect. 2013, 141, 1214–1222. [Google Scholar] [CrossRef] [PubMed]
- Menegucci, T.C.; Fedrigo, N.H.; Lodi, F.G.; Albiero, J.; Nishiyama, S.A.B.; Mazucheli, J.; Carrara-Marroni, F.E.; Voelkner, N.M.F.; Gong, H.; Sy, S.K.B.; et al. Pharmacodynamic Effects of Sulbactam/Meropenem/Polymyxin-B Combination Against Extremely Drug Resistant Acinetobacter Baumannii Using Checkerboard Information. Microb. Drug Resist. 2019, 25, 1266–1274. [Google Scholar] [CrossRef]
- Mansour, S.C.; Pena, O.M.; Hancock, R.E.W. Host Defense Peptides: Front-Line Immunomodulators. Trends Immunol. 2014, 35, 443–450. [Google Scholar] [CrossRef]
- Falanga, A.; Lombardi, L.; Franci, G.; Vitiello, M.; Iovene, M.R.; Morelli, G.; Galdiero, M.; Galdiero, S. Marine Antimicrobial Peptides: Nature Provides Templates for the Design of Novel Compounds against Pathogenic Bacteria. Int. J. Mol. Sci. 2016, 17, 785. [Google Scholar] [CrossRef]
- Fan, L.; Sun, J.; Zhou, M.; Zhou, J.; Lao, X.; Zheng, H.; Xu, H. DRAMP: A Comprehensive Data Repository of Antimicrobial Peptides. Sci. Rep. 2016, 6, 24482. [Google Scholar] [CrossRef]
- Kumar, P.; Kizhakkedathu, J.N.; Straus, S.K. Antimicrobial Peptides: Diversity, Mechanism of Action and Strategies to Improve the Activity and Biocompatibility In Vivo. Biomolecules 2018, 8, 4. [Google Scholar] [CrossRef]
- Govender, T.; Dawood, A.; Esterhuyse, A.J.; Katerere, D.R. Antimicrobial Properties of the Skin Secretions of Frogs. S. Afr. J. Sci. 2012, 108, 25–30. [Google Scholar] [CrossRef][Green Version]
- Kościuczuk, E.M.; Lisowski, P.; Jarczak, J.; Strzałkowska, N.; Jóźwik, A.; Horbańczuk, J.; Krzyżewski, J.; Zwierzchowski, L.; Bagnicka, E. Cathelicidins: Family of Antimicrobial Peptides. A Review. Mol. Biol. Rep. 2012, 39, 10957–10970. [Google Scholar] [CrossRef]
- Zhao, F.; Lan, X.-Q.; Du, Y.; Chen, P.-Y.; Zhao, J.; Zhao, F.; Lee, W.-H.; Zhang, Y. King Cobra Peptide OH-CATH30 as a Potential Candidate Drug through Clinic Drug-Resistant Isolates. Zool. Res. 2018, 39, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Dekan, Z.; Headey, S.J.; Scanlon, M.; Baldo, B.A.; Lee, T.-H.; Aguilar, M.-I.; Deuis, J.R.; Vetter, I.; Elliott, A.G.; Amado, M.; et al. Δ-Myrtoxin-Mp1a Is a Helical Heterodimer from the Venom of the Jack Jumper Ant That Has Antimicrobial, Membrane-Disrupting, and Nociceptive Activities. Angew. Chem. Int. Ed. Engl. 2017, 56, 8495–8499. [Google Scholar] [CrossRef] [PubMed]
- Mwangi, J.; Yin, Y.; Wang, G.; Yang, M.; Li, Y.; Zhang, Z.; Lai, R. The Antimicrobial Peptide ZY4 Combats Multidrug-Resistant Pseudomonas Aeruginosa and Acinetobacter Baumannii Infection. Proc. Natl. Acad. Sci. USA 2019, 116, 26516–26522. [Google Scholar] [CrossRef] [PubMed]
- Tajbakhsh, M.; Akhavan, M.M.; Fallah, F.; Karimi, A. A Recombinant Snake Cathelicidin Derivative Peptide: Antibiofilm Properties and Expression in Escherichia Coli. Biomolecules 2018, 8, 118. [Google Scholar] [CrossRef]
- Al-Asmari, A.K.; Alamri, M.A.; Almasoudi, A.S.; Abbasmanthiri, R.; Mahfoud, M. Evaluation of the in Vitro Antimicrobial Activity of Selected Saudi Scorpion Venoms Tested against Multidrug-Resistant Micro-Organisms. J. Glob. Antimicrob. Resist. 2017, 10, 14–18. [Google Scholar] [CrossRef]
- Lin, C.-H.; Lee, M.-C.; Tzen, J.T.C.; Lee, H.-M.; Chang, S.-M.; Tu, W.-C.; Lin, C.-F. Efficacy of Mastoparan-AF Alone and in Combination with Clinically Used Antibiotics on Nosocomial Multidrug-Resistant Acinetobacter Baumannii. Saudi J. Biol. Sci. 2017, 24, 1023–1029. [Google Scholar] [CrossRef]
- Shamova, O.V.; Orlov, D.S.; Zharkova, M.S.; Balandin, S.V.; Yamschikova, E.V.; Knappe, D.; Hoffmann, R.; Kokryakov, V.N.; Ovchinnikova, T.V. Minibactenecins ChBac7.Nα and ChBac7. Nβ—Antimicrobial Peptides from Leukocytes of the Goat Capra Hircus. Acta Nat. 2016, 8, 136–146. [Google Scholar] [CrossRef]
