DNA from Lactobacillus paragasseri SBT2055 Activates Plasmacytoid Dendritic Cells and Induces IFN-α via TLR9
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of LG2055
2.2. DNA Extraction
2.3. Lipoteichoic Acid (LTA) and Peptidoglycan (PGN) Preparation
2.4. DNA Digestion
2.5. PGN Digestion
2.6. PBMC Culture
2.7. pDC Isolation from PBMCs
2.8. Flow Cytometric Analysis of pDC Activity
2.9. Enzyme-Linked Immunosorbent Assay (ELISA)
2.10. Phagocytosis Assays
2.11. In Vitro M Cell Model
2.12. Statistical Analysis
3. Results
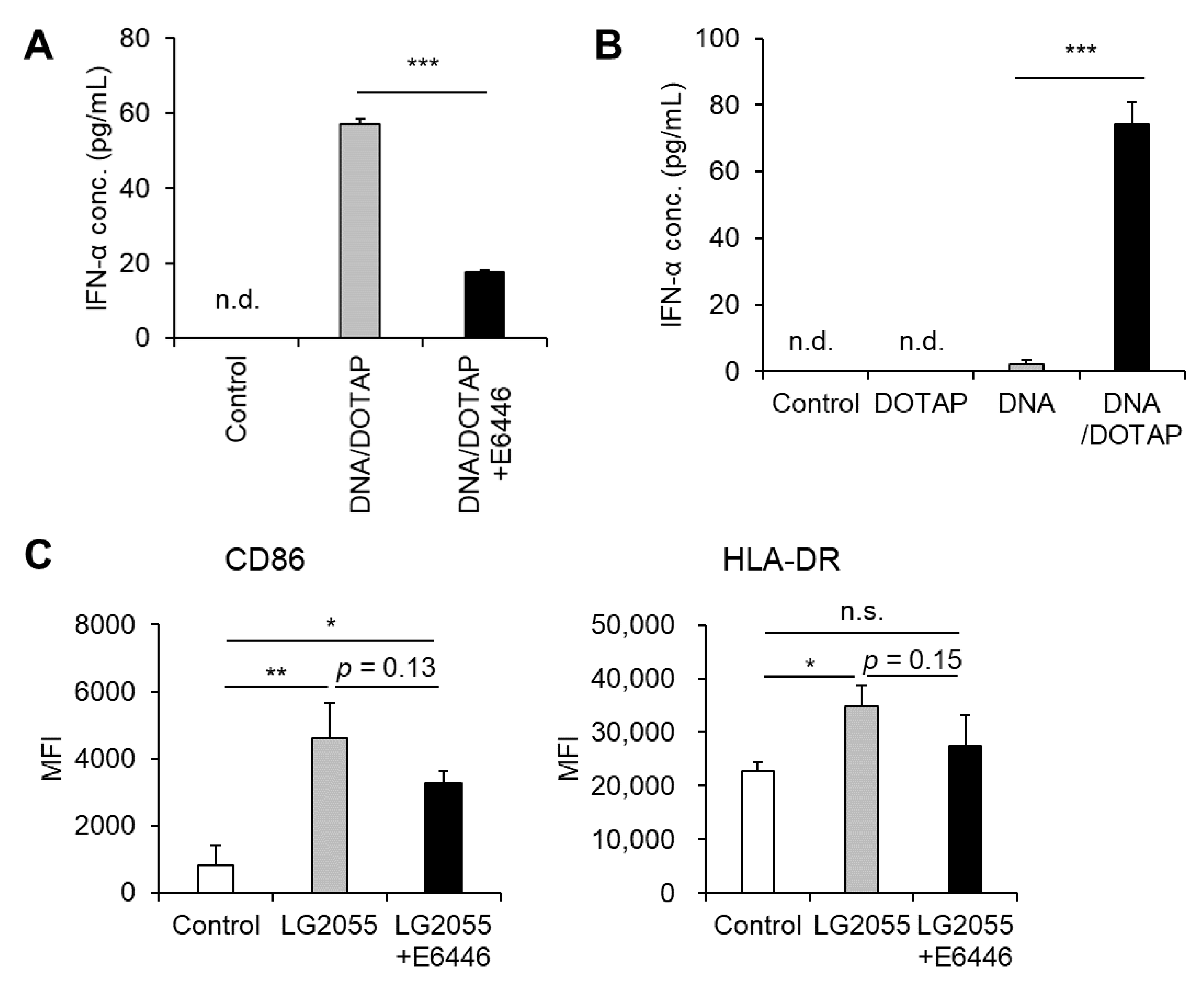
3.1. LG2055 Induced pDC Activation and Promoted Type I IFN Production
3.2. TLR9 Mediated LG2055 DNA-Induced Type I IFN Production
3.3. LG2055 Was Taken up by Intestinal M Cells and Phagocytosed by pDCs
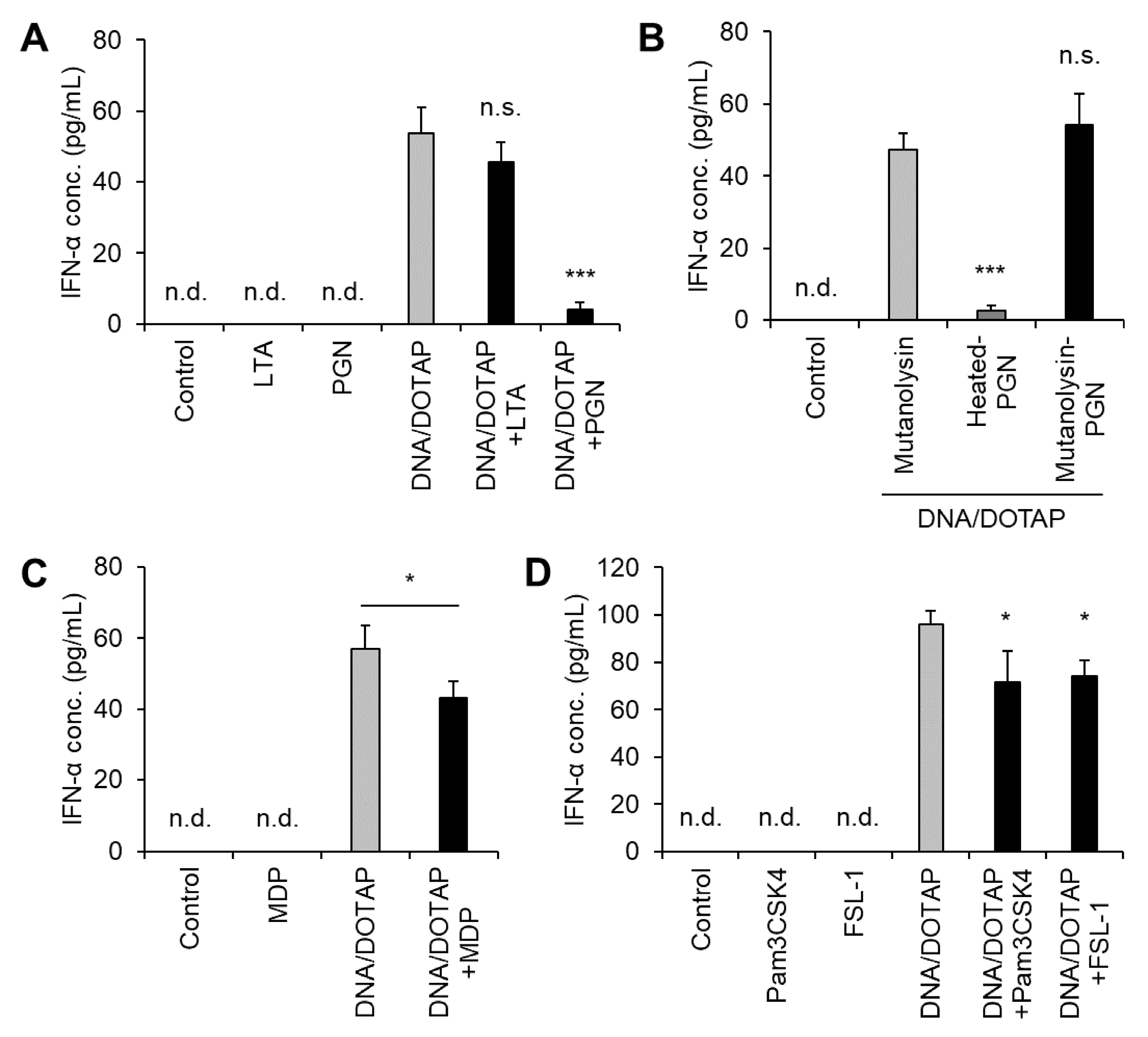
3.4. LG2055 PGN Suppressed IFN-α Production Induced by LG2055 DNA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of variance |
| BSA | Bovine serum albumin |
| CpG | cytosine-phosphate-guanine |
| DMEM | Dulbecco’s Modified Eagle’s Medium |
| DOTAP | 1,2-dioleoyl-3-trimethylammonium-propane |
| ELISA | Enzyme-linked immunosorbent assay |
| FBS | Fetal bovine serum |
| HBS | HEPES-buffered saline |
| IgA | Immunoglobulin A |
| IFN | Interferon |
| LAB | Lactic acid bacteria |
| LG2055 | Lactobacillus paragasseri SBT2055 |
| LTA | Lipoteichoic acid |
| MDP | Muramyl dipeptide |
| MRS | de Man, Rogosa, and Sharpe |
| PBMC | Peripheral blood mononuclear cell |
| PBS | Phosphate-buffered saline |
| PGN | Peptidoglycan |
| pDC | Plasmacytoid dendritic cell |
| PPs | Peyer’s patches |
| RPMI | Rosswell Park Memorial Institute |
| TLR | Toll-like receptor |
References
- Seto, Y.; Kimura, A.; Akai, Y.; Fujiwara, S. Distribution of the Lactobacillus acidophilus complex in human fecal specimens examined by restriction fragment length polymorphism of the 16S rRNA genes. Biosci. Microflora 2003, 22, 75–83. [Google Scholar] [CrossRef][Green Version]
- Takahashi, H.; Fujita, T.; Suzuki, Y.; Benno, Y. Monitoring and survival of Lactobacillus gasseri SBT2055 in the human intestinal tract. Microbiol. Immunol. 2006, 50, 867–870. [Google Scholar] [CrossRef]
