Phenotypes Associated with Pathogenicity: Their Expression in Arctic Fungal Isolates
Abstract
1. Introduction
2. Materials and Methods
2.1. Site and Sample Description
2.2. Fungal Cultivation and Isolation
2.3. Fungal Identification
2.4. Thermotolerance Assay
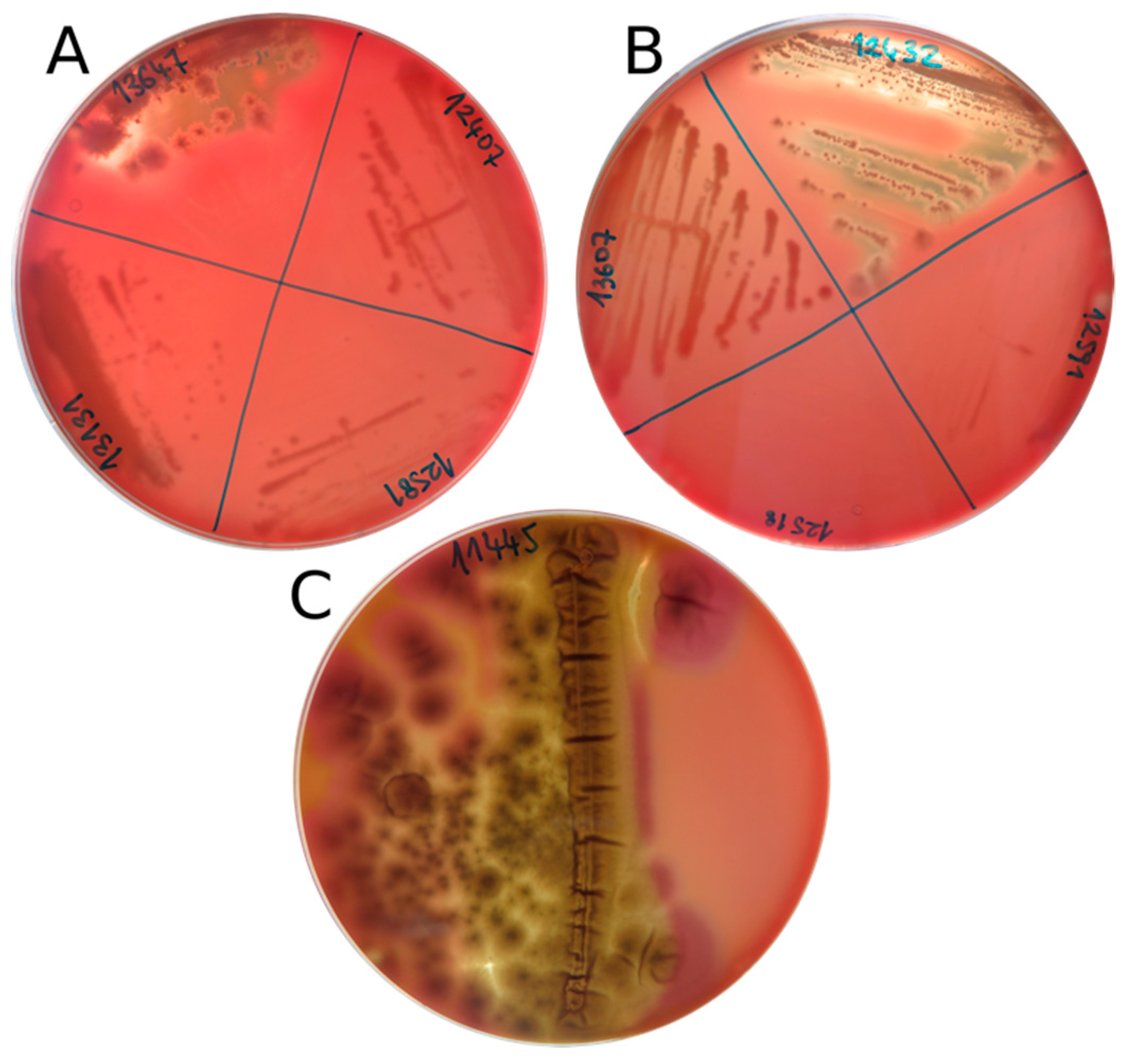
2.5. Hemolytic Assay on Blood Agar
2.6. Antifungal Susceptibility Test (AFST)
3. Results
3.1. Fungal Isolation and Identification
3.2. Thermotolerance
3.3. Hemolytic Assay on Blood Agar
3.4. Antifungal Susceptibility Test (AFST)
3.4.1. Azoles
3.4.2. Echinocandins
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Anesio, A.M.; Laybourn-Parry, J. Glaciers and ice sheets as a biome. Trends Ecol. Evol. 2012, 27, 219–225. [Google Scholar] [CrossRef]
- Kirby, B.M.; Easton, S.; Tuffin, I.M.; Cowan, D.M. Bacterial diversity in polar habitats. In Polar Microbiology: Life in a Deep Freeze; Miller, R.V., Whyte, L., Eds.; ASM Press: Washington, DC, USA, 2012; p. 30. [Google Scholar]
- Hassan, N.; Rafiq, M.; Hayat, M.; Ali Shah, A.; Hasan, F. Psychrophilic and psychrotrophic fungi: A comprehensive review. Rev. Environ. Sci. Biotechnol. 2016, 15, 147–172. [Google Scholar] [CrossRef]
- Perini, L.; Gostinčar, C.; Anesio, A.M.; Williamson, C.; Tranter, M.; Gunde-Cimerman, N. Darkening of the Greenland ice sheet: Fungal abundance and diversity are associated with algal bloom. Front Microbiol. 2019, 10, 557. [Google Scholar] [CrossRef]
- Van den Ende, G.; de Hoog, G.S. Variability and molecular diagnostics of the neurotropic species Cladophialophora bantiana. Stud. Mycol. 1999, 43, 151–162. [Google Scholar]
- Gesheva, V. Distribution of psychrophilic microorganisms in soils of Terra Nova Bay and Edmonson Point, Victoria Land and their biosynthetic capabilities. Polar Biol. 2009, 32, 1287–1291. [Google Scholar] [CrossRef]
- Bell, T. Experimental tests of the bacterial distance-decay relationship. ISME J. 2010, 4, 1357–1365. [Google Scholar] [CrossRef]
- Chong, C.W.; Pearce, D.A.; Convey, P. Emerging spatial patterns in Antarctic prokaryotes. Front Microbiol. 2015, 6, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kleinteich, J.; Hildebrand, F.; Bahram, M.; Voigt, A.Y.; Wood, S.A.; Jungblut, A.D.; Küpper, F.C.; Quesada, A.; Camacho, A.; Pearce, D.A. Pole-to-Pole connections: Similarities between Arctic and Antarctic microbiomes and their vulnerability to environmental change. Front Ecol. Evol. 2017, 5, 1–11. [Google Scholar] [CrossRef]
- Pearce, D.A.; Bridge, P.D.; Hughes, K.A.; Sattler, B.; Psenner, R.; Russell, N.J. Microorganisms in the atmosphere over Antarctica. FEMS Microbiol. Ecol. 2009, 69, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.O.; Starmer, W.T.; Castello, J.D. Recycling of pathogenic microbes through survival in ice. Med. Hypotheses 2004, 63, 773–777. [Google Scholar] [CrossRef]