- Hirsch, R.; Wiesner, J.; Marker, A.; Pfeifer, Y.; Bauer, A.; Hammann, P.E.; Vilcinskas, A. Profiling Antimicrobial Peptides from the Medical Maggot Lucilia Sericata as Potential Antibiotics for MDR Gram-Negative Bacteria. J. Antimicrob. Chemother. 2019, 74, 96–107. [Google Scholar] [CrossRef]
- Domhan, C.; Uhl, P.; Kleist, C.; Zimmermann, S.; Umstätter, F.; Leotta, K.; Mier, W.; Wink, M. Replacement of L-Amino Acids by d-Amino Acids in the Antimicrobial Peptide Ranalexin and Its Consequences for Antimicrobial Activity and Biodistribution. Molecules 2019, 24, 2987. [Google Scholar] [CrossRef]
- Jaśkiewicz, M.; Neubauer, D.; Kazor, K.; Bartoszewska, S.; Kamysz, W. Antimicrobial Activity of Selected Antimicrobial Peptides Against Planktonic Culture and Biofilm of Acinetobacter Baumannii. Probiotics Antimicrob. Proteins 2019, 11, 317–324. [Google Scholar] [CrossRef]
- Peng, J.; Long, H.; Liu, W.; Wu, Z.; Wang, T.; Zeng, Z.; Guo, G.; Wu, J. Antibacterial Mechanism of Peptide Cec4 against Acinetobacter Baumannii. Infect. Drug Resist. 2019, 12, 2417–2428. [Google Scholar] [CrossRef] [PubMed]
- Han, H.M.; Ko, S.; Cheong, M.-J.; Bang, J.K.; Seo, C.H.; Luchian, T.; Park, Y. Myxinidin2 and Myxinidin3 Suppress Inflammatory Responses through STAT3 and MAPKs to Promote Wound Healing. Oncotarget 2017, 8, 87582–87597. [Google Scholar] [CrossRef] [PubMed]
- Gordya, N.; Yakovlev, A.; Kruglikova, A.; Tulin, D.; Potolitsina, E.; Suborova, T.; Bordo, D.; Rosano, C.; Chernysh, S. Natural Antimicrobial Peptide Complexes in the Fighting of Antibiotic Resistant Biofilms: Calliphora Vicina Medicinal Maggots. PLoS ONE 2017, 12, e0173559. [Google Scholar] [CrossRef] [PubMed]
- Mourtada, R.; Herce, H.D.; Yin, D.J.; Moroco, J.A.; Wales, T.E.; Engen, J.R.; Walensky, L.D. Design of Stapled Antimicrobial Peptides That Are Stable, Nontoxic and Kill Antibiotic-Resistant Bacteria in Mice. Nat. Biotechnol. 2019, 37, 1186–1197. [Google Scholar] [CrossRef] [PubMed]
- Rose, M.; Lapuebla, A.; Landman, D.; Quale, J. In Vitro and In Vivo Activity of a Novel Antisense Peptide Nucleic Acid Compound Against Multidrug-Resistant Acinetobacter Baumannii. Microb. Drug Resist. 2019, 25, 961–965. [Google Scholar] [CrossRef]
- Dathe, M.; Wieprecht, T. Structural Features of Helical Antimicrobial Peptides: Their Potential to Modulate Activity on Model Membranes and Biological Cells. Biochim. Biophys. Acta 1999, 1462, 71–87. [Google Scholar] [CrossRef]
- Starr, C.G.; Wimley, W.C. Antimicrobial Peptides Are Degraded by the Cytosolic Proteases of Human Erythrocytes. Biochim. Biophys. Acta Biomembr. 2017, 1859, 2319–2326. [Google Scholar] [CrossRef]
- McPhee, J.B.; Hancock, R.E.W. Function and Therapeutic Potential of Host Defence Peptides. J. Pept. Sci. 2005, 11, 677–687. [Google Scholar] [CrossRef]
- Cantisani, M.; Finamore, E.; Mignogna, E.; Falanga, A.; Nicoletti, G.F.; Pedone, C.; Morelli, G.; Leone, M.; Galdiero, M.; Galdiero, S. Structural Insights into and Activity Analysis of the Antimicrobial Peptide Myxinidin. Antimicrob. Agents Chemother. 2014, 58, 5280–5290. [Google Scholar] [CrossRef]
- Kim, H.; Jang, J.H.; Kim, S.C.; Cho, J.H. De Novo Generation of Short Antimicrobial Peptides with Enhanced Stability and Cell Specificity. J. Antimicrob. Chemother. 2014, 69, 121–132. [Google Scholar] [CrossRef]
- Andersson, D.I.; Hughes, D.; Kubicek-Sutherland, J.Z. Mechanisms and Consequences of Bacterial Resistance to Antimicrobial Peptides. Drug Resist. Update Rev. Comment. Antimicrob. Anticancer Chemother. 2016, 26, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Xu, M.; Wang, T.; You, C.; Wang, X.; Ren, H.; Zhou, H.; Khan, A.; Han, C.; Li, P. Catechol Cross-Linked Antimicrobial Peptide Hydrogels Prevent Multidrug-Resistant Acinetobacter Baumannii Infection in Burn Wounds. Biosci. Rep. 2019, 39. [Google Scholar] [CrossRef] [PubMed]
- Ostorhazi, E.; Hoffmann, R.; Herth, N.; Wade, J.D.; Kraus, C.N.; Otvos, L.J. Advantage of a Narrow Spectrum Host Defense (Antimicrobial) Peptide Over a Broad Spectrum Analog in Preclinical Drug Development. Front. Chem. 2018, 6, 359. [Google Scholar] [CrossRef] [PubMed]