- Kobayashi, T.; Takano, Y.; Akai, Y.; Ikuyama, K.; Kawasaki, Y.; Tsuchida, T. Safety evaluation of excessive intake of fermented milk containing the probiotic Lactobacillus gasseri SBT2055. Jpn. Pharmacol. Ther. 2013, 41, 989–997. [Google Scholar]
- Nakayama, Y.; Moriya, T.; Sakai, F.; Ikeda, N.; Shiozaki, T.; Hosoya, T.; Nakagawa, H.; Miyazaki, T. Oral administration of Lactobacillus gasseri SBT2055 is effective for preventing influenza in mice. Sci. Rep. 2014, 4, 4638. [Google Scholar] [CrossRef] [PubMed]
- Eguchi, K.; Fujitani, N.; Nakagawa, H.; Miyazaki, T. Prevention of respiratory syncytial virus infection with the probiotic lactic acid bacterium Lactobacillus gasseri SBT2055. Sci. Rep. 2019, 9, 4812. [Google Scholar] [CrossRef] [PubMed]
- Sakai, F.; Hosoya, T.; Ono-Ohmachi, A.; Ukibe, K.; Ogawa, A.; Moriya, T.; Kadooka, Y.; Shiozaki, T.; Nakagawa, H.; Nakayama, Y.; et al. Lactobacillus gasseri SBT2055 induces TGF-β expression in dendritic cells and activates TLR2 signaling to produce IgA in the small intestine. PLoS ONE 2014, 9, e105370. [Google Scholar] [CrossRef]
- Nishihira, J.; Moriya, T.; Sakai, F.; Kabuki, T.; Kawasaki, Y.; Nishimura, M. Lactobacillus gasseri SBT2055 stimulates immunoglobulin production and innate immunity after influenza vaccination in healthy adult volunteers: A randomized, double-blind, placebo-controlled, parallel-group study. Funct. Foods Health Dis. 2016, 6, 544–568. [Google Scholar] [CrossRef]
- Kobatake, E.; Iwama, Y.; Arai, T.; Shioya, N.; Kise, M.; Kabuki, T. Intake of Lactobacillus paragasseri SBT2055 improves subjective symptoms of common cold during the winter season in healthy adults: A randomized, double-blind, placebo-controlled parallel-group comparative study. Front. Nutr. 2022, 9, 1063584. [Google Scholar] [CrossRef]
- Kobatake, E.; Iwama, Y.; Arai, T.; Tsukisaka, Y.; Kabuki, T. Lactobacillus paragasseri SBT2055 activates plasmacytoid dendritic cells and improves subjective symptoms of common cold in healthy adults: A randomized, double-blind, placebo-controlled parallel-group comparative trial. Nutrients 2023, 15, 4458. [Google Scholar] [CrossRef]
- Colonna, M.; Trinchieri, G.; Liu, Y.J. Plasmacytoid dendritic cells in immunity. Nat. Immunol. 2004, 5, 1219–1226. [Google Scholar] [CrossRef]
