Establishment of a Challenge Model for Sheeppox Virus Infection
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Design and Collection of Samples
2.3. Molecular Analyses of Different Sample Matrices
2.4. Serological Examination
2.5. Sequencing of SPPV-“India/2013/Surankote” and SPPV-“Egypt/2018”
3. Results
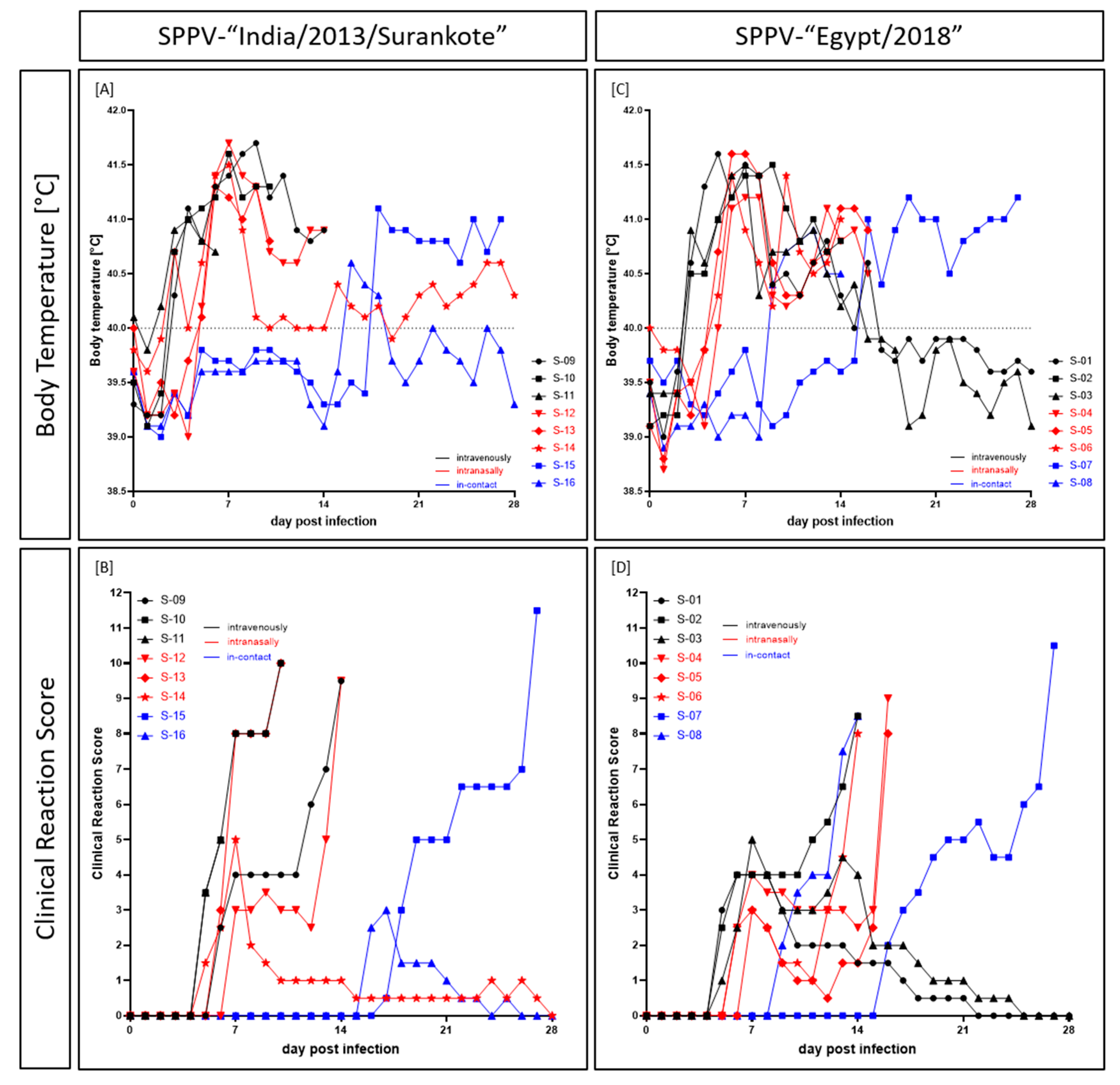
3.1. Clinical Signs after Experimental Infection
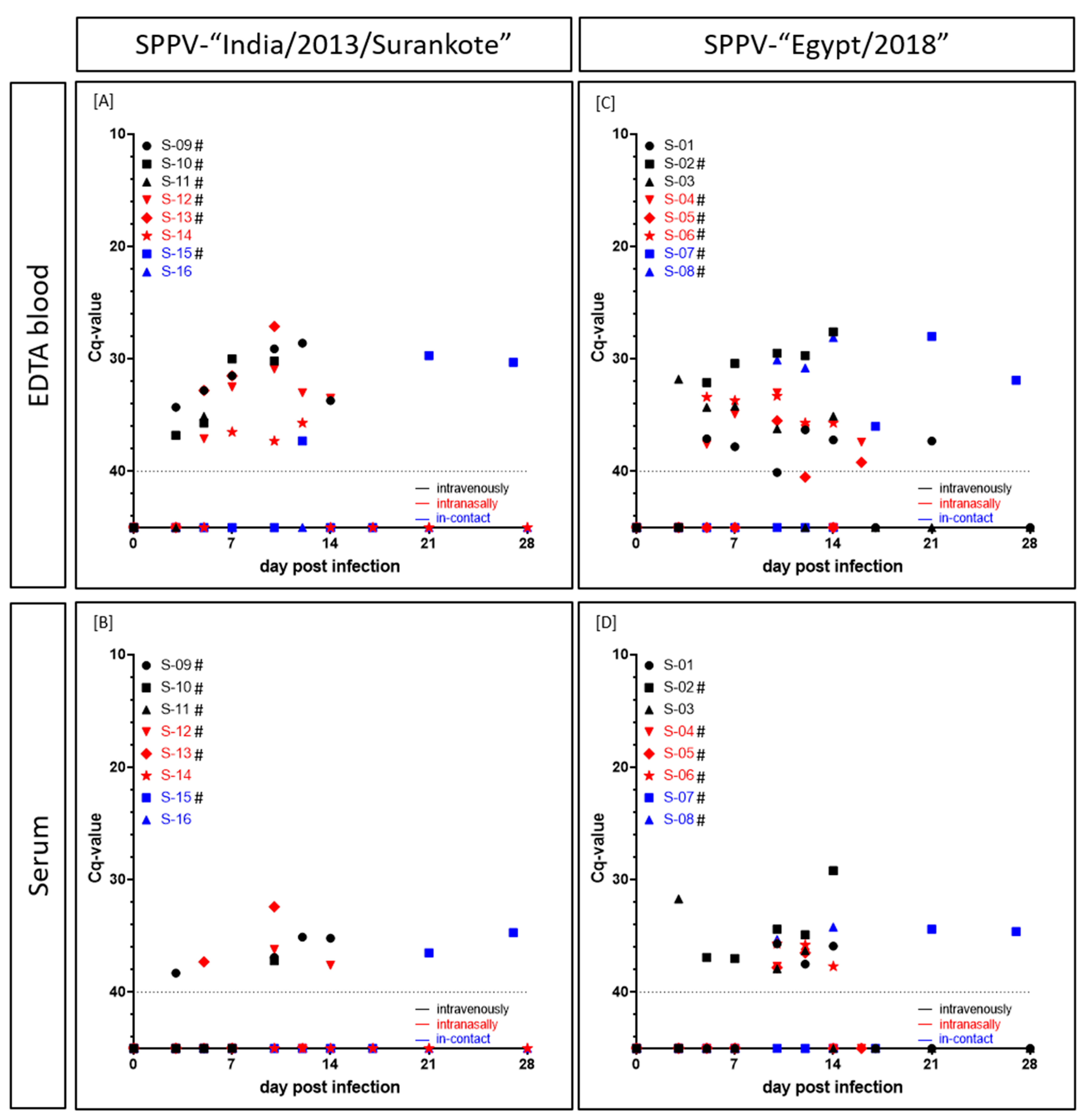