- Mant, C.T.; Jiang, Z.; Gera, L.; Davis, T.; Nelson, K.L.; Bevers, S.; Hodges, R.S. De Novo Designed Amphipathic α-Helical Antimicrobial Peptides Incorporating Dab and Dap Residues on the Polar Face To Treat the Gram-Negative Pathogen, Acinetobacter Baumannii. J. Med. Chem. 2019, 62, 3354–3366. [Google Scholar] [CrossRef] [PubMed]
- Tejman-Yarden, N.; Robinson, A.; Davidov, Y.; Shulman, A.; Varvak, A.; Reyes, F.; Rahav, G.; Nissan, I. Delftibactin-A, a Non-Ribosomal Peptide With Broad Antimicrobial Activity. Front. Microbiol. 2019, 10, 2377. [Google Scholar] [CrossRef] [PubMed]
- Taheri, B.; Mohammadi, M.; Momenzadeh, N.; Farshadzadeh, Z.; Roozbehani, M.; Dehghani, P.; Hajian, S.; Darvishi, S.; Shamseddin, J. Substitution of Lysine for Isoleucine at the Center of the Nonpolar Face of the Antimicrobial Peptide, Piscidin-1, Leads to an Increase in the Rapidity of Bactericidal Activity and a Reduction in Toxicity. Infect. Drug Resist. 2019, 12, 1629–1647. [Google Scholar] [CrossRef] [PubMed]
- Nagarajan, D.; Roy, N.; Kulkarni, O.; Nanajkar, N.; Datey, A.; Ravichandran, S.; Thakur, C.; Sandeep, T.; Aprameya, I.V.; Sarma, S.P.; et al. Ω76: A Designed Antimicrobial Peptide to Combat Carbapenem- and Tigecycline-Resistant Acinetobacter Baumannii. Sci. Adv. 2019, 5, eaax1946. [Google Scholar] [CrossRef]
- Hacioglu, M.; Oyardi, O.; Bozkurt-Guzel, C.; Savage, P.B. Antibiofilm Activities of Ceragenins and Antimicrobial Peptides against Fungal-Bacterial Mono and Multispecies Biofilms. J. Antibiot. 2020. [Google Scholar] [CrossRef]
- Jenei, S.; Tiricz, H.; Szolomájer, J.; Tímár, E.; Klement, É.; Al Bouni, M.A.; Lima, R.M.; Kata, D.; Harmati, M.; Buzás, K.; et al. Potent Chimeric Antimicrobial Derivatives of the Medicago Truncatula NCR247 Symbiotic Peptide. Front. Microbiol. 2020, 11, 270. [Google Scholar] [CrossRef]
- Heulot, M.; Jacquier, N.; Aeby, S.; Le Roy, D.; Roger, T.; Trofimenko, E.; Barras, D.; Greub, G.; Widmann, C. The Anticancer Peptide TAT-RasGAP(317-326) Exerts Broad Antimicrobial Activity. Front. Microbiol. 2017, 8, 994. [Google Scholar] [CrossRef]
- Swedan, S.; Shubair, Z.; Almaaytah, A. Synergism of Cationic Antimicrobial Peptide WLBU2 with Antibacterial Agents against Biofilms of Multi-Drug Resistant Acinetobacter Baumannii and Klebsiella Pneumoniae. Infect. Drug Resist. 2019, 12, 2019–2030. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-L.; Su, P.-Y.; Kuo, S.-C.; Lauderdale, T.-L.Y.; Shih, C. Adding a C-Terminal Cysteine (CTC) Can Enhance the Bactericidal Activity of Three Different Antimicrobial Peptides. Front. Microbiol. 2018, 9, 1440. [Google Scholar] [CrossRef] [PubMed]
- Mohan, N.M.; Zorgani, A.; Jalowicki, G.; Kerr, A.; Khaldi, N.; Martins, M. Unlocking NuriPep 1653 From Common Pea Protein: A Potent Antimicrobial Peptide to Tackle a Pan-Drug Resistant Acinetobacter Baumannii. Front. Microbiol. 2019, 10, 2086. [Google Scholar] [CrossRef] [PubMed]
- Kaushal, A.; Gupta, K.; van Hoek, M.L. Characterization of Cimex Lectularius (Bedbug) Defensin Peptide and Its Antimicrobial Activity against Human Skin Microflora. Biochem. Biophys. Res. Commun. 2016, 470, 955–960. [Google Scholar] [CrossRef][Green Version]
- Christiansen, S.H.; Murphy, R.A.; Juul-Madsen, K.; Fredborg, M.; Hvam, M.L.; Axelgaard, E.; Skovdal, S.M.; Meyer, R.L.; Sørensen, U.B.S.; Möller, A.; et al. The Immunomodulatory Drug Glatiramer Acetate Is Also an Effective Antimicrobial Agent That Kills Gram-Negative Bacteria. Sci. Rep. 2017, 7, 15653. [Google Scholar] [CrossRef]
- Kirkpatrick, C.L.; Broberg, C.A.; McCool, E.N.; Lee, W.J.; Chao, A.; McConnell, E.W.; Pritchard, D.A.; Hebert, M.; Fleeman, R.; Adams, J.; et al. The “PepSAVI-MS” Pipeline for Natural Product Bioactive Peptide Discovery. Anal. Chem. 2017, 89, 1194–1201. [Google Scholar] [CrossRef]