- Christner, B.C.; Morris, C.E.; Foreman, C.M.; Rongman, C.; Sands, D.C. Ubiquity of biological ice nucleators in snowfall. Science 2008, 319, 1214. [Google Scholar] [CrossRef] [PubMed]
- Shen, F.; Yao, M. Are We Biologically Safe with Snow Precipitation? A Case Study in Beijing. PLoS ONE 2013, 8, e65249. [Google Scholar] [CrossRef] [PubMed]
- Gostinčar, C.; Zajc, J.; Lenassi, M.; Plemenitas, A.; de Hoog, S.; Al-Hatmi, A.M.S.; Gunde-Cimerman, N. Fungi between extremotolerance and opportunistic pathogenicity on humans. Fungal Divers 2018, 93, 195–213. [Google Scholar] [CrossRef]
- Ejdys, E.; Biedunkiewicz, A.; Dynowska, M.; Sucharzweska, E. Snow in the city as a spore bank of potentially pathogenic fungi. Sci. Total Environ. 2014, 470–471, 646–650. [Google Scholar] [CrossRef] [PubMed]
- Edwards, A. Coming in from the cold: Potential microbial threats from the terrestrial cryosphere. Front. Earth Sci. 2015, 3, 10–13. [Google Scholar] [CrossRef]
- D’Amico, S.; Collins, T.; Marx, J.-C.C.; Feller, G.; Gerday, C. Psychrophilic microorganisms: Challenges for life. EMBO Rep. 2006, 7, 385–389. [Google Scholar] [CrossRef]
- Gostinčar, C.; Grube, M.; Gunde-Cimerman, N. Evolution of Fungal Pathogens in Domestic Environments? Fungal. Biol. 2011, 115, 1008–1018. [Google Scholar] [CrossRef]
- Murray, P.R.; Rosenthal, K.S.; Pfaller, M.A. Medical Microbiology; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Campoy, S.; Adrio, J. Antifungals. Biochem. Pharmacol. 2017, 133, 86–96. [Google Scholar] [CrossRef]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2015, 62, e1–e50. [Google Scholar] [CrossRef]
- Perfect, J.R.; Dismukes, W.E.; Dromer, F.; Goldman, D.L.; Graybill, J.R.; Hamill, R.J.; Harrison, T.S.; Larsen, R.A.; Lortholary, O.; Nguyen, M.-H.; et al. Clinical Practice Guidelines for the Management of Cryptococcal Disease: 2010 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2010, 50, 291–322. [Google Scholar] [CrossRef]
- Peyton, L.R.; Gallagher, S.; Hashemzadeh, M. Triazole antifungals: A review. Drugs Today 2015, 51, 705–718. [Google Scholar] [CrossRef] [PubMed]
- Perlin, D.S.; Rautemaa-Richardson, R.; Alastruey-Izquierdo, A. The Global Problem of Antifungal Resistance: Prevalence, Mechanisms, and Management. Lancet Infect. Dis. 2017. [Google Scholar] [CrossRef]
- Zhang, T.; Wang, N.F.; Zhang, Y.Q.; Liu, H.-Y.; Yu, L.-Y. Diversity and Distribution of Aquatic Fungal Communities in the Ny-Alesund Region, Svalbard (High Arctic): Aquatic Fungi in the Arctic. Microb. Ecol. 2016, 71, 543–554. [Google Scholar] [CrossRef] [PubMed]
- Mirski, T.; Bartoszcze, M.; Bielawska-Drózd, A. Impact of climate change on infectious diseases. Polish J. Environ. Stud. 2012, 21, 525–532. [Google Scholar]
- Altizer, S.; Ostfeld, R.S.; Johnson, P.T.J.; Kutz, S.; Harvell, C.D. Climate Change and Infectious Diseases: From Evidence to a Predictive Framework. Science 2013, 341, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Intergovernmental Panel on Climate Change IPCC. Climate Change 2014, Impacts, Adaptation and Vulnerability. Part B: Regional Aspects; Cambridge University Press: Makati, UK, 2014. [Google Scholar]