3.2. Viremia and Shedding of Virus
3.3. Presence of Viral Gnome in Organ Samples
3.4. Serological Response
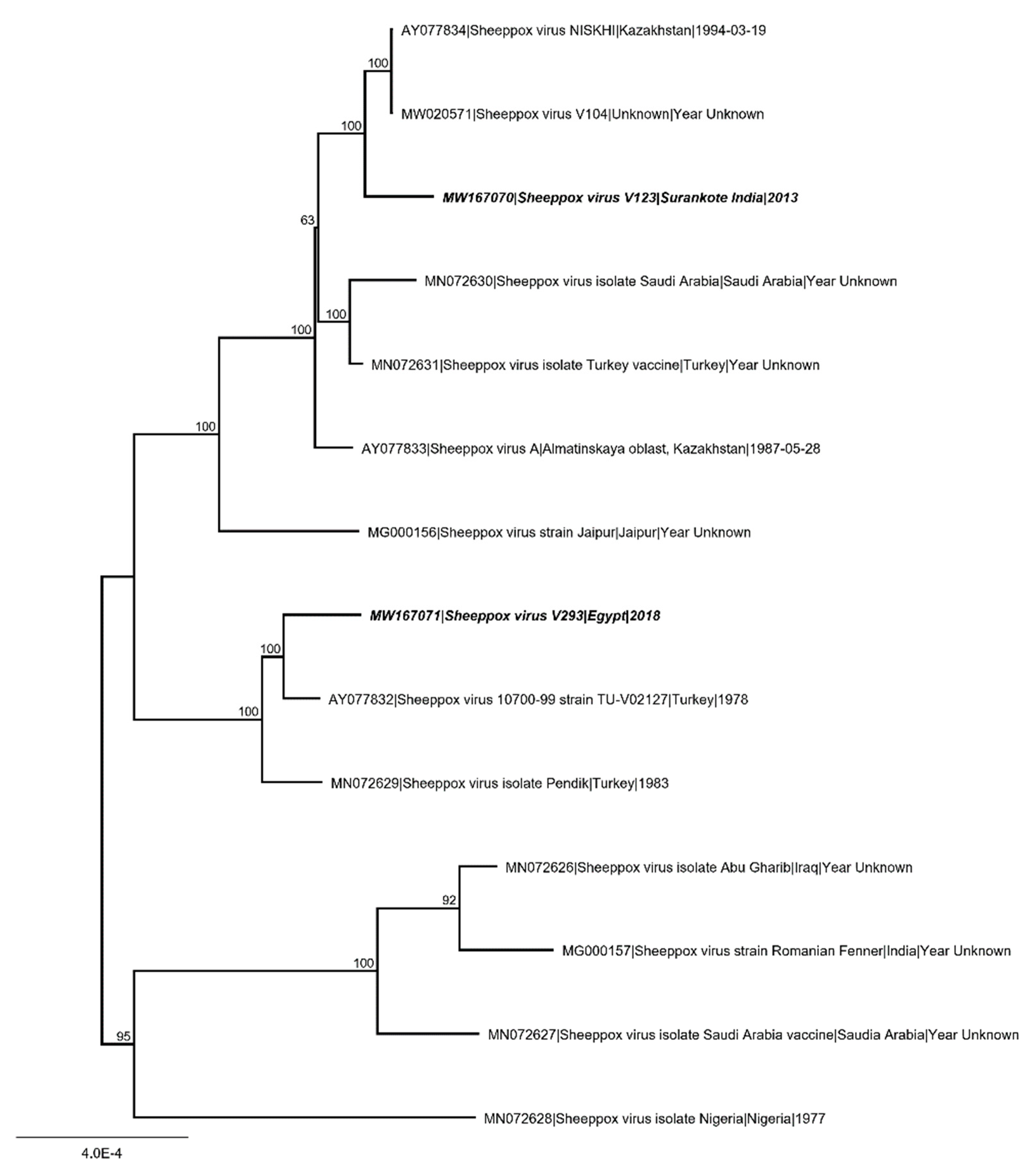
3.5. Full Genome Sequencing of SPPV-“India/2013/Surankote” and SPPV-“Egypt/2018”
4. Discussion
4.1. Genetic Relationship of SPPV-“India/2013/Surankote” and SPPV-“Egypt/2018”
4.2. Pathogenesis in Sheep after Experimental Infection
4.3. Establishment of a Challenge Model for SPPV Infections
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- King, A.M.Q.; Adams, M.J.; Carstens, E.B.; Lefkowitz, E. Virus Taxonomy—Classification and Nomenclature of Viruses: Ninth Report of the International Committee on Taxonomy of Viruses; Elsevier Academic Press: San Diego, CA, USA, 2012; pp. 291–309. [Google Scholar]
- International Committee on Taxonomy of Viruses. Virus Taxonomy: 2019 Release. Available online: https://talk.ictvonline.org/taxonomy/ (accessed on 9 September 2020).