- Defraine, V.; Schuermans, J.; Grymonprez, B.; Govers, S.K.; Aertsen, A.; Fauvart, M.; Michiels, J.; Lavigne, R.; Briers, Y. Efficacy of Artilysin Art-175 against Resistant and Persistent Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2016, 60, 3480–3488. [Google Scholar] [CrossRef]
- Mahdi, L.; Mahdi, N.; Al-Kakei, S.; Musafer, H.; Al-Joofy, I.; Essa, R.; Zwain, L.; Salman, I.; Mater, H.; Al-Alak, S.; et al. Treatment Strategy by Lactoperoxidase and Lactoferrin Combination: Immunomodulatory and Antibacterial Activity against Multidrug-Resistant Acinetobacter Baumannii. Microb. Pathog. 2018, 114, 147–152. [Google Scholar] [CrossRef]
- Morroni, G.; Simonetti, O.; Brenciani, A.; Brescini, L.; Kamysz, W.; Kamysz, E.; Neubauer, D.; Caffarini, M.; Orciani, M.; Giovanetti, E.; et al. In Vitro Activity of Protegrin-1, Alone and in Combination with Clinically Useful Antibiotics, against Acinetobacter Baumannii Strains Isolated from Surgical Wounds. Med. Microbiol. Immunol. 2019, 208, 877–883. [Google Scholar] [CrossRef]
- Vrancianu, C.O.; Popa, L.I.; Bleotu, C.; Chifiriuc, M.C. Targeting Plasmids to Limit Acquisition and Transmission of Antimicrobial Resistance. Front. Microbiol. 2020, 11, 761. [Google Scholar] [CrossRef]
- Harada, L.K.; Silva, E.C.; Campos, W.F.; Del Fiol, F.S.; Vila, M.; Dąbrowska, K.; Krylov, V.N.; Balcão, V.M. Biotechnological Applications of Bacteriophages: State of the Art. Microbiol. Res. 2018, 212–213, 38–58. [Google Scholar] [CrossRef] [PubMed]
- Buckling, A.; Rainey, P.B. Antagonistic Coevolution between a Bacterium and a Bacteriophage. Proc. Biol. Sci. 2002, 269, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.M.; Koskella, B.; Lin, H.C. Phage Therapy: An Alternative to Antibiotics in the Age of Multi-Drug Resistance. World J. Gastrointest. Pharmacol. Ther. 2017, 8, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Sulakvelidze, A.; Alavidze, Z.; Morris, J.G.J. Bacteriophage Therapy. Antimicrob. Agents Chemother. 2001, 45, 649–659. [Google Scholar] [CrossRef]
- Clark, J.R.; March, J.B. Bacteriophages and Biotechnology: Vaccines, Gene Therapy and Antibacterials. Trends Biotechnol. 2006, 24, 212–218. [Google Scholar] [CrossRef]
- Międzybrodzki, R.; Borysowski, J.; Weber-Dąbrowska, B.; Fortuna, W.; Letkiewicz, S.; Szufnarowski, K.; Pawełczyk, Z.; Rogóż, P.; Kłak, M.; Wojtasik, E.; et al. Clinical Aspects of Phage Therapy. Adv. Virus Res. 2012, 83, 73–121. [Google Scholar] [CrossRef]
- Shen, G.-H.; Wang, J.-L.; Wen, F.-S.; Chang, K.-M.; Kuo, C.-F.; Lin, C.-H.; Luo, H.-R.; Hung, C.-H. Isolation and Characterization of Φkm18p, a Novel Lytic Phage with Therapeutic Potential against Extensively Drug Resistant Acinetobacter Baumannii. PLoS ONE 2012, 7, e46537. [Google Scholar] [CrossRef]
- Merabishvili, M.; Vandenheuvel, D.; Kropinski, A.M.; Mast, J.; De Vos, D.; Verbeken, G.; Noben, J.-P.; Lavigne, R.; Vaneechoutte, M.; Pirnay, J.-P. Characterization of Newly Isolated Lytic Bacteriophages Active against Acinetobacter Baumannii. PLoS ONE 2014, 9, e104853. [Google Scholar] [CrossRef]
- Ghajavand, H.; Esfahani, B.N.; Havaei, A.; Fazeli, H.; Jafari, R.; Moghim, S. Isolation of Bacteriophages against Multidrug Resistant Acinetobacter Baumannii. Res. Pharm. Sci. 2017, 12, 373–380. [Google Scholar] [CrossRef]
- Turner, D.; Wand, M.E.; Briers, Y.; Lavigne, R.; Sutton, J.M.; Reynolds, D.M. Characterisation and Genome Sequence of the Lytic Acinetobacter Baumannii Bacteriophage VB_AbaS_Loki. PLoS ONE 2017, 12, e0172303. [Google Scholar] [CrossRef]
- Hernandez-Morales, A.C.; Lessor, L.L.; Wood, T.L.; Migl, D.; Mijalis, E.M.; Cahill, J.; Russell, W.K.; Young, R.F.; Gill, J.J. Genomic and Biochemical Characterization of Acinetobacter Podophage Petty Reveals a Novel Lysis Mechanism and Tail-Associated Depolymerase Activity. J. Virol. 2018, 92. [Google Scholar] [CrossRef] [PubMed]