- Nirenberg, H.I. A simplified method for identifying Fusarium spp. occurring on wheat. Can. J. Bot. 1981, 59, 1599–1609. [Google Scholar] [CrossRef]
- De Vries, R.P.; Burgers, K.; van de Vondervoort, P.; Frisvad, J.C.; Samson, R.A.; Visser, J. A New Black Aspergillus Species, A. vadensis, Is a Promising Host for Homologous and Heterologous Protein Production. Appl. Environ. Microbiol. 2004, 70, 3954–3959. [Google Scholar] [CrossRef]
- King, A.D.; Hocking, A.D.; Pitt, J.I. Dichloran-rose bengal medium for enumeration and isolation of molds from foods. Appl. Environ. Microbiol. 1979, 37, 959–964. [Google Scholar]
- Reasoner, D.J.; Geldreich, E.E. A new medium for the enumeration and subculture of bacteria from potable water. Appl. Environ. Microbiol. 1985, 49, 1–7. [Google Scholar]
- Pitt, J.I.; Hocking, A.D. Fungi and Food Spoilage; Springer: New York, NY, USA, 2009. [Google Scholar] [CrossRef]
- White, T.J.; Bruns, T.; Lee SJ, W.T.; Taylor, J. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In PCR Protocols—A Guide to Methods and Applications; Academic Press: Cambridge, MA, USA, 1990; pp. 315–322. [Google Scholar] [CrossRef]
- Boekhout, T.; Kurtzman, C.P. Principles and Methods Used in Yeast Classification, and an Overview of Currently Accepted Yeast Genera. In Nonconventional Yeasts in Biotechnology; Springer: Berlin/Heidelberg, Germany, 1996; pp. 1–81. [Google Scholar] [CrossRef]
- Glass, N.L.; Donaldson, G.C. Development of primer sets designed for use with the PCR to amplify conserved genes from filamentous ascomycetes. Appl. Environ. Microbiol. 1995, 61, 1323–1330. [Google Scholar]
- Carbone, I.; Kohn, L.M. A method for designing primer sets for speciation studies in filamentous ascomycetes. Mycologia 1999, 91, 553–556. [Google Scholar] [CrossRef]
- Edgar, R.C. MUSCLE: Multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res. 2004, 32, 1792–1797. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular Evolutionary Genetics Analysis Version 7.0 for Bigger Datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef] [PubMed]
- Favero, D.; Furlaneto-Maia, L.; França, E.J.G.; Peggau Góes, H.; Furlaneto, M.C. Hemolytic factor production by clinical isolates of Candida species. Curr. Microbiol. 2014, 68, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Furlaneto, M.C.; Góes, H.P.; Perini, H.F.; dos Santos, R.C.; Furlaneto-Maia, L. How much do we know about hemolytic capability of pathogenic Candida species? Folia Microbiol. 2018, 63, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Buxton, R. Blood Agar Plates and Hemolysis Protocols. American Society for Microbiology, 2005. Available online: https://www.asm.org/getattachment/7ec0de2b-bb16-4f6e-ba07-2aea25a43e76/protocol-2885.pdf (accessed on 20 November 2019).