- Babiuk, S.; Bowden, T.R.; Boyle, D.B.; Wallace, D.B.; Kitching, R.P. Capripoxviruses: An emerging worldwide threat to sheep, goats and cattle. Transbound. Emerg. Dis. 2008, 55, 263–272. [Google Scholar] [CrossRef]
- Bowden, T.R.; Babiuk, S.L.; Parkyn, G.R.; Copps, J.S.; Boyle, D.B. Capripoxvirus tissue tropism and shedding: A quantitative study in experimentally infected sheep and goats. Virology 2008, 371, 380–393. [Google Scholar] [CrossRef]
- Boumart, Z.; Daouam, S.; Belkourati, I.; Rafi, L.; Tuppurainen, E.; Tadlaoui, K.O.; El Harrak, M. Comparative innocuity and efficacy of live and inactivated sheeppox vaccines. BMC Vet. Res. 2016, 12, 133. [Google Scholar] [CrossRef]
- Kitching, P. Progress towards sheep and goat pox vaccines. Vaccine 1983, 1, 4–9. [Google Scholar] [CrossRef]
- Babiuk, S.; Bowden, T.R.; Parkyn, G.; Dalman, B.; Hoa, D.M.; Long, N.T.; Vu, P.P.; Bieu, D.X.; Copps, J.; Boyle, D.B. Yemen and Vietnam capripoxviruses demonstrate a distinct host preference for goats compared with sheep. J. Gen. Virol. 2009, 90, 105–114. [Google Scholar] [CrossRef]
- Kitching, R.P.; Carn, V.M. Sheep pox and goat pox. In Office International des Epizooties Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (Mammals, Birds and Bees); OIE: Paris, France, 2004. [Google Scholar]
- Carn, V.M. Control of capripoxvirus infections. Vaccine 1993, 11, 1275–1279. [Google Scholar] [CrossRef]
- Bhanuprakash, V.; Indrani, B.K.; Hosamani, M.; Singh, R.K. The current status of sheep pox disease. Comp. Immunol. Microbiol. Infect. Dis. 2006, 29, 27–60. [Google Scholar] [CrossRef]
- Rao, T.V.; Bandyopadhyay, S.K. A comprehensive review of goat pox and sheep pox and their diagnosis. Anim. Health Res. Rev. 2000, 1, 127–136. [Google Scholar] [CrossRef]
- Tuppurainen, E.S.M.; Venter, E.H.; Shisler, J.L.; Gari, G.; Mekonnen, G.A.; Juleff, N.; Lyons, N.A.; De Clercq, K.; Upton, C.; Bowden, T.R.; et al. Review: Capripoxvirus Diseases: Current Status and Opportunities for Control. Transbound. Emerg. Dis. 2017, 64, 729–745. [Google Scholar] [CrossRef]
- Boshra, H.; Truong, T.; Babiuk, S.; Hemida, M.G. Seroprevalence of Sheep and Goat Pox, Peste Des Petits Ruminants and Rift Valley Fever in Saudi Arabia. PLoS ONE 2015, 10, e0140328. [Google Scholar] [CrossRef]
- OIE. Technical Disease Card: Sheep Pox and Goat Pox; OIE: Paris, France, 2013. [Google Scholar]
- OIE. Sheep pox and goat pox. In OIE Terrestrial Manual 2017; Chapter 2.7.13; OIE: Paris, France, 2017. [Google Scholar]
- Kitching, R.P.; Taylor, W.P. Transmission of capripoxvirus. Res. Vet. Sci. 1985, 39, 196–199. [Google Scholar] [CrossRef]
- Mellor, P.S.; Kitching, R.P.; Wilkinson, P.J. Mechanical transmission of capripox virus and African swine fever virus by Stomoxys calcitrans. Res. Vet. Sci. 1987, 43, 109–112. [Google Scholar] [CrossRef]
- Chamchod, F. Modeling the spread of capripoxvirus among livestock and optimal vaccination strategies. J. Theor. Biol. 2018, 437, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Davies, F.G. Characteristics of a virus causing a pox disease in sheep and goats in Kenya, with observation on the epidemiology and control. J. Hyg. 1976, 76, 163–171. [Google Scholar] [CrossRef]
- Yeruham, I.; Yadin, H.; Van Ham, M.; Bumbarov, V.; Soham, A.; Perl, S. Economic and epidemiological aspects of an outbreak of sheeppox in a dairy sheep flock. Vet Rec. 2007, 160, 236–237. [Google Scholar] [CrossRef]
- OIE. OIE-Listed Diseases, Infections and Infestations in Force in 2020. Available online: https://www.oie.int/animal-health-in-the-world/oie-listed-diseases-2020/ (accessed on 16 October 2020).
