Pathogenicity in Chicken Anemia Virus with Eimeria tenella: Concurrent Co-Infection and Secondary Eimeria tenella Infection
Abstract
1. Introduction
2. Materials and Methods
2.1. Chickens and Housing
2.2. CAV Propagation and TCID50 Determination
2.3. Isolation and Propagation of E. tenella
2.4. Experimental Design
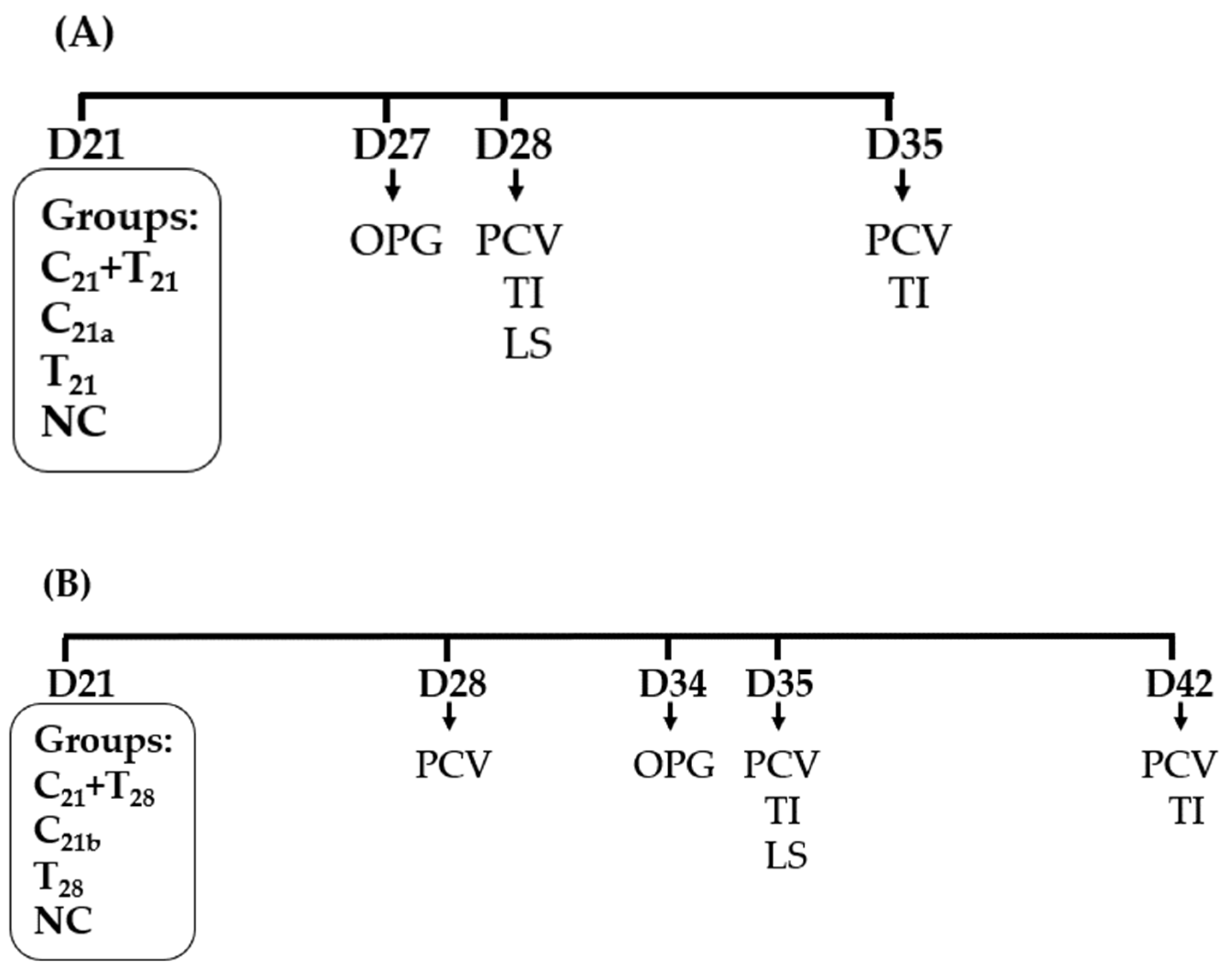
2.4.1. Trial A: Concurrent Co-Infection
2.4.2. Trial B: Secondary E. tenella Infection
2.5. Ceca Lesion Assessment
2.6. Fecal Oocyst Output
2.7. Hematocrit Determination
2.8. Thymus Weight to Body Weight Ratio
2.9. Statistical Analysis
3. Results
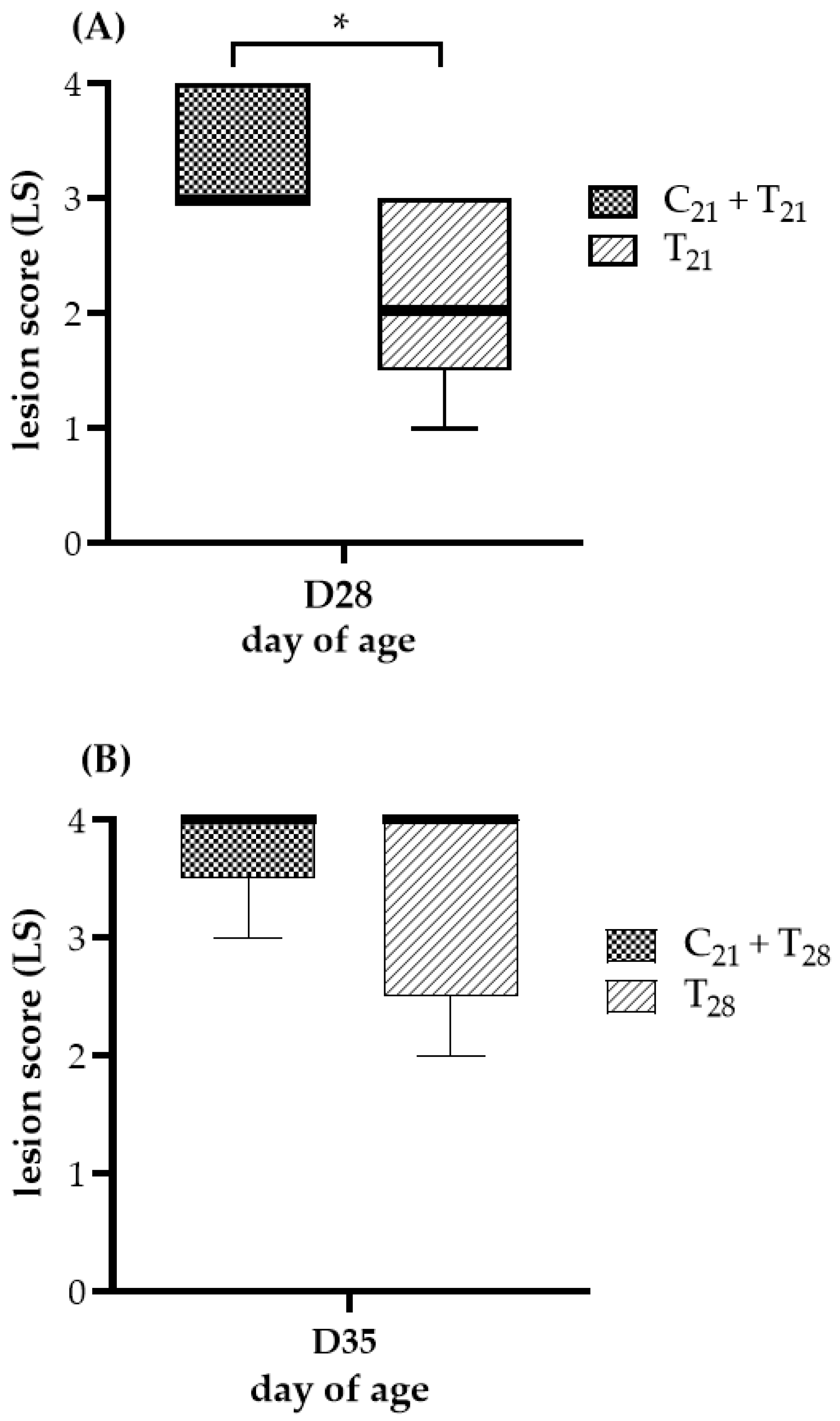
3.1. Potential Ceca Lesion Variability in CAV and E. tenella Co-Infected Groups
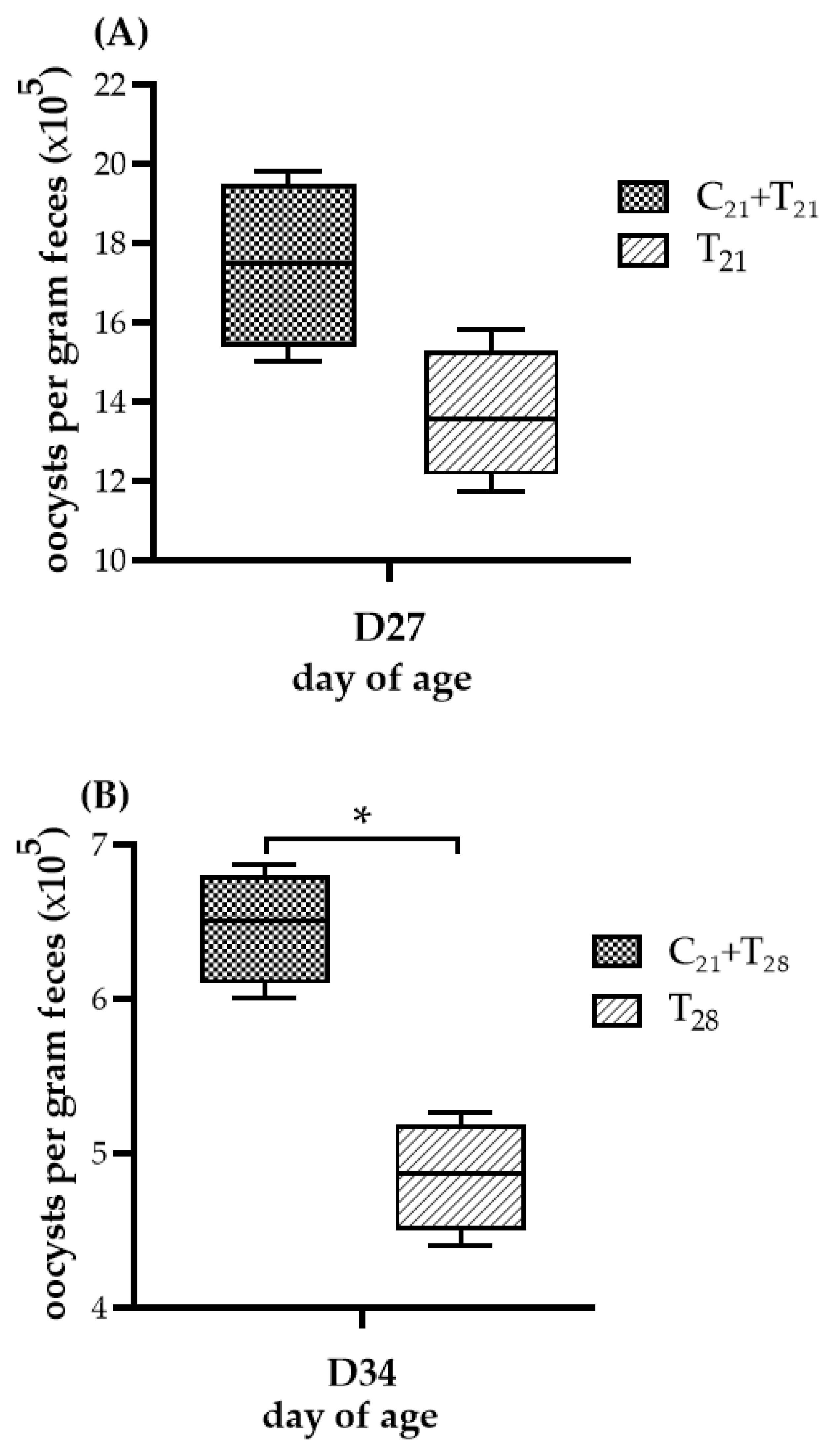
3.2. Oocyst Counts Observed in Dual Infection with CAV and E. tenella
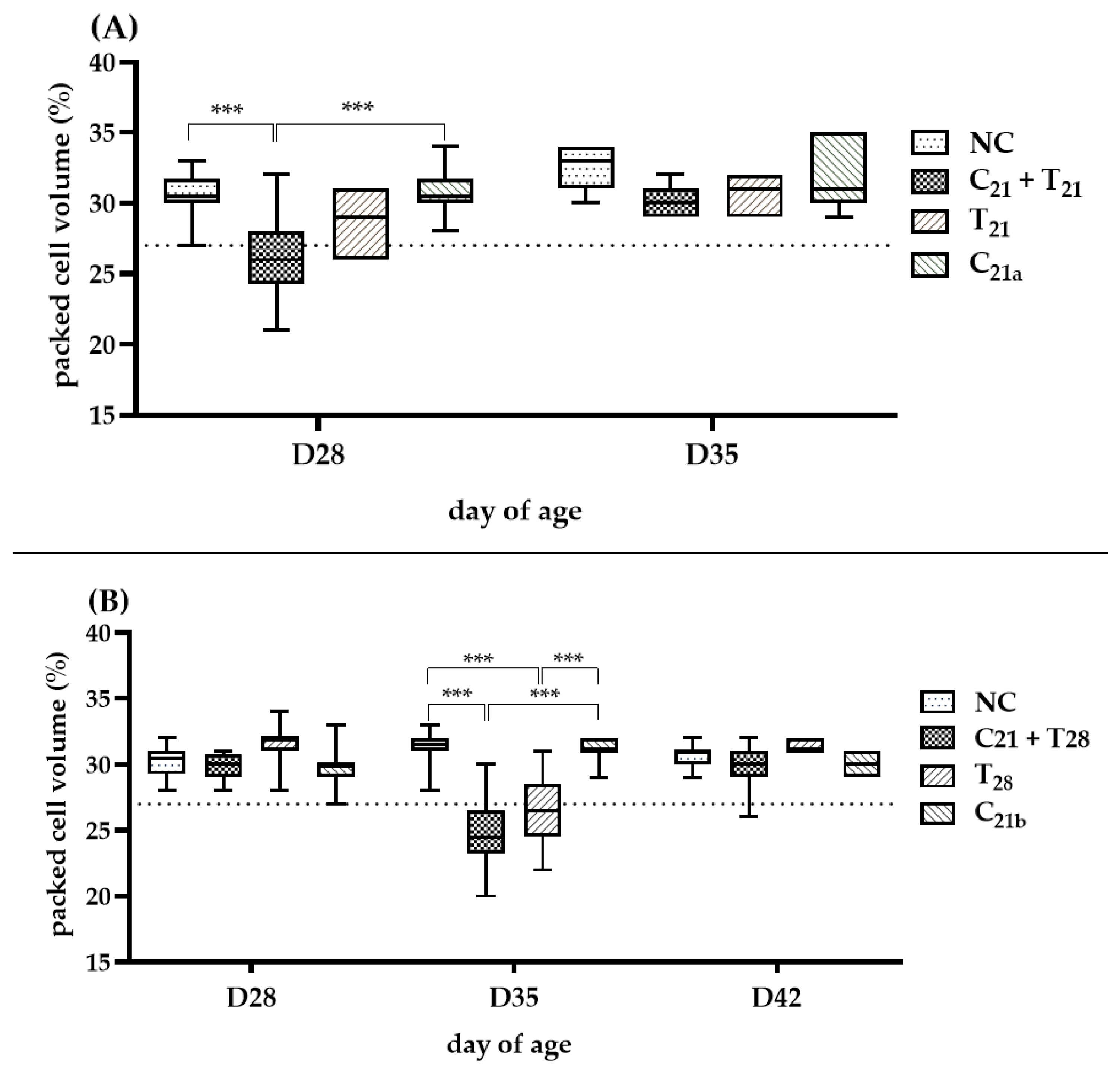
3.3. Potential Interactions of Concurrent and Secondary Infection on Severity of Anemia
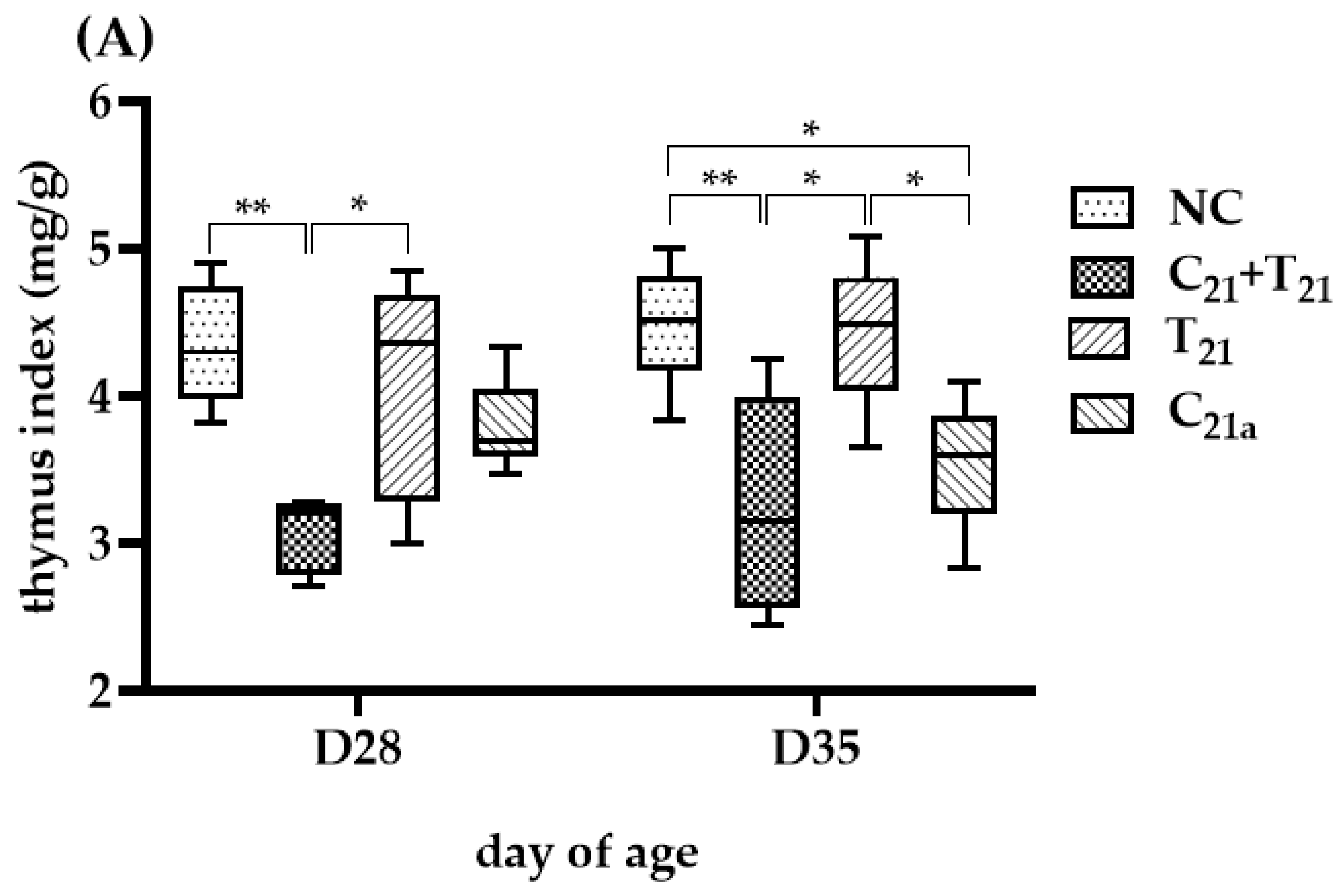
3.4. Variable Thymus Atrophy Under Dual Infection with CAV and E. tenella
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yuasa, N.; Taniguchi, T.; Yoshida, I. Isolation and some characteristics of an agent inducing anemia in chicks. Avian Dis. 1979, 17, 366–385. [Google Scholar] [CrossRef]
- McConnell, C.D.G.; Adair, B.M.; McNulty, M.S. Effects of chicken anemia virus on cell-mediated immune function in chickens exposed to the virus by a natural route. Avian Dis. 1993, 37, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Swayne, D.E.; Boulianne, M.; Logue, C.M.; McDougald, L.R.; Nair, V.; Suarez, D.L. Chicken Infectious Anemia and Circovirus Infections in Commercial Flocks. In Diseases of Poultry, 14th ed.; Santen, V.L., Schat, K.A., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2020; pp. 284–306. [Google Scholar]