- Fera, M.T.; La Camera, E.; De Sarro, A. New triazoles and echinocandins: Mode of action, in vitro activity and mechanisms of resistance. Expert Rev. Anti. Infect Ther. 2009, 7, 981–998. [Google Scholar] [CrossRef] [PubMed]
- Perea, S.; Patterson, T.F. Antifungal Resistance in Pathogenic Fungi. Clin. Infect Dis. 2002, 35, 1073–1080. [Google Scholar] [CrossRef]
- Schaller, M.; Borelli, C.; Korting, H.C.; Hube, B. Hydrolytic enzymes as virulence factors of Candida albicans. Mycoses 2005, 48, 365–377. [Google Scholar] [CrossRef]
- Khan, M.S.A.; Ahmad, I.; Aqil, F.; Owais, M.; Shahid, M.; Musarrat, J. Virulence and pathogenicity of fungal pathogens with special reference to Candida albicans. In Combating Fungal Infections; Ahmad, I., Owais, M., Shahid, M., Aqil, F., Eds.; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar] [CrossRef]
- Sepčić, K.; Zalar, P.; Gunde-Cimerman, N. Low water activity induces the production of bioactive metabolites in halophilic and halotolerant fungi. Mar. Drugs 2011, 9, 43–58. [Google Scholar] [CrossRef]
- Donohue, M.; Chung, Y.; Magnuson, M.L.; Ward, M.; Selgrade, M.J.; Vesper, S. Hemolysin chrysolysinTM from Penicillium chrysogenum promotes inflammatory response. Int. J. Hyg. Environ. Health 2005, 208, 279–285. [Google Scholar] [CrossRef]
- Kirtsideli, I.Y.; Vlasov, D.Y.; Abakumov, E.V.; Barantsevich, E.P.; Novozhilov, Y.K.; Krylenkov, V.A.; Sokolov, V.T. Airborne fungi in arctic settlement Tiksi (Russian Arctic, coast of the Laptev Sea). Czech Polar Rep. 2017, 7, 300–310. [Google Scholar] [CrossRef]
- Madrid, C.; Nieto, J.M.; Paytubi, S.; Falconi, M.; Gualerzi, C.O.; Juarez, A. Temperature- and H-NS-dependent regulation of a plasmid-encoded virulence operon expressing Escherichia coli hemolysin. J. Bacteriol. 2002, 184, 5058–5066. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, H.T.; Barton, H.A. Comparison of the white-nose syndrome agent Pseudogymnoascus destructans to cave-dwelling relatives suggests reduced saprotrophic enzyme activity. PLoS ONE 2014, 9, e86437. [Google Scholar] [CrossRef] [PubMed]
- Nayak, A.P.; Green, B.J.; Beezhold, D.H. Fungal hemolysins. Med. Mycol. 2013, 51, 1–16. [Google Scholar] [CrossRef]
- Odds, F.C. Candida and Candidosis: A Review and Bibliography; Bailliere Tindall: Philadelphia, PA, USA, 1998. [Google Scholar]
- Vesper, S.J.; Jo Vesper, M. Possible role of fungal hemolysins in sick building syndrome. Adv. Appl. Microbiol. 2004, 55, 191–213. [Google Scholar]
- Rementeria, A.; López-Molina, N.; Ludwig, A.; Vivanco, A.B.; Bikandi, J.; Pontón, J.; Garaizar, J. Genes and molecules involved in Aspergillus fumigatus virulence. Rev. Iberoam. Micol. 2005, 22, 1–23. [Google Scholar] [CrossRef]
- Calera, J.A.; Haas, H. Cations (Zn, Fe). In Aspergillus fumigatus and Aspergillosis; Latgé, J.-P., Steinbach, W.J., Eds.; American Society of Microbiology: New York, NY, USA, 2009. [Google Scholar] [CrossRef]
- Chen, C.; Pande, K.; French, S.D.; Tuch, B.B.; Noble, S.M. An iron homeostasis regulatory circuit with reciprocal roles in Candida albicans commensalism and pathogenesis. Cell Host. Microbe 2011, 10, 118–135. [Google Scholar] [CrossRef]
- Berne, S.; Križaj, I.; Pohleven, F.; Turk, T.; Maček, P.; Sepčić, K. Pleurotus and Agrocybe hemolysins, new proteins hypothetically involved in fungal fruiting. Biochim. Biophys. Acta-Gen Subj. 2002, 1570, 153–159. [Google Scholar] [CrossRef]