- Hua, Y.; Luo, T.; Yang, Y.; Dong, D.; Wang, R.; Wang, Y.; Xu, M.; Guo, X.; Hu, F.; He, P. Phage Therapy as a Promising New Treatment for Lung Infection Caused by Carbapenem-Resistant Acinetobacter Baumannii in Mice. Front. Microbiol. 2017, 8, 2659. [Google Scholar] [CrossRef] [PubMed]
- Kusradze, I.; Karumidze, N.; Rigvava, S.; Dvalidze, T.; Katsitadze, M.; Amiranashvili, I.; Goderdzishvili, M. Characterization and Testing the Efficiency of Acinetobacter Baumannii Phage VB-GEC_Ab-M-G7 as an Antibacterial Agent. Front. Microbiol. 2016, 7, 1590. [Google Scholar] [CrossRef] [PubMed]
- Yin, S.; Huang, G.; Zhang, Y.; Jiang, B.; Yang, Z.; Dong, Z.; You, B.; Yuan, Z.; Hu, F.; Zhao, Y.; et al. Phage Abp1 Rescues Human Cells and Mice from Infection by Pan-Drug Resistant Acinetobacter Baumannii. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2017, 44, 2337–2345. [Google Scholar] [CrossRef]
- Cha, K.; Oh, H.K.; Jang, J.Y.; Jo, Y.; Kim, W.K.; Ha, G.U.; Ko, K.S.; Myung, H. Characterization of Two Novel Bacteriophages Infecting Multidrug-Resistant (MDR) Acinetobacter Baumannii and Evaluation of Their Therapeutic Efficacy in Vivo. Front. Microbiol. 2018, 9, 696. [Google Scholar] [CrossRef]
- Zhou, W.; Feng, Y.; Zong, Z. Two New Lytic Bacteriophages of the Myoviridae Family Against Carbapenem-Resistant Acinetobacter Baumannii. Front. Microbiol. 2018, 9, 850. [Google Scholar] [CrossRef]
- Wu, M.; Hu, K.; Xie, Y.; Liu, Y.; Mu, D.; Guo, H.; Zhang, Z.; Zhang, Y.; Chang, D.; Shi, Y. A Novel Phage PD-6A3, and Its Endolysin Ply6A3, With Extended Lytic Activity Against Acinetobacter Baumannii. Front. Microbiol. 2018, 9, 3302. [Google Scholar] [CrossRef]
- Jeon, J.; Park, J.-H.; Yong, D. Efficacy of Bacteriophage Treatment against Carbapenem-Resistant Acinetobacter Baumannii in Galleria Mellonella Larvae and a Mouse Model of Acute Pneumonia. BMC Microbiol. 2019, 19, 70. [Google Scholar] [CrossRef]
- Jasim, H.N.; Hafidh, R.R.; Abdulamir, A.S. Formation of Therapeutic Phage Cocktail and Endolysin to Highly Multi-Drug Resistant Acinetobacter Baumannii: In Vitro and in Vivo Study. Iran. J. Basic Med. Sci. 2018, 21, 1100–1108. [Google Scholar] [CrossRef]
- WC, S. Bacteriophage:Early Research. In Bacteriophage: Biology and Applications; CRC Press: Boca Raton, FL, USA, 2005; p. 510. [Google Scholar]
- Abedon, S.T.; Kuhl, S.J.; Blasdel, B.G.; Kutter, E.M. Phage Treatment of Human Infections. Bacteriophage 2011, 1, 66–85. [Google Scholar] [CrossRef]
- Ventola, C.L. The Antibiotic Resistance Crisis: Part 1: Causes and Threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Kumarasamy, K.K.; Toleman, M.A.; Walsh, T.R.; Bagaria, J.; Butt, F.; Balakrishnan, R.; Chaudhary, U.; Doumith, M.; Giske, C.G.; Irfan, S.; et al. Emergence of a New Antibiotic Resistance Mechanism in India, Pakistan, and the UK: A Molecular, Biological, and Epidemiological Study. Lancet Infect. Dis. 2010, 10, 597–602. [Google Scholar] [CrossRef]
- Schooley, R.T.; Biswas, B.; Gill, J.J.; Hernandez-Morales, A.; Lancaster, J.; Lessor, L.; Barr, J.J.; Reed, S.L.; Rohwer, F.; Benler, S.; et al. Development and Use of Personalized Bacteriophage-Based Therapeutic Cocktails To Treat a Patient with a Disseminated Resistant Acinetobacter Baumannii Infection. Antimicrob. Agents Chemother. 2017, 61. [Google Scholar] [CrossRef] [PubMed]
- Sarker, S.A.; Sultana, S.; Reuteler, G.; Moine, D.; Descombes, P.; Charton, F.; Bourdin, G.; McCallin, S.; Ngom-Bru, C.; Neville, T.; et al. Oral Phage Therapy of Acute Bacterial Diarrhea With Two Coliphage Preparations: A Randomized Trial in Children From Bangladesh. EBioMedicine 2016, 4, 124–137. [Google Scholar] [CrossRef]
- Jault, P.; Leclerc, T.; Jennes, S.; Pirnay, J.P.; Que, Y.-A.; Resch, G.; Rousseau, A.F.; Ravat, F.; Carsin, H.; Le Floch, R.; et al. Efficacy and Tolerability of a Cocktail of Bacteriophages to Treat Burn Wounds Infected by Pseudomonas Aeruginosa (PhagoBurn): A Randomised, Controlled, Double-Blind Phase 1/2 Trial. Lancet Infect. Dis. 2019, 19, 35–45. [Google Scholar] [CrossRef]