- Rodgers, J.D.; McCullagh, J.J.; McNamee, P.T.; Smyth, J.A.; Ball, H. The anti-nuclease humoral immune response of broiler chickens exposed to Staphylococcus aureus, infectious bursal disease virus and chicken anaemia virus in an experimental model for bacterial chondronecrosis and osteomyelitis. Avian Dis. 2006, 35, 302–308. [Google Scholar] [CrossRef][Green Version]
- Suohu, S.; Balasubramaniam, G.; Arulmozhi, A.; Gopalakrishnamurthy, T.; Raja, A. Pathological studies on chicken infectious anaemia and concurrent infections in layer flocks of Namakkal, Tamil Nadu. Indian J. Anim. Sci. 2024, 94, 739–745. [Google Scholar] [CrossRef]
- Hoerr, F. Clinical aspects of immunosuppression in poultry. Avian Dis. 2010, 54, 2–15. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, K.; Imai, K.; Van Dong, H.; Ogawa, H.; Suzutou, M.; Linn, S.H.; Kurokawa, A.; Yamamoto, Y. Pathological and virological analysis of concurrent disease of chicken anemia virus infection and infectious bronchitis in Japanese native chicks. J. Vet. Med. Sci. 2020, 82, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Toro, H.; Van Santen, V.; Hoerr, F.; Breedlove, C. Effects of chicken anemia virus and infectious bursal disease virus in commercial chickens. Avian Dis. 2009, 53, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Haridy, M.; Goryo, M.; Sasaki, J.; Okada, K. Pathological and immunohistochemical study of chickens with co-infection of Marek’s disease virus and chicken anaemia virus. Avian Pathol. 2009, 38, 469–483. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Li, W.; Nie, Y.; Chen, S.; Li, H.; Zhang, X.; Xie, Q.; Chen, W. Synergy of subgroup J avian leukosis virus and chicken infectious anemia virus enhances the pathogenicity in chickens. Microorganisms 2024, 12, 740. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Gao, W.; Chang, J.; Liu, J.; Huang, Z.; Sun, W.; Song, Y.; Li, X. Co-Infection of Chicken Infectious Anemia Virus and Fowl Adenovirus Serotype E8b Increases Mortality in Chickens. Viruses 2025, 17, 620. [Google Scholar] [CrossRef] [PubMed]
- McNeilly, F.; Smyth, J.; Adair, B.; McNulty, M. Synergism between chicken anemia virus (CAV) and avian reovirus following dual infection of 1-day-old chicks by a natural route. Avian Dis. 1995, 532–537. [Google Scholar] [CrossRef]
- El-Azm, K.I.A.; Hamed, M.F.; Matter, A.; Rozmyslowicz, T.; Rahman, S.A.E.; Gaulton, G.N.; Bau, H.H.; El-Tholoth, M. Molecular and pathological characterization of natural co-infection of poultry farms with the recently emerged Leucocytozoon caulleryi and chicken anemia virus in Egypt. Trop. Anim. Health Prod. 2022, 54, 91. [Google Scholar] [CrossRef] [PubMed]
- Silveira, P.; Marin, S.Y.; Moreira, P.A.; Tocantins, B.B.; Lacorte, G.; Paixao, T.A.; Martins, N.R.; Braga, E.M. Interactions of Plasmodium juxtanucleare and chicken anaemia virus: Establishing a model. Parasitology 2013, 140, 1777–1788. [Google Scholar] [CrossRef] [PubMed]
- Hornok, S.; Heijmans, J.; Békési, L.; Peek, H.; Dobos-Kovacs, M.; Drén, C.N.; Varga, I. Interaction of chicken anaemia virus and Cryptosporidium baileyi in experimentally infected chickens. Vet. Parasitol. 1998, 76, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Blake, D.P.; Knox, J.; Dehaeck, B.; Huntington, B.; Rathinam, T.; Ravipati, V.; Ayoade, S.; Gilbert, W.; Adebambo, A.O.; Jatau, I.D. Re-calculating the cost of coccidiosis in chickens. Vet. Res. 2020, 51, 115. [Google Scholar] [CrossRef] [PubMed]