- Lakkireddy, K.K.R.; Navarro-González, M.; Velagapudi, R.; Kües, U. Proteins Expressed During Hyphal Aggregation for Fruiting Body Formation in Basidiomycetes. In Proceedings of the 7th International Conference on Mushroom Biology and Mushroom Products (ICMBMP7), Arcachon, France, 4–7 October 2011; pp. 82–94. [Google Scholar]
- Chi, Z.; Wang, F.; Chi, Z.; Yue, L.; Liu, G.; Zhang, T. Bioproducts from Aureobasidium pullulans, a biotechnologically important yeast. Appl. Microbiol. Biotechnol. 2009, 82, 793–804. [Google Scholar] [CrossRef]
- Rebolj, K.; Ulrih, N.P.; Maček, P.; Sepčić, K. Steroid structural requirements for interaction of ostreolysin, a lipid-raft binding cytolysin, with lipid monolayers and bilayers. Biochim. Biophys. Acta 2006, 1758, 1662–1670. [Google Scholar] [CrossRef][Green Version]
- Khawcharoenporn, T.; Apisarnthanarak, A.; Mundy, L.M. Non-neoformans cryptococcal infections: A systematic review. Infection 2007, 35, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.; Sehring, M.; Chambers, J.; Patel, P. Perspectives on non-neoformans cryptococcal opportunistic infections. J. Commun. Hosp. Intern. Med. Perspect. 2017, 7, 214–217. [Google Scholar] [CrossRef] [PubMed]
- Ghajari, A.; Lotfali, E.; Norouzi, M.; Arab-Mazar, Z. First report of Vulvovaginitis due to Cryptococcus magnus in Iran. Curr. Med. Mycol. 2018, 4, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Kano, R.; Hosaka, S.; Hasegawa, A. First isolation of Cryptococcus magnus from a cat. Mycopathologia 2004, 157, 263–264. [Google Scholar] [CrossRef] [PubMed]
- Poth, T.; Seibold, M.; Werckenthin, C.; Hermanns, W. First report of a Cryptococcus magnus infection in a cat. Med. Mycol. 2010, 48, 1000–1004. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Pedroso, R.; Ferreira, J.C.; Candido, R.C. In Vitro susceptibility to antifungal agents of environmental Cryptococcus spp. isolated in the city of Ribeirão Preto, São Paulo, Brazil. Mem. Inst. Oswaldo Cruz 2006, 101, 239–243. [Google Scholar] [CrossRef]
- Bernal-Martinez, L.; Gomez-Lopez, A.; Castelli, M.V.; Mesa-Arango, A.C.; Zaragoza, O.; Rodriguez-Tudela, J.L.; Cuenca-Estrella, M. Susceptibility profile of clinical isolates of non-Cryptococcus neoformans/non-Cryptococcus gattii Cryptococcus species and literature review. Med. Mycol. 2010, 48, 90–96. [Google Scholar] [CrossRef]
- Falces-Romero, I.; Cendejas-Bueno, E.; Romero-Gómez, M.P.; García-Rodríguez, J. Isolation of Rhodotorula mucilaginosa from blood cultures in a tertiary care hospital. Mycoses 2018, 61, 35–39. [Google Scholar] [CrossRef]
- Gomez-Lopez, A.; Mellado, E.; Rodriguez-Tudela, J.L.; Cuenca-Estrella, M. Susceptibility profile of 29 clinical isolates of Rhodotorula spp. and literature review. J. Antimicrob. Chemother. 2005, 55, 312–316. [Google Scholar] [CrossRef]
- Capoor, M.R.; Aggarwal, S.; Raghvan, C.; Gupta, D.K.; Jain, A.K.; Chaudhary, R. Clinical and microbiological characteristics of Rhodotorula mucilaginosa infections in a tertiary-Care facility. Indian J. Med. Microbiol. 2014, 32, 304–309. [Google Scholar] [CrossRef]
- Chan, G.F.; Puad, M.S.A.; Chin, C.F.; Abdul Rashid, N.A. Emergence of Aureobasidium pullulans as human fungal pathogen and molecular assay for future medical diagnosis. Folia Microbiol. 2011, 56, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Gostinčar, C.; Ohm, R.A.; Kogej, T.; Sonjak, S.; Turk, M.; Zajc, J.; Zalar, P.; Grube, M.; Sun, H.; Han, J.; et al. Genome sequencing of four Aureobasidium pullulans varieties: Biotechnological potential, stress tolerance, and description of new species. BMC Genom. 2014, 15. [Google Scholar] [CrossRef] [PubMed]