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; Zsak, L.; Kutish, G.F.; Rock, D.L. Genome of lumpy skin disease virus. J. Virol. 2001, 75, 7122–7130. [Google Scholar] [CrossRef]
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; Zsak, L.; Sur, J.H.; Sandybaev, N.T.; Kerembekova, U.Z.; Zaitsev, V.L.; Kutish, G.F.; Rock, D.L. The genomes of sheeppox and goatpox viruses. J. Virol. 2002, 76, 6054–6061. [Google Scholar] [CrossRef]
- Biswas, S.; Noyce, R.S.; Babiuk, L.A.; Lung, O.; Bulach, D.M.; Bowden, T.R.; Boyle, D.B.; Babiuk, S.; Evans, D.H. Extended sequencing of vaccine and wild-type capripoxvirus isolates provides insights into genes modulating virulence and host range. Transbound. Emerg. Dis. 2020, 67, 80–97. [Google Scholar] [CrossRef]
- Wolff, J.; King, J.; Moritz, T.; Pohlmann, A.; Hoffmann, D.; Beer, M.; Hoffmann, B. Experimental Infection and Genetic Characterization of Two Different Capripox Virus Isolates in Small Ruminants. Viruses 2020, 12, 1098. [Google Scholar] [CrossRef]
- Forth, J.H.; Forth, L.F.; King, J.; Groza, O.; Hubner, A.; Olesen, A.S.; Hoper, D.; Dixon, L.K.; Netherton, C.L.; Rasmussen, T.B.; et al. A Deep-Sequencing Workflow for the Fast and Efficient Generation of High-Quality African Swine Fever Virus Whole-Genome Sequences. Viruses 2019, 11, 846. [Google Scholar] [CrossRef]
- Bhanuprakash, V.; Hosamani, M.; Singh, R.K. Prospects of control and eradication of capripox from the Indian subcontinent: A perspective. Antivir. Res. 2011, 91, 225–232. [Google Scholar] [CrossRef]
- Bhanuprakash, V.; Moorthy, A.R.; Krishnappa, G.; Srinivasa Gowda, R.N.; Indrani, B.K. An epidemiological study of sheep pox infection in Karnataka State, India. Rev. Sci. Tech. 2005, 24, 909–920. [Google Scholar] [CrossRef] [PubMed]
- Manjunatha Reddy, G.B.; Balamurugan, V.; Suresh, K.P.; Hemadri, D.; Patil, S.S.; Govindaraj, G. Epidemiology and Impact Analysis of Sheep and Goat Pox; ICAR-National Institute of Veterinary Epidemiology and Disease Informatics (ICAR-NIVEDI) Annual Report; ICAR: New Delhi, India, 2015. [Google Scholar]
- Fares, M.; Fawzy, M.; Shahin, M.; Elshahidy, M. A Comprehensive Review of Sheep and Goat Pox Viruses: Perspective of Their Epidemiology and Economic Importance in Egypt. SCVMJ 2019, 24, 313–328. [Google Scholar] [CrossRef][Green Version]
- Mahmoud, M.A.; Khafagi, M.H. Detection, identification, and differentiation of sheep pox virus and goat pox virus from clinical cases in Giza Governorate, Egypt. Vet. World 2016, 9, 1445–1449. [Google Scholar] [CrossRef] [PubMed]
- Abd-Elfatah, E.B.; El-Mekkawi, M.F.; Bastawecy, I.M.; Fawzi, E.M. Identification and phylogentic analysis of sheep pox during an outbreak of sheep in Sharkia Governorate, Egypt. Genet. Mol. Res. 2018, 17, gmr16039901. [Google Scholar] [CrossRef]
- Wolff, J.; Krstevski, K.; Beer, M.; Hoffmann, B. Minimum Infective Dose of a Lumpy Skin Disease Virus Field Strain from North Macedonia. Viruses 2020, 12, 768. [Google Scholar] [CrossRef] [PubMed]
- Carn, V.M.; Kitching, R.P. The clinical response of cattle experimentally infected with lumpy skin disease (Neethling) virus. Arch. Virol. 1995, 140, 503–513. [Google Scholar] [CrossRef]