- Cantacessi, C.; Riddell, S.; Morris, G.M.; Doran, T.; Woods, W.G.; Otranto, D.; Gasser, R.B. Genetic characterization of three unique operational taxonomic units of Eimeria from chickens in Australia based on nuclear spacer ribosomal DNA. Vet. Parasitol. 2008, 152, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Blake, D.P.; Vrba, V.; Xia, D.; Jatau, I.D.; Spiro, S.; Nolan, M.J.; Underwood, G.; Tomley, F.M. Genetic and biological characterisation of three cryptic Eimeria operational taxonomic units that infect chickens (Gallus gallus domesticus). Int. J. Parasitol. 2021, 51, 621–634. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, S.E.; van Diemen, P.M.; Martineau, H.; Stevens, M.P.; Tomley, F.M.; Stabler, R.A.; Blake, D.P. Impact of Eimeria tenella coinfection on Campylobacter jejuni colonization of the chicken. Infect. Immun. 2019, 87, 10–1128. [Google Scholar] [CrossRef] [PubMed]
- Lien, Y.-Y.; Shyur, L.-F.; Cheng, Y.-B.; Chang, M.-T.; Chang, C.-T.; Chen, Y.-H.; Lai, G.-H.; Liao, H.-Y.; Cheng, M.-C. Trifolium pratense as a novel phytogenic supplement, is an anticoccidial agent in chickens. Poult. Sci. 2024, 103, 104064. [Google Scholar] [CrossRef] [PubMed]
- Conway, D.P.; McKenzie, M.E. Poultry Coccidiosis: Diagnostic and Testing Procedures, 3rd ed.; John Wiley & Sons: Iowa, IA, USA, 2007; pp. 7–15. [Google Scholar]
- Mesa-Pineda, C.; Navarro-Ruíz, J.L.; López-Osorio, S.; Chaparro-Gutiérrez, J.J.; Gómez-Osorio, L.M. Chicken coccidiosis: From the parasite lifecycle to control of the disease. Front. Vet. Sci. 2021, 8, 787653. [Google Scholar] [CrossRef] [PubMed]