- Joshi, A.; Singh, R.; Shah, M.S.; Umesh, S.; Khattry, N. Subcutaneous mycosis and fungemia by Aureobasidium pullulans: A rare pathogenic fungus in a post allogeneic BM transplant patient. Bone Marrow Trans. 2010, 45, 203–204. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.R.; Johns, S.; Stark, P.; Fierer, J. Successful treatment of Aureobasidium pullulans central catheter-related fungemia and septic pulmonary emboli. IDCases 2017, 10, 65–67. [Google Scholar] [CrossRef]
- Nogueira, R.; Melo, N.; Novais, E.; Bastos, H.; Martins, N.; Delgado, L.; Morais, A.; Mota, P. Hypersensitivity pneumonitis: Antigen diversity and disease implications. Pulmonology 2019, 25, 97–108. [Google Scholar] [CrossRef]
- Chowdhary, A.; Kathuria, S.; Agarwal, K.; Sachdeva, N.; Singh, P.K.; Jain, S.; Meis, J.F. Voriconazole-Resistant Penicillium oxalicum: An Emerging Pathogen in Immunocompromised Hosts. Open Forum Infect. Dis. 2014. [Google Scholar] [CrossRef]
- Sharma, C.; Chowdhary, A. Molecular bases of antifungal resistance in filamentous fungi. Int. J. Antimicrob. Agents 2017, 50, 607–616. [Google Scholar] [CrossRef]
- Espinel-Ingroff, A.; Arendrup, M.C.; Pfaller, M.A.; Bonfietti, L.X.; Bustamante, B.; Canton, E.; Chryssanthou, E.; Cuenca-Estrella, M.; Dannaoui, E.; Fothergill, A.; et al. Interlaboratory variability of caspofungin MICs for Candida spp. using CLSI and EUCAST methods: Should the clinical laboratory Be testing this agent? Antimicrob. Agents Chemother. 2013, 57, 5836–5842. [Google Scholar] [CrossRef]
| Sampling Area | Sampling Location | Sample Type | Sampling Year | GPS Coordinates |
|---|---|---|---|---|
| Kangerlussuaq, Greenland | Greenland Ice Sheet | Snow | 2016/2017 | 67°04′43″ N 49°20′29″ W |
| Dark ice | ||||
| Clear ice | ||||
| Supraglacial water | ||||
| Russell Glacier | Air | 2018 | 67°05′45″ N 50°13′00″ W | |
| Ny-Ålesund, Svalbard | Midtre Lovénbreen | Subglacial ice | 2017 | 78°53′37″ N 12°04′13″ E |
| Glacial meltwater | 78°53′25″ N 12°03′15″ E | |||
| Vestre Brøggerbreen | Subglacial ice | 78°54′55″ N 11°45′48″ E | ||
| Pedersenbreen | Subglacial ice | 78°52′46″ N 12°17′57″ E |
| Isolate (EXF-) | Species | Phylum | Sample | Sample Location | Sampling Year | Isolation Media * | GenBank Accession Number |
|---|---|---|---|---|---|---|---|
| 11445 | Penicillium bialowiezense-like | Ascomycota | Dark ice | Greenland Ice Sheet | 2016 | DG18 | MN356456 |
| 12407 | Vishniacozyma victoriae | Basidiomycota | Dark ice | Greenland Ice Sheet | 2017 | R2A | MK454786 |
| 12427 | Cladosporium sp. | Ascomycota | Dark ice | Greenland Ice Sheet | 2017 | DG18 | MK460331 |
| 12432 | Aureobasidium pullulans | Ascomycota | Snow | Greenland Ice Sheet | 2017 | SNA | MK460317 |
| 12443 | Penicillium chrysogenum | Ascomycota | Snow | Greenland Ice Sheet | 2017 | R2A | MK460375 |
| 12448 | Preussia sp. | Ascomycota | Snow | Greenland Ice Sheet | 2017 | R2A | MK460381 |
| 12518 | Mrakia sp. | Basidiomycota | Dark ice | Greenland Ice Sheet | 2017 | R2A | MK454832 |
| 12523 | Phenoliferia glacialis | Basidiomycota | Supraglacial water | Greenland Ice Sheet | 2017 | R2A | MK454852 |
| 12580 | Filobasidium magnum | Basidiomycota | Subglacial ice | Svalbard—Midre Lovenbreen | 2017 | DRBC | MK670462 |