- Azam, A.H.; Tanji, Y. Bacteriophage-Host Arm Race: An Update on the Mechanism of Phage Resistance in Bacteria and Revenge of the Phage with the Perspective for Phage Therapy. Appl. Microbiol. Biotechnol. 2019, 103, 2121–2131. [Google Scholar] [CrossRef]
- Taylor, V.L.; Fitzpatrick, A.D.; Islam, Z.; Maxwell, K.L. The Diverse Impacts of Phage Morons on Bacterial Fitness and Virulence. Adv. Virus Res. 2019, 103, 1–31. [Google Scholar] [CrossRef]
- Yuan, Y.; Wang, L.; Li, X.; Tan, D.; Cong, C.; Xu, Y. Efficacy of a Phage Cocktail in Controlling Phage Resistance Development in Multidrug Resistant Acinetobacter Baumannii. Virus Res. 2019, 272, 197734. [Google Scholar] [CrossRef]
- Chadha, P.; Katare, O.P.; Chhibber, S. In Vivo Efficacy of Single Phage versus Phage Cocktail in Resolving Burn Wound Infection in BALB/c Mice. Microb. Pathog. 2016, 99, 68–77. [Google Scholar] [CrossRef]
- Sneppen, K.; Semsey, S.; Seshasayee, A.S.N.; Krishna, S. Restriction Modification Systems as Engines of Diversity. Front. Microbiol. 2015, 6, 528. [Google Scholar] [CrossRef]
- Van Belleghem, J.D.; Dąbrowska, K.; Vaneechoutte, M.; Barr, J.J.; Bollyky, P.L. Interactions between Bacteriophage, Bacteria, and the Mammalian Immune System. Viruses 2018, 11, 10. [Google Scholar] [CrossRef]
- Kumaran, D.; Taha, M.; Yi, Q.; Ramirez-Arcos, S.; Diallo, J.-S.; Carli, A.; Abdelbary, H. Does Treatment Order Matter? Investigating the Ability of Bacteriophage to Augment Antibiotic Activity against Staphylococcus Aureus Biofilms. Front. Microbiol. 2018, 9, 127. [Google Scholar] [CrossRef]
- Ishino, Y.; Shinagawa, H.; Makino, K.; Amemura, M.; Nakata, A. Nucleotide Sequence of the Iap Gene, Responsible for Alkaline Phosphatase Isozyme Conversion in Escherichia Coli, and Identification of the Gene Product. J. Bacteriol. 1987, 169, 5429–5433. [Google Scholar] [CrossRef]
- Li, H.-Y.; Kao, C.-Y.; Lin, W.-H.; Zheng, P.-X.; Yan, J.-J.; Wang, M.-C.; Teng, C.-H.; Tseng, C.-C.; Wu, J.-J. Characterization of CRISPR-Cas Systems in Clinical Klebsiella Pneumoniae Isolates Uncovers Its Potential Association With Antibiotic Susceptibility. Front. Microbiol. 2018, 9, 1595. [Google Scholar] [CrossRef] [PubMed]
- Crawley, A.B.; Henriksen, E.D.; Stout, E.; Brandt, K.; Barrangou, R. Characterizing the Activity of Abundant, Diverse and Active CRISPR-Cas Systems in Lactobacilli. Sci. Rep. 2018, 8, 11544. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, A.; Shi, Y.; Kage-Nakadai, E.; Mitani, S.; Xue, D. Caspase-Dependent Conversion of Dicer Ribonuclease into a Death-Promoting Deoxyribonuclease. Science 2010, 328, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Walker, F.C.; Hatoum-Aslan, A. Conjugation Assay for Testing CRISPR-Cas Anti-Plasmid Immunity in Staphylococci. Bio-Protocol 2017, 7. [Google Scholar] [CrossRef]
- Marraffini, L.A.; Sontheimer, E.J. CRISPR Interference Limits Horizontal Gene Transfer in Staphylococci by Targeting DNA. Science 2008, 322, 1843–1845. [Google Scholar] [CrossRef]
- Di Nocera, P.P.; Rocco, F.; Giannouli, M.; Triassi, M.; Zarrilli, R. Genome Organization of Epidemic Acinetobacter Baumannii Strains. BMC Microbiol. 2011, 11, 224. [Google Scholar] [CrossRef] [PubMed]
- Hauck, Y.; Soler, C.; Jault, P.; Mérens, A.; Gérome, P.; Nab, C.M.; Trueba, F.; Bargues, L.; Thien, H.V.; Vergnaud, G.; et al. Diversity of Acinetobacter Baumannii in Four French Military Hospitals, as Assessed by Multiple Locus Variable Number of Tandem Repeats Analysis. PLoS ONE 2012, 7, e44597. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.R.; Lee, S.Y. CRISPR Technologies for Bacterial Systems: Current Achievements and Future Directions. Biotechnol. Adv. 2016, 34, 1180–1209. [Google Scholar] [CrossRef]