- Swayne, D.E.; Boulianne, M.; Logue, C.M.; McDougald, L.R.; Nair, V.; Suarez, D.L. Protozoal Infections. In Diseases of Poultry, 14th ed.; Hector, M., Cervantes, L.R.M., Jenkins, M.C., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2020; pp. 1193–1212. [Google Scholar]
- Pietruk, K.; Karamon, J.; Jedziniak, P.; Tokarzewski, S.; Olejnik, M.J.A. Influence of Eimeria spp. and Clostridium perfringens infection on growth performance and toltrazuril residues in chickens. Animals 2025, 15, 216. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.K.; AbuOun, M.; Cawthraw, S.A.; Humphrey, T.J.; Rothwell, L.; Kaiser, P.; Barrow, P.A.; Jones, M.A. Campylobacter colonization of the chicken induces a proinflammatory response in mucosal tissues. FEMS Immunol. Med. Microbiol. 2008, 54, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-L.; Zhao, X.-Y.; Zhao, G.-X.; Huang, H.-B.; Li, H.-R.; Shi, C.-W.; Yang, W.-T.; Jiang, Y.-L.; Wang, J.-Z.; Ye, L.-P. Dissection of the cecal microbial community in chickens after Eimeria tenella infection. Parasit Vectors 2020, 13, 56. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Rehman, M.U.; He, Y.; Li, A.; Jian, F.; Zhang, L.; Huang, S. Exploring the interplay between Eimeria spp. infection and the host: Understanding the dynamics of gut barrier function. Vet. Q. 2025, 45, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Tongkamsai, S.; Boobphahom, S.; Apphaicha, R.; Chansiripornchai, N. Prevalence and anticoccidial drug sensitivity of Eimeria tenella isolated from commercial broiler farms in Thailand. Vet. World 2025, 18, 1561–1570. [Google Scholar] [CrossRef]