- Hoffmann, B.; Depner, K.; Schirrmeier, H.; Beer, M. A universal heterologous internal control system for duplex real-time RT-PCR assays used in a detection system for pestiviruses. J. Virol. Methods 2006, 136, 200–209. [Google Scholar] [CrossRef]
- Dietze, K.; Moritz, T.; Alexandrov, T.; Krstevski, K.; Schlottau, K.; Milovanovic, M.; Hoffmann, D.; Hoffmann, B. Suitability of group-level oral fluid sampling in ruminant populations for lumpy skin disease virus detection. Vet. Microbiol. 2018, 221, 44–48. [Google Scholar] [CrossRef]
- Spearman, C. The Method of ‘Right and Wrong Cases’ (‘Constant Stimuli’) without Gauss’s Formulae. Br. J. Psychol. 1908, 2, 227–242. [Google Scholar] [CrossRef]
- Kärber, G. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Naunyn-Schmiedebergs Arch. Exp. Pathol. Pharmakol. 1931, 162, 480–483. [Google Scholar] [CrossRef]
- Katoh, K.; Standley, D.M. MAFFT multiple sequence alignment software version 7: Improvements in performance and usability. Mol. Biol. Evol. 2013, 30, 772–780. [Google Scholar] [CrossRef]
- Stamatakis, A. RAxML version 8: A tool for phylogenetic analysis and post-analysis of large phylogenies. Bioinformatics 2014, 30, 1312–1313. [Google Scholar] [CrossRef]
- Möller, J.; Moritz, T.; Schlottau, K.; Krstevski, K.; Hoffmann, D.; Beer, M.; Hoffmann, B. Experimental lumpy skin disease virus infection of cattle: Comparison of a field strain and a vaccine strain. Arch. Virol. 2019, 164, 2931–2941. [Google Scholar] [CrossRef]
- Hajjou, S.; Khataby, K.; Amghar, S.; El Fahime, M.; El Harrak, M.; Fakiri, M.; Loutfi, C. Assessment and comparison of the pathogenicity of Sheeppox Virus strains isolated in Morocco. Iran. J. Microbiol. 2017, 9, 372–380. [Google Scholar]
- Hamdi, J.; Bamouh, Z.; Jazouli, M.; Boumart, Z.; Tadlaoui, K.O.; Fihri, O.F.; El Harrak, M. Experimental evaluation of the cross-protection between Sheeppox and bovine Lumpy skin vaccines. Sci. Rep. 2020, 10, 8888. [Google Scholar] [CrossRef]
- Eschbaumer, M.; Schulz, C.; Wackerlin, R.; Gauly, M.; Beer, M.; Hoffmann, B. Limitations of sandwich ELISAs for bluetongue virus antibody detection. Vet. Rec. 2011, 168, 643. [Google Scholar] [CrossRef]



| Animal ID | IND-IV-09 | IND-IV-10 | IND-IV-11 | IND-IN-12 | IND-IN-13 | IND-IN-14 | IND-IC-15 | IND-IC-16 |
| Days Until Euthanasia | 14 dpi | 10 dpi | 7 dpi | 14 dpi | 10 dpi | recovered | 27 dpi | recovered |
| Animal ID | EG-IV-01 | EG-IV-02 | EG-IV-03 | EG-IN-04 | EG-IN-05 | EG-IN-06 | EG-IC-07 | EG-IC-08 |
| Days Until Euthanasia | recovered | 14 dpi | recovered | 16 dpi | 16 dpi | 14 dpi | 27 dpi | 14 dpi |
| Evaluation Group | Symptomatic | Score |
|---|---|---|
| General condition | Unremarkable | 0 |
| Reduced activity | 1 | |
| Reduced activity, depressive | 2 | |
| Increased resting, clearly reduced activity | 3 | |
| Apathy and/or lateral position, animal does not react to stimuli | Abandonment | |
| Feed and water intake | Unremarkable | 0 |
| Reduced feed or water intake, increased salivation | 1 | |
| Clearly reduced feed or water intake, slight weight loss | 2 | |
| No feed or water intake (1 day), marked weight loss | 3 | |