- Karah, N.; Samuelsen, Ø.; Zarrilli, R.; Sahl, J.W.; Wai, S.N.; Uhlin, B.E. CRISPR-Cas Subtype I-Fb in Acinetobacter Baumannii: Evolution and Utilization for Strain Subtyping. PLoS ONE 2015, 10, e0118205. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Bikard, D.; Cox, D.; Zhang, F.; Marraffini, L.A. RNA-Guided Editing of Bacterial Genomes Using CRISPR-Cas Systems. Nat. Biotechnol. 2013, 31, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Citorik, R.J.; Mimee, M.; Lu, T.K. Sequence-Specific Antimicrobials Using Efficiently Delivered RNA-Guided Nucleases. Nat. Biotechnol. 2014, 32, 1141–1145. [Google Scholar] [CrossRef] [PubMed]
- Bikard, D.; Euler, C.W.; Jiang, W.; Nussenzweig, P.M.; Goldberg, G.W.; Duportet, X.; Fischetti, V.A.; Marraffini, L.A. Exploiting CRISPR-Cas Nucleases to Produce Sequence-Specific Antimicrobials. Nat. Biotechnol. 2014, 32, 1146–1150. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-S.; Cho, D.-H.; Park, M.; Chung, W.-J.; Shin, D.; Ko, K.S.; Kweon, D.-H. CRISPR/Cas9-Mediated Re-Sensitization of Antibiotic-Resistant Escherichia Coli Harboring Extended-Spectrum β-Lactamases. J. Microbiol. Biotechnol. 2016, 26, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; He, T.; Zhang, L.; Pang, M.; Zhang, Q.; Zhou, Y.; Bao, H.; Wang, R. Generation of Newly Discovered Resistance Gene Mcr-1 Knockout in Escherichia Coli Using the CRISPR/Cas9 System. J. Microbiol. Biotechnol. 2017, 27, 1276–1280. [Google Scholar] [CrossRef]
- Liu, Q.; Jiang, Y.; Shao, L.; Yang, P.; Sun, B.; Yang, S.; Chen, D. CRISPR/Cas9-Based Efficient Genome Editing in Staphylococcus Aureus. Acta Biochim. Biophys. Sin. 2017, 49, 764–770. [Google Scholar] [CrossRef]
- So, Y.; Park, S.-Y.; Park, E.-H.; Park, S.-H.; Kim, E.-J.; Pan, J.-G.; Choi, S.-K. A Highly Efficient CRISPR-Cas9-Mediated Large Genomic Deletion in Bacillus Subtilis. Front. Microbiol. 2017, 8, 1167. [Google Scholar] [CrossRef]
- Dong, H.; Xiang, H.; Mu, D.; Wang, D.; Wang, T. Exploiting a Conjugative CRISPR/Cas9 System to Eliminate Plasmid Harbouring the Mcr-1 Gene from Escherichia Coli. Int. J. Antimicrob. Agents 2019, 53, 1–8. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, Z.; Chen, Y.; Hua, X.; Yu, Y.; Ji, Q. A Highly Efficient CRISPR-Cas9-Based Genome Engineering Platform in Acinetobacter Baumannii to Understand the H(2)O(2)-Sensing Mechanism of OxyR. Cell Chem. Biol. 2019, 26, 1732–1742.e5. [Google Scholar] [CrossRef] [PubMed]
- Mangas, E.L.; Rubio, A.; Álvarez-Marín, R.; Labrador-Herrera, G.; Pachón, J.; Pachón-Ibáñez, M.E.; Divina, F.; Pérez-Pulido, A.J. Pangenome of Acinetobacter Baumannii Uncovers Two Groups of Genomes, One of Them with Genes Involved in CRISPR/Cas Defence Systems Associated with the Absence of Plasmids and Exclusive Genes for Biofilm Formation. Microb. Genom. 2019, 5. [Google Scholar] [CrossRef] [PubMed]
- Karlapudi, A.P.; Venkateswarulu, T.C.; Tammineedi, J.; Srirama, K.; Kanumuri, L.; Prabhakar Kodali, V. In Silico SgRNA Tool Design for CRISPR Control of Quorum Sensing in Acinetobacter Species. Genes Dis. 2018, 5, 123–129. [Google Scholar] [CrossRef]
- Zhang, F.; Wen, Y.; Guo, X. CRISPR/Cas9 for Genome Editing: Progress, Implications and Challenges. Hum. Mol. Genet. 2014, 23, R40–R46. [Google Scholar] [CrossRef] [PubMed]
- Bozzuto, G.; Molinari, A. Liposomes as Nanomedical Devices. Int. J. Nanomed. 2015, 10, 975–999. [Google Scholar] [CrossRef] [PubMed]
- Taranejoo, S.; Liu, J.; Verma, P.; Hourigan, K. A Review of the Developments of Characteristics of PEI Derivatives for Gene Delivery Applications. J. Appl. Polym. Sci. 2015, 132. [Google Scholar] [CrossRef]
- Terwee, C.B.; Roorda, L.D.; Dekker, J.; Bierma-Zeinstra, S.M.; Peat, G.; Jordan, K.P.; Croft, P.; de Vet, H.C.W. Mind the MIC: Large Variation among Populations and Methods. J. Clin. Epidemiol. 2010, 63, 524–534. [Google Scholar] [CrossRef]
- Çağlan, E.; Nigiz, Ş.; Sancak, B.; Gür, D. Resistance and Heteroresistance to Colistin among Clinical Isolates of Acinetobacter Baumannii. Acta Microbiol. Immunol. Hung. 2019, 1–5. [Google Scholar] [CrossRef]