- Liao, S.; Lin, X.; Zhou, Q.; Wang, Z.; Yan, Z.; Wang, D.; Su, G.; Li, J.; Lv, M.; Hu, J. Epidemiological investigation of coccidiosis and associated risk factors in broiler chickens immunized with live anticoccidial vaccines in China. Front. Vet. Sci. 2024, 11, 1375026. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Xiang, Q.; Li, M.; Sun, X.; Lu, M.; Yan, R.; Song, X.; Li, X. Pathogenic effects of single or mixed infections of Eimeria mitis, Eimeria necatrix, and Eimeria tenella in chickens. Vet. Sci. 2022, 9, 657. [Google Scholar] [CrossRef] [PubMed]
- Yuasa, N. Effect of chemicals on the infectivity of chicken anaemia virus. Avian Pathol. 1992, 21, 315–319. [Google Scholar] [CrossRef] [PubMed]
- You, M.J. Suppression of Eimeria tenella sporulation by disinfectants. Korean J. Parasitol. 2014, 52, 435–438. [Google Scholar] [CrossRef] [PubMed]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Lei, C.; Yang, J.; Hu, J.; Sun, X. On the calculation of TCID 50 for quantitation of virus infectivity. Virol. Sin. 2021, 36, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Molan, A.L.; Liu, Z.; De, S. Effect of pine bark (Pinus radiata) extracts on sporulation of coccidian oocysts. Folia Parasit. 2009, 56, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.; Reid, W.M. Anticoccidial drugs: Lesion scoring techniques in battery and floor-pen experiments with chickens. Exp. Parasitol. 1970, 28, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.; Caldwell, D.J.; Klein, J.; Coppedge, J.; Pohl, S.; Fitz-Coy, S.; Lee, J.T. Eimeria tenella oocyst shedding and output in cecal or fecal contents following experimental challenge in broilers. Poult. Sci. 2011, 90, 990–995. [Google Scholar] [CrossRef] [PubMed]