- Arroyo Hornero, R.; Idoyaga, J. Plasmacytoid dendritic cells: A dendritic cell in disguise. Mol. Immunol. 2023, 159, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Krug, A.; Rothenfusser, S.; Hornung, V.; Jahrsdörfer, B.; Blackwell, S.; Ballas, Z.K.; Endres, S.; Krieg, A.M.; Hartmann, G. Identification of CpG oligonucleotide sequences with high induction of IFN-alpha/beta in plasmacytoid dendritic cells. Eur. J. Immunol. 2001, 31, 2154–2163. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Yao, H.P.; Lv, G.C.; Chen, Z. Downregulation of TLR7/9 leads to deficient production of IFN-α from plasmacytoid dendritic cells in chronic hepatitis B. Inflamm. Res. 2012, 61, 997–1004. [Google Scholar] [CrossRef]
- Kader, M.; Smith, A.P.; Guiducci, C.; Wonderlich, E.R.; Normolle, D.; Watkins, S.C.; Barrat, F.J.; Barratt-Boyes, S.M. Blocking TLR7- and TLR9-mediated IFN-α production by plasmacytoid dendritic cells does not diminish immune activation in early SIV infection. PLoS Pathog. 2013, 9, e1003530. [Google Scholar] [CrossRef] [PubMed]
- Horie, A.; Tomita, Y.; Ohshio, K.; Fujiwara, D.; Fujii, T. Characterization of genomic DNA of lactic acid bacteria for activation of plasmacytoid dendritic cells. BMC Microbiol. 2019, 19, 88. [Google Scholar] [CrossRef]
- Dalpke, A.; Frank, J.; Peter, M.; Heeg, K. Activation of Toll-like receptor 9 by DNA from different bacterial species. Infect. Immun. 2006, 74, 940–946. [Google Scholar] [CrossRef]
- Ohto, U.; Ishida, H.; Shibata, T.; Sato, R.; Miyake, K.; Shimizu, T. Toll-like receptor 9 contains two DNA binding sites that function cooperatively to promote receptor dimerization and activation. Immunity 2018, 48, 649–658.e4. [Google Scholar] [CrossRef]
- Raieli, S.; Trichot, C.; Korniotis, S.; Pattarini, L.; Soumelis, V. TLR1/2 orchestrate human plasmacytoid predendritic cell response to gram-positive bacteria. PLoS Biol. 2019, 17, e3000209. [Google Scholar] [CrossRef]
- Katsuki, R.; Shiraishi, T.; Sakata, S.; Hirota, T.; Nakamura, Y.; Yokota, S. Inhibitory effect of the glycerophosphate moiety of lipoteichoic acid from lactic acid bacteria on dexamethasone-induced Atrogin-1 expression in C2C12 myotubes. J. Nutr. Sci. Vitaminol. 2021, 67, 351–357. [Google Scholar] [CrossRef]
- Kobatake, E.; Kabuki, T. S-layer protein of Lactobacillus helveticus SBT2171 promotes human β-defensin 2 expression via TLR2-JNK signaling. Front. Microbiol. 2019, 10, 2414. [Google Scholar] [CrossRef]