| 12581 | Naganishia albida | Basidiomycota | Subglacial ice | Svalbard—Midre Lovenbreen | 2017 | MM | MK670463 |
| 12591 | Glaciozyma watsonii | Basidiomycota | Subglacial ice | Svalbard—Vestre Broggerbreen | 2017 | SNA | MK670501 |
| 12629 | Penicillium crustosum | Ascomycota | Subglacial ice | Svalbard—Pedersenbreen | 2017 | MM | MK671620 |
| 12639 | Pseudogymnoascus sp. | Ascomycota | Subglacial ice | Svalbard—Vestre Broggerbreen | 2017 | SNA | MK671632 |
| 12718 | Rhodotorula svalbardensis pro. tem. | Basidiomycota | Clear ice | Greenland Ice Sheet | 2017 | DRBC | MK460392 |
| 12875 | Comoclathris sp. | Ascomycota | Snow | Greenland Ice Sheet | 2017 | R2A | MK460354 |
| 12951 | Phenoliferia psychrophenolica | Basidiomycota | Subglacial ice | Svalbard—Midre Lovenbreen | 2017 | DG18 | MK670452 |
| 12990 | Venturia sp. | Ascomycota | Subglacial ice | Svalbard—Pedersenbreen | 2017 | R2A | MK671645 |
| 13072 | Articulospora sp. | Ascomycota | Dark ice | Greenland Ice Sheet | 2016 | DG18 | MN356457 |
| 13083 | Oleoguttula mirabilis | Ascomycota | Clear ice | Greenland Ice Sheet | 2017 | R2A | MK454839 |
| 13100 | Neocucurbitaria sp. | Ascomycota | Snow | Greenland Ice Sheet | 2017 | SNA | MK460385 |
| 13102 | Glaciozyma-related taxon | Basidiomycota | Glacial meltwater | Svalbard—Midre Lovenbreen | 2017 | MM | MK670451 |
| 13131 | Dothiora sp. | Ascomycota | Snow | Greenland Ice Sheet | 2017 | MM | MK460359 |
| 13607 | Rhodotorula mucilaginosa | Basidiomycota | Air | Greenland—Russell glacier | 2018 | DG18 | MN356458 |
| 13647 | Aureobasidium melanogenum | Ascomycota | Air | Greenland—Russell glacier | 2018 | DG18 | MN356459 |
| EXF- | Species | Phylum | MIC (μg/mL) | |||||
|---|---|---|---|---|---|---|---|---|
| FL | CS | VO | MYC | KE | AND | |||
| 13072 | Articulospora sp. | Ascomycota | 256 | 0.032 | 0.004 | 0.012 | 0.002 | 0.023 |
| 13647 | Aureobasidium melanogenum | Ascomycota | 16 | 0.25 | 0.38 | 0.25 | 0.5 | 0.125 |
| 12432 | Aureobasidium pullulans | Ascomycota | 48 | 0.38 | 0.094 | 0.094 | 0.19 | 0.38 |
| 14635 CTRL | Candida albicans | Ascomycota | 0.032 | 0.064 | ≤0.002 | 0.016 | ≤0.002 | 0.008 |
| 12427 | Cladosporium sp. | Ascomycota | 16 | 2 | 0.023 | 0.008 | 0.006 | 0.004 |
| 12875 | Comoclathris sp. | Ascomycota | 256 | 0.125 | 0.38 | 0.064 | 0.5 | 0.006 |
| 13131 | Dothiora sp. | Ascomycota | 0.38 | 0.064 | 0.003 | 0.006 | 0.003 | 0.002 |
| 13100 | Neocucurbitaria sp. | Ascomycota | 256 | 32 | 0.002 | 0.006 | 0.004 | 0.002 |
| 13083 | Oleoguttula mirabilis | Ascomycota | 256 | 0.002 | 0.002 | 0.002 | 0.002 | 0.002 |
| 11445 | Penicillium bialowiezense-like | Ascomycota | 256 | 0.016 | 1.5 | 0.002 | 0.38 | 0.002 |
| 12443 | Penicillium chrysogenum | Ascomycota | 256 | 0.016 | 0.5 | 0.002 | 2 | 0.002 |
| 12629 | Penicillium crustosum | Ascomycota | 256 | 0.5 | 0.25 | 0.008 | 12 | 0.008 |
| 12448 | Preussia sp. | Ascomycota | 256 | 0.125 | 0.19 | 0.004 | 0.032 | 0.016 |
| 12639 | Pseudogymnoascus sp. | Ascomycota | 8 | 1 | 0.094 | 0.125 | 0.38 | 0.25 |
| 12990 | Venturia sp. | Ascomycota | 64 | 0.002 | 0.016 | 0.125 | 0.032 | 0.032 |
| 12580 | Filobasidium magnum | Basidiomycota | 4 | NT | 0.032 | NT | 0.023 | NT |
| 13102 | Glaciozyma-related taxon | Basidiomycota | 0.25 | NT | 0.002 | NT | 0.002 | NT |
| 12591 | Glaciozyma watsonii | Basidiomycota | 256 | NT | 0.002 | NT | 0.002 | NT |
| 12518 | Mrakia sp. | Basidiomycota | NG | NG | NG | NG | NG | NG |
| 12581 | Naganishia albida | Basidiomycota | 64 | NT | 2 | NT | 0.047 | NT |