- Mouton, J.W.; Muller, A.E.; Canton, R.; Giske, C.G.; Kahlmeter, G.; Turnidge, J. MIC-Based Dose Adjustment: Facts and Fables. J. Antimicrob. Chemother. 2018, 73, 564–568. [Google Scholar] [CrossRef]
- Wiegand, I.; Hilpert, K.; Hancock, R.E.W. Agar and Broth Dilution Methods to Determine the Minimal Inhibitory Concentration (MIC) of Antimicrobial Substances. Nat. Protoc. 2008, 3, 163–175. [Google Scholar] [CrossRef]
- Pankey, G.A.; Sabath, L.D. Clinical Relevance of Bacteriostatic versus Bactericidal Mechanisms of Action in the Treatment of Gram-Positive Bacterial Infections. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2004, 38, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Hoen, B.; Tornos, P.; Thuny, F.; Prendergast, B.; Vilacosta, I.; Moreillon, P.; de Jesus Antunes, M.; Thilen, U.; Lekakis, J.; et al. Guidelines on the Prevention, Diagnosis, and Treatment of Infective Endocarditis (New Version 2009): The Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the Europea. Eur. Heart J. 2009, 30, 2369–2413. [Google Scholar] [CrossRef] [PubMed]
- Nau, R.; Djukic, M.; Spreer, A.; Ribes, S.; Eiffert, H. Bacterial Meningitis: An Update of New Treatment Options. Expert Rev. Anti-Infect. Ther. 2015, 13, 1401–1423. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, C.P.; Van Anglen, L.J.; Dretler, R.H.; Adams, J.S.; Prokesch, R.C.; Luu, Q.; Krinsky, A.H. Outpatient Treatment of Osteomyelitis with Telavancin. Int. J. Antimicrob. Agents 2017, 50, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Rafailidis, P.I.; Kouranos, V.D.; Christodoulou, C.; Falagas, M.E. Linezolid for Patients with Neutropenia: Are Bacteriostatic Agents Appropriate? Expert Rev. Anti-Infect. Ther. 2009, 7, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Nau, R.; Eiffert, H. Modulation of Release of Proinflammatory Bacterial Compounds by Antibacterials: Potential Impact on Course of Inflammation and Outcome in Sepsis and Meningitis. Clin. Microbiol. Rev. 2002, 15, 95–110. [Google Scholar] [CrossRef] [PubMed]
- El-Halfawy, O.M.; Valvano, M.A. Antimicrobial Heteroresistance: An Emerging Field in Need of Clarity. Clin. Microbiol. Rev. 2015, 28, 191–207. [Google Scholar] [CrossRef]
- Anderson, S.E.; Sherman, E.X.; Weiss, D.S.; Rather, P.N. Aminoglycoside Heteroresistance in Acinetobacter Baumannii AB5075. mSphere 2018, 3. [Google Scholar] [CrossRef]
- Lee, H.-Y.; Chen, C.-L.; Wang, S.-B.; Su, L.-H.; Chen, S.-H.; Liu, S.-Y.; Wu, T.-L.; Lin, T.-Y.; Chiu, C.-H. Imipenem Heteroresistance Induced by Imipenem in Multidrug-Resistant Acinetobacter Baumannii: Mechanism and Clinical Implications. Int. J. Antimicrob. Agents 2011, 37, 302–308. [Google Scholar] [CrossRef]
- Hung, K.-H.; Wang, M.-C.; Huang, A.-H.; Yan, J.-J.; Wu, J.-J. Heteroresistance to Cephalosporins and Penicillins in Acinetobacter Baumannii. J. Clin. Microbiol. 2012, 50, 721–726. [Google Scholar] [CrossRef]
- Li, J.; Rayner, C.R.; Nation, R.L.; Owen, R.J.; Spelman, D.; Tan, K.E.; Liolios, L. Heteroresistance to Colistin in Multidrug-Resistant Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2006, 50, 2946–2950. [Google Scholar] [CrossRef] [PubMed]
- Sola, C.; Lamberghini, R.O.; Ciarlantini, M.; Egea, A.L.; Gonzalez, P.; Diaz, E.G.; Huerta, V.; Gonzalez, J.; Corso, A.; Vilaro, M.; et al. Heterogeneous Vancomycin-Intermediate Susceptibility in a Community-Associated Methicillin-Resistant Staphylococcus Aureus Epidemic Clone, in a Case of Infective Endocarditis in Argentina. Ann. Clin. Microbiol. Antimicrob. 2011, 10, 15. [Google Scholar] [CrossRef] [PubMed]
- Hawley, J.S.; Murray, C.K.; Jorgensen, J.H. Colistin Heteroresistance in Acinetobacter and Its Association with Previous Colistin Therapy. Antimicrob. Agents Chemother. 2008, 52, 351–352. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).