- Gullberg, E.; Leonard, M.; Karlsson, J.; Hopkins, A.M.; Brayden, D.; Baird, A.W.; Artursson, P. Expression of specific markers and particle transport in a new human intestinal M-cell model. Biochem. Biophys. Res. Commun. 2000, 279, 808–813. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Jounai, K.; Ikado, K.; Sugimura, T.; Ano, Y.; Braun, J.; Fujiwara, D. Spherical lactic acid bacteria activate plasmacytoid dendritic cells’ immunomodulatory function via TLR9-dependent crosstalk with myeloid dendritic cells. PLoS ONE 2012, 7, e32588. [Google Scholar] [CrossRef]
- Shimosato, T.; Kitazawa, H.; Katoh, S.; Tohno, M.; Iliev, I.D.; Nagasawa, C.; Kimura, T.; Kawai, Y.; Saito, T. Augmentation of TH-1 type response by immunoactive AT oligonucleotide from lactic acid bacteria via Toll-like receptor 9 signaling. Biochem. Biophys. Res. Commun. 2005, 326, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Aoki, T.; Iwabuchi, S.; Arai, S.; Iwabuchi, N.; Motobayashi, H.; Tanaka, M.; Hashimoto, S. Immunomodulatory activity of heat-killed Lacticaseibacillus paracasei MCC1849 based on the activation of plasmacytoid dendritic cells in the peripheral blood of healthy adults. Food Sci. Nutr. 2024, 12, 3452–3460. [Google Scholar] [CrossRef] [PubMed]
- Shida, K.; Kiyoshima-Shibata, J.; Nagaoka, M.; Watanabe, K.; Nanno, M. Induction of interleukin-12 by Lactobacillus strains having a rigid cell wall resistant to intracellular digestion. J. Dairy Sci. 2006, 89, 3306–3317. [Google Scholar] [CrossRef]
- Yoshikawa, M.; Yamada, S.; Sugamata, M.; Kanauchi, O.; Morita, Y. Dectin-2 mediates phagocytosis of Lactobacillus paracasei KW3110 and IL-10 production by macrophages. Sci. Rep. 2021, 11, 17737. [Google Scholar] [CrossRef]
- Moretti, J.; Blander, J.M. Insights into phagocytosis-coupled activation of pattern recognition receptors and inflammasomes. Curr. Opin. Immunol. 2014, 26, 100–110. [Google Scholar] [CrossRef]
- Taverniti, V.; Marengo, M.; Fuglsang, E.; Skovsted, H.M.; Arioli, S.; Mantegazza, G.; Gargari, G.; Iametti, S.; Bonomi, F.; Guglielmetti, S.; et al. Surface layer of Lactobacillus helveticus MIMLh5 promotes endocytosis by dendritic cells. Appl. Environ. Microbiol. 2019, 85, e00138-19. [Google Scholar] [CrossRef]