- Tongkamsai, S.; Lee, M.-S.; Tsai, Y.-L.; Chung, H.-H.; Lai, G.-H.; Cheng, J.-H.; Cheng, M.-C.; Lien, Y.-Y. Oral inoculation of specific-pathogen-free chickens with chicken anemia virus induces dose-dependent viremia and transient anemia. Pathogens 2019, 8, 141. [Google Scholar] [CrossRef] [PubMed]
- Tongkamsai, S.; Lee, M.S.; Cheng, M.C.; Chaung, H.C.; Tsai, Y.L.; Lien, Y.Y. Persistent infection with chicken anemia virus in 3-week-old chickens induced by inoculation of the virus by the natural route. Pathogens 2019, 8, 48. [Google Scholar] [CrossRef] [PubMed]
- Kotob, M.H.; Menanteau-Ledouble, S.; Kumar, G.; Abdelzaher, M.; El-Matbouli, M. The impact of co-infections on fish: A review. Vet. Res. 2017, 47, 98. [Google Scholar] [CrossRef] [PubMed]
- Bakaletz, L.O. Developing animal models for polymicrobial diseases. Nat. Rev. Microbiol. 2004, 2, 552–568. [Google Scholar] [CrossRef] [PubMed]
- Karvonen, A.; Jokela, J.; Laine, A.-L. Importance of sequence and timing in parasite coinfections. Trends Parasitol. 2019, 35, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.G.; Ley, D.H.; Barnes, H.J.; Gerig, T.M.; Corbett, W.T. Experimental cryptosporidiosis and infectious bursal disease virus infection of specific-pathogen-free chickens. Avian Dis. 1988, 32, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, M.; Awais, M.M.; Anwar, M.I.; Ehtisham-ul-Haque, S.; Nasir, A.; Saleemi, M.K.; Ashraf, K. The effect of infection with mixed Eimeria species on hematology and immune responses following Newcastle disease and infectious bursal disease booster vaccination in broilers. Vet. Q. 2015, 35, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Smyth, J.A.; Moffett, D.A.; Connor, T.J.; McNulty, M.S. Chicken anaemia virus inoculated by the oral route causes lymphocyte depletion in the thymus in 3-week-old and 6-week-old chickens. Avian Pathol. 