| No feed or water intake (2 day), weight loss >10% compared to the day of experimental infection | Abandonment | |
| Respiratory tract | Unremarkable | 0 |
| Slightly difficult breathing | 1 | |
| Marked difficult breathing, breathing sound, slight abdominal breathing | 2 | |
| Marked difficult breathing, clear breathing sound, moderate abdominal breathing | 3 | |
| Strong difficult breathing, strong breathing sound, strong abdominal breathing | Abandonment | |
| Nasal discharge | Not observed | 0 |
| Slight to moderate nasal discharge, nose not/only slightly sticky | 1 | |
| Strong nasal discharge, nose clearly sticky | 2 | |
| Skin changes | Unremarkable | 0 |
| Sporadic skin nodules/lesions/papules | 1 | |
| Many skin nodules/lesions/papules | 2 | |
| Generalized skin lesions/nodules/papules | 3 | |
| Multiple abscesses or phlegmons | Abandonment | |
| Additional clinical signs | Lameness | 1 |
| Mild swelling of cervical lymph node | 1 | |
| Strong swelling of cervical lymph node | 2 |
| SPPV-“India/2013/Surankote” | Capri-p32-Taq-FAM | |||||||
|---|---|---|---|---|---|---|---|---|
| Organ Sample | Intravenously | Intranasally | In-Contact | |||||
| IND-IV-09 | IND-IV-10 | IND-IV-11 | IND-IN-12 | IND-IN-13 | IND-IN-14 | IND-IC-15 | IND-IC-16 | |
| cervical lymph node | 31.0 | 33.0 | 32.4 | 34.7 | 25.9 | no Cq | 30.4 | no Cq |
| mediastinal lymph node | no Cq | 33.0 | 31.0 | no Cq | no Cq | no Cq | no Cq | no Cq |
| mesenterial lymph node | no Cq | no Cq | no Cq | no Cq | no Cq | no Cq | 35.6 | no Cq |
| liver | no Cq | no Cq | 34.1 | no Cq | 36.4 | no Cq | 35.7 | no Cq |
| spleen | no Cq | no Cq | 36.4 | no Cq | 34.3 | no Cq | no Cq | no Cq |
| lung | 34.3 | 26.8 | 22.8 | no Cq | 33.1 | no Cq | 37.0 | no Cq |
| Additional Samples | ||||||||
| coagulated heart blood | - | - | 29.4 | - | - | - | - | - |
| lung fluid | - | - | 31.4 | - | - | - | - | - |
| Location of Skin Sample | ||||||||
| breast | - | 29.5 | - | - | 28.5 | - | - | - |
| - | 19.4 | - | - | 29.5 | - | - | - | |
| - | 28.9 | - | - | 23.1 | - | - | - | |
| - | 20.4 | - | - | 28.3 | - | - | - | |
| axilla | 16.6 | 28.4 | 21.2 | 36.3 | 27.4 | - | 25.9 | - |
| 29.7 | 25.0 | 27.9 | 36.5 | 23.9 | - | 23.3 | - | |
| 27.3 | 30.7 | 30.4 | 36.3 | 24.2 | - | 24.5 | - | |
| 29.2 | 20.9 | 24.0 | 37.2 | 23.4 | - | 28.1 | - | |
| back | - | - | - | - | 23.3 | - | - | - |
| - | - | - | - | 26.2 | - | - | - | |
| - | - | - | - | 17.4 | - | - | - | |
| - | - | - | - | 16.9 | - | - | - | |
| hind leg | - | 32.8 | - | - | 21.3 | - | 21.0 | - |
| - | 31.7 | - | - | 18.5 | - | 19.7 | - | |
| - | 30.5 | - | - | 18.4 | - | 20.5 | - | |
| - | 32.0 | - | - | 18.1 | - | 19.3 | - | |
| tail | - | - | - | - | - | - | 19.5 | - |
| scrotum | - | 20.1 | - | - | 25.9 | - | 21.0 | - |
| - | - | - | - | 27.8 | - | 19.7 | - | |
| prepuce | - | 18.4 | - | - | 17.6 | - | 18.9 | - |
| - | 18.2 | - | - | - | - | 16.7 | - | |
| pox-like lesion lung | 35.7 | - | - | - | - | - | 21.9 | - |
| 35.4 | - | - | - | - | - | 33.8 | - | |
| SPPV-“Egypt/2018” | Capri-p32-Taq-FAM | |||||||
|---|---|---|---|---|---|---|---|---|