- Franklin, B.S.; Ishizaka, S.T.; Lamphier, M.; Gusovsky, F.; Hansen, H.; Rose, J.; Zheng, W.; Ataíde, M.A.; de Oliveira, R.B.; Golenbock, D.T.; et al. Therapeutical targeting of nucleic acid-sensing Toll-like receptors prevents experimental cerebral malaria. Proc. Natl. Acad. Sci. USA 2011, 108, 3689–3694. [Google Scholar] [CrossRef]
- Sugimura, T.; Jounai, K.; Ohshio, K.; Tanaka, T.; Suwa, M.; Fujiwara, D. Immunomodulatory effect of Lactococcus lactis JCM5805 on human plasmacytoid dendritic cells. Clin. Immunol. 2013, 149, 509–518. [Google Scholar] [CrossRef] [PubMed]
- Sugimura, T.; Takahashi, H.; Jounai, K.; Ohshio, K.; Kanayama, M.; Tazumi, K.; Tanihata, Y.; Miura, Y.; Fujiwara, D.; Yamamoto, N. Effects of oral intake of plasmacytoid dendritic cell-stimulative lactic acid bacterial strain on pathogenesis of influenza-like illness and immunological response to influenza virus. Br. J. Nutr. 2015, 114, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Arai, S.; Sato, S.; Iwabuchi, N.; Takara, T.; Tanaka, M. Effects of heat-killed Lacticaseibacillus paracasei MCC1849 on immune parameters in healthy adults: A randomized, double-blind, placebo-controlled, parallel-group study. Nutrients 2024, 16, 216. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Arai, S.; Iwabuchi, N.; Tanaka, M.; Hase, R.; Sakane, N. Effects of heat-killed Lacticaseibacillus paracasei MCC1849 on the maintenance of physical condition in healthy adults: A randomized, double-blind, placebo-controlled, parallel-group study. Nutrients 2023, 15, 3450. [Google Scholar] [CrossRef]
- Bonnardel, J.; Da Silva, C.; Henri, S.; Tamoutounour, S.; Chasson, L.; Montañana-Sanchis, F.; Gorvel, J.P.; Lelouard, H. Innate and adaptive immune functions of Peyer’s patch monocyte-derived cells. Cell Rep. 2015, 11, 770–784. [Google Scholar] [CrossRef]
- Da Silva, C.; Wagner, C.; Bonnardel, J.; Gorvel, J.P.; Lelouard, H. The Peyer’s Patch Mononuclear Phagocyte System at Steady State and during Infection. Front. Immunol. 2017, 8, 1254. [Google Scholar] [CrossRef]
- Aoki-Yoshida, A.; Yamada, K.; Hachimura, S.; Sashihara, T.; Ikegami, S.; Shimizu, M.; Totsuka, M. Enhancement of Oral Tolerance Induction in DO11.10 Mice by Lactobacillus gasseri OLL2809 via Increase of Effector Regulatory T Cells. PLoS ONE 2016, 11, e0158643. [Google Scholar] [CrossRef]