2006, 35, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Hebbandi Nanjundappa, R.; Sokke Umeshappa, C.; Geuking, M.B. The impact of the gut microbiota on T cell ontogeny in the thymus. Cell Mol. Life Sci. 2022, 79, 221. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chung, H.-H.; Tongkamsai, S.; Cheng, M.-C.; Tsai, Y.-L.; Lee, M.-S.; Lien, Y.-Y.; Chen, Y.-M. Pathogenicity in Chicken Anemia Virus with Eimeria tenella: Concurrent Co-Infection and Secondary Eimeria tenella Infection. Microorganisms 2025, 13, 1676. https://doi.org/10.3390/microorganisms13071676
Chung H-H, Tongkamsai S, Cheng M-C, Tsai Y-L, Lee M-S, Lien Y-Y, Chen Y-M. Pathogenicity in Chicken Anemia Virus with Eimeria tenella: Concurrent Co-Infection and Secondary Eimeria tenella Infection. Microorganisms. 2025; 13(7):1676. https://doi.org/10.3390/microorganisms13071676
Chicago/Turabian StyleChung, Hsyang-Hsun, Suttitas Tongkamsai, Ming-Chu Cheng, Yi-Lun Tsai, Meng-Shiou Lee, Yi-Yang Lien, and Ya-Mei Chen. 2025. "Pathogenicity in Chicken Anemia Virus with Eimeria tenella: Concurrent Co-Infection and Secondary Eimeria tenella Infection" Microorganisms 13, no. 7: 1676. https://doi.org/10.3390/microorganisms13071676
APA StyleChung, H.-H., Tongkamsai, S., Cheng, M.-C., Tsai, Y.-L., Lee, M.-S., Lien, Y.-Y., & Chen, Y.-M. (2025). Pathogenicity in Chicken Anemia Virus with Eimeria tenella: Concurrent Co-Infection and Secondary Eimeria tenella Infection. Microorganisms, 13(7), 1676. https://doi.org/10.3390/microorganisms13071676