| Organ Sample | Intravenously | Intranasally | In-Contact | |||||
| EG-IV-01 | EG-IV-02 | EG-IV-03 | EG-IN-04 | EG-IN-05 | EG-IN-06 | EG-IC-07 | EG-IC-08 | |
| cervical lymph node | no Cq | 32.0 | no Cq | 32.2 | no Cq | no Cq | 27.0 | 28.8 |
| mediastinal lymph node | 36.5 | no Cq | no Cq | 37.2 | no Cq | no Cq | 33.2 | 39.3 |
| mesenterial lymph node | no Cq | 36.7 | no Cq | no Cq | 35.7 | no Cq | 37.4 | no Cq |
| liver | no Cq | no Cq | no Cq | no Cq | no Cq | no Cq | no Cq | no Cq |
| spleen | 37.7 | 31.9 | 37.4 | 39.1 | no Cq | 38.1 | 39.1 | 36.8 |
| lung | no Cq | 30.4 | 37.4 | 33.8 | 33.2 | 34.3 | 35.2 | 33.6 |
| Additional Samples | ||||||||
| brain | - | - | - | - | - | - | - | no Cq |
| - | - | - | - | - | - | - | no Cq | |
| - | - | - | - | - | - | - | no Cq | |
| nasal septum | - | - | - | 21.3 | 28.1 | - | - | - |
| Location of Skin Sample | - | - | - | |||||
| ear | - | - | - | - | 16.7 | - | - | - |
| - | - | - | - | 14.7 | - | - | - | |
| - | - | - | - | 16.0 | - | - | - | |
| foreleg | - | - | - | - | - | - | 18.0 | - |
| - | - | - | - | - | - | 20.2 | - | |
| axilla | - | 22.2 | - | - | - | - | - | 23.8 |
| - | 21.0 | - | - | - | - | - | 22.4 | |
| - | 22.0 | - | - | - | - | - | 28.5 | |
| - | 18.8 | - | - | - | - | - | - | |
| hind leg | - | - | - | - | - | - | 19.8 | - |
| tail | - | - | - | - | - | - | 18.0 | - |
| - | - | - | - | - | - | 19.0 | - | |
| - | - | - | - | - | - | 20.1 | - | |
| prepuce | - | 16.3 | - | 22.3 | - | - | 20.5 | 18.2 |
| - | 14.7 | - | 19.9 | - | - | 16.4 | - | |
| pox-like lesion lung | - | - | - | 26.5 | 32.9 | - | - | - |
| - | - | - | 26.2 | - | - | - | - | |
| - | - | - | 27.7 | - | - | - | - | |
| healed skin lesion | 28.1 | - | 23.5 | - | 24.1 | - | - | - |
| 27.8 | - | 19.8 | - | - | - | - | - | |
| 32.1 | - | 24.6 | - | - | - | - | - | |
| 28.4 | - | 30.3 | - | - | - | - | - | |
| 25.7 | - | - | - | - | - | - | - | |
| encrusted skin lesion | - | - | 13.8 | - | - | - | - | - |
| - | - | 15.5 | - | - | - | - | - | |
| - | - | 15.9 | - | - | - | - | - | |
| - | - | 17.8 | - | - | - | - | - | |
| - | - | 14.1 | - | - | - | - | - | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolff, J.; Abd El Rahman, S.; King, J.; El-Beskawy, M.; Pohlmann, A.; Beer, M.; Hoffmann, B. Establishment of a Challenge Model for Sheeppox Virus Infection. Microorganisms 2020, 8, 2001. https://doi.org/10.3390/microorganisms8122001
Wolff J, Abd El Rahman S, King J, El-Beskawy M, Pohlmann A, Beer M, Hoffmann B. Establishment of a Challenge Model for Sheeppox Virus Infection. Microorganisms. 2020; 8(12):2001. https://doi.org/10.3390/microorganisms8122001
Chicago/Turabian StyleWolff, Janika, Sahar Abd El Rahman, Jacqueline King, Mohamed El-Beskawy, Anne Pohlmann, Martin Beer, and Bernd Hoffmann. 2020. "Establishment of a Challenge Model for Sheeppox Virus Infection" Microorganisms 8, no. 12: 2001. https://doi.org/10.3390/microorganisms8122001
APA StyleWolff, J., Abd El Rahman, S., King, J., El-Beskawy, M., Pohlmann, A., Beer, M., & Hoffmann, B. (2020). Establishment of a Challenge Model for Sheeppox Virus Infection. Microorganisms, 8(12), 2001. https://doi.org/10.3390/microorganisms8122001