- Sekirov, I.; Russell, S.L.; Antunes, L.C.; Finlay, B.B. Gut microbiota in health and disease. Physiol. Rev. 2010, 90, 859–904. [Google Scholar] [CrossRef]
- Fujiwara, S.; Seto, Y.; Kimura, A.; Hashiba, H. Establishment of orally administered Lactobacillus gasseri SBT2055SR in the gastrointestinal tract of humans and its influence on intestinal microflora and metabolism. J. Appl. Microbiol. 2001, 90, 343–352. [Google Scholar] [CrossRef]
- Simmons, D.P.; Canaday, D.H.; Liu, Y.; Li, Q.; Huang, A.; Boom, W.H.; Harding, C.V. Mycobacterium tuberculosis and TLR2 agonists inhibit the induction of type I IFN and class I MHC antigen cross-processing by TLR9. J. Immunol. 2010, 185, 2405–2415. [Google Scholar] [CrossRef]
- Liu, Y.C.; Simmons, D.P.; Li, X.; Abbott, D.W.; Boom, W.H.; Harding, C.V. TLR2 signaling depletes IRAK1 and inhibits the induction of type I IFN and class I MHC antigen cross-processing by TLR7/9. J. Immunol. 2012, 188, 1019–1026. [Google Scholar] [CrossRef]
- Masuta, Y.; Minaga, K.; Kurimoto, M.; Sekai, I.; Hara, A.; Omaru, N.; Okai, N.; Otsuka, Y.; Takada, R.; Yoshikawa, T.; et al. Activation of nucleotide-binding oligomerization domain 2 by muramyl dipeptide negatively regulates Toll-like receptor 9-mediated colonic inflammation through the induction of deubiquitinating enzyme A expression. Int. Immunol. 2023, 35, 79–94. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Wu, M. Pattern recognition receptors in health and diseases. Signal Transduct. Target. Ther. 2021, 6, 291. [Google Scholar] [CrossRef]
- Shiraishi, T.; Yokota, S.; Fukiya, S.; Yokota, A. Structural diversity and biological significance of lipoteichoic acid in Gram-positive bacteria: Focusing on beneficial probiotic lactic acid bacteria. Biosci. Microflora Food Health 2016, 35, 147–161. [Google Scholar] [CrossRef] [PubMed]
- Ryu, Y.H.; Baik, J.E.; Yang, J.S.; Kang, S.S.; Im, J.; Yun, C.H.; Kim, D.W.; Lee, K.; Chung, D.K.; Ju, H.R.; et al. Differential immunostimulatory effects of Gram-positive bacteria due to their lipoteichoic acids. Int. Immunopharmacol. 2009, 9, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, T.; Yokota, S.; Morita, N.; Fukiya, S.; Tomita, S.; Tanaka, N.; Okada, S.; Yokota, A. Characterization of a Lactobacillus gasseri JCM 1131T lipoteichoic acid with a novel glycolipid anchor structure. Appl. Environ. Microbiol. 2013, 79, 3315–3318. [Google Scholar] [CrossRef]