| 12523 | Phenoliferia glacialis | Basidiomycota | 0.016 | NT | 0.002 | NT | 0.004 | NT |
| 12951 | Phenoliferia psychrophenolica | Basidiomycota | 0.047 | R | 0.002 | R | 0.002 | R |
| 12718 | Rhodotorula svalbardensis pro. tem. | Basidiomycota | NG | NG | NG | NG | NG | NG |
| 13607 | Rhodotorula mucilaginosa | Basidiomycota | 256 | 32 | 0.032 | 32 | 0.032 | 32 |
| 12407 | Vishniacozyma victoriae | Basidiomycota | 1 | NT | 0.016 | NT | 0.032 | NT |
| Range | 0.016–256 | 0.002–32 | 0.002–2 | 0.002–32 | 0.002–12 | 0.002–32 | ||
| Geometric mean MIC | 114.8 | 0.263 | 0.672 | 4.57 | 2.24 | 2.35 | ||
| MIC50 | 64 | 0.032 | 0.032 | 0.125 | 0.008 | 0.008 | ||
| MIC90 | 256 | 0.5 | 0.5 | 32 | 0.25 | 0.5 | ||
| EXF- | Species | Phylum | Hemolysis in Bovine Blood | |
|---|---|---|---|---|
| 15 °C | 37 °C | |||
| 11445 | Penicillium bialowiezense-like | Ascomycota | α/β − | NG |
| 12407 | Vishniacozyma victoriae | Basidiomycota | γ | NG |
| 12427 | Cladosporium sp. | Ascomycota | γ | NG |
| 12432 | Aureobasidium pullulans | Ascomycota | β | NG |
| 12443 | Penicillium chrysogenum | Ascomycota | α − | γ − (little growth) |
| 12448 | Preussia sp. | Ascomycota | α | NG |
| 12518 | Mrakia sp. | Basidiomycota | γ | NG |
| 12523 | Phenoliferia glacialis | Basidiomycota | γ | NG |
| 12580 | Filobasidium magnum | Basidiomycota | γ | NG |
| 12581 | Naganishia albida | Basidiomycota | γ | γ − (little growth) |
| 12591 | Glaciozyma watsonii | Basidiomycota | γ | NG |
| 12629 | Penicillium crustosum | Ascomycota | γ | NG |
| 12639 | Pseudogymnoascus sp. | Ascomycota | α * | NG |
| 12718 | Rhodotorula svalbardensis pro. tem. | Basidiomycota | NG | NG |
| 12875 | Comoclathris sp. | Ascomycota | γ | NG |
| 12951 | Phenoliferia psychrophenolica | Basidiomycota | α − | NG |
| 12990 | Venturia sp. | Ascomycota | γ | NG |
| 13072 | Articulospora sp. | Ascomycota | γ | NG |
| 13083 | Oleoguttula mirabilis | Ascomycota | α | NG |
| 13100 | Neocucurbitaria sp. | Ascomycota | α - | NG |
| 13102 | Glaciozyma-related taxon | Basidiomycota | γ | NG |
| 13131 | Dothiora sp. | Ascomycota | γ | NG |
| 13607 | Rhodotorula mucilaginosa | Basidiomycota | α - | β |
| 13647 | Aureobasidium melanogenum | Ascomycota | β | γ − (little growth) |
| 14635 CTRL | Candida albicans | Ascomycota | γ | β |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perini, L.; Mogrovejo, D.C.; Tomazin, R.; Gostinčar, C.; Brill, F.H.H.; Gunde-Cimerman, N. Phenotypes Associated with Pathogenicity: Their Expression in Arctic Fungal Isolates. Microorganisms 2019, 7, 600. https://doi.org/10.3390/microorganisms7120600
Perini L, Mogrovejo DC, Tomazin R, Gostinčar C, Brill FHH, Gunde-Cimerman N. Phenotypes Associated with Pathogenicity: Their Expression in Arctic Fungal Isolates. Microorganisms. 2019; 7(12):600. https://doi.org/10.3390/microorganisms7120600
Chicago/Turabian StylePerini, Laura, Diana C. Mogrovejo, Rok Tomazin, Cene Gostinčar, Florian H. H. Brill, and Nina Gunde-Cimerman. 2019. "Phenotypes Associated with Pathogenicity: Their Expression in Arctic Fungal Isolates" Microorganisms 7, no. 12: 600. https://doi.org/10.3390/microorganisms7120600
APA StylePerini, L., Mogrovejo, D. C., Tomazin, R., Gostinčar, C., Brill, F. H. H., & Gunde-Cimerman, N. (2019). Phenotypes Associated with Pathogenicity: Their Expression in Arctic Fungal Isolates. Microorganisms, 7(12), 600. https://doi.org/10.3390/microorganisms7120600