- Shiraishi, T.; Kutomi, R.; Sato, Y.; Morita, N.; Fukiya, S.; Sato, T.; Yokota, A.; Yokota, S.I. A unique species-specific structure of lipoteichoic acid common to Lactobacillus gasseri. Endotoxin Innate Immun. 2018, 21, 35–37. [Google Scholar] [CrossRef]
- Aghamohammad, S.; Sepehr, A.; Miri, S.T.; Najafi, S.; Pourshafie, M.R.; Rohani, M. Anti-inflammatory and immunomodulatory effects of Lactobacillus spp. as a preservative and therapeutic agent for IBD control. Immun. Inflamm. Dis. 2022, 10, e635. [Google Scholar] [CrossRef]
- Li, C.; Peng, K.; Xiao, S.; Long, Y.; Yu, Q. The role of Lactobacillus in inflammatory bowel disease: From actualities to prospects. Cell Death Discov. 2023, 9, 361. [Google Scholar] [CrossRef]
- Kim, M.J.; Shin, S.K.; Han, J.W.; Kim, J.E.; Lee, M.J.; Bae, H.R.; Kwon, E.Y. Lactobacillus paragasseri SBT2055 attenuates obesity via the adipose tissue-muscle-gut axis in obese mice. Microbiol. Res. 2025, 290, 127972. [Google Scholar] [CrossRef]
- Kobatake, E.; Nakagawa, H.; Seki, T.; Miyazaki, T. Protective effects and functional mechanisms of Lactobacillus gasseri SBT2055 against oxidative stress. PLoS ONE 2017, 12, e0177106. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kobatake, E.; Arai, T. DNA from Lactobacillus paragasseri SBT2055 Activates Plasmacytoid Dendritic Cells and Induces IFN-α via TLR9. Microorganisms 2025, 13, 1440. https://doi.org/10.3390/microorganisms13071440
Kobatake E, Arai T. DNA from Lactobacillus paragasseri SBT2055 Activates Plasmacytoid Dendritic Cells and Induces IFN-α via TLR9. Microorganisms. 2025; 13(7):1440. https://doi.org/10.3390/microorganisms13071440
Chicago/Turabian StyleKobatake, Eiji, and Toshinobu Arai. 2025. "DNA from Lactobacillus paragasseri SBT2055 Activates Plasmacytoid Dendritic Cells and Induces IFN-α via TLR9" Microorganisms 13, no. 7: 1440. https://doi.org/10.3390/microorganisms13071440
APA StyleKobatake, E., & Arai, T. (2025). DNA from Lactobacillus paragasseri SBT2055 Activates Plasmacytoid Dendritic Cells and Induces IFN-α via TLR9. Microorganisms, 13(7), 1440. https://doi.org/10.3390/microorganisms13071